Abstract
The present study uses latent class methods and multiple regression to shed light on hypothesized cocaine dependence syndromes experienced by community residents, who initiated cocaine use within 24 months of survey assessment, and explores possible variation in risk. Identified within public use data files from the United States National Household Surveys on Drug Abuse (NHSDA), and with assessments completed between 1995 and 1998, the study sample consists of 927 recent-onset cocaine users, defined as having initiated cocaine use no more than 24 months prior to assessment (approximate median elapsed time since onset of use ∼12–13 months). The NHSDA included items to assess seven clinical features often associated with cocaine dependence, which were used in latent class modeling. Empirically derived latent classes, in conjunction with prior theory, tend to support a three-class solution, according to which 4% of recent-onset users are members of a class that resembles the DSM-IV cocaine dependence syndrome (mean: 5.4 clinical features (CF)); 16% might be in a cocaine dependence prodrome (mean: 2.4 CF); 80% of recent-onset cocaine users had few or no clinical features (mean<1 CF). Results from latent class regressions indicate that susceptibility to rapid transition from first cocaine use to onset of the LCA-assigned cocaine dependence syndrome might depend upon whether the user starts smoking crack-cocaine and, independently, age at first cocaine use.
Similar content being viewed by others
INTRODUCTION
In a series of research reports on the epidemiology of cocaine dependence, our research group has followed conventions that originated with the American Psychiatric Association's Diagnostic and Statistical Manuals (DSM) from DSM-III, DSM-IIIR, and DSM-IV. For example, using data from the National Comorbidity Survey, we estimated that about one in six cocaine users had developed a cocaine dependence syndrome (see Anthony et al, 1994), and that there is an explosive onset of DSM-IIIR cocaine dependence during the first 1–2 years after onset of cocaine use. An estimated 5–6% of cocaine users manifest the DSM-IIIR syndrome of cocaine dependence within these first 2 years after onset of use (Wagner and Anthony, 2002). By comparison, we found evidence for a more languorous and insidious onset of cannabis dependence and alcohol dependence, with risk estimates on the order of 1–4% within the first 2 years after first use of these drugs (Wagner and Anthony, 2002). More recently, with estimates from the National Household Surveys on Drug Abuse (NHSDA) conducted between 2000 and 2001, we found additional evidence that some 5–6% of recent-onset cocaine users are developing DSM-IV cocaine dependence syndromes within 24 months after onset of cocaine use (approximate median elapsed time 12–13 months; O'Brien and Anthony, 2005).
In work of this type, there is reason to examine alternatives to the DSM formulations of the cocaine dependence syndrome. First, clinical experts on the DSM task panels tend to base their specifications for diagnostic criteria on the experiences with cocaine users who are seeking treatment for cocaine dependence. However, the cocaine experiences and sociodemographic backgrounds of cocaine treatment seekers and nonseekers can be somewhat different. For example, drawing upon results from the National Institute of Mental Health Epidemiologic Catchment Area (ECA) program, we reported evidence that patterns of DSM-III-ascribed clinical features of cocaine and heroin dependence observed in community survey respondents might be considerably different from corresponding patterns observed in samples of patients seeking drug dependence treatment (Anthony and Petronis, 1989). In a study of adult crack users, Pottieger et al (1995) found that crack users in residential treatment were more likely to use multiple forms of cocaine, to use cocaine in a binge pattern, and to pay for cocaine with cash they got for a job, as compared to street users. Carroll and Rounsaville (1992) found that nontreatment seeking cocaine users tend to minimize negative consequences of cocaine use compared to treatment seeking cocaine users despite equivalent levels of use. Second, a large fraction of cocaine users in treatment take cocaine for many years before seeking treatment (Dennis et al, 2005). Evidence from animal studies suggests that behavioural responses to cocaine are shaped in part by prior cocaine-related behavioural and pharmacological histories (Nader, 1998). This means that the configuration of clinical features of the cocaine dependence syndrome observed in the earliest months and years after onset of cocaine use may not be same as the corresponding clinical features observed after 2 or more years of cocaine self-administration. A third reason to consider an alternative to DSM is that there is a meager evidence base to support combining interdependent clinical features via simple algorithms; subtypes or subgroups of cocaine dependence cases might be missed or ignored unless there is thorough probing of the patterns of interdependencies among clinical features. In addition, simple additive algorithms make no allowance for unreliability of measurement; each reported clinical feature during the field research assessment generally has been accepted at face value.
