Abstract
Taste receptors on enteroendocrine cells sense nutrients and transmit signals that control gut hormone release. This study aimed to investigate the amino acid (AA) sensing mechanisms of the ghrelin cell in a gastric ghrelinoma cell line, tissue segments and mice. Peptone and specific classes of amino acids stimulate ghrelin secretion in the ghrelinoma cell line. Sensing of L-Phe occurs via the CaSR, monosodium glutamate via the TAS1R1-TAS1R3 while L-Ala and peptone act via 2 different amino acid taste receptors: CaSR & TAS1R1-TAS1R3 and CaSR & GPRC6A, respectively. The stimulatory effect of peptone on ghrelin release was mimicked ex vivo in gastric but not in jejunal tissue segments, where peptone inhibited ghrelin release. The latter effect could not be blocked by receptor antagonists for CCK, GLP-1 or somatostatin. In vivo, plasma ghrelin levels were reduced both upon intragastric (peptone or L-Phe) or intravenous (L-Phe) administration, indicating that AA- sensing is not polarized and is due to inhibition of ghrelin release from the stomach or duodenum respectively. In conclusion, functional AA taste receptors regulate AA-induced ghrelin release in vitro. The effects differ between stomach and jejunum but these local nutrient sensing mechanisms are overruled in vivo by indirect mechanisms inhibiting ghrelin release.
Similar content being viewed by others
Introduction
Obesity is one of the major healthcare problems of our western society reaching epidemic proportions. To date, gastric bypass surgery is the only intervention that consistently induces sustained weight loss and remission of concomitant diseases1,2. A less drastic tool to induce weight loss is focussing on the macronutrient composition of a diet.
A high-protein diet has beneficial effects on both weight loss and weight maintenance compared to an isoenergetic intake of fat and carbohydrates3. A large European study showed that a diet with a modest increase in protein content and a modest reduction in glycaemic index led to an improvement in maintenance of weight loss4. It is already known that dietary protein intake results in the release of satiety hormones like peptide YY (PYY), glucagon-like peptide 1 (GLP-1) and cholecystokinin (CCK)5. Studies in PYY null mice showed an important role for PYY in protein-mediated satiation and body weight regulation6. In addition, several studies reported a decrease in plasma ghrelin levels following ingestion of a high-protein diet7,8.
Ghrelin is a 28-amino acid peptide released from the X/A-like cells of the gastric oxyntic mucosa in response to hunger and starvation9. A posttranslational modification by the enzyme ghrelin-O-acyltransferase (GOAT), placing an octanoyl group on the third amino acid serine (Ser3), is required for ghrelin’s biological activity10,11. Although initially discovered as a hormone that stimulates growth hormone secretion, ghrelin is now considered as a multifunctional hormone that stimulates food intake, prevents fat utilization, increases body weight, inhibits glucose-induced insulin release and stimulates gastrointestinal motility9,12,13,14.
The chemosensory signalling pathways involved in sensing of peptides and amino acids by the ghrelin cell are unknown. Specific amino acid taste receptors on enteroendocrine cells, similar to those in the lingual system and transporters on enterocytes in the gut are candidates for sensing and uptake of protein breakdown products15,16. Up to now, three important amino acid taste receptors are cloned and characterized, each with a specific preference for a particular class of amino acids. The calcium sensing receptor (CaSR), expressed in gastrin- (G-cells), cholecystokinin- (CCK) (I-cells) and somatostatin-secreting cells (D-cells), mainly senses aromatic amino acids and calcium (Ca2+)17,18,19. The G-protein coupled receptor family C group 6 member A (GPRC6A), a receptor that predominantly senses basic amino acids and Ca2+, acts in concert with the CaSR and is expressed in gastric antral D- and G-cells18,20. The heterodimer taste receptor type 1 member 1 - taste receptor type 1 member 3 (TAS1R1-TAS1R3), also known as the umami taste receptor, is mainly activated by umami stimuli, glutamic and aspartic acids, in humans but in rodents it broadly detects most of the 20 L-amino acids21,22. One of the subtypes, TAS1R3, which is also involved in sensing of carbohydrates, is expressed in L-cells and X/A-like cells23,24. Besides TAS1R1-TAS1R3, also metabotropic glutamate receptors, present in the stomach and small intestine, can sense umami taste25. Peptone, an enzymatic digest from animal milk or protein mimicking dietary protein digests in the lumen, is likely sensed by the lysophosphatidic acid receptor 5 (LPAR5; also known as GPR92 and GPR93)26. Furthermore, free amino acids can be absorbed via various amino acid transporters with different group specificities whereas di- and tripeptides are taken up by the peptide transporter PepT127,28. Studies in Pept1−/− mice showed that PepT1 participates in the control of food intake in mice fed a high-protein diet28. Collectively, these data suggest that sensing of amino acids and protein hydrolysates by endocrine cells in the gut is finely tuned by different receptors and transporters that may play an important role in protein-induced satiety.
Recent studies showed that the ghrelin cell expresses TAS1R3, involved in sensing of sweet and umami, but also the free fatty acid receptor GPR120 and the gustatory G-proteins, α-gustducin and α-transducin, coupled to several taste receptors23,29,30. This study aimed to examine the role of specific amino acid taste receptors in the effect of peptone, a casein hydrolysate rich in peptides and amino acids and individual amino acids on ghrelin release in the ghrelinoma cell line. Since ghrelin cells exist as closed-type cells in the stomach, not reaching the epithelial surface, or opened-type cells in the small intestine, making contact to the lumen, we investigated whether the effect of peptone on ghrelin release differed in ex vivo segments from corpus and jejunum31. Finally, we examined whether amino acids are sensed via the lumen or bloodstream by comparing the effect of intragastric versus intravenous administration of peptone or L-Phe on ghrelin release in mice.
