Abstract
Differentiation between intestinal tuberculosis (ITB) and Crohn’s disease (CD) is challenging in geographical regions where both these diseases are prevalent. There is a need of biomarkers for differentiation between these two disorders. Colonic biopsies from inflamed mucosa of treatment-naive patients with ITB, CD and controls were used for analysis. Protein extracted from biopsies was digested with trypsin and resulting peptides were labeled with iTRAQ reagents. The peptides were subsequently analyzed using LC-MS/MS for identification and quantification. Gene ontology annotation for proteins was analyzed in PANTHER. Validation experiments were done for six differentially expressed proteins using immunohistochemistry. 533 proteins were identified and 241 proteins were quantified from 5 sets of iTRAQ experiments. While 63 were differentially expressed in colonic mucosa of patients with CD and ITB in at least one set of iTRAQ experiment, 11 proteins were differentially expressed in more than one set of experiments. Six proteins used for validation using immunohistochemistry in a larger cohort of patients; none of them however was differentially expressed in patients with ITB and CD. There are differentially expressed proteins in tissue proteome of CD and ITB. Further experiments are required using a larger cohort of homogeneous tissue samples.
Similar content being viewed by others
Introduction
Intestinal tuberculosis (ITB) and Crohn’s disease (CD) are chronic inflammatory diseases of the intestine1,2,3,4. The clinical, morphological and histological features of ITB and CD are so similar that it becomes difficult to differentiate between these two entities1,2,3,4. In geographical regions such as India where both ITB and CD are prevalent, differential diagnosis between the two is challenging5,6. The natural history of CD is quite different from that of ITB5,6. While ITB gets cured with appropriate anti-tuberculosis treatment, CD has a remitting/relapsing or persistent course and stays life-long usually. Furthermore, biologics, which have now become one of the important treatment modalities for CD, their use however can lead to flare not only the latent tuberculosis but also the disease if the mistaken diagnosis of CD is made in a patient having ITB5,6,7. Because of similarity in the clinical presentation, endoscopic appearance and histological characteristics between these two diseases, many of them are treated empirically with anti-tuberculous drugs at times2,3,4,5,6,8,9,10,11,12. While anti-saccharomyces cerevisiae antibodies has been reported more often in patients with CD in comparison to that in ulcerative colitis; ASCA is also positive in almost half of patients with ITB and hence a differentiation between CD and ITB can not be made using ASCA13,14. There is a need for a biomarker which can differentiation CD from ITB, none really exist at present.
Keeping in view of the recent developments in the field of clinical proteomics, we used this technique to identify biological marker(s) that can differentiate ITB from CD. Proteomics is a promising technology and it is used to understand the biological processes involved in inflammatory bowel diseases (IBD)15. Since, both ITB and CD manifest first at the intestinal mucosa, comparing the mucosal proteome of these two diseases might help in identifying differentially expressed proteins, their possible networks and interactions involved in development of these two diseases. A proteomic approach has been used earlier for finding out differences between different forms of colitides and for exploring a biomarker for the activity of the disease16,17,18,19,20. Proteomics has also been employed in the area of tuberculosis research in the quest for biomarkers21. This technology has yet not been explored to detect potentially useful markers that can help differentiating ITB from CD.
In this study, we analyzed and compared the proteome of the inflamed colonic mucosa of patients with ITB and CD. Isobaric Tags for Relative and Absolute Quantification (iTRAQ) labeling technology followed by two-dimensional liquid chromatography and tandem mass spectrometry was used to compare the proteome of these two conditions for identification of potential biomarkers for differentiation of these two diseases with each other.
Patients and Methods
Patients with CD and ITB were recruited from the Gastroenterology Clinic of All India Institute of Medical Sciences, New Delhi. The Ethics Committee of our Institution approved this study. The study was conducted as per guidelines of Indian Council of Medical Research/Good Clinical Practice. Informed and written consent was obtained from each participant of this study.