In order to strengthen the available evidence on the hypothesized explosive onset of cocaine dependence syndromes in the first months and years after onset of cocaine use (eg see Wagner and Anthony, 2002), we have reapproached the task of studying the phenomenon of cocaine dependence among recent-onset cocaine users using data from the 1995–1998 NHSDA and here we present an alternative approach to diagnostic decision rules now used to identify cocaine dependent individuals. Specifically, we use latent class analysis (LCA) to identify subgroups (classes) of recent-onset cocaine users with similar patterns of clinical features of cocaine dependence (Lazarsfeld and Henry, 1968; McCutcheon, 1987; Clogg, 1995; Hagenaars and McCutcheon, 2002). LC analyses of empirical data help us to characterize a cocaine dependence syndrome or syndromes as they emerge soon after onset of cocaine use, and to study underlying patterns of clinical features that might support DSM-like algorithms based on adding up the number of clinical features endorsed or that might disclose subtype differences in qualitative content of syndromes based on which clinical features are endorsed. The aims of this paper are: (1) to use empirical data to characterize the cocaine dependence syndrome among recent-onset cocaine users in a nationally representative sample, (2) to provide new estimates about how many cocaine users might be becoming dependent upon cocaine during this initial interval of cocaine use, and (3) to better understand the variation in the patterns of clinical features of cocaine dependence as manifest early in the course of the disorder. Subgroup variations of particular interest have been defined in relation to age of first cocaine use, male–female differences, race–ethnicity, and form of cocaine use (HCl powder only vs crack and powder). One of the issues that cannot be addressed in this research is the existence of a nondependent ‘abuse’ category that appears in the DSM-IV manuals. In the study data, there were too few indicators of the clinical features of ‘cocaine abuse’ for detailed probing into that particular subclass of cocaine users.
METHODS
Subjects
All data for this study are from the National Household Surveys on Drug Abuse (NHSDA) for the period 1995–1998, with an aggregate community sample size approaching 90 000 individuals (n=86 021). The NHSDA (recently renamed the National Household Surveys of Drug Use and Health) are ongoing cross-sectional surveys of the drug experiences of United States citizens aged 12 years and over. Each year for the past decade, the NHSDA team has drawn nationally representative samples of dwelling units (eg households) and individual respondents via multistage sampling procedures. Potential participants are allowed to decline or refuse participation in accord with a protocol approved by the cognizant Institutional Review Board. During the 1995–1998 intervals, survey participation rates have approached or exceeded 80% (ie 77–81% in recent years). A more detailed description of methods and other information on the NHSDA study population, and each year's sample, are available in published reports (SAMHSA, 1997, 1998, 1999, 2000).
For this study, we combined data from the 1995 to 1998 data files in order to assemble a sample of recent-onset cocaine HCl or crack cocaine users large enough to achieve precision and to reduce statistical uncertainty in the study estimates. During the period of 1995–1998, the NHSDA methods of assessment for each participant's drug experiences were consistent (ie held constant from year to year). These years preceded introduction of the more recent NHSDA methodological innovations such as the use of computerized self-interview methods and changes in assessment of cocaine dependence, which thwarted our attempts to include more recent data. That is, our intent is to complete parallel LCA work with the more recently gathered national survey data from this SAMHSA initiative, but due to differences in assessment methods and sampling plans, our approach is stepwise, with an intent to derive initial estimates based upon the 1995–1998 data, and to probe the robustness of these estimates with the later survey data.
Assessments
For the 1995–1998 NHSDA, survey respondents generally filled out a self-administered answer sheet in response to standardized survey questions, in order to provide information about their drug experiences and other personal characteristics (eg age, sex, minority group membership). A small number of respondents chose to have the interviewer read the questions aloud and then mark the answers for them.
For cocaine involvement, each participant responded to a series of standardized questions (eg age of first use; number of cumulative days of use since first occasion of use) for ‘all forms of cocaine (including cocaine HCl powder and crack cocaine)’. A small subset of these questions asked about ‘crack cocaine’ separately. Seven clinical features associated with recently active DSM-IV cocaine dependence were assessed by means of standardized items that asked about experiences during the year prior to assessment for active users of any form of cocaine. For our analyses on each individual clinical feature, we created a variable coded ‘1’ for users whose experience included that feature; the code was ‘0’ when the feature was not experienced. The responses to these seven items on cocaine dependence formed the basis for our LCA.
The cocaine users were not asked to attribute their cocaine problems to cocaine HCl powder vs crack. For this reason, we have not had to rely on subjective causal attributions to one or another form of cocaine use. Instead, we have been able to estimate risk of cocaine dependence as a function of the form of recent-onset cocaine experiences (ie nasal insufflation of cocaine HCl powder with and without crack smoking), using multiple regression methods (in lieu of asking users what caused what).
For this project, recent-onset cocaine HCl users were identified as those who reported having used cocaine HCl powder in the year prior to assessment, and whose age at first use of cocaine HCl powder was equal to the age at the time of assessment, or was no more than 1 year different from the age of assessment. Similar criteria were also applied to identify recent-onset crack users. Then, the accumulated total of 927 recent-onset users of powder and/or crack was categorized into subgroups. The first subgroup consisted of 699 individuals who had just started to use powder but never smoked crack. The second subgroup included 228 recent-onset crack-smokers who also were recent-onset cocaine HCl powder users or who had a pre-existing history of having used cocaine HCl powder. We were unable to identify recent-onset crack smokers with no concurrent or past history of using cocaine HCl powder.
