Abstract
Background:
Advanced prostate cancer is a phenotypically diverse disease that evolves through multiple clinical courses. PSA level is the most widely used parameter for disease monitoring, but it has well-recognized limitations. Unlike in clinical trials, in practice, clinicians may rely on PSA monitoring alone to determine disease status on therapy. This approach has not been adequately tested.
Methods:
Chemotherapy-naive asymptomatic or mildly symptomatic men (n=872) with metastatic castration-resistant prostate cancer (mCRPC) who were treated with the androgen receptor inhibitor enzalutamide in the PREVAIL study were analyzed post hoc for rising versus nonrising PSA (empirically defined as >1.05 vs ⩽1.05 times the PSA level from 3 months earlier) at the time of radiographic progression. Clinical characteristics and disease outcomes were compared between the rising and nonrising PSA groups.
Results:
Of 265 PREVAIL patients with radiographic progression and evaluable PSA levels on the enzalutamide arm, nearly one-quarter had a nonrising PSA. Median progression-free survival in this cohort was 8.3 months versus 11.1 months in the rising PSA cohort (hazard ratio 1.68; 95% confidence interval 1.26–2.23); overall survival was similar between the two groups, although less than half of patients in either group were still at risk at 24 months. Baseline clinical characteristics of the two groups were similar.
Conclusions:
Non-rising PSA at radiographic progression is a common phenomenon in mCRPC patients treated with enzalutamide. As restaging in advanced prostate cancer patients is often guided by increases in PSA levels, our results demonstrate that disease progression on enzalutamide can occur without rising PSA levels. Therefore, a disease monitoring strategy that includes imaging not entirely reliant on serial serum PSA measurement may more accurately identify disease progression.
Similar content being viewed by others
Introduction
Serial PSA testing is standard practice when monitoring prostate cancer. As a direct, downstream target gene of the androgen receptor (AR), PSA production and secretion into the circulation generally denotes AR-driven cellular proliferation. On the other hand, the lack of PSA production in the setting of advanced metastatic castration-resistant prostate cancer (mCRPC) is typically interpreted to indicate dedifferentiation of AR-driven prostate cancer into a more anaplastic or small-cell phenotype.1, 2 These features fit into an evolving framework wherein prostate cancer is thought to evolve from endocrine-dependent disease driven by testis-derived androgen production, to intracrine-dependent disease with intratumoral androgen production, to ligand-independent but still AR-dependent disease and, finally, to AR-independent disease.3 Whether these stages evolve over time or co-exist early in the disease course, as suggested by recent autopsy data,4 is not yet clear.
PREVAIL is the largest treatment study ever conducted in men with chemotherapy-naive mCRPC. 5 PREVAIL randomized 1717 men to enzalutamide or placebo, with coprimary end points of radiographic progression-free survival (rPFS) and overall survival (OS). In the primary analysis, enzalutamide significantly improved rPFS and OS relative to placebo in men with asymptomatic or minimally symptomatic mCRPC.5 Patients were monitored with frequent laboratory tests, including PSA level, complete blood count, comprehensive metabolic panel and regular imaging, which included bone scan and computed tomography or magnetic resonance imaging of the chest, abdomen and pelvis every 8 weeks during the first 6 months then every 12 weeks thereafter.
Conversely, in routine clinical practice, imaging is not consistently obtained with the same frequency as was performed in PREVAIL. Many practitioners rely on PSA and physical examination as the principal measure of response and progression, and imaging is often reserved for the evaluation of symptoms or at the time of PSA progression. However, this practice has not been validated and could result in delayed detection of disease progression if disease progression occurs without a rise in PSA.
In this post hoc analysis of enzalutamide-treated PREVAIL participants, we evaluated baseline characteristics and primary treatment outcomes in patients with radiographic progression in the presence or absence of a concomitant increase in PSA.