Complete evaluation of patients including their clinical, endoscopic, radiological and histological characteristics was done. Details of intake of anti-tuberculosis treatment in the past were documented. All patients underwent a colonoscopic (and retrograde ileoscopy where feasible) examination using a video-colonoscope after colon preparation with colonic lavage solution (polyethylene glycol). While as many as 30 patients were recruited and their biopsies were preserved in −80 °C, for the exploratory analysis of the proteome, the biopsies of only those patients were included where the follow up was complete and the diagnosis of either ITB or CD was confirmed. Since the present study was a pilot exploratory study, we have included 15 patients in the exploratory phase and 52 patients in the validation phase.
Collection of biological samples
During colonoscopy, a segment-wise involvement of the colon was documented. Multiple mucosal biopsies, including five to six pieces from the macroscopically abnormal area (ulcerations, nodularity) and two to three biopsy pieces from the endoscopically normal looking areas, were obtained. Four bits of biopsies were fixed separately in 10% buffered formal-saline for histological features. After adequate fixation paraffin blocks were processed. From each block, 20 step sections of 4 μm thickness were prepared for detailed morphological assessment. The sections were stained by hematoxylin and eosin stain and were examined by two pathologists with special interest in gastrointestinal pathology who were blinded about the clinical data and final diagnoses of the patients. For proteomic study, 6–8 pieces of mucosal biopsies were obtained from the most involved area of the colon, mostly right side of the colon and ileocecal valve. Biopsies from the normal appearing colonic mucosa from ITB patients were also taken, which served as controls. These biopsies were snap frozen in liquid nitrogen and stored at −80 °C.
Diagnostic criteria for CD and ITB
The diagnosis of CD was established on the basis of the European Crohn’s and Colitis Organization guidelines which is a combination of clinical, endoscopic and histological features22. The diagnosis of ITB was made on the basis of characteristic clinical features (abdominal pain, constipation and/or diarrhea, constitutional symptoms, and intestinal obstruction), endoscopic features (ileocecal area involvement, ulcerations, nodularity, and strictures), histological features (presence of granulomas), microbiological tests (presence of acid-fast bacilli on the smear examination or demonstration of acid fast bacilli by polymerase chain reaction), and response to anti-tuberculous treatment (Paustian’s criteria with Logan’s modification)23,24.
Sample preparation for iTRAQ labeling and strong cation exchange chromatography
Snap frozen colonic biopsies were homogenized, re-suspended in lysis solution (8M urea, 2M thiourea and 4% CHAPS (3-[(3-Cholamidopropyl) dimethylammonio]-1-propanesulfonate]) and centrifuged at 10,000 g for 15 minutes at 4 °C. Debris was discarded and the supernatant was transferred onto a fresh Eppendorf tube. Protein extracted with lysis solution was buffer exchanged with 250 mM TEAB (Triethylammonium bicarbonate) using a 3 kDa cut off membrane filters to bring down the concentration of urea well below 0.1 M. Protein amount was quantified using the Bradford assay. 100 μg of protein was then trypsinized and labeled with 4 plex iTRAQ reagents (Siex, Framingham, MA, USA). Briefly, one unit of iTRAQ reagent required to label 100 μg of protein was thawed and reconstituted in 70 μl ethanol. Protein from each group was reduced, cysteine blocked and digested with trypsin. Tryptic peptides of reference pool which was pool of all 15 samples, CD, ITB and control groups were labeled with 114, 115, 116, and 117 iTRAQ tags, respectively, by incubating at room temperature for one hour for the first set of experiments. Remaining sets were labeled as given in the Table 1 on study design. The peptide mixtures belonging to each set were then pooled and dried in a speed vac. The pooled mixtures for each sample set were fractionated by a strong cation exchange chromatography.
Cation exchange chromatography was done using liquid chromatography system (Shimadzu, Kyoto, Japan). The peptide mixture was diluted with 1ml of buffer A (10 mM potassium phosphate, 25% acetonitrile, pH 2.9) and loaded onto a 2.1 mm × 150 mm cation column containing 5 μm particles and a 300 μm pore size (ZORBAX SCX 300; Agilent Technologies, Santa Clara, CA, USA). The peptides were eluted at a flow rate of 300 μl/minute with a gradient of 0% Buffer B (1M KCl, 10mM potassium phosphate, 25% acetonitrile, pH 2.9) for 10 minutes, 0–30% Buffer B for 25 minutes, 30–60% Buffer B for 10 minutes, 60–100% Buffer B for 5 minutes. The system was then maintained in 100% Buffer B for 10 minutes before equilibrating with 0% Buffer B for 30 minutes prior to the next injection. Thirty fractions were collected every minute. Monitoring of the elutions was dome by measuring absorbance at 220 nm, and vacuum-dried.