Hereinafter, as shown in Table 1, ‘Cocaine HCl’ refers to recent-onset users of cocaine hydrochloride only (no history of crack use). ‘Crack+Powder’ refers to recent-onset crack users also with recent-onset use of cocaine HCl powder or a past history of HCl powder use. If crack-smoking exacerbates risk of cocaine dependence among users of cocaine HCl powder, we would expect to see lower risk values for the first subgroup for recent-onset users of cocaine HCl powder with no crack experiences. Higher risk of cocaine dependence should be seen in the other subgroup with recent-onset crack smoking against a background of recent or earlier onset of cocaine HCl powder self-administration.
Statistical Analyses
Latent class analysis (LCA) was used to identify classes of recent-onset cocaine users with similar patterns of clinical features of cocaine dependence using Latent GOLD Version 3.0 (Vermunt and Magidson, 2003). The goal of LCA is to identify the smallest number of latent classes that adequately describes the associations among the clinical features (Bansfield and Raftery, 1993; Bandeen-Roche et al, 1999; Magidson and Vermunt, 2000). As such, the model building strategy involved starting with the most parsimonious one class model (‘all recent-onset cocaine users the same’) and fitting successive models with increasing numbers of classes. Conventional goodness of fit statistics were used to select the optimal model and to probe the standard assumption of local independence that the specified number of classes is sufficient to explain the associations among the clinical features. To clarify the nature of the derived latent classes of the cocaine dependence syndrome from the best fitting model, respondents were assigned to LCA-derived cocaine dependence classes based on their estimated posterior probabilities of class membership given their observed patterns of clinical features. Individual-level class membership indicators were then treated as dependent variables in multinomial logistic regression analyses performed in STATA Version 7.0 (STATA, 2000) and relationships with sex (male/female), age at onset, race–ethnicity, and form of cocaine used were explored. Owing to the stratification and clustering present in the NHSDA data, it can be useful to account for sample design features within the analysis. We used Taylor series estimation methods (STATA svy regression commands) to obtain proper standard error estimates. As it happened, in this instance, when we compared these estimates with and without attention to design features, we found that the results did not differ appreciably. As noted below, the LCA results sometimes yielded latent classes with some 40–50 users within a class; in order to probe the statistical stability of the estimates, we used a bootstrap resampling approach.
RESULTS
Table 1 characterizes the aggregate NHSDA study sample of recent-onset cocaine users in relation to (a) age of first cocaine use, (b) form of cocaine use (HCl powder vs ‘Crack plus Powder’), (c) sex (male vs female), and (d) race-ethnicity. As shown, almost 19% of these recent-onset users had initiated cocaine use during young adulthood (age 21–29 years), whereas the others were adolescent-onset cocaine users. Roughly 25% had initiated ‘crack-smoking’ by the time of survey assessment, but the vast majority had used cocaine HCl powder only. The female-male ratio among recent-onset cocaine users in this sample was 49:51. Only about four percent (4%) self-identified as non-Hispanic Blacks; 31% were Hispanics without African heritage; almost 60% were self-designated as non-Hispanic Whites; and 7.4% were in an ‘other’ category that includes people of Asian heritage, Pacific Islanders, Native Americans, and others.
The estimated prevalence of each clinical feature associated with cocaine dependence is presented in Table 2. Overall, being unable to stop or cut down on cocaine use (cut down), spending a great deal of time getting or using cocaine (salience), using cocaine much more often or in larger amounts than intended (control), and having experienced emotional or psychological problems (emotional) attributed to cocaine use were the most commonly experienced clinical features of the cocaine users who had initiated cocaine use within the 24 months prior to survey assessment. Subjectively felt tolerance (tolerance), narrowing of the nondrug behavioural repertoire (narrowing), and health problems (health) attributed to cocaine were seen less often. The occurrence of each clinical feature varied somewhat in relation to sex, race, age of onset, and form of cocaine used (HCl powder only vs ‘crack plus powder’). As compared to female cocaine users, males were less likely to experience narrowing of their nondrug behaviour repertoire (estimated odds ratio, OR=0.5, p=0.02), spending a month or more getting and using cocaine (OR=0.6, p=0.03), and using cocaine more often than intended (OR=0.6, p=0.03). In contrast to non-Hispanic Whites and Hispanics, other minorities were more likely to experience narrowing of their nondrug behavioural repertoire (OR=2.6, p=0.01 and OR=2.5, p=0.03, respectively) and failed efforts to cut down on cocaine use (OR=2.0, p=0.02 and OR=1.7, p=0.10). None of the Non-Hispanic Blacks had experienced narrowing of their non-drug behaviour repertoire; roughly 3% described failed efforts to cut down. As compared to users of HCl powder, the crack cocaine users were more likely to report clinical features of the cocaine dependence syndrome (OR ranging from 2.0 to 3.9, p<0.02), a detail already probed by Chen and Anthony (2004).
We noted several age differences in the occurrence of these clinical features. However, many of these contrasts were at the margin of conventional frequentist standards for statistical significance (ie alpha set at 0.05), and should be regarded as tentative until they can be confirmed in later research. Nonetheless, if we relax the conventional frequentist standards, those first using cocaine between the ages of 18 and 29 were less likely to experience clinical features, as compared to those initiating in early adolescence (OR ranging from 0.1 to 0.6, p<0.10). Compared to individuals initiating cocaine use in early adolescence, those who initiated their cocaine use during middle adolescence (ages 15–17) were less likely to experience several of the clinical features of cocaine dependence (OR=0.6, p<0.10); exceptions were having cocaine-associated emotional problems, cocaine-associated health problems, and experiencing a period of 1 month or more when the user spent a great deal of time getting cocaine, using cocaine, or getting over its effects.
Latent class models were fit to the data on the patterns of clinical features associated with cocaine dependence. One of the global fit measures, the Akaike Information Criterion, favoured a four-class (4C) model relative to a three-class (3C) model (4C_AIC=−79.3 vs 3C_AIC=−66.1, where smaller is better). However, an alternative fit index, the Bayesian Information Criterion (BIC) supported a two-class model (2C_BIC=−580.3, 3C_BIC=−568.6, 4C_BIC=−543.2). While Lin and Dayton (1997) argue that the AIC is more appropriate than the BIC for complex latent class models, others have argued that the AIC is an inconsistent and overly liberal indicator of the number of classes (McLachlan and Peel, 2000). Nevertheless, within the framework of a comprehensive latent class analysis, there are considerations other than global goodness-of-fit indices. For example, an LCA investigator generally would like to see that there are no statistically robust residual pairwise associations among the clinical features, once the basic LCA model has been held constant. Probing for residual associations between clinical features, we found that the fit of the 2-class model was compromised by statistically robust residuals between: (1) cocaine-associated problems with health and cocaine-associated narrowing of the nondrug behavioural repertoire, and (2) cocaine-associated problems with health and cocaine-associated emotional problems (data not shown). The addition of a third class explained these residual associations among clinical features providing support for a 3C model over a 2C model. Despite the fact that the 4C model had a smaller AIC value, no statistically significant residuals were found for the 3C model. As such, we have presented results for both the more parsimonious 3C model in addition to the 4C model.
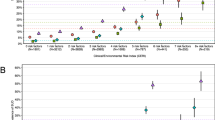
Figure 1 plots the estimated prevalence for each clinical feature associated with cocaine dependence among recent-onset cocaine users under the 3C model. Classes differed not only in relation to a severity or intensity dimension (increase in the prevalence of clinical features across classes), but also in content indicated by patterns of clinical features that were endorsed more or less frequently by members assigned to each latent class. For example, under the 3C model, the mean number of clinical features observed among recent-onset cocaine users in Class 1 was a value between zero and one, representing a group of individuals yet to develop much in the way of clinical features associated with cocaine dependence; the estimated prevalence of Class 1 among recent-onset cocaine users is 80%. For recent-onset cocaine users assigned to Class 2, a mean of 2.4 clinical features was found, which would imply a relatively low level of cocaine dependence (eg as gauged against DSM-type criteria); estimated prevalence of assignment to Class 2 among recent-onset cocaine users is 16%. By comparison, the third class of recent-onset cocaine users experienced a mean of 5.4 clinical features associated with cocaine dependence, and the estimated prevalence of recent-onset cocaine users assigned to this class was 4%. In addition to an observed excess probability of experiencing cocaine-associated clinical features relative to Classes 1 and 2 members, the members of Class 3 are characterized by an especially high probability of reporting narrowing of the nondrug behavioural repertoire, one of the hallmarks of a cocaine dependence syndrome.
A study of the results based upon the 4C model provided evidence of content differences between the classes found among recent-onset cocaine users (Figure 2). Under this 4C model, Class 2 recent-onset users have a higher probability of experiencing each cocaine-associated clinical feature as compared to their counterparts in Class 1. However, under this model, Classes 3 and 4 are qualitatively distinct; moreover, the clinical feature of cocaine-associated health problems violates a standard monotonicity assumption in that it occurs very rarely among members assigned to Class 3, as shown in Figure 2. In addition, loss of control over cocaine use occurs more often among members of Class 3 than it does among members of Class 4 (Figure 2). In contrast, recent-onset users assigned to Class 4 have especially high probabilities of reporting three clinical features that often occur among patients with DSM-specified cocaine dependence syndromes, even though two of these clinical features are not distinctive features with respect to DSM cocaine dependence. For example, among members of Class 4 recent-onset cocaine users, 98% have experienced emotional problems attributed to cocaine, and 92% have experienced health problems attributed to cocaine. Within Class 4, an estimated 82% have experienced narrowing of the nondrug behavioural repertoire due to their use of cocaine, which is a clinical feature that generally helps to discriminate individuals who have developed cocaine dependence. The estimated prevalences are 5 and 4% for Classes 3 and 4, respectively. If subsequent research confirms that both of these classes are different sub-types of cocaine dependence then we should sum the estimated prevalence of Class 3 (5%) with the estimated prevalence of Class 4 (4%), yielding an estimate that 9% of recent-onset cocaine users have developed one or another form of cocaine dependence within 24 months after starting cocaine use.
Between 1995 and 1998, the standard NHSDA approach to ascertainment of DSM-IIIR cocaine dependence was to require three reported clinical features among those surveyed. In an exploratory analysis, we estimated the associations between this approach to ‘diagnosing’ cocaine dependence in relation to the latent class approaches. According to the 3C model, an estimated 0.1% of recent-onset cocaine users assigned to Class 1 had experienced three or more clinical features of cocaine dependence, and by comparison, an estimated 99.1% of the recent-onset cocaine users assigned to Class 3 had experienced at least three of the clinical features under study. Within the intermediate class, an estimated 46.9% of the Class 2 members had experienced at least three of these clinical features. According to the 4C model, an estimated 99.3% of the Class 4 members had experienced at least three of the cocaine-associated clinical features; the corresponding estimate for Class 3 members was 90.5%.
To learn more about the LCA-derived classes of cocaine dependence among recent-onset cocaine users, multinomial logistic regression analyses were completed to estimate associations with demographic and cocaine characteristics. These regression analyses cover the two LCA models best supported by prior evidence and theory namely, the 3C model and the 4C model. We note that when respondents are randomly assigned to latent classes based on their estimated class membership probabilities, some degree of misclassification error is likely to arise. However, the estimated classification error rates were a respectable 5 and 9% for the three- and 4C models, respectively. With respect to the 3C model, we found statistically robust and independent associations that linked crack-smoking with risk of becoming cocaine dependent, as specified under the 3C model; independently, earlier-onset cocaine use was associated with risk of becoming cocaine dependent. For example, as shown in Table 3, when a recent-onset cocaine user has started to smoke crack-cocaine, that user is an estimated 3.6 times more likely to be assigned to Class 3 of the 3C model, as compared to a recent-onset user with only cocaine HCl powder use. Interpreted as an adjusted relative risk (aRR) estimate, the resulting values are consistent with excess risk of developing cocaine dependence (aRR=3.6; 95% confidence interval, CI=1.6, 8.0). A less pronounced but noteworthy association is seen in relation to Class 2 under the 3C model (aRR=1.9; 95% CI=1.3, 2.9). Independently, when a recent-onset cocaine user has started to use cocaine in young adulthood (age 21–29 years), that user is an estimated 1/10th as likely to be assigned to Class 3 of the 3C model, as compared to a recent-onset user who started to use cocaine during the early years of adolescence. Interpreted as an adjusted relative risk (aRR) estimate, the resulting values are consistent with markedly lower risk of developing cocaine dependence when cocaine use starts in young adulthood (aRR=0.1; 95% CI=0.01, 0.6). Here also, a less pronounced but noteworthy inverse association also is seen in relation to Class 2 under the 3C model (aRR=0.4; 95% CI=0.2, 0.8; Table 3). Under this 3C model, there is no support for the idea that cocaine dependence occurs more explosively within the 24 months after onset of cocaine use for males vs females, or for one race-ethnicity subgroup vs another.
Under the 4C model, a similar pattern of associations is observed. Here also the onset of crack-smoking is associated with an excess risk of experiencing clinical features associated with cocaine dependence (see Table 4, with respect to the Classes 2, 3, and 4 estimates). In addition, the onset of cocaine use during young adulthood is associated with a reduced risk of experiencing clinical features associated with cocaine dependence. For example, crack-smoking is associated with an estimated 4.3 fold excess risk of membership in Class 3 (95% CI=2.3, 8.0) and an estimated 2.7 fold excess risk of membership in Class 4 (95% CI=1.2, 5.7) within 24 months after onset of cocaine use. Independently, those starting to use cocaine at age 21–29 years are an estimated 0.2 times as likely to become members of Class 4 within 24 months after onset of cocaine use, as compared to those starting to use cocaine at age 11–14 years (Table 4).
DISCUSSION
The epidemiological evidence of this study generally helps to confirm prevailing estimates that no more than about 6% of cocaine users develop cocaine dependence syndromes within 24 months after onset of cocaine use, as previously reported by Wagner and Anthony (2002), who analysed data from the National Comorbidity Survey, and by O'Brien and Anthony (2005), who analysed data from recent National Surveys on Drug Use and Health. Here, if Class 3 of the 3C model is assumed to be correct, an estimated 4% of recent-onset cocaine users have developed the syndrome of cocaine dependence within a short interval of time after onset of cocaine use. If Classes 3 and 4 of the 4C model are assumed to be different subtypes or subforms of cocaine dependence, then in aggregate, an estimated nine percent of recent-onset cocaine users have developed a cocaine dependence syndrome within 24 months after onset of cocaine use, with 4% assigned to Class 4 cocaine dependence and 5% assigned to Class 3 cocaine dependence under this model. Of course, for any observer who is wedded to the Bayesian Information Criterion as an index of model fit, the 2C model is to be preferred. Under these circumstances, the estimated risk of becoming cocaine dependent within 24 months after onset of cocaine use is roughly 16%—a value that is substantially larger than previously published estimates. Two conditions motivate our research group to favour the 3C or 4C models rather than the 2C model. These conditions are: (i) incongruence of the 2C model relative to previously derived estimates of risk to develop cocaine dependence, all based upon DSM criteria, and (ii) violations of the local independence assumption probed via pairwise residuals, as described in the Results section.
We were somewhat surprised that classification of cocaine dependence by the LCA method was not appreciably different from the approach specified by the NHSDA research team for identifying DSM cocaine dependence (ie adding up the clinical features within a simple algorithmic index). This evidence suggests that the standard assigned cutoff of three clinical features might be serving well to sort out cocaine dependent individuals among recent-onset cocaine users. However, the latent class model provided useful information to aid our understanding of the cocaine dependence syndrome. First, the 3C model identified what might be a prodromal class of recent-onset users (estimated prevalence 16%) with at least several clinical features of cocaine dependence. The most notable clinical features experienced by this subgroup were spending a lot of time getting or using cocaine, using cocaine much more often or in larger amounts than intended and difficulty cutting down. Not surprisingly, this class of recent-onset users has yet to build up a subjectively-felt tolerance to cocaine or to have it interfere with their lives emotionally, physically or socially. With greater understanding of this type of progression of clinical features of cocaine dependence soon after onset of cocaine use, we may become able to provide useful information for the design of appropriate interventions among recent-onset cocaine users prior to the emergence of full-blown dependence. Second, the latent class structure under the 4C model exhibited differences of qualitative content in addition to severity gradations or levels of dependence. Classes 3 and 4 were both associated with a high probability of meeting DSM criteria for cocaine dependence, as ascertained by the standard NHSDA approach. However, the patterns of clinical features observed in these two classes were qualitatively different. Both subgroups of recent-onset cocaine users had relatively high and equal probabilities of reporting subjectively felt tolerance, spending a lot of time getting or using cocaine, using cocaine much more often or in larger amounts than intended and difficulty cutting down. It is notable that these are the same clinical features highlighted in the prodromal class under the 3C model possibly providing support for the idea that these features appear first in the course of drug dependence. Class 4, however, is distinguished by its high probabilities of reporting narrowing of the nondrug behaviour repertoire, emotional problems and health problems. This may reflect a subtype of dependence with its own prognostic outcome or it may represent a progression in dependence of a qualitative nature. In the absence of longitudinal data, however, we are unable to make this distinction.
The study findings also included results from exploratory analyses regarding variation in reporting of individual clinical features as well as variation in risk of LCA-derived cocaine dependence by subgroup characteristics. We refer to these analyses as exploratory due to the small numbers of cocaine users sorted by LCA into the cocaine dependence classes for both the 3C- and 4C models. In consequence, the information value of this study's assessment of variation in the risk of dependence based on subgroup characteristics was constrained as seen in wider confidence intervals.
The most common clinical features emerging soon after onset of cocaine use were trouble cutting down or cutting back on cocaine use, difficulty controlling cocaine use, and salience of cocaine use within the behavioural repertoire of users; emotional problems attributed to cocaine also were prominent. Results from both the three- and 4C models suggest that males are less likely to become dependent upon cocaine within 24 months of first use although the results did not reach statistical significance. These results are consistent with some recent research. Chen and Kandel (2002) studied prevalent cocaine dependence cases within the 1991–1993 NHSDA samples and found that females were twice as likely as male subjects to be active cases of cocaine dependence (OR=1.67; 95% CI=1.1, 2.6). Chen and Anthony (2004) and O'Brien and Anthony (2005) identified recent-onset cocaine users from within the 1998 NHSDA sample and 2000–2001 NHSDA sample, respectively, and found that female recent-onset users were more likely than males to have developed clinical features of cocaine dependence soon after onset of cocaine use. These convergent findings, however, are all based on the same survey instrument (NHSDA) and it is possible that male cocaine users provide less complete or less accurate autobiographies of cocaine problems and dependence-related experiences, as compared to female cocaine users. Nonetheless, these epidemiological findings are consistent with some preclinical data that have found neural as well as hormonal differences in rats (Hu et al, 2004) and rhesus monkeys (Mello et al, 2004) that might account for sex differences in the regulation of cocaine acquisition.
With respect to race-ethnicity, self-designated members of racial-ethnic minority groups were found to be more likely to experience narrowing of their nondrug behavioural repertoire and failed efforts to cut down on cocaine use. Although members of these subgroups had an excess risk of becoming cocaine dependent soon after onset of cocaine use compared to non-Hispanic Whites, the CI for these estimates are quite wide due to a relatively small number of minorities (n=69) among recent-onset cocaine users; these differences are not statistically significant by conventional standards. Nonetheless, the direction of this result is supported by evidence reported by O'Brien and Anthony (2005), who had a similarly small number of minority recent-onset cocaine users.
As might be expected from prior research relating earlier drug use to later drug involvement (Breslau et al, 1993; Ellickson et al, 2001; Kandel, 1982; Kandel and Davies, 1992; Robins and Przybeck, 1985), those starting to use cocaine at age 21–29 years were less likely to become dependent on cocaine compared to those who started using cocaine at age 11–14 years. The reasons for this difference by age of onset still are not known with any certainty. Finally, as might be expected based on findings from other analyses of NHSDA data (O'Brien and Anthony, 2005; Chen and Kandel, 2002) including a recent analysis of the 1995–1998 NHSDA (Chen and Anthony, 2004), there was an excess risk of becoming dependent on cocaine among recent-onset users who had started to smoke crack-cocaine as compared to those who had not smoked crack.
Several limitations should be noted, including limitations inherent in the NHSDA methodological approach, its community-residence sampling frame,and levels of respondent non-participation, as well as its survey methods in general (eg see Chen and Anthony, 2004; O'Brien and Anthony, 2005). In particular, the survey design requires looking backwards to identify recent-onset users and to characterize them in relation to just-experienced and just-reported clinical features of cocaine dependence. These cross-sectional snapshots of cocaine users, taken within the first 24 months after onset of cocaine use, do not have the power to resolve important open questions about the stability and generalization of the classes. Future research might yield a different set of findings with respect to a more extensive array of clinical features of cocaine dependence assessed in other samples.
We also can return to an issue mentioned in our methods section. Namely, the current investigation requires an assumption that cocaine dependence develops insidiously, over time, and has a relatively chronic course with persistence over a span of weeks and months as opposed to an acute onset and short-term course of the type seen in ‘rapid onset, rapid offset’ conditions (eg the ‘common cold’). If there is a form of cocaine dependence that has the ‘rapid onset, rapid offset’ form, then this investigation's research approach might be under-estimating the risk of cocaine dependence within 24 months after onset of cocaine use.
The value of this study's estimates on risk of cocaine dependence soon after onset of cocaine use has been outlined in a recent article by O'Brien and Anthony (2005). Within the collection of prior studies on cocaine dependence, most have not had the benefit of a nationally representative sample of recent-onset cocaine users; most studies focus upon cocaine users seeking treatment or prevalent cocaine users; most of these users had started cocaine use many years before they entered the study sample. The present study has attempted to shed light on recent-onset cocaine users, in an approximation of estimates that might be obtained via properly conducted prospective studies with nationally representative samples. As such, the research may set the stage for future and more probing research on the nature and form of cocaine dependence syndromes that emerge soon after onset of cocaine use and the topic of which cocaine users might be at excess risk of becoming cocaine dependent soon after onset of cocaine use.
References
Anthony JC, Petronis KR (1989). Cocaine and heroin dependence compared: evidence from an Epidemiologic Field Survey. Am J Public Health 79: 1409–1410.
Anthony JC, Warner LA, Kessler RC (1994). Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol 2: 244–268.
Bandeen-Roche K, Huang GH, Munoz B, Rubin GS (1999). Determination of risk factor associations with questionnaire outcomes: a methods case study. Am J Epidemiology 150: 1165–1178.
Bansfield JD, Raftery AE (1993). Model-based Gaussian and non-Gaussian clustering. Biometrics 49: 803–821.
Breslau N, Fenn N, Peterson EL (1993). Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Dependence 33: 129–138.
Carroll KM, Rounsaville BJ (1992). Contrast of treatment-seeking and untreated cocaine abusers. Arch Gen Psychiatry 49: 464–471.
Chen CY, Anthony JC (2004). Epidemiological estimate of risk to become dependent upon cocaine: cocaine hydrochloride powder vs crack cocaine. Psychopharmacology 172: 78–86.
Chen K, Kandel D (2002). Relationship between extent of cocaine use and dependence among adolescents and adults in the United States. Drug Alcohol Dependence 68: 65–85.
Clogg CC (1995). Latent class models. In: Arminger G, Clogg C, Sobel ME (eds). Handbook of Statistical Modeling for the Behavioral and Social Sciences. Plenum Publishing Corporation: New York, NY. pp 311–359.
Dennis ML, Scott CK, Funk R, Foss MA (2005). The duration and correlates of addiction and treatment careers. J Substance Abuse Treatment 28 (Suppl 1): S51–S62.
Ellickson PL, Tucker JS, Klein DJ (2001). High-risk behaviors associated with early smoking: results from a 5-year follow-up. J Adolescent Health 28: 465–473.
Hagenaars JA, McCutcheon AL (eds) (2002). Applied Latent Class Analysis. Cambridge University Press: Cambridge United Kingdom.
Hu M, Crombag HS, Robinson TE, Becker JB (2004). Biological basis of sex differences in the propensity to self-administer cocaine. Neuropsychopharmacology 29: 81–85.
Kandel DB (1982). Epidemiological and psychosocial perspectives on adolescent drug use. J Am Acad Child Adolescent Psychiatry 21: 328–347.
Kandel DB, Davies M (1992). Progression to regular marijuana involvement: phenomenology and risk factors for near-daily use. In: Glantz M, Pickens R (eds). Vulnerability to Drug Abuse. American Psychological Association: Washington, DC. pp 211–254.
Lazarsfeld PF, Henry NW (1968). Latent Structure Analysis. Hougton Mifflin: Boston.
Lin TS, Dayton CM (1997). Model-selection information criteria for non-nested latent class models. J Edu Behav Statist 22: 249–264.
Magidson J, Vermunt JK (2000). Latent class cluster analysis. In: Hagenaars JA, McCutcheon AL (eds). Applied latent class analysis. Cambridge University Press: Cambridge.
McCutcheon AL (1987). Latent Class Analysis. (Sage university paper series on quantitative applications in the social sciences, no 07–064). Sage Publications: Newberry Park, CA.
McLachlan GJ, Peel D (2000). Finite Mixture Models. John Wiley: New York.
Mello NK, Mendelson JH, Negus SS, Kelly M, Knudson I, Roth ME (2004). The effects of cocaine on gonadal steroid hormones and LH in male and female rhesus monkeys. Neuropsychopharmacology 29: 2024–2034.
Nader MA (1998). The influence of behavioral and pharmacological history on the reinforcing effects of cocaine in rhesus monkeys. NIDA Res Monograph 169: 26–55.
O'Brien MS, Anthony JC (2005). Risk of becoming cocaine dependent: epidemiological estimates for the United States, 2000–2001. Neuropsychopharmacology 30: 1006–1018.
Pottieger AE, Tressell PA, Surratt HL, Inciardi JA, Chitwood DD (1995). Drug use patterns of adult crack users in street versus residential treatment samples. J Psychoactive Drugs 27: 27–38.
Robins LN, Przybeck TR (1985). Age at onset of drug use as a factor in drug and other disorders. In: Implications for Prevention (NIDA Research Monograph 56). US Government Printing Office: Washington, DC. pp 178–192.
STATA Corp (2000). STATA Statistical Software Release 7.0 Reference Manual. STATA Press: Texas.
Substance Abuse and Mental Health Services Administration (1997). National Household Survey on Drug Abuse: Public Release Codebook, 1995. US Department of Health and Human Services: Rockville, MD.
Substance Abuse and Mental Health Services Administration (1998). National Household Survey on Drug Abuse: Public Release Codebook, 1996. US Department of Health and Human Services: Rockville, MD.
Substance Abuse and Mental Health Services Administration (1999). National Household Survey on Drug Abuse: Public Release Codebook, 1997. US Department of Health and Human Services: Rockville, MD.
Substance Abuse and Mental Health Services Administration (2000). National Household Survey on Drug Abuse: Public Release Codebook, 1998. US Department of Health and Human Services: Rockville, MD.
Vermunt JK, Magidson J (2003). Latent Gold 3.0 User's Guide. Statistical Innovations Inc.: Belmont, MA.
Wagner FA, Anthony JC (2002). From first drug use to drug dependence; developmental periods of risk for dependence upon marijuana, cocaine and alcohol. Neuropsychopharmacology 26: 479–488.
Acknowledgements
The authors wish to acknowledge the project's funding sources: NIDA awards K01DA016279, R01DA09897, R01DA04392 and its ‘Transitions’ supplement, and K05DA015799. In addition, data reported herein come from national survey data collected under the auspices of the Office of Applied Studies at the US Substance Abuse Mental Health Services Administration. We thank OAS and SAMHSA for completing these studies, commissioning the creation of the public use data files, and making them available in a timely fashion.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reboussin, B., Anthony, J. Is there Epidemiological Evidence to Support the Idea that a Cocaine Dependence Syndrome Emerges Soon after Onset of Cocaine Use?. Neuropsychopharmacol 31, 2055–2064 (2006). https://doi.org/10.1038/sj.npp.1301037
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301037
Keywords
This article is cited by
-
Transitioning from First Drug Use to Dependence Onset: Illustration of a Multiparametric Approach for Comparative Epidemiology
Neuropsychopharmacology (2016)
-
Compulsive Overeating as an Addictive Behavior: Overlap Between Food Addiction and Binge Eating Disorder
Current Obesity Reports (2013)
-
Influence of abstinence and intervals between extinction trials on the expression of cocaine-conditioned place preference in adolescent rats
Psychopharmacology (2013)
-
Effects of self-administered cocaine in adolescent and adult male rats on orbitofrontal cortex-related neurocognitive functioning
Psychopharmacology (2009)
-
Differential effects of self-administered cocaine in adolescent and adult rats on stimulus–reward learning
Psychopharmacology (2007)