Materials and methods
The PREVAIL study design and methodology have been published.5 In brief, the study enrolled men with mCRPC who were asymptomatic or minimally symptomatic, had an Eastern Cooperative Oncology Group Performance Status of 0 or 1 and had not received prior chemotherapy. Patients were randomized 1:1 to receive 160 mg oral enzalutamide or placebo once daily and continued to receive one of these treatments until intolerance or confirmed radiographic disease progression or initiation of another therapy for prostate cancer. Patients were required to continue androgen deprivation therapy while treated in the study.5
Assessment of PSA, ALP and LDH
Blood samples for PSA determination were collected at screening, at baseline immediately before the first dose of study drug, at weeks 13, 17, 21 and 25, and every 12 weeks thereafter. Serum levels of alkaline phosphatase (ALP) and lactate dehydrogenase (LDH) were determined at baseline, at weeks 1, 5, 13 and 25, and every 12 weeks thereafter.
Assessment of radiographic progression
Radiographic disease in soft tissue was evaluated using either computed tomography or magnetic resonance imaging and in bone using technetium bone scintigraphy. Imaging was performed at screening, at weeks 9, 17 and 25, and every 12 weeks thereafter.5 Radiographic progression was determined by independent central radiology review and separately by investigators using Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST) for soft tissue or criteria adapted from the Prostate Cancer Clinical Trials Working Group 2 (PCWG2) for osseous disease.6, 7, 8 Radiographic disease progression in bone (⩾2 new lesions on radionuclide bone scan) observed at week 9 required two additional new lesions on a confirmatory scan ⩾6 weeks later; radiographic disease progression in bone observed after week 9 required persistence of two new lesions on a confirmatory scan ⩾6 weeks later. Radiographic disease progression in soft tissue did not require a confirmatory scan for purposes of analysis.
Analysis populations and end points
Our post hoc analyses were conducted only in patients randomized to enzalutamide in PREVAIL. The coprimary end points of rPFS and OS were evaluated in two subgroups: (1) patients who met the dual conditions of radiographic progression and a PSA level at the time of radiographic progression that was ⩽1.05 times the PSA level from 3 months earlier (‘nonrising PSA group’); and (2) patients whose PSA taken just before or at the time of radiographic progression was >1.05 times the PSA level from 3 months earlier (‘rising PSA group’). The value of 1.05 was chosen conservatively to limit the analysis to patients whose PSA rise was deemed nonsignificant in clinical terms and to create clear separation from the PCWG2 definition of PSA progression (PSA rise of 25%).
Statistical analysis
For our analyses, rPFS was defined as the time from randomization to the first objective evidence of radiographic disease progression as assessed by the investigator, using the same cutoff date as the OS analyses (September 16, 2013). This methodology differs from the primary analysis of rPFS in PREVAIL, which was event-driven and based on independent central review, using a cutoff of 6 May 2012.5 Investigator-assessed radiographic progression was selected because of the longer follow-up period. Analyzing the cohorts at the later cutoff allowed for a greater number of events and was deemed to be acceptable given the 90.9% concordance between investigator and independent review previously reported.9
For both rPFS and OS, estimates of the median and 95% confidence intervals (CIs) were determined using the Kaplan–Meier method. Hazard ratios were determined using an unstratified Cox regression model (with the nonrising PSA group as the only covariate) and was relative to rising PSA, with a value less than unity favoring nonrising PSA.
We also determined the change from baseline and change at progression from 3 months earlier in serum levels of ALP and LDH.
Code availability
Computer code used to generate the results of the time-to-event analyses is provided in the online supplement.
Results
Of 872 patients randomized to receive enzalutamide, 65 (7.5%) had a nonrising PSA and 200 (22.9%) had a rising PSA at the time of radiographic progression (excluding death) based on investigators’ assessments as of the 16 September 2013, data cutoff. LDH showed little change in either group, with a mean change from 3 months earlier of 4.31% (95% CI 0.48–8.15) in the rising PSA group and −0.6% (95% CI −4.29–3.06) in the nonrising PSA group. On the other hand, ALP was rising at the time of radiographic progression in both groups; compared with 3 months earlier, mean ALP had increased by 14.45% (95% CI 10.55–18.35) in the rising PSA group and 4.98% (95% CI 0.72–9.24) in the nonrising PSA group.
Median time on treatment was 8.3 months (interquartile range (IQR) 5.6–11.2) in the nonrising PSA group and 11.1 months (IQR 8.3–16.4) in the rising PSA group.
Baseline characteristics
Baseline patient and disease characteristics were generally similar between the nonrising PSA and rising PSA groups with respect to demographics and prognostic characteristics, including age, performance status, baseline pain, baseline laboratory values, Gleason score (median and proportion of patients with a Gleason score ⩾8 at initial diagnosis) and prior therapies (Table 1).10, 11, 12 The proportion of patients with a rising PSA at study entry was 92.3% in the nonrising PSA group and 78.0% in the rising PSA group. The proportion of patients with bone disease in the nonrising PSA and rising PSA groups was similar (87.7% vs 80.5%, respectively), although the proportion of patients with bone-only disease was slightly lower in the nonrising PSA group (24.6% vs 30.5%). The proportion of patients in the nonrising PSA group and rising PSA group with soft tissue disease was 75.4% and 68.5%, respectively, which included visceral disease (liver and/or lung, 16.9% and 10.5%) and non-liver/lung visceral metastases (primarily affecting the renal and urologic system, 23.1% and 17.5%; represented as other soft-tissue disease in Table 1).
As noted above, the overall rate of PSA discordance (radiographic progression without PSA progression) was 24.5% (65/265). By site of baseline disease, the rate of discordance was 20.8% (16/77) in patients with bone-only disease, 34.4% (11/32) in patients with lung or liver metastases and 30.0% (15/50) in patients with non-liver/lung visceral metastases (Table 1).
Clinical outcomes
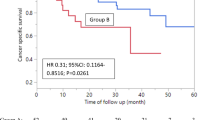
Investigator-assessed median PFS was 8.3 months (95% CI 8.0–10.3) in the nonrising PSA group and 11.1 months (95% CI 11.0–13.4) in the rising PSA group (hazards ratio 1.68; 95% CI 1.26–2.23) (Figure 1). There was no differential pattern of radiographic progression in the nonrising or rising PSA groups, with a preponderance of soft-tissue progression over bone-only progression (Table 2). Ninety-five patients had bone-only progression at the time of progression on enzalutamide, whereas 164 patients had soft-tissue-only progression and six had both soft-tissue and bone progression. Notably, in patients who had bone-only disease at study entry, 40.3% (31/77) developed soft-tissue disease at progression.
We queried the best radiographic response in all patients with measurable disease (46 and 106 in the nonrising PSA and rising PSA groups, respectively). Complete or partial radiographic responses in measurable disease occurred in 63.0% of patients in the nonrising PSA group and 67.0% in the rising PSA group (Supplementary Table S1). Complete response rates were lower in the nonrising PSA group than in the rising PSA group (8.7% vs 18.9%). Although median PSA levels at the time of study entry were higher in the nonrising PSA group than in the rising PSA group (82.2 ng ml−1 vs 61.3 ng ml−1), this was not so at the time of radiographic progression (5.5 ng ml−1 vs 23.0 ng ml−1). Thus, patients with radiographic progression in the nonrising PSA group had greater change from-baseline-to-progression reductions in PSA levels than those in the rising PSA group (89.8% vs 50.1%; Supplementary Table S2).
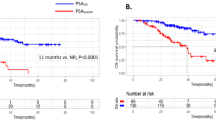
Overall survival was similar between the two groups (not yet reached vs 32.4 months; hazards ratio 0.68; 95% CI 0.37–1.26) (Figure 2); however, fewer than half of the patients in either group were still at risk at 24 months. The use of subsequent therapies with a known survival benefit in prostate cancer was 46.2% in the nonrising PSA group and 58.0% in the rising PSA group (Table 3).
Discussion
Radiographic progression with a stable or falling serum PSA level is surprisingly common in patients treated with enzalutamide. Although this phenomenon is recognized anecdotally, no formal analysis has been previously reported from a prospective, randomized trial. The nearly one-quarter of patients who progressed on enzalutamide without any PSA progression was a much larger proportion than expected. In fact, almost one-third of men with visceral metastases had discordance between the PSA and radiographic findings. It was also surprising that the median PSA level of this population at study entry was equal to that of patients with radiographic progression and a rising PSA. Indeed, there were no baseline clinical characteristics that would predict for discordance between PSA and radiographic findings. The limited number of patients in this retrospective analysis restricts our capacity to identify statistically significant differences between the groups. The slight preponderance toward baseline visceral disease was anticipated, but the magnitude of the difference was inadequate to vary surveillance recommendations based on visceral disease burden.
Our results also affirm the role of total ALP as a marker of progression in patients with bone metastases. Even in the absence of PSA progression, a rise in ALP occurred at the time of radiographic progression. That the mean change was greater in the rising than nonrising PSA group is likely more of a point of interest than it is clinically important. The value of LDH appears less clear. Although there is a modest change in LDH in the rising PSA group, it is unchanged in the nonrising PSA group and in general is clinically nonspecific. Given the normal fluctuations in LDH, it is hard to cite a <5% rise in LDH as an indicator of progression.
In designing this analysis, we chose a definition of nonrising PSA (a level at progression ⩽1.05 times greater than that from 3 months before radiographic progression). Although arguments could be made for some variation of this definition, our data set was not sufficiently powered to allow multiple subset analyses using varying PSA levels. Given that PCWG2 criterion for rising PSA is an arbitrary 25% increase over nadir, we felt it necessary to create a wide boundary between the PCWG2 cutoff and the cutoff for our study group to eliminate scenarios in which a PSA rise just short of 25% was included in our study group.
The inferior PFS and OS detected in our analysis for patients with radiographic progression and nonrising PSA levels may signify a more aggressive clinical phenotype. The inferior PFS in the PSA discordant groups (8.3 vs 11.1 months) was markedly shorter than the PFS in the entire enzalutamide-treated cohort in PREVAIL (20.0 months).9 In part this is a consequence of our cohorts being limited to patients who developed radiographic progression by the time of the data cutoff, thus excluding patients who were still responding at that time. As a result, the cohorts described herein represent early progression with or without a rising PSA. At the time of the final PREVAIL datalock, 61% of enzalutamide-treated patients had not developed radiographic progression. Similarly, the OS for the rising PSA cohort in our analysis was only 32.4 months. In the final PREVAIL analysis, median OS was 35.3 months in enzalutamide-treated patients and 31.3 months in placebo-treated patients.13 That most patients in both of our cohorts were no longer at risk for death by 24 months means that survival estimates nearly a year later were unstable and likely to change with longer follow-up. Indeed, the OS curves are largely overlapping with a majority of patients at risk, and they only separate once less than one-quarter of the patients in each group remain. Figure 2 illustrates that the proportion of patients in the nonrising PSA group decreases over the timeline covered in this analysis, although it is unknown whether that trend would continue with ongoing follow-up. It may be that the phenomenon of nonrising PSA is most common in the first 18 months on enzalutamide.
The lack of PSA progression may indicate that these tumors have become less reliant on the AR for their growth and may indicate the need for chemotherapy or treatment using non-AR targeting strategies. Genomic overlap between castration-resistant tumors characterized histologically as prostate adenocarcinomas and neuroendocrine prostate cancer has been detected by whole-exome sequencing data of metastatic biopsies from a wide range of anatomical sites.14 Analysis of serial biopsy samples from the same patients revealed divergent evolution of neuroendocrine prostate cancer from one or more prostate adenocarcinomas, an adaptive process that promotes emergence of an alternative, ‘AR-indifferent’ cell state as a treatment-resistance mechanism in advanced prostate cancer.14 In addition, the West Coast Prostate Cancer Dream Team identified a new histologic subset of mCRPC termed ‘intermediate atypical carcinoma', which shares many features with neuroendocrine prostate cancer and was detected in CRPC patients exhibiting resistance to the AR-signaling inhibitors enzalutamide and abiraterone acetate.15, 16 Whether the histologic patterns reported by those investigators are related to the clinical picture of a stable PSA with imaging progression described in our analysis is not known. An ongoing study of enzalutamide in the same population as PREVAIL (patients with chemotherapy-naive mCRPC) incorporates biopsies at baseline and progression (NCT02099864). The histology from these biopsies should indicate whether the intermediate atypical carcinoma phenotype is present in those with stable PSA and progression on imaging studies.
The role of imaging in monitoring patients with mCRPC is another question for which these results may be impactful. Some clinicians monitor mCRPC with PSA alone, even though a European Consensus Panel recommended early imaging in patients receiving AR-pathway inhibitors independently of PSA response because of the discordance between PSA levels and radiographic progression.17 The panel specifically cited the need to identify early resistance and the shortcoming of PSA as a reliable marker of progression.17 Based on our results, avoidance of imaging might miss early disease progression. However, we do not know if the pattern of PSA stability continues until symptoms develop, or if the PSA eventually begins to rise as the disease progresses.
The development of soft-tissue metastases in patients who start therapy with bone-only disease represents another reminder that comprehensive imaging may be necessary to fully monitor disease status in advanced prostate cancer. Our finding that over 40% of patients who start with bone-only disease go on to develop soft tissue disease at progression is novel and, to our knowledge, has not been reported before. This finding may have implications for treatment selection and sequencing given the availability of bone directed radiopharmaceuticals such as radium-223 dichloride.
It is difficult to know if patients are harmed by delayed detection of disease progression. Whether health-related quality of life and pain were indicative of progression with nonrising PSA progression was not answerable in our data set because of a lack of data. Regardless, the utility of early detection of progression depends on the ability to act upon that information in a way that benefits patients. As more effective treatments become available for patients with advanced prostate cancer, it may be increasingly important to detect treatment failure promptly so that opportunities to receive life-prolonging therapy are not lost. Further, as we gain insights into the distinct drivers of enzalutamide-resistant mCRPC, identifying progression earlier may lead to targeted treatments for specific emergent resistant mechanisms. In prostate cancer, early institution of effective agents has been well supported by the CHAARTED and STAMPEDE studies of early docetaxel in hormone-sensitive metastatic disease.18, 19, 20 In the randomized, double-blind ALSYMPCA study of radium-223 in mCRPC, patients on active therapy benefited from a higher quality of life than patients receiving placebo,21 thus illustrating that effective treatment of disease is the most effective way to prevent the morbidity of cancer progression.
To the best of our knowledge, this paper represents the first systematic description of patients with nonrising PSA at radiographic progression on AR-directed therapy. This population may represent a divergent phenotype of disease requiring a different treatment approach for patients with rising PSA, such as chemotherapy or biopsies to better define the pathology. Ongoing studies to define biomarkers of aggressiveness and tumor evolution may help identify baseline characteristics of this cohort and/or mechanistic differences underlying PSA discordance with progression. Future clinical trials should report on PSA discordant progression to better characterize this population.
References
Aparicio AM, Harzstark AL, Corn PG, Wen S, Araujo JC, Tu SM et al. Platinum-based chemotherapy for variant castrate-resistant prostate cancer. Clin Cancer Res 2013; 19: 3621–3630.
Beltran H, Tomlins S, Aparicio A, Arora V, Rickman D, Ayala G et al. Aggressive variants of castration-resistant prostate cancer. Clin Cancer Res 2014; 20: 2846–2850.
Nelson PS . Molecular states underlying androgen receptor activation: a framework for therapeutics targeting androgen signaling in prostate cancer. J Clin Oncol 2012; 30: 644–646.
Gundem G, Van Loo P, Kremeyer B, Alexandrov LB, Tubio JM, Papaemmanuil E et al. The evolutionary history of lethal metastatic prostate cancer. Nature 2015; 520: 353–357.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014; 371: 424–433.
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA et al. Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the Prostate Cancer Clinical Trials Working Group. J Clin Oncol 2008; 26: 1148–1159.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 2000; 92: 205–216.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009; 45: 228–247.
Morris MJ, Loriot Y, Beer TM, Higano CS, Armstrong AJ, Sternberg CN et al. Sensitivity analyses for radiographic progression-free survival (rPFS): results from the phase 3 PREVAIL trial comparing enzalutamide to placebo [abstract 5054]. J Clin Oncol 2014; 32.
Armstrong AJ, Garrett-Mayer ES, Yang YC, de Wit R, Tannock IF, Eisenberger M . A contemporary prognostic nomogram for men with hormone-refractory metastatic prostate cancer: a TAX327 study analysis. Clin Cancer Res 2007; 13: 6396–6403.
Halabi S, Small EJ, Kantoff PW, Kattan MW, Kaplan EB, Dawson NA et al. Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol 2003; 21: 1232–1237.
Smaletz O, Scher HI, Small EJ, Verbel DA, McMillan A, Regan K et al. Nomogram for overall survival of patients with progressive metastatic prostate cancer after castration. J Clin Oncol 2002; 20: 3972–3982.
Beer TM, Armstrong AJ, Sternberg CN, Higano CS, Rathkopf DE, Loriot Y et al. Enzalutamide (ENZA) in men with chemotherapy-naive metastatic castration-resistant prostate cancer (mCRPC): final analysis of the phase 3 PREVAIL study [abstract 5036]. J Clin Oncol 2015; 33.
Beltran H, Prandi D, Mosquera JM, Benelli M, Puca L, Cyrta J et al. Divergent clonal evolution of castration-resistant neuroendocrine prostate cancer. Nat Med 2016; 22: 298–305.
Small EJ, Huang J, Youngren J, Sokolov A, Aggarwal RR, Thomas GV et al. Characterization of neuroendocrine prostate cancer (NEPC) in patients with metastatic castration resistant prostate cancer (mCRPC) resistant to abiraterone (Abi) or enzalutamide (Enz): preliminary results from the SU2C/PCF/AACR West Coast Prostate Cancer Dream Team (WCDT) [abstract 5003]. J Clin Oncol 2015; 33.
Small EJ, Aggarwal RR, Huang J, Sokolov A, Zhang L, Alumkal JJ et al. Clinical and genomic characterization of metastatic small cell/neuroendocrine prostate cancer (SCNC) and intermediate atypical prostate cancer (IAC): results from the SU2C/PCF/AACRWest Coast Prostate Cancer Dream Team (WCDT) [abstract 5019]. Presented at the 2016 American Society of Clinical Oncology Annual Meeting; 3–7 June, 2016: Chicago, IL, USA.
Fitzpatrick JM, Bellmunt J, Fizazi K, Heidenreich A, Sternberg CN, Tombal B et al. Optimal management of metastatic castration-resistant prostate cancer: highlights from a European Expert Consensus Panel. Eur J Cancer 2014; 50: 1617–1627.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 2016; 387: 1163–1177.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med 2015; 373: 737–746.
Vale CL, Burdett S, Rydzewska LH, Albiges L, Clarke NW, Fisher D et al. Addition of docetaxel or bisphosphonates to standard of care in men with localised or metastatic, hormone-sensitive prostate cancer: a systematic review and meta-analyses of aggregate data. Lancet Oncol 2016; 17: 243–256.
Hoskin P, Sartor O, O'Sullivan JM, Johannessen DC, Helle SI, Logue J et al. Efficacy and safety of radium-223 dichloride in patients with castration-resistant prostate cancer and symptomatic bone metastases, with or without previous docetaxel use: a prespecified subgroup analysis from the randomised, double-blind, phase 3 ALSYMPCA trial. Lancet Oncol 2014; 15: 1397–1406.
Acknowledgements
The study sponsors, Medivation (acquired by Pfizer, in September 2016) and Astellas Pharma, contributed to the design of the study, reviewed the manuscript, and provided comments to the authors. Medical writing and editorial support was provided Timothy Lohret, PhD, Malcolm Darkes, PhD and Shannon Davis of Ashfield Healthcare Communications, which was funded by the study sponsors. This study was supported by Medivation (acquired by Pfizer in September 2016) and Astellas Pharma, the co-developers of enzalutamide. Trial registration: PREVAIL ClinicalTrials.gov number, NCT01212991.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AHB has nothing to disclose. JJA’s institution has received research funding from Aragon Pharmaceuticals, Astellas Pharma, AstraZeneca, Bristol-Myers Squibb, ImClone Systems, Millennium and Novartis. JJA has received income for consulting with Astellas Pharma and for educational sessions with Bayer HealthCare Pharmaceuticals. AA is an advisor for Astellas, Bayer, Dendreon, Janssen, Medivation and Sanofi; he has received honoraria from Dendreon and Sanofi; he is on a speakers bureau for Dendreon; his institution has received research funding from Active Biotech, Astellas, Bayer, Dendreon, Janssen, Medivation, Novartis, Pfizer and Sanofi; he has received travel expenses from Dendreon, Janssen and Medivation; and he has a patent pending that involves his institution and Janssen for technology relating to oncology. CSH is an advisor for AbbVie, Bayer, BHR Pharma, Dendreon, Emergent BioSolutions, Ferring, Genentech, Medivation, Orion Corporation, Pfizer and Sanofi; her institution has received research funding from Algeta/Bayer, Aragon Pharmaceuticals, AstraZeneca, Dendreon, Emergent BioSolutions, Exelixis, Genentech, Medivation, Millennium, OncoGenex, Sanofi and Teva; and she has received travel expenses from AbbVie, Amgen, Astellas Pharma, Bayer, Dendreon, Emergent BioSolutions, Ferring, Genentech, Johnson & Johnson, Medivation, Ockham, Orion Pharma, Pfizer, Sanofi and Teva. PI is an advisor for Astellas, Ferring, Janssen and Medivation, and has received research funding from Astellas, Bavarian Nordic and Medivation. CNS has received institutional research funding or honoraria from Astellas, Bayer, Cougar Biotechnology (now Janssen Oncology), Medivation and Sanofi. DR has received research funding from Celgene, Ferring, Janssen, Medivation, Millenium and Novartis. YL is an advisor for Astellas, Bristol-Myers Squibb, Ipsen, Janssen, Roche and Sanofi; his institution has received research funding from Sanofi; and he has received travel expenses from Astellas, Bristol-Myers Squibb and Sanofi. JD has received honoraria from, is an advisor for, and is on a speakers bureau for Astellas. BT has received research funding from Astellas, Ferring and Sanofi, and honoraria from Astellas, Bayer, Ferring, Medivation and Sanofi. SA was an employee of Medivation at the time of study conduct. PL is an employee of Medivation. AK is an employee of Astellas. DP is an employee of Astellas. TMB has stock and other ownership interests in Salarius Pharmaceuticals; he is an advisor for Astellas, AstraZeneca, Bayer, Churchill Pharmaceuticals, Dendreon, Janssen Japan, Novartis and F Hoffmann-La Roche; and his institution has received research funding from Astellas, Bristol-Myers Squibb, Dendreon, Janssen Research & Development, Medivation, OncoGenex and Sotio.
Additional information
Supplementary Information accompanies the paper on the Prostate Cancer and Prostatic Diseases website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Bryce, A., Alumkal, J., Armstrong, A. et al. Radiographic progression with nonrising PSA in metastatic castration-resistant prostate cancer: post hoc analysis of PREVAIL. Prostate Cancer Prostatic Dis 20, 221–227 (2017). https://doi.org/10.1038/pcan.2016.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.71
This article is cited by
-
A multidisciplinary approach to address unmet needs in the management of patients with non-metastatic castration-resistant prostate cancer
Prostate Cancer and Prostatic Diseases (2024)
-
Early PSA decline after starting second-generation hormone therapy in the post-docetaxel setting predicts cancer-specific survival in metastatic castrate-resistant prostate cancer
Prostate Cancer and Prostatic Diseases (2023)
-
Progression-free survival, disease-free survival and other composite end points in oncology: improved reporting is needed
Nature Reviews Clinical Oncology (2023)
-
Optimization Therapy by Coupling Intermittent Androgen Suppression with Impulsive Chemotherapy for a Prostate Cancer Model
Bulletin of Mathematical Biology (2023)
-
Editor’ summary: A paradigm shift in castration-resistant prostate cancer management
Prostate Cancer and Prostatic Diseases (2022)