Protein identification and quantitation
The peptides from each cation exchange fraction were resuspended in 0.1% formic acid and 3% acetonitrile solution and injected to a nano-LC system (TempoTM; Siex, Framingham, MA, USA) equipped with a C18-75 μm × 150 mm column (Michrom Bioresources, Inc. USA). The samples were desalted online and an 84 minutes gradient of increasing acetonitrile concentration was used to separate the peptides. The eluent was sprayed into a tandem mass spectrometer (QSTAR XL; Siex, Framingham, MA, USA) and analyzed in Information Dependent Acquisition (IDA) mode using software (Analyst QS 1.1; Siex, Framingham, MA, USA). The collision energy was set with an intercept value +4 higher than that normally used for peptides, to provide for sufficient peptide fragmentation and generation of the iTRAQ reporter groups.
Mascot, version 3.2.2b, (Matrix Sciences, London, UK) was used for protein identification and quantitation from MS/MS data. For Mascot search, the nano-LC-ESI MS/MS data for 2+, 3+ and 4+ charged precursor ions were converted to centroid data, without smoothing, using the mascot.dll script in Analyst QS1.1. The MS/MS settings included: spectra de-isotoped except for the iTRAQ reporter region, peak areas reported, spectra rejected if they contained less than 10 peaks, and peaks not removed if they were close to the precursor m/z. The data were searched with a tolerance of 100 ppm for the precursor ions and 0.3 Da for the fragment ions. The following settings were used: trypsin was the cleavage enzyme, one missed cleavage allowed, carboxymethyl modification of cysteines was fixed modification and methionine oxidation was selected as a variable modification. Quantitaion method was iTRAQ 4 plex. Spectra were searched against SwissProt 57.15 database (515203 sequences; 181334896 residues) with taxonomy: Homo sapiens (human) (20266 sequences). The following settings were used to obtain the quantification results: the protein ratio type was the ‘weighted’ geometric mean, normalization with summed intensities and outlier removal was ‘automatic’. The peptide threshold was ‘at least homology’ (peptide score does not exceed absolute threshold but is an outlier from the quasi-normal distribution of random scores), the minimum number of peptides was two and peptides were required to be the top ranking peptide matches. An automatic decoy database search was also performed to estimate false discovery rate (FDR) for the search. The list of proteins identified and quantitated from each set was imported to an excel sheet. Since hemoglobin was consistently identified in each set of experiment, we normalized the data to one of the house keeping genes, beta actin, to exclude the effect of blood derived proteins. Average quantitation value for each protein was calculated and a t-test was performed for each protein, when it was present in more than two set of experiments.
Bioinformatics analyses
Swiss Prot accession numbers of the proteins identified were used to extract gene ontology annotations from Protein Analysis through Evolutionary Relationships (PANTHER) classification system. Protein function and sub-cellular localization analyses were then performed using the gene ontology information and charts were made using the PANTHER (http://pantherdb.org; version 9.0) classification system. The PANTHER database was ideal for high throughput functional analysis for the datasets of protein sequences identified.
Immunohistochemistry
Sections were cut from the archived paraffin blocks of colonic biopsies, dewaxed and rehydrated. Then endogenous peroxidase activity was blocked by 3% hydrogen peroxide (H2O2) and 0.1% protease, digested for 2 minutes at room temperature. The sections were then incubated with primary antibodies (Abcam, UK) and incubated overnight at 4 °C. Primary antibodies against Trefoil factor-3 (TFF3; 1:200), Thioredoxin (TRX; 1:500), Transgelin (SM22; 1:200), Tropomyosin (TPM; 1:50), IgGFc-binding protein (FCGBP; 1:200) and Myosin (MYH; 1:100) were used to validate the results of proteomic analysis as these proteins were found to be differently expressed in the inflamed mucosa of patients with CD and ITB.