Results
In vitro studies in the ghrelinoma cell line
MGN3-1 cells release octanoyl ghrelin in response to a casein hydrolysate and L-amino acids
The effect of peptone and of different classes of amino acids on octanoyl ghrelin release was investigated in a ghrelinoma cell line, MGN3-1. Peptone stimulated octanoyl ghrelin release in a concentration-dependent manner with maximal effects at 3% (P = 0.01) and 5% peptone (P = 0.04) (Fig. 1a). The aromatic amino acids L-Phe and L-Trp stimulated octanoyl ghrelin release with 37 ± 6% (P = 0.000001) and 90 ± 18% (P = 0.00005) respectively (Fig. 1b). L-Phe increased ghrelin levels between 5 and 10 mM with no further increases up to 20 mM. Since natural proteins are exclusively built from L-amino acids and amino acid taste receptors are only selective for L-amino acids22,32, the effect of D-Phe was tested to determine the specificity of the observed effect. D-Phe was without effect up to 20 mM, indicating that the effect of L-Phe was indeed stereoselective (Fig. 1c). The aliphatic amino acid L-Ala 10 mM (P = 0.000007) and the sulphur- or hydroxyl-containing amino acids L-Met 10 mM (P = 0.002) and L-Thr 10 mM (P = 0.0098) significantly increased octanoyl ghrelin release. None of the other classes of amino acids (branched-chain, basic, acidic and amidic amino acids) were effective at 10 mM (Fig. 1b). Monosodium glutamate (MSG), known for its specific umami taste, increased octanoyl ghrelin release, compared to NaCl as control, in a concentration-dependent manner (P = 0.00001) without reaching a plateau at 40 mM (Fig. 1d). Application of a mixture of L-amino acids, mimicking the fasting levels of amino acids in human plasma, increased (P = 0.0009) octanoyl ghrelin release with 63 ± 14% (Fig. 1e).
Effect of peptone and amino acids on octanoyl ghrelin release in MGN3-1 cells.
(a) Concentration-dependent effect of a 3 h stimulation with peptone on octanoyl ghrelin release (n = 8). (b) Effect of amino acids from 7 different classes (10 mM) on octanoyl ghrelin release compared to the control stimulation (HEPES buffer) in each condition. (c) Stereoselective effect of L-Phe on octanoyl ghrelin release (n = 3–11). (d) Concentration-dependent effect of MSG on octanoyl ghrelin release compared to NaCl as control (n = 5–6). (e) Effect of an amino acid mixture (L-AA mix), mimicking the fasting levels of amino acids in human plasma, on octanoyl ghrelin release (n = 12) compared to HEPES buffer as control. *P < 0.05 vs. control; **P < 0.01 vs. control; ***P < 0.001 vs. control; ###P < 0.001 vs. D-Phe.
The effect of individual amino acids on octanoyl ghrelin release in the ghrelinoma cell line is mediated by different amino acid taste receptors
Real-time PCR studies showed that all three known amino acid taste receptors (CaSR, TAS1R1-TAS1R3 and GPRC6A) as well as the peptone receptor, LPAR5, were present in the ghrelinoma cell line although at different expression levels (see Supplementary Fig. S1). The role of these specific amino acid taste receptors in amino acid-induced octanoyl ghrelin release was evaluated for the 3 most potent amino acids (10 mM L-Phe, 10 mM L-Ala, 40 mM MSG) and for 3% peptone. L-Phe-induced octanoyl ghrelin release was significantly (treatment*antagonist P = 0.0004) decreased after preincubation of the cells with the CaSR antagonist, Calhex-231 (5 μM) (Fig. 2a). The TAS1R1-TAS1R3 antagonist, gurmarin and the GPRC6A antagonist, calindol, were without effect (Fig. 2c,e). The effect of L-Phe was mimicked by the CaSR agonist, cinacalcet (10 μM), which increased octanoyl ghrelin release from 5.99 ± 0.75 to 11.07 ± 2.18 pg/100,000 cells (P = 0.010). The effect of MSG on octanoyl ghrelin release was only reduced by the TAS1R1-TAS1R3 antagonist, gurmarin (30 μg/ml) (treatment*antagonist P = 0.045) (Fig. 2b,d,f). Both calhex-231 (treatment*antagonist P = 0.006) and gurmarin (treatment*antagonist P = 0.02), but not calindol, reduced the effect of L-Ala on octanoyl ghrelin release (Fig. 3a,c,e). Peptone-induced octanoyl ghrelin release involved both the CaSR (treatment*antagonist P = 0.0001) and the GPRC6A (treatment*antagonist P = 0.000006) but not TAS1R1-TAS1R3 (Fig. 3b,d,f).
Effect of amino acid taste receptor blockers on L-Phe- and MSG-induced octanoyl ghrelin release in MGN3-1 cells.
Effect of preincubation (30 min) of MGN3-1 cells with a (a,b) CaSR antagonist (calhex-213 5 μM) (n = 6–15), (c,d) GPRC6A antagonist (calindol 5 μM) (n = 9–12) or (e,f) TAS1R1-TAS1R3 antagonist (gurmarin 30 μg/ml) (n = 9) or their respective vehicle on the effect of (a,c,e) L-Phe 10 mM or (b,d,f) MSG 40 mM compared to HEPES buffer on octanoyl ghrelin release in MGN3-1 cells. **P < 0.01, ***P < 0.001 vs. vehicle or vehicle with antagonist; #P < 0.05, ###P < 0.001 in the absence vs. presence of antagonist.
Effect of amino acid taste receptor blockers on L-Ala- and peptone-induced octanoyl ghrelin release.
Effect of preincubation (30 min) of MGN3-1 cells with a (a,b) CaSR antagonist (calhex-213 5 μM) (n = 6–9), (c,d) GPRC6A antagonist (calindol 5 μM) (n = 9) or (e,f) TAS1R1-TAS1R3 antagonist (gurmarin 30 μg/ml) (n = 9) or their respective vehicle on the effect of (a,c,e) L-Ala 10 mM or (b,d,f) peptone 3% compared to HEPES buffer on octanoyl ghrelin release in the MGN3-1 cells. *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle or vehicle with antagonist; #P < 0.05, ##P < 0.01, ###P < 0.001 in the absence vs. presence of antagonist.
The intracellular Ca2+ signalling pathway is involved in MSG- and peptone-induced octanoyl ghrelin release in MGN3-1 cells
Acute administration of L-Ala (10 mM) or MSG (40 mM) stimulated intracellular Ca2+ release in MGN3-1 cells, while L-Phe was without effect at concentrations between 10 and 40 mM (see Supplementary Fig. S2). The acute effect of peptone on intracellular Ca2+ release could not be determined due to the inherent yellow colour of peptone which interfered with the fluorescence measurements. However, peptone-induced ghrelin release was blocked after incubation of MGN3-1 cells with the phospholipase C antagonist, U-73122 (10 μM) (treatment*antagonist P = 0.03) and the SERCA pump antagonist, thapsigargin (1 μM) (treatment*antagonist P = 0.00009) but not with the L-type Ca2+ channel antagonist, nifedipine (1 μM), thereby confirming a role for intracellular but not extracellular Ca2+ (Fig. 4a,c,e). Similar effects were observed with these blockers on MSG-induced ghrelin release (PLC antagonist: treatment*antagonist P = 0.04; SERCA pump blocker: treatment*antagonist P = 0.0004) (Fig. 4b,d,f).
Effect of Ca2+-signalling pathway antagonists on peptone- and MSG-induced octanoyl ghrelin release in MGN3-1 cells.
Effect of preincubation (30 min) of MGN3-1 cells with a (a,b) phospholipase C (PLC) antagonist (U-73122 10 μM) (n = 8), (c,d) SERCA pump antagonist (thapsigargin 1 μM) (n = 6) or (e,f) L-type Ca2+ channel antagonist (nifedipine 1 μM) (n = 6) or their respective vehicle on the effect of (a,c,e) peptone 3% or (b,d,f) MSG 40 mM compared to HEPES buffer on octanoyl ghrelin release in the MGN3-1 cells. *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle or vehicle with antagonist; #P < 0.05, ###P < 0.001 in the absence vs. presence of antagonist.
Ex vivo studies in intestinal segments
The effect of peptone on octanoyl ghrelin release differs between corpus and jejunum
Peptone caused a concentration-dependent increase in octanoyl ghrelin release in segments from the corpus, similar to the effects observed in the gastric ghrelinoma cell line. In contrast, octanoyl ghrelin release was significantly (P = 8·10−16) decreased after stimulation of jejunal segments with peptone. Furthermore, the jejunum was more sensitive to peptone since 1.5% peptone decreased octanoyl ghrelin release with 73 ± 4% (P = 0.0006), while in the corpus octanoyl ghrelin release was not yet maximal at 5% peptone (Fig. 5a,b). We hypothesized that the inhibitory effect of peptone on ghrelin release in the jejunum might represent a paracrine effect mediated via peptone-induced release of other hormones (CCK, GLP-1, somatostatin). The role of these three gut peptides in peptone-induced octanoyl ghrelin release was evaluated by pre-treating jejunal segments with a CCK1 receptor antagonist (devazepide 10 μM), a GLP-1 receptor antagonist (exendin 9-39 500 nM) or a somatostatin receptor antagonist (BIM-23627 10 μM). However, none of these gut peptide receptor antagonists could reverse the peptone-induced inhibition of octanoyl ghrelin release in the jejunum (Fig. 5c–e).
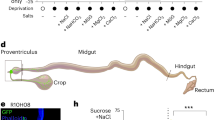
Concentration-dependent effect of peptone on octanoyl ghrelin release in gastric and jejunal mouse tissue segments.
Effect of a 2 h stimulation with increasing concentrations of peptone or vehicle (Krebs buffer) on octanoyl ghrelin release from tissue segments of (a) the corpus (n = 8–9) or (b) the jejunum (n = 3–12). Effect of preincubation (30 min) of jejunal tissue segments with a (c) CCK receptor antagonist (devazepide 10 μM) (n 5–6), (d) GLP-1 receptor antagonist (exendin (9–39) 500 nM) (n = 5–6) or (e) somatostatin receptor antagonist (BIM-23627 10 μM) (n = 5–6) or their respective vehicle on the effect of peptone 2% compared to Krebs buffer on octanoyl ghrelin release from jejunal segments. *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle or vehicle with antagonist.
In vivo studies in mice
Intragastric administration of peptone inhibits plasma ghrelin levels
Intragastric administration of 8% peptone decreased both octanoyl (P = 0.001) and total plasma ghrelin (P = 0.03) levels with 41 ± 4% and 22 ± 5% respectively (Fig. 6a,b). This was accompanied by a significant increase (P = 0.003) in octanoyl ghrelin content in stomach extracts, but not in duodenal extracts indicating that the inhibition of ghrelin release occurs at the level of the stomach (Fig. 6c–f).
The inhibition in plasma ghrelin levels after intragastric administration of peptone originates mainly from gastric ghrelin cells.
Effect of intragastric administration of 8% peptone on octanoyl and total ghrelin secretion. Mice were gavaged with 8% peptone (n = 6–8) or vehicle (water, n = 6–7). Octanoyl and total ghrelin levels were determined in (a,b) plasma, (c,d) protein extracts of the stomach and (e,f) duodenum 40 minutes after injection. *P < 0.05 vs. control; **P < 0.01 vs. control.
Sensing of L-Phe is not polarized
To determine whether L-Phe is sensed by the ghrelin cell in the stomach or duodenum via the lumen or whether amino acid uptake into the blood is required for mediating the effect on ghrelin release, the effect of intragastric versus intravenous administration of L-Phe (100 mM) on ghrelin release was compared. Intragastric administration of L-Phe significantly (P = 0.003) decreased total but not octanoyl plasma ghrelin levels compared to water-treated control mice (Fig. 7a,b). This was probably due to an inhibition of ghrelin release from the stomach since total ghrelin content in the stomach, but not in the duodenum, tended (P = 0.057) to be increased in L-Phe-treated compared to water-treated mice (Fig. 7c–f). Intravenous injection of L-Phe tended (P = 0.07) to decrease octanoyl plasma ghrelin levels and significantly (P = 0.048) decreased total plasma ghrelin levels. This effect was accompanied by an increase in octanoyl (P = 0.003) and total (P = 0.005) ghrelin content in duodenal but not in gastric tissue extracts (Fig. 8).
The inhibition in plasma ghrelin levels after intragastric administration of L-Phe originates from gastric ghrelin cells.
Effect of intragastric administration of L-Phe on the secretion of octanoyl and total ghrelin. Mice were gavaged with 100 mM L-Phe (n = 6–7) or vehicle (NaCl 0.9%, n = 6–7). Octanoyl and total ghrelin levels were determined in (a,b) plasma, (c,d) protein extracts of the stomach and (e,f) duodenum 40 minutes after injection. **P < 0.01 vs. control.
The inhibition in plasma ghrelin levels after intravenous administration of L-Phe originates from duodenal ghrelin cells.
Effect of intravenous injection of L-Phe on the secretion of octanoyl and total ghrelin. Mice were intravenously injected into the tail vene with 100 mM L-Phe (n = 9–12) or vehicle (NaCl 0.9%, n = 8–12). Octanoyl and total ghrelin levels were determined in (a,b) plasma, (c,d) protein extracts of the stomach and (e,f) protein extracts of the duodenum 40 minutes after injection. *P < 0.05 vs. control; **P < 0.01 vs. control.
Discussion
Our findings in the ghrelinoma cell line MGN3-1 provide for the first time evidence that peptone, umami and specific classes of amino acids (aromatic, aliphatic and sulphur- or hydroxyl-containing) are sensed by amino acid taste receptors (CaSR, GPRC6A, TAS1R1-TAS1R3 or a combination) on the gastric ghrelin cell and stimulate octanoyl ghrelin release. Ex vivo, the peptone-induced ghrelin release is mimicked in tissue segments from the mouse corpus, which contain closed-type ghrelin cells, but not from the jejunum, where sensing by open-type ghrelin cells results in an inhibition of ghrelin release. The latter effect is not mediated via an indirect paracrine effect of peptone on nearby GLP-1-, CCK- or somatostatin-containing endocrine cells but probably involves other downstream signalling pathways. In contrast to the in vitro and ex vivo (corpus tissue) data, intragastric administration of peptone led to a significant reduction in plasma ghrelin levels, originating from a reduced ghrelin release from the gastric but not duodenal ghrelin cells. These findings therefore suggest that in vivo an indirect mediator is overriding local nutrient sensing mechanisms. Finally, we observed that amino acid (L-Phe) sensing is not polarized and occurs both via the lumen and the blood stream.
In the first part of this study, we focused on the effect of a casein hydrolysate and of individual amino acids on ghrelin release in the ghrelinoma cell line. Of the 7 different classes of amino acids investigated, the aromatic amino acids (L-Phe and L-Trp), the aliphatic amino acid L-Ala and the sulphur- or hydroxyl-containing amino acids (L-Met and L-Thr) increased octanoyl ghrelin secretion at 10 mM. This concentration falls within the affinity range of amino acid taste receptors for their ligands and is in agreement with the the physiological concentration of free L-amino acids observed in the stomach 3 hours after food intake17,22,33,34. Umami stimuli (MSG) affected ghrelin release at higher concentrations (40 mM) and the effect of peptone was maximal at 3%. An amino acid mixture, emulating the fasting levels of amino acids in human plasma, increased octanoyl ghrelin release in MGN3-1 cells, which is in line with the observed increase in octanoyl ghrelin levels in humans during the fasting state17.
All putative amino acid taste receptors are expressed in the ghrelinoma cell line. GPRC6A, which is the most sensitive amino acid taste receptor with a binding affinity in the micromolar range32, is abundantly expressed whereas expression levels of the putative peptide-responsive receptor LPAR5 were very low. Our studies showed that sensing of L-Phe occurs via the CaSR, MSG via the TAS1R1-TAS1R3 while L-Ala and peptone act via 2 different amino acid taste receptors: CaSR & TAS1R1-TAS1R3 and CaSR & GPRC6A, respectively. The involvement of multiple receptors for amino acid sensing was demonstrated before both in the lingual epithelium and in the gut35,36. CCK secretion following L-Phe administration in mouse proximal small intestine segments involved both the CaSR and the TAS1R1-TAS1R335.
Until now, the CaSR is involved in L-Phe-induced release of four other gut peptides: gastrin and somatostatin in the stomach and CCK and GLP-1 in the small intestine. Studies in wildtype and CaSR−/− mice confirmed that the CaSR is mediating the effect of oral administration of L-Phe on gastrin release37. Immunohistochemistry studies showed that a small population of CaSR-containing cells in the antrum of human, mouse and pig also express somatostatin18. Two independent studies demonstrated that the CaSR is involved in sensing of L-Phe both in the CCK-producing enteroendocrine cell line, STC-1 and in native I-cells19,38. In humans, administration of L-Phe before a meal enhanced CCK secretion and decreased subsequent food intake39. Finally, perfusion of isolated loops of rat small intestine with L-Phe stimulated GLP-1 secretion via the CaSR40. The role of CaSR in the release of ghrelin is less straightforward. Engelstoft et al. (2013) observed a concentration-dependent decrease in octanoyl ghrelin release in primary gastric ghrelin cells after administration of R-568, an allosteric agonist of the CaSR in the presence of 1.8 mM CaCl2. Increasing the CaCl2 concentration to 4 mM shifted the effect of R-568 on ghrelin release from an inhibition to a stimulation41. In contrast, we showed an increase in octanoyl ghrelin release after stimulation with the calcimimetic agent cinacalcet in the presence of 1.8 mM CaCl2.
Both the CaSR and GPRC6A, known to be involved in amino acid-induced GLP-1 release from GLUTag cells, mediate the effect of peptone on ghrelin release42. The low expression level of the putative peptone receptor, LPAR5, did not allow us to perform reproducible and effective RNA silencing studies. Therefore the role of this receptor remains elusive.
Gurmarin, an inhibitor of the sweet taste receptor complex TAS1R2-TAS1R3, also inhibits sensing of TAS1R1-TAS1R3 through binding to the extracellular venus flytrap module of TAS1R3 leading to suppressed umami responses in taste buds43. Gurmarin partially reduced the increased octanoyl ghrelin secretion in response to MSG in the ghrelinoma cell line.
Our observation that both MSG and L-Ala activate a common taste receptor (TAS1R1-TAS1R3) is supported by studies in the lingual system and the finding that these 2 amino acids share perceptual qualities in rats44. In addition, L-Ala-induced ghrelin release is also mediated by the CaSR. Previous studies showed that L-Ala is sensed by the CaSR in HEK-293 cells expressing the human CaSR and in normal human parathyroid cells17,45.
The intracellular signalling pathways involved in amino acid sensing by specific taste receptors are mainly studied in the tongue (recently reviewed46,47) but similar studies in enteroendocrine cells are emerging. Intracellular Ca2+ mobilization plays a key role in amino acid sensing by GPRC6A in GLUTag cells and by CaSR in STC-1 cells leading to GLP-1 and CCK secretion, respectively38,42. In the present study, a role for the intracellular Ca2+ signalling pathway was revealed in the effect of L-Ala, MSG and peptone but not of L-Phe on ghrelin release. It is therefore likely that both TAS1R1-TAS1R3 and GPRC6A, involved in sensing of L-Ala and MSG, but not CaSR, mediating the effect of L-Phe, are predominantly Gαq-coupled. Studies in isolated primary ghrelin cells and in CaSR-transfected HEK-293 cells showed that CaSR has the potential for biased signalling and couples through both Gαq and Gαi41,48. At least in the ghrelinoma cell line, intracellular Ca2+ does not seem to be mobilized after activation of CaSR. It is therefore likely that CaSR is coupled to Gαs as has been reported for AtT-20 cells49.
In the second part of the study, the effect of peptone on ghrelin release was studied in gastric and jejunal segments, which represent a more integrated system. In addition this enabled us to compare whether the functional responses of the closed-type ghrelin cells in the stomach differ from the opened-type ghrelin cells that are in contact with the lumen in the small intestine31. Peptone induced a concentration-dependent increase in octanoyl ghrelin release from tissue segments of the corpus, thereby mimicking the observed effect in the ghrelinoma cell line, originating from a gastric ghrelin-producing tumour. In contrast, a concentration-dependent decrease in octanoyl ghrelin release was observed in jejunal segments. Since peptone is known to stimulate the release of gut peptide hormones CCK, GLP-1 and somatostatin, which can in turn inhibit ghrelin release, we hypothesized that the inhibitory effect of peptone on ghrelin release in jejunal segments was indirect and mediated via peptone-induced release of these gut hormones50,51,52. However, none of the receptor antagonists for these hormones could reverse the peptone-induced ghrelin inhibition. In line with our observations, GLP-1 or CCK did not induce octanoyl ghrelin release in isolated primary ghrelin cells which expressed the GLP-1 and both the CCK1 and CCK2 receptor41. Nevertheless, three out of five somatostatin receptors (SSTR1, SSTR2, SSTR3) are expressed at relatively high levels in primary ghrelin cells but somatostatin only reduced ghrelin secretion partially41. We speculate that other downstream signalling pathways are coupled to the taste receptors in the jejunum, resulting in inhibition of ghrelin release but future studies are necessary to elucidate these mechanisms.
Intragastric administration of 8% peptone in mice decreased plasma octanoyl and total ghrelin levels, which was due to an inhibition of octanoyl ghrelin release from the stomach. Indeed, in humans, others described a reduction in ghrelin release after a casein-rich meal53. These observations are in line with the physiological function of ghrelin as an orexigenic or meal initiating factor. In humans plasma ghrelin levels decrease after a meal, mimicked in the present study by peptone, to prevent further food intake and increase thereafter to dictate the timing of the next meal54. Nevertheless, these in vivo results are at variance with the increase in octanoyl ghrelin release in the ghrelinoma cell line and in the gastric mucosal segments after stimulation with peptone, suggesting that these local effects are overruled in vivo by an indirect mechanism. Our studies with jejunal segments together with the findings in primary gastric ghrelin cells argue against an important role of GLP-1, CCK or somatostatin.
It is still possible that the inhibition of gastric ghrelin release after intragastric administration with peptone originates from intestinal regions more distally from the stomach and the jejunum. A possible candidate is PYY, mainly secreted by the L-cells in the distal gut. Ullrich et al. (2015) showed that intraduodenal administration of a whey hydrolysate in humans led to reduced plasma ghrelin levels accompanied by an increase in PYY levels55. Although this suggests that PPY can function as a regulator of ghrelin secretion, Engelstoft et al. (2013) could not demonstrate the presence of the NPY1 or NPY2 receptor on isolated ghrelin cells41.
Knowing that ghrelin and insulin levels correlate inversely after intake of a protein-rich meal in humans and that a casein hydrolysate is able to stimulate insulin release, insulin is also a possible candidate for the direct inhibitory effect of peptone on ghrelin release56,57. The insulin receptor is expressed in the ghrelinoma cell line and in a primary culture of gastric ghrelin-secreting cells58,59. However the effects of insulin on ghrelin release in these cells are contradictory: two studies reported a decrease, while two other studies did not observe an effect58,59,60,61. We could also not confirm an effect of insulin on ghrelin release in the ghrelinoma cell line (data not shown). Moreover the observed peptone-induced decrease in octanoyl ghrelin release in the jejunal segments cannot be clarified by the effect of insulin.
A potential role for the enteric nervous system (ENS) or the vagus in the effect of amino acids on ghrelin release in vivo cannot be excluded. Amino acids/peptides might be sensed by the enteric nerve endings after absorption. It is known that the dipeptide receptor PEPT2 and amino acid receptors involved in glutamate and glycine sensing are present on enteric neurons62,63,64 which directly increase the excitability of the enteric neurons63,65,66. Perhaps more importantly, amino acids affect the synthesis and release of neurotransmitters that can initiate a neural reflex to affect ghrelin release. L-cysteine and L-arginine, for example, are substrates for enzymes involved in the synthesis of the enteric neurotransmitters, nitric oxide and hydrogen sulfide, respectively67. Uptake of L-tryptophan can increase the synthesis and release of serotonin since tryptophan hydroxylase 2 (TPH2), the enzyme responsible for the production of 5-HT, is produced by enteric neurons68.
In addition, administration of amino acids (L-Lysine and MSG) or a meat hydrolysate activate vagal afferent fibers, indicating that the vagus nerve is of importance to transfer peripheral information to the central nervous system after amino acid/peptide intake69,70,71,72. Several in vivo studies indicate that the fasting-induced increase in plasma ghrelin levels is mediated by both the cholinergic and adrenergic arms of the autonomic nervous system73. Although the presence of β1 adrenergic receptors has been confirmed on the ghrelin cell, acetylcholine fails to affect ghrelin release in MGN3-1 ghrelinoma cells or primary cultures from rat stomach58,74,75. However, further research is required to clarify the role of the ENS and vagus nerve in the effect of amino acids on ghrelin release.
Since amino acids can be absorbed via various apical amino acid transporters with certain group specificities, we determined whether L-Phe is sensed via the luminal or blood-born direction76. Both intragastric and intravenous administration of L-Phe significantly decreased plasma total ghrelin levels while the effect on octanoyl ghrelin release was less pronounced. Thus overall sensing of L-Phe is not polarized although the sensing in the different regions of the gut seems to be dependent upon the route of administration. The ghrelin content in the duodenum was significantly increased after intravenous administration whereas the ghrelin content in the stomach was significantly increased after intragastric administration. These findings highlight the complexity of the mechanisms in the postprandial effects of ghrelin.
In conclusion, amino acids and di-/tripeptides are sensed by various taste receptors on the ghrelin cells that stimulate a chemosensory signalling pathway regulating local ghrelin release which might be stimulatory or inhibitory depending on the region in the gut. In vivo, post-absorptive and indirect mechanisms, probably involving insulin or another signal, overrule these effects to shut down the release of ghrelin and hence hunger signalling.
Materials and Methods
Materials
All amino acids and peptone were obtained from Sigma (St. Louis, MO). The composition of the amino acid mixture mimicking the fasting levels of amino acids in human plasma17 (referred to as L-AA mix) was as follows (in μM): 50 L-Phe; 50 L-Trp; 80 L-His; 60 L-Tyr; 30 L-Cys; 300 L-Ala; 200 L-Thr; 50 L-Asn; 600 L-Gln; 125 L-Ser; 30 L-Glu; 250 L-Gly; 180 L-Pro; 250 L-Val; 30 L-Met; 10 L-Asp; 200 L-Lys; 100 L-Arg; 75 L-Ile; 150 L-Leu. The CaSR agonist, cinacalcet, was obtained from Biorbyt (cinacalcet hydrochloride, Biorbyt Ltd., Cambridge, United Kingdom). The CaSR antagonist, calhex-231 and the GPRC6A antagonist, calindol, were purchased from Santa Cruz Biotechnology (Santa Cruz Biotechnology, Inc., Dallas, Texas). All stock solutions were made in DMSO and further dilutions were made in HEPES buffer resulting in a final concentration of 0.1% DMSO (CaSR agonist), 0.01% DMSO (CaSR antagonist) and 0.01% DMSO (GPRC6A antagonist) during the cell experiment. Gurmarin was heterologously secreted using the yeast Pichia pastoris and subsequently purified as previously described77.
Mice
Male C57BL/6 WT mice were obtained from Janvier. All mice (11–12 weeks of age) were housed (20–22 °C) under a 14-h:10-h light-dark cycle and had ad libitum access to food and drinking water. All experimental procedures were approved and carried out in accordance to the regulations and guidelines of the Ethical committee for Animal Experiments of the KU Leuven (project number 048/2011).
Experimental design
Overnight-fasted mice were either gavaged with peptone 8%, L-Phe 100 mM or vehicle or injected intravenously (IV) into the tail vene with 100 mM L-Phe or vehicle. Forty minutes after IV injection or gavage, mice were sacrificed and blood was collected by cardiac puncture. The stomach and duodenum were removed and stored for protein extraction.
Ghrelin tissue extraction
Tissue from stomach and duodenum was boiled for 10 minutes followed by homogenization in 3 volumes of water with protease inhibitors (MP Biomedicals, Santa Ana, CA) and 9 volumes of 6% acetic acid. After 10 minutes of boiling, the homogenate was centrifuged to collect the supernatant which was diluted and subjected to radioimmunoassay (RIA). Protein levels were determined using the Pierce BCA Protein Assay Kit (Thermo Fisher Scientific Inc., Waltham, MA).
Ghrelin release from ghrelinoma cells
The ghrelinoma cell line, MGN3-1, was kindly provided by Prof. Hiroshi Iwakura (Kyoto University Hospital, Kyoto, Japan). Cells were cultured in Dulbecco’s modified eagle medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin and streptomycin at 5% CO2 and at 37 °C. Cells were incubated for 3 hours with the individual amino acids, L-AA mix, peptone or cinacalcet78 at the indicated concentration in HEPES buffer. The effect of specific amino acid taste receptor antagonists (calhex-231 5 μM40,79, calindol 5 μM42,80 or gurmarin 30 ng/mg35,77) and Ca2+ signalling pathway antagonists (U-73122 10 μM42,81, thapsigargin 1 μM58,82 or nifedipine 1 μM83) was investigated by preincubation of the cells during 30 minutes with the respective antagonist after which the culture medium was removed and replaced by a combination of the antagonist and an amino acid or peptone. Following 3 hours of incubation, the supernatant was collected, acidified (0.1M HCl) and stored at −80 °C.
Ghrelin release from intestinal segments
Overnight fasted mice were refed for 2 hours prior to being sacrificed. Segments of the intact corpus of the stomach (0.2 × 0.2 cm) and jejunum (0.2 × 0.5 cm) were dissected and incubated at 37 °C in Krebs buffer with the test solutions for 2 hours. The culture medium was collected, acidified (1M HCl) and stored at −80 °C for RIA. The role of GLP-1, CCK and somatostatin was investigated by preincubation of the intact jejunum (0.2 × 0.8 cm) during 30 minutes with the respective antagonist (exendin (9–39) 500 nM84,85, devazepide 10 μM86,87, BIM-23627 10 μM41,88) after which the culture medium was removed and replaced by a combination of the antagonist and peptone. Following 2 hours of incubation, the supernatant was collected, acidified (0.1 M HCl) and stored at −80 °C. Tissue segments were dried to correct the ghrelin release for dry tissue weight of the segment.
Radioimmunoassay (RIA)
Plasma samples and cell/tissue culture supernatants were extracted on a SEP-Pak C18 cartridge (Waters Corporation, Milford, MA), vacuum-dried and subjected to ghrelin RIA. The RIA was performed as previously described29.
Intracellular Ca2+ release experiments
MGN3-1 cells were loaded with 10 μM Fluo-4-AM (Molecular Probes, Life Technologies, Paisley, UK) at room temperature in HEPES buffer (pH 7.4) during 20 minutes. Changes in intracellular Ca2+ release [Ca2+]i were measured in a fluorescence reader (FLUOstar Omega, BMG Laboratories, Offenburg, Germany) at 520 nm and normalized to their initial baseline value recorded 1 min before the application of the test compound.
Quantitative real-time PCR
RNA was isolated from MGN3-1 cells using the Qiagen RNeasy kit (Qiagen, Hilden, Germany) and reversed transcribed to cDNA using Superscript II Reverse Transcriptase (Invitrogen, Carlsbad, CA, USA). Quantitative real-time PCR was performed as previously described89. Primer sequences were as follows: GAPDH: forward CCCCAATgTgTCCgTCgTg, reverse gCCTgCTTCACCACCTTCT; TAS1R1: forward CCCCTggCAgCTTCTTCAgCAg, reverse AggTCCATTCCAgTCCCAggCg; TAS1R3: forward CCCAACAgCATCCCgTgCAA, reverse CTCCACAgCCATCTTCATAgC; CaSR: forward ACCTgCTTACCCggAAgAgggCTTT, reverse AATTCAggTgCCgTAggTgTTTCAg; GPRC6A: forward gTgTTCgCCCTTggTCATgCCA, reverse CAgCACggCAAgTAgCTCCCATg; LPAR5: forward TCCACgCTggCTgTATATgg, reverse TCgCggTCCTgAATACTgTTC.
Statistical analysis
Results are presented as means ± SEM. Data were analysed using Statistica 12 (StatSoft Inc., Tulsa, OK, USA). Differences in octanoyl ghrelin release in the presence of individual amino acids/the amino acid mixture compared to the control stimulation in MGN3-1 cells and the difference between peptone-/L-Phe-treated mice and vehicle-treated mice in gavage and IV experiments were analysed with an unpaired Student’s t-test. All other data were analysed using a one- or two-way ANOVA (factors: treatment and antagonists). In case of a significant interaction effect or treatment effect, tests with contrasts were performed to locate pairs of factor levels with significant differences in the examined variables followed by post hoc Bonferroni testing. Significance was accepted at the 5% level.
Additional Information
How to cite this article: Vancleef, L. et al. Chemosensory signalling pathways involved in sensing of amino acids by the ghrelin cell. Sci. Rep. 5, 15725; doi: 10.1038/srep15725 (2015).
References
Sjostrom, L. et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N. Engl. J. Med. 357, 741–752 (2007).
Mingrone, G. et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N. Engl. J. Med. 366, 1577–1585 (2012).
Westerterp-Plantenga, M. S. The significance of protein in food intake and body weight regulation. Curr. Opin. Clin. Nutr. Metab. Care. 6, 635–638 (2003).
Larsen, T. M. et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N. Engl. J. Med. 363, 2102–2113 (2010).
Westerterp-Plantenga, M. S., Nieuwenhuizen, A., Tome, D., Soenen, S. & Westerterp, K. R. Dietary protein, weight loss and weight maintenance. Annu. Rev. Nutr. 29, 21–41 (2009).
Batterham, R. L. et al. Critical role for peptide YY in protein-mediated satiation and body-weight regulation. Cell Metab. 4, 223–233 (2006).
Lejeune, M. P., Westerterp, K. R., Adam, T. C., Luscombe-Marsh, N. D. & Westerterp-Plantenga, M. S. Ghrelin and glucagon-like peptide 1 concentrations, 24-h satiety and energy and substrate metabolism during a high-protein diet and measured in a respiration chamber. Am. J. Clin. Nutr. 83, 89–94 (2006).
Smeets, A. J., Soenen, S., Luscombe-Marsh, N. D., Ueland, O. & Westerterp-Plantenga, M. S. Energy expenditure, satiety and plasma ghrelin, glucagon-like peptide 1 and peptide tyrosine-tyrosine concentrations following a single high-protein lunch. J. Nutr. 138, 698–702 (2008).
Kojima, M. et al. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 402, 656–660 (1999).
Gutierrez, J. A. et al. Ghrelin octanoylation mediated by an orphan lipid transferase. Proc. Natl. Acad. Sci. USA 105, 6320–6325 (2008).
Yang, J., Brown, M. S., Liang, G., Grishin, N. V. & Goldstein, J. L. Identification of the acyltransferase that octanoylates ghrelin, an appetite-stimulating peptide hormone. Cell. 132, 387–396 (2008).
Depoortere, I. Targeting the ghrelin receptor to regulate food intake. Regul. Pept. 156, 13–23 (2009).
Avau, B., Carbone, F., Tack, J. & Depoortere, I. Ghrelin signaling in the gut, its physiological properties and therapeutic potential. Neurogastroenterol. Motil. 25, 720–732 (2013).
Verhulst, P. J. & Depoortere, I. Ghrelin’s second life: from appetite stimulator to glucose regulator. World J. Gastroenterol. 18, 3183–3195 (2012).
Janssen, S. & Depoortere, I. Nutrient sensing in the gut: new roads to therapeutics? Trends Endocrinol. Metab. 24, 92–100 (2013).
Depoortere, I. Taste receptors of the gut: emerging roles in health and disease. Gut. 63, 179–190 (2014).
Conigrave, A. D., Quinn, S. J. & Brown, E. M. L-amino acid sensing by the extracellular Ca2+-sensing receptor. Proc. Natl. Acad. Sci. USA 97, 4814–4819 (2000).
Haid, D. C., Jordan-Biegger, C., Widmayer, P. & Breer, H. Receptors responsive to protein breakdown products in g-cells and d-cells of mouse, swine and human. Front. Physiol. 3, 65 (2012).
Liou, A. P. et al. The extracellular calcium-sensing receptor is required for cholecystokinin secretion in response to L-phenylalanine in acutely isolated intestinal I cells. Am. J. Physiol. Gastrointest. Liver Physiol. 300, G538–546 (2011).
Wellendorph, P., Johansen, L. D. & Brauner-Osborne, H. Molecular pharmacology of promiscuous seven transmembrane receptors sensing organic nutrients. Mol. Pharmacol. 76, 453–465 (2009).
Li, X. et al. Human receptors for sweet and umami taste. Proc. Natl. Acad. Sci. USA 99, 4692–4696 (2002).
Nelson, G. et al. An amino-acid taste receptor. Nature. 416, 199–202 (2002).
Hass, N., Schwarzenbacher, K. & Breer, H. T1R3 is expressed in brush cells and ghrelin-producing cells of murine stomach. Cell Tissue Res. 339, 493–504 (2010).
Jang, H. J. et al. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc. Natl. Acad. Sci. USA 104, 15069–15074 (2007).
Akiba, Y., Watanabe, C., Mizumori, M. & Kaunitz, J. D. Luminal L-glutamate enhances duodenal mucosal defense mechanisms via multiple glutamate receptors in rats. Am. J. Physiol. Gastrointest. Liver Physiol. 297, G781–791 (2009).
Choi, S., Lee, M., Shiu, A. L., Yo, S. J. & Aponte, G. W. Identification of a protein hydrolysate responsive G protein-coupled receptor in enterocytes. Am. J. Physiol. Gastrointest. Liver Physiol. 292, G98–G112 (2007).
Hundal, H. S. & Taylor, P. M. Amino acid transceptors: gate keepers of nutrient exchange and regulators of nutrient signaling. Am. J. Physiol. Endocrinol. Metab. 296, E603–613 (2009).
Nassl, A. M., Rubio-Aliaga, I., Sailer, M. & Daniel, H. The intestinal peptide transporter PEPT1 is involved in food intake regulation in mice fed a high-protein diet. PLoS One. 6, e26407 (2011).
Janssen, S. et al. Bitter taste receptors and alpha-gustducin regulate the secretion of ghrelin with functional effects on food intake and gastric emptying. Proc. Natl. Acad. Sci. USA 108, 2094–2099 (2011).
Janssen, S., Laermans, J., Iwakura, H., Tack, J. & Depoortere, I. Sensing of fatty acids for octanoylation of ghrelin involves a gustatory G-protein. PLoS One. 7, e40168 (2012).
Sakata, I. et al. Ghrelin-producing cells exist as two types of cells, closed- and opened-type cells, in the rat gastrