Abstract
To determine CYP2C19 and CYP2C8 allele frequencies, 28 coding and/or functional variants were genotyped in 1250 African-American, Asian, Caucasian, Hispanic and Ashkenazi Jewish (AJ) individuals. The combined CYP2C19 variant allele frequencies ranged from ∼0.30 to 0.41; however, the CYP2C8 frequencies were much lower (∼0.04–0.13). After incorporating previously reported CYP2C9 genotyping results from these populations (36 total CYP2C variants), 16 multi-ethnic CYP2C haplotypes were inferred with frequencies >0.5%. Notably, the 2C19*17-2C9*1-2C8*2 haplotype was identified among African-Americans (8%) and Hispanics (2%), indicating that CYP2C19*17 does not always tag a CYP2C haplotype that encodes efficient CYP2C-substrate metabolism. The 2C19*1-2C9*2-2C8*3 haplotype was identified in all populations except African-Americans and additional novel haplotypes were identified in selected populations (for example, 2C19*2-2C9*1-2C8*4 and 2C19*4B-2C9*1-2C8*1), together indicating that both CYP2C19*17 and *2 can be linked with other CYP2C loss-of-function alleles. These results have important implications for pharmacogenomic association studies involving the CYP2C locus and are clinically relevant when administering CYP2C-substrate medications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Daly AK . Pharmacogenetics of the cytochromes P450. Curr Top Med Chem 2004; 4: 1733–1744.
Gray IC, Nobile C, Muresu R, Ford S, Spurr NK . A 2.4-megabase physical map spanning the CYP2C gene cluster on chromosome 10q24. Genomics 1995; 28: 328–332.
Goldstein JA . Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol 2001; 52: 349–355.
Chen Y, Goldstein JA . The transcriptional regulation of the human CYP2C genes. Curr Drug Metab 2009; 10: 567–578.
Desta Z, Zhao X, Shin JG, Flockhart DA . Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet 2002; 41: 913–958.
Price MJ, Tantry US, Gurbel PA . The influence of CYP2C19 polymorphisms on the pharmacokinetics, pharmacodynamics, and clinical effectiveness of P2Y(12) inhibitors. Rev Cardiovasc Med 2011; 12: 1–12.
Scott SA, Sangkuhl K, Shuldiner AR, Hulot JS, Thorn CF, Altman RB et al. PharmGKB summary: very important pharmacogene information for cytochrome P450, family 2, subfamily C, polypeptide 19. Pharmacogenet Genomics 2011; 22: 159–165.
Miners JO, Birkett DJ . Cytochrome P4502C9: an enzyme of major importance in human drug metabolism. Br J Clin Pharmacol 1998; 45: 525–538.
Van Booven D, Marsh S, McLeod H, Carrillo MW, Sangkuhl K, Klein TE et al. Cytochrome P450 2C9-CYP2C9. Pharmacogenet Genomics 2010; 20: 277–281.
Lai XS, Yang LP, Li XT, Liu JP, Zhou ZW, Zhou SF . Human CYP2C8: structure, substrate specificity, inhibitor selectivity, inducers and polymorphisms. Curr Drug Metab 2009; 10: 1009–1047.
Tsuneoka Y, Matsuo Y, Okuyama E, Watanabe Y, Ichikawa Y . Genetic analysis of the cytochrome P-45OIIC18 (CYP2C18) gene and a novel member of the CYP2C subfamily. FEBS Lett 1996; 384: 281–284.
Komai K, Sumida K, Kaneko H, Nakatsuka I . Identification of a new non-functional CYP2C18 allele in Japanese: substitution of T204 to A in exon2 generates a premature stop codon. Pharmacogenetics 1996; 6: 117–119.
Sim SC, Ingelman-Sundberg M . The Human Cytochrome P450 (CYP) Allele Nomenclature website: a peer-reviewed database of CYP variants and their associated effects. Hum Genomics 2010; 4: 278–281.
Xie HG, Prasad HC, Kim RB, Stein CM . CYP2C9 allelic variants: ethnic distribution and functional significance. Adv Drug Deliv Rev 2002; 54: 1257–1270.
Ross KA, Bigham AW, Edwards M, Gozdzik A, Suarez-Kurtz G, Parra EJ . Worldwide allele frequency distribution of four polymorphisms associated with warfarin dose requirements. J Hum Genet 2010; 55: 582–589.
Scott SA, Khasawneh R, Peter I, Kornreich R, Desnick RJ . Combined CYP2C9, VKORC1 and CYP4F2 frequencies among racial and ethnic groups. Pharmacogenomics 2010; 11: 781–791.
Georgitsi M, Viennas E, Gkantouna V, Christodoulopoulou E, Zagoriti Z, Tafrali C et al. Population-specific documentation of pharmacogenomic markers and their allelic frequencies in FINDbase. Pharmacogenomics 2011; 12: 49–58.
Ahmadi KR, Weale ME, Xue ZY, Soranzo N, Yarnall DP, Briley JD et al. A single-nucleotide polymorphism tagging set for human drug metabolism and transport. Nat Genet 2005; 37: 84–89.
Walton R, Kimber M, Rockett K, Trafford C, Kwiatkowski D, Sirugo G . Haplotype block structure of the cytochrome P450 CYP2C gene cluster on chromosome 10. Nat Genet 2005; 37: 915–916, author reply 916.
Yasar U, Lundgren S, Eliasson E, Bennet A, Wiman B, de Faire U et al. Linkage between the CYP2C8 and CYP2C9 genetic polymorphisms. Biochem Biophys Res Commun 2002; 299: 25–28.
Speed WC, Kang SP, Tuck DP, Harris LN, Kidd KK . Global variation in CYP2C8-CYP2C9 functional haplotypes. Pharmacogenomics J 2009; 9: 283–290.
Pedersen RS, Brasch-Andersen C, Sim SC, Bergmann TK, Halling J, Petersen MS et al. Linkage disequilibrium between the CYP2C19*17 allele and wildtype CYP2C8 and CYP2C9 alleles: identification of CYP2C haplotypes in healthy Nordic populations. Eur J Clin Pharmacol 2010; 66: 1199–1205.
Suarez-Kurtz G, Genro JP, de Moraes MO, Ojopi EB, Pena SD, Perini JA et al. Global pharmacogenomics: impact of population diversity on the distribution of polymorphisms in the CYP2C cluster among Brazilians. Pharmacogenomics J 2012 (in press).
Suarez-Kurtz G . Linkage disequilibrium between the CYP2C19*17 and CYP2C8*2 alleles in populations of African descent. Eur J Clin Pharmacol 2011; 67: 211–212.
Scott SA, Jaremko M, Lubitz SA, Kornreich R, Halperin JL, Desnick RJ . CYP2C9*8 is prevalent among African-Americans: implications for pharmacogenetic dosing. Pharmacogenomics 2009; 10: 1243–1255.
Scott SA, Martis S, Peter I, Kasai Y, Kornreich R, Desnick RJ . Identification of CYP2C19*4B: pharmacogenetic implications for drug metabolism including clopidogrel responsiveness. Pharmacogenomics J 2012 (in press).
Gurbel PA, Tantry US, Shuldiner AR, Kereiakes DJ . Genotyping: one piece of the puzzle to personalize antiplatelet therapy. J Am Coll Cardiol 2010; 56: 112–116.
Holmes Jr DR, Dehmer GJ, Kaul S, Leifer D, O′Gara PT, Stein CM . ACCF/AHA clopidogrel clinical alert: approaches to the FDA ″boxed warning″: a report of the American College of Cardiology Foundation Task Force on clinical expert consensus documents and the American Heart Association endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol 2010; 56: 321–341.
Beitelshees AL, Horenstein RB, Vesely MR, Mehra MR, Shuldiner AR . Pharmacogenetics and clopidogrel response in patients undergoing percutaneous coronary interventions. Clin Pharmacol Ther 2011; 89: 455–459.
Scott SA, Sangkuhl K, Gardner EE, Stein CM, Hulot JS, Johnson JA et al. Clinical pharmacogenetics implementation consortium guidelines for Cytochrome P450-2C19 (CYP2C19) genotype and clopidogrel therapy. Clin Pharmacol Ther 2011; 90: 328–332.
Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H et al. Pharmacogenetics: from bench to byte--an update of guidelines. Clin Pharmacol Ther 2011; 89: 662–673.
Taubert D, von Beckerath N, Grimberg G, Lazar A, Jung N, Goeser T et al. Impact of P-glycoprotein on clopidogrel absorption. Clin Pharmacol Ther 2006; 80: 486–501.
Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, Meneveau N et al. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med 2009; 360: 363–375.
Mega JL, Close SL, Wiviott SD, Shen L, Walker JR, Simon T et al. Genetic variants in ABCB1 and CYP2C19 and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial: a pharmacogenetic analysis. Lancet 2010; 376: 1312–1319.
Wallentin L, James S, Storey RF, Armstrong M, Barratt BJ, Horrow J et al. Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelor versus clopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trial. Lancet 2010; 376: 1320–1328.
Scott SA, Edelmann L, Kornreich R, Erazo M, Desnick RJ . CYP2C9, CYP2C19 and CYP2D6 allele frequencies in the Ashkenazi Jewish population. Pharmacogenomics 2007; 8: 721–730.
Scott SA, Edelmann L, Kornreich R, Desnick RJ . Warfarin pharmacogenetics: CYP2C9 and VKORC1 genotypes predict different sensitivity and resistance frequencies in the Ashkenazi and Sephardi Jewish populations. Am J Hum Genet 2008; 82: 495–500.
Scott SA, Edelmann L, Liu L, Luo M, Desnick RJ, Kornreich R . Experience with carrier screening and prenatal diagnosis for 16 Ashkenazi Jewish genetic diseases. Hum Mutat 2010; 31: 1240–1250.
de Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, Goldstein JA . The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem 1994; 269: 15419–15422.
Brandt JT, Close SL, Iturria SJ, Payne CD, Farid NA, Ernest 2nd CS et al. Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost 2007; 5: 2429–2436.
Collet JP, Hulot JS, Anzaha G, Pena A, Chastre T, Caron C et al. High doses of clopidogrel to overcome genetic resistance: the randomized crossover CLOVIS-2 (Clopidogrel and response variability investigation study 2). JACC Cardiovasc Interv 2011; 4: 392–402.
Hulot JS, Bura A, Villard E, Azizi M, Remones V, Goyenvalle C et al. Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood 2006; 108: 2244–2247.
Giusti B, Gori AM, Marcucci R, Saracini C, Sestini I, Paniccia R et al. Cytochrome P450 2C19 loss-of-function polymorphism, but not CYP3A4 IVS10 + 12G/A and P2Y12 T744C polymorphisms, is associated with response variability to dual antiplatelet treatment in high-risk vascular patients. Pharmacogenet Genomics 2007; 17: 1057–1064.
Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 2009; 360: 354–362.
Shuldiner AR, O′Connell JR, Bliden KP, Gandhi A, Ryan K, Horenstein RB et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA 2009; 302: 849–857.
Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, Silvain J et al. Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet 2009; 373: 309–317.
Hulot JS, Collet JP, Silvain J, Pena A, Bellemain-Appaix A, Barthelemy O et al. Cardiovascular risk in clopidogrel-treated patients according to cytochrome P450 2C19*2 loss-of-function allele or proton pump inhibitor coadministration: a systematic meta-analysis. J Am Coll Cardiol 2010; 56: 134–143.
Mega JL, Simon T, Collet JP, Anderson JL, Antman EM, Bliden K et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA 2010; 304: 1821–1830.
Gladding P, Panattoni L, Webster M, Cho L, Ellis S . Clopidogrel pharmacogenomics: next steps: a clinical algorithm, gene-gene interactions, and an elusive outcomes trial. JACC Cardiovasc Interv 2010; 3: 995–1000.
Roden DM, Shuldiner AR . Responding to the clopidogrel warning by the US food and drug administration: real life is complicated. Circulation 2010; 122: 445–448.
Ned Mmsc Phd RM . Genetic testing for CYP450 polymorphisms to predict response to clopidogrel: current evidence and test availability. Application: pharmacogenomics. PLoS Curr 2010; 2: RRN1180.
Lee CC, McMillin GA, Babic N, Melis R, Yeo KT . Evaluation of a CYP2C19 genotype panel on the GenMark eSensor(R) platform and the comparison to the Autogenomics Infiniti and Luminex CYP2C19 panels. Clin Chim Acta 2011; 412: 1133–1137.
Cayla G, Hulot JS, O′Connor SA, Pathak A, Scott SA, Gruel Y et al. Clinical, angiographic, and genetic factors associated with early coronary stent thrombosis. JAMA 2011; 306: 1765–1774.
Hoffmeyer S, Burk O, von Richter O, Arnold HP, Brockmoller J, Johne A et al. Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. Proc Natl Acad Sci USA 2000; 97: 3473–3478.
Nakamura T, Sakaeda T, Horinouchi M, Tamura T, Aoyama N, Shirakawa T et al. Effect of the mutation (C3435T) at exon 26 of the MDR1 gene on expression level of MDR1 messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clin Pharmacol Ther 2002; 71: 297–303.
Owen A, Goldring C, Morgan P, Chadwick D, Park BK, Pirmohamed M . Relationship between the C3435T and G2677T(A) polymorphisms in the ABCB1 gene and P-glycoprotein expression in human liver. Br J Clin Pharmacol 2005; 59: 365–370.
Rahman A, Korzekwa KR, Grogan J, Gonzalez FJ, Harris JW . Selective biotransformation of taxol to 6 alpha-hydroxytaxol by human cytochrome P450 2C8. Cancer Res 1994; 54: 5543–5546.
Dai D, Zeldin DC, Blaisdell JA, Chanas B, Coulter SJ, Ghanayem BI et al. Polymorphisms in human CYP2C8 decrease metabolism of the anticancer drug paclitaxel and arachidonic acid. Pharmacogenetics 2001; 11: 597–607.
Totah RA, Rettie AE . Cytochrome P450 2C8: substrates, inhibitors, pharmacogenetics, and clinical relevance. Clin Pharmacol Ther 2005; 77: 341–352.
Daily EB, Aquilante CL . Cytochrome P450 2C8 pharmacogenetics: a review of clinical studies. Pharmacogenomics 2009; 10: 1489–1510.
Soyama A, Saito Y, Komamura K, Ueno K, Kamakura S, Ozawa S et al. Five novel single nucleotide polymorphisms in the CYP2C8 gene, one of which induces a frame-shift. Drug Metab Pharmacokinet 2002; 17: 374–377.
Hichiya H, Tanaka-Kagawa T, Soyama A, Jinno H, Koyano S, Katori N et al. Functional characterization of five novel CYP2C8 variants, G171S, R186X, R186G, K247R, and K383N, found in a Japanese population. Drug Metab Dispos 2005; 33: 630–636.
Nakajima Y, Yoshitani T, Fukushima-Uesaka H, Saito Y, Kaniwa N, Kurose K et al. Impact of the haplotype CYP3A4*16B harboring the Thr185Ser substitution on paclitaxel metabolism in Japanese patients with cancer. Clin Pharmacol Ther 2006; 80: 179–191.
Saito Y, Katori N, Soyama A, Nakajima Y, Yoshitani T, Kim SR et al. CYP2C8 haplotype structures and their influence on pharmacokinetics of paclitaxel in a Japanese population. Pharmacogenet Genomics 2007; 17: 461–471.
Mao X, Bigham AW, Mei R, Gutierrez G, Weiss KM, Brutsaert TD et al. A genomewide admixture mapping panel for Hispanic/Latino populations. Am J Hum Genet 2007; 80: 1171–1178.
Perera MA, Gamazon E, Cavallari LH, Patel SR, Poindexter S, Kittles RA et al. The missing association: sequencing-based discovery of novel SNPs in VKORC1 and CYP2C9 that affect warfarin dose in African Americans. Clin Pharmacol Ther 2011; 89: 408–415.
Lane S, Al-Zubiedi S, Hatch E, Matthews I, Jorgensen AL, Deloukas P et al. The population pharmacokinetics of R- and S-warfarin: effect of genetic and clinical factors. Br J Clin Pharmacol 2012; 73: 66–76.
Li-Wan-Po A, Girard T, Farndon P, Cooley C, Lithgow J . Pharmacogenetics of CYP2C19: functional and clinical implications of a new variant CYP2C19*17. Br J Clin Pharmacol 2010; 69: 222–230.
Acknowledgements
This research was supported in part by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2 RR029885 (SAS). The eSensor 2C19 Test reagents used in this study were generously provided by GenMark Diagnostics (Carlsbad, CA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
J-SH has received research grant support from Fondation de France, INSERM, Fédération Francaise de Cardiologie, Biotronik and Medco Research Institute; consulting fees from Biotronik and Medco Health Solutions; and lecture fees from Daiichi Sankyo, Eli Lilly and Bristol-Myers Squibb. SAS has been a consultant to USDS, Inc.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Martis, S., Peter, I., Hulot, JS. et al. Multi-ethnic distribution of clinically relevant CYP2C genotypes and haplotypes. Pharmacogenomics J 13, 369–377 (2013). https://doi.org/10.1038/tpj.2012.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2012.10
Keywords
This article is cited by
-
Personalizing atomoxetine dosing in children with ADHD: what can we learn from current supporting evidence
European Journal of Clinical Pharmacology (2023)
-
Therapeutic Drug Monitoring of Lacosamide in Chinese Pediatric Patients with Epilepsy: Efficacy and Factors Influencing the Plasma Concentration
European Journal of Drug Metabolism and Pharmacokinetics (2023)
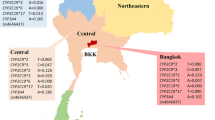
-
Allele frequencies of single nucleotide polymorphisms of clinically important drug-metabolizing enzymes CYP2C9, CYP2C19, and CYP3A4 in a Thai population
Scientific Reports (2021)
-
Modeling Approach to Predict the Impact of Inflammation on the Pharmacokinetics of CYP2C19 and CYP3A4 Substrates
Pharmaceutical Research (2021)
-
Effects of switching from clopidogrel to prasugrel at the chronic phase after coronary stenting on antiplatelet action and vascular endothelial function: Switch-Pras study
Heart and Vessels (2021)