The slides were then washed thrice with tris-buffered saline (pH 7.6) and finally incubated for 30 minutes with universal secondary antibody (BioCare Universal Kit, MACH4, Concord, CA, USA). The antigen-antibody reaction was visualized with peroxidase-substrate reaction by using 3, 3′-Diaminobenzidine (DAB) as chromogen. During interpretation a semi-quantitative grading as performed by considering total areas of stain expression and intensity of staining. The extent of protein staining was scored from 1 to 4, and the intensity of staining was scored from 1 to 3. The scores were then multiplied together and the final scores were classified as follows: 1–3, weak staining; 4–8, moderate staining; and 9–12, strong staining. A Fisher’s exact test was performed to assess the distribution pattern of the immunochemical score for expression of the protein.
Results
Proteomic experiments
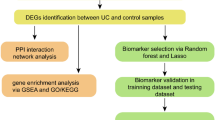
The strategy used for the proteomics analysis in this study is shown in Fig. 1. The colonic mucosal biopsy samples from 15 patients (5 with ITB, CD and controls each) were used as per the design shown in Table 1. A total of 533 proteins were identified in the five sets of experiments carried out and 241 proteins among these were quantified with the criteria of at least two peptides being quantified in the mascot. One hundred and thirty eight proteins among these were identified and quantified in at least two sets of experiments (Table 2). The results from the five sets of experiments were comparable in terms of total number of proteins identified and quantified and false discovery rate was consistently low. It was noted that hemoglobin was consistently common. A Bioinformatics analysis of all the identified proteins was carried out in PANTHER. A detailed gene ontology analysis of these proteins has been depicted in Fig. 2.
(A) Pie chart showing the Gene ontology annotation distribution of all the proteins identified in the macroscopically affected colonic mucosal biopsies in the proteome analysis. The proteins are grouped according to their molecular function. (B) Pie chart showing the Gene ontology annotation distribution of all the proteins identified in the macroscopically affected colonic mucosa in the proteome analysis. The proteins are grouped according to the known biological processes they are involved in. (C). Pie chart showing the Gene ontology annotation distribution of all the proteins identified in the macroscopically affected colonic mucosa in the proteome analysis. The proteins are grouped according to the cellular distribution.
Differential expression of proteins in the macroscopically affected colonic mucosa of patients with ITB in comparison to control biopsies
Fifty-one proteins were differentially expressed in biopsies from patients with ITB with reference to controls with the criteria of iTRAQ ratio <0.7 or >1.3, in at least one set of iTRAQ experiment. Twenty-three proteins were under-expressed in ITB and 28 proteins were overexpressed with respect to controls. Among those proteins, which were identified in more than one experiment, four proteins (myosin-11, macrophage migration inhibitory factor, heterogeneous nuclear ribonucleoprotein A1-like 2 and myosin-10) were significantly underexpressed (p value < 0.05) and four proteins (histone H2B type 1-B, hemoglobin subunit alpha, beta and delta) were overexpressed (p value < 0.05) in macroscopically affected colonic mucosa of patients with ITB with reference to control biopsies.
Differential expression of proteins in the macroscopically affected colonic mucosa of patients with CD in comparison to control colonic biopsies
Seventy-eight proteins were differentially expressed in the colonic mucosa of patients with CD with reference to control biopsies with the criteria of ratio <0.7 or >1.3, in at least one set of iTRAQ experiment. Nineteen proteins were under-expressed and 59 proteins were overexpressed in patients with CD with respect to control biopsies. Among those proteins, which were identified in more than one experiment, six proteins were significantly underexpressed (alpha 1 acid glycoprotein, fatty acid-binding protein, serum albumin, IG kappa chain, mucin-2 precursor, and serotransferrin) (p value < 0.05) and 13 proteins were over-expressed (apolipoprotein A1, annexin A5, myosin-14, glyceraldehyde-3-phosphate dehydrogenase, histone H2B type 1-B, tropomyosin alpha-1 chain, transgelin, tropomyosin alpha-4 chain, L-lactate dehydrogenase B chain, fructose-bisphosphate aldolase A, peroxiredoxin-1, cofilin-1, protein disulfide-isomerase) (p value < 0.05) in patients with CD with reference to controls.
Differential expression of proteins in macroscopically affected colonic mucosa of patients with CD and ITB
Sixty-three proteins were differentially expressed in the colonic mucosa of patients with patients with CD and ITB in at least one set of iTRAQ experiment. Twenty proteins were underexpressed and 41 proteins were overexpressed in the colonic mucosa of patients with CD with respect to that in colonic mucosa of patients with ITB. Among those proteins, which were identified in more than one experiment, two proteins were significantly underexpressed (p value <0.05, ratio <0.7) and nine proteins were overexpressed (p value < 0.05, ratio > 1.3) in patients with CD with reference to ITB. List of all the proteins differentially expressed are shown in Tables 3 and 4 and Fig. 3.
Bioinformatics analysis
A Bioinformatics analysis of both overexpressed and underexpressed proteins was carried out in PANTHER. The molecular function, biologic process and cellular location of these proteins was similar to the overall proteome covered. A pathway analysis of these differentially expressed proteins was carried out in PANTHER. The different pathways, with which these differentially expressed proteins possibly are involved, has been shown in Fig. 4. The underexpressed proteins were annotated to fructose galactose metabolism, apoptosis signaling pathway, plasminogen activating cascade, Parkinson’s disease, gonadotropin releasing hormone receptor pathway, glycolysis and blood coagulation pathways. On the other hand, the overexpressed proteins were annotated to pathways including cytoskeletal regulation, inflammation, integrin signaling pathway, hypoxia, oxidative stress response, FAS signaling pathway and G-protein signaling pathways.
(A) Pie chart showing the Gene ontology annotation and the pathway distribution of underexpressed proteins in the macroscopically affected mucosa of patients with CD and ITB. (B) Pie chart showing the Gene ontology annotation and the pathway distribution of overexpressed proteins in the macroscopically affected mucosa of patients with CD and ITB.
Validation of differentially expressed proteins using immunohistochemistry
Amongst the entire protein expression pattern studied by immunohistochemistry in the colonic biopsies, trefoil factor 3 expression pattern was significantly different in ITB in comparison to the biopsies from patients with CD in the initial analysis on 29 patients. While in the former the expression of trefoil factor 3 was predominantly weak to moderate, in ITB expression of trefoil factor 3 was always moderate to strong. However, this was not observed when we increased the sample size to 52 (Table 5). The expression patterns of IgGFc-binding protein, myosin, thioredoxin, transgelin and tropomysin proteins were not different in colonic biopsies in either of the diseases. Tropomysin was expressed in blood vessels and was not expressed in the epithelial cells. All other proteins as described above were however expressed over colonic epithelial cells. While trefoil factor 3 and IgGFc-binding protein proteins were expressed mostly in the goblet cell cytoplasm (Fig. 5A,B); Myosin and thioredoxin proteins were expressed in the epithelial cell cytoplasm in the control biopsies. Transgelin and topomyosin proteins were seen in the wall of the blood vessels (Fig. 5C–F). The expression of myosin, thioredoxin and transgelin proteins were particularly strong in both the CD and ITB in colonic biopsies.
Microphotograph showing normal expression pattern of trefoil factor-3 [arrow] ((A), IHC [TFF3] x40), IgGFc-binding protein [arrow] ((B), IHC [FCGBP] x40), Myosin [arrow] ((C), IHC [MYH] x40), transgelin ((D), IHC [SM22] x40), tropomyosin ((E), IHC [Tropomyosin] x40) and Thioredoxin protein [arrow] ((F), IHC [TRX] x40). Comparative expression patterns of trefoil factor-3 in colon biopsies: (G) showing trefoil factor-3 expression score 12 ((G), IHC [TFF3] x40), expression score 6 ((H), IHC [TFF3] x40), and expression score 0 ((I), IHC [TFF3] x40).
Discussion
The present study is the first ever proteomics analysis of mucosal biopsies from patients with CD and ITB and it has revealed several promising biomarker candidates for differentiation between these two diseases. In five sets of iTRAQ experiments, 533 proteins were identified and 241 proteins were quantified. Overall 63 proteins were differentially expressed in the colonic mucosa of patients with CD and ITB in at least one set of iTRAQ experiment, of them 11 proteins were differentially expressed in more than one set of experiments. Of them, We propose that trefoil factor 3, fatty acid synthase, Myosin 14, Myosin 11, Human thioredoxin 1, IgG Fc-binding protein, transgelin, and tropomyosin as potential candidates for biomarker development for differentiation between CD and ITB.
The proteins, which were differentially expressed in the colonic mucosa of patients with CD and ITB, may be playing a role in the pathogenesis of the disease or they may have appeared in the tissue as a consequence of thee diseases. For example, significantly lower expression of trefoil factor-3 level in patients with CD is likely to be marker of the activity of the disease. While we included both CD and ITB in the their active phase, the differentially lower expression of trefoil peptide-3 in patients with CD in comparison to that in ITB is reflective of larger area of mucosal involvement in those with CD. In one of our another study, we observed a higher level of serum trefoil factor-3 in the serum of patients with healed stage of ulcerative colitis in comparision to those having active disease25. Both these observations suggest that trefoil factor 3 may be a good marker of disease activity. Trefoil factor-3 is one of the three small, compact proteins expressed by the goblet cells in the gastrointestinal tract26. In addition to having anti-inflammatory properties, trefoil peptide also play an important role in the maintenance and repair of the gastrointestinal tract mucosa. The expression of trefoil is suppressed by tumor necrosis factor-α, the level of which remains high in patients with CD27.
While, distal and terminal ileum is involved both in CD and ITB, the quantum of mucosal involvement is more in patients with CD than that in ITB. A four-fold increase in the expression of fatty acid synthase in patients with CD as compared to that in ITB may partly be attributed to the higher altered fat metabolism and enterohepatic circulation of bile acids in patients with CD than that in ITB28,29,30.
While in the discovery experiments, several proteins were differentially expressed in the colonic mucosa of patients with CD and ITB with the ratio cut-off of <0.7 and >1.3; a very few proteins were expressed with sufficiently high fold differences required for development of a candidate biomarker. Whereas the individual pairs of the biopsies yielded several differentially expressed proteins in each experiment, this was not reflected consistently in all the five experiments. Furthermore, a lower level of differential expression of proteins in the colonic biopsies of patients with CD and ITB was also reflected by similar pattern of expression of these proteins by immunohistochemistry in a larger cohort of biopsies from patients with CD and ITB. This phenomenon may partly be attributed to the heterogeneity of the colonic mucosal biopsies as both CD and ITB are very diverse diseases. As colon contains four layers and the depth of involvement in both CD and ITB may vary in individual patients and thereby the tissue obtained from the edge of ulcers may also vary. These cell layers will have different protein expression profiles. The variable depth of biopsies therefore might have contributed to the heterogeneity of the proteome and skewed the quantitative proteome data. A proteome analysis in a more histologically directed manner is perhaps a better approach in this scenario. Since the intestine is a complex tissue, isolation and proteome analysis of a particular cell type involved actively in the disease process, such as colonocytes, is likely to provide a proteome enriched in low abundant proteins and a better resolution of proteome. Laser capture micro-dissection of intestinal biopsy specimens to obtain specific cells or density gradient separation to separate various cell types could be another strategy in this direction for future studies31. A complementary technique, MALDI imaging, may also be useful to obtain peptide signature for a particular layer of the intestine32.
In conclusion, a comparative analysis of the proteome profile of colonic biopsies from the macroscopically affected areas of the colons of patients with CD and ITB yielded 533 proteins of which 241 proteins could be quantified. There were differentially expressed proteins in the tissue proteome of patients with CD and ITB. Further experiments are required using a larger cohort of homogeneous tissue samples in order to find a biomarker for differentiation between CD and ITB.
Additional Information
How to cite this article: Rukmangadachar, L. A. et al. Proteome analysis of the macroscopically affected colonic mucosa of Crohn's disease and intestinal tuberculosis. Sci. Rep. 6, 23162; doi: 10.1038/srep23162 (2016).
References
Almadi, M. A., Ghosh, S. & Aljebreen, A. M. Differentiating intestinal tuberculosis from Crohn’s disease: a diagnostic challenge. Am. J. Gastroenterol. 104, 1003–12 (2009).
Epstein, D., Watermeyer, G. & Kirsch, R. Review article: the diagnosis and management of Crohn’s disease in populations with high-risk rates for tuberculosis. Aliment. Pharmacol. Ther. 25, 1373–1388 (2007).
Makharia, G. K. et al. Clinical, endoscopic, and histological differentiations between Crohn’s disease and intestinal tuberculosis. Am. J. Gastroenterol. 105, 642–51 (2010).
Pulimood, A. B. et al. Differentiation of Crohn’s disease from intestinal tuberculosis in India in 2010. World J. Gastroenterol. 17, 433–43 (2011).
Ooi, C. J. et al. Asia Pacific Association of Gastroenterology (APAGE) Working Group on Inflammatory Bowel Disease. Asia-Pacific consensus statements on Crohn’s disease. Part 2: Management. J. Gastroenterol. Hepatol. 31, 56–68 (2016).
Ramakrishna, B. S. et al. Indian Society of Gastroenterology Task Force on Inflammatory Bowel Diseases. Indian Society of Gastroenterology consensus statements on Crohn’s disease in India. Indian J. Gastroenterol. 34, 3–22 (2015).
Li, X. et al. Predictors of clinical and endoscopic findings in differentiating Crohn’s disease from intestinal tuberculosis. Dig. Dis. Sci. 56, 188–96 (2011).
Pulimood, A. B. et al. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn’s disease. J. Gastroenterol. Hepatol. 20, 688–96 (2005).
Lee, Y. J. et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn’s disease. Endoscopy. 38, 592–7 (2006).
Kirsch, R., Pentecost, M., Hall, Pde, M., Epstein, D. P., Watermeyer, G. & Friederich, P.W. Role of colonoscopic biopsy in distinguishing between Crohn’s disease and intestinal tuberculosis. J. Clin. Pathol. 59, 840–844 (2006).
Ng, S. C. et al. Systematic review with meta-analysis: accuracy of interferon-gamma releasing assay and anti-Saccharomyces cerevisiae antibody in differentiating intestinal tuberculosis from Crohn’s disease in Asians. J. Gastroenterol. Hepatol. 29, 1664–70 (2014).
Du, J., Ma, Y. Y., Xiang, H. & Li,Y. M. Confluent granulomas and ulcers lined by epithelioid histiocytes: new ideal method for differentiation of ITB and CD? A meta analysis. PLoS One. 9, e103303 (2014).
Makharia, G. K., Sachdev, V., Gupta, R., Lal, S. & Pandey, R. M. Anti-Saccharomyces cerevisiae antibody does not differentiate between Crohn’s disease and intestinal tuberculosis. Dig. Dis. Sci. 52, 33–39 (2007).
Ghoshal, U. C., Ghoshal, U., Singh, H. & Tiwari, S. Anti-Saccharomyces cerevisiae antibody is not useful to differentiate between Crohn’s disease and intestinal tuberculosis in India. J. Postgrad. Med. 53, 166–170 (2007).
Roda, G. et al. New proteomic approaches for biomarker discovery in inflammatory bowel disease. Inflamm. Bowel Dis. 16, 1239–46 (2010).
M’Koma, A. E. Proteomic profiling of mucosal and submucosal colonic tissues yields protein signatures that differentiate the inflammatory colitides. Inflamm. Bowel Dis. 17, 875–83 (2011).
Han, N. Y., Choi, W., Park, J. M., Kim, E. H., Lee, H. & Hahm, K. B. Label-free quantification for discovering novel biomarkers in the diagnosis and assessment of disease activity in inflammatory bowel disease. J. Dig. Dis. 14, 166–74 (2013).
Shen, J., Qiao, Y., Ran, Z., Wang, T., Xu, J. & Feng, J. Intestinal protein expression profile identifies inflammatory bowel disease and predicts relapse. Int. J. Clin. Exp. Pathol. 6, 917–25 (2013)
Townsend, P. et al. Serum Proteome Profiles in Stricturing Crohn’s Disease: A Pilot Study. Inflamm. Bowel Dis. 21, 1935–41 (2015)..
Meuwis, M. A. et al. Biomarker discovery for inflammatory bowel disease, using proteomic serum profiling. Biochem. Pharmacol. 73, 1422–33 (2007).
Liu, Q. et al. Serum protein profiling of smear-positive and smear-negative pulmonary tuberculosis using SELDI-TOF mass spectrometry. Lung. 188, 15–23 (2010).
Van Assche, G. et al. European Crohn’s and Colitis Organisation (ECCO). The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Definitions and diagnosis. J. Crohns Colitis. 4, 7–27 (2010).
Paustian, F. F. Tuberculosis of the intestine. In: Bockus H. L., ed. Bockus Gastroenterology, Volume 4. 5th ed. Philadelphia: Saunders (1995).
Logan, V. S. Anorectal tuberculosis. Proc R Soc Med. 62, 1227–30 (1969).
Srivastava, S. et al. Serum human trefoil factor 3 is a biomarker for mucosal healing in ulcerative colitis patients with minimal disease activity. J. Crohns Colitis. 9, 575–9 (2015).
Madsen, J., Nielsen, O., Tornøe, I., Thim, L. & Holmskov, U. Tissue localization of human trefoil factors 1, 2, and 3. J. Histochem. Cytochem. 55, 505–13 (2007).
Zhu, Y. Q. & Tan, X. D. TFF3 modulates NF-{kappa}B and a novel negative regulatory molecule of NF-{kappa}B in intestinal epithelial cells via a mechanism distinct from TNF-{alpha}. Am. J. Physiol. Cell Physiol. 289, C1085–93 (2005).
Marion-Letellier, R., Savoye, G., Beck, P. L., Panaccione, R. & Ghosh, S. Polyunsaturated fatty acids in inflammatory bowel diseases: a reappraisal of effects and therapeutic approaches. Inflamm. Bowel Dis. 19, 650–61 (2013).
Nolan, J. D., Johnston, I. M. & Walters, J. R., Altered enterohepatic circulation of bile acids in Crohn’s disease and their clinical significance: a new perspective. Expert Rev. Gastroenterol. Hepatol. 7, 49–56 (2013).
Boehm, D. et al. Lipid peroxidation markers in Crohn’s disease: the associations and diagnostic value. Clin. Chem. Lab. Med. 50, 1359–66 (2012).
Alex, P., Gucek, M. & Li, X. Applications of proteomics in the study of inflammatory bowel diseases: Current status and future directions with available technologies. Inflamm. Bowel Dis. 15, 616–29 (2009).
Seeley, E. H. & Caprioli, R. M. MALDI imaging mass spectrometry of human tissue: method challenges and clinical perspectives. Trends Biotechnol. 29, 136–43 (2011).
Acknowledgements
This study was financed by a research grant from Department of Biotechnology, Government of India (BT/PR 9304/Med/29/18/2007).
Author information
Authors and Affiliations
Contributions
The research study was conceptualized, design and supervised by V.A., G.K.M., A.S. and S.K.A. Fund was organized by S.K.A. Recruitment of patients was done by A.M., G.M. and V.A. Performance of laboratory experiments was done by L.A.R. Interpretations of histology slides was performed by P.D. and S.D.G. Analysis and interpretation of data, writing and drafting of the manuscript was done by L.A.R. and G.H. Critical review of the manuscript was done by G.K.M., G.H., A.S. and V.A. All authors were involved in the preparation and finalization of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Rukmangadachar, L., Makharia, G., Mishra, A. et al. Proteome analysis of the macroscopically affected colonic mucosa of Crohn’s disease and intestinal tuberculosis. Sci Rep 6, 23162 (2016). https://doi.org/10.1038/srep23162
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23162
This article is cited by
-
Evidence-based approach to diagnosis and management of abdominal tuberculosis
Indian Journal of Gastroenterology (2023)
-
Genome-wide DNA methylation profiling in differentiating Crohn’s disease from intestinal tuberculosis
Genes & Genomics (2022)
-
Proteomic analysis-based discovery of a novel biomarker that differentiates intestinal Behçet’s disease from Crohn’s disease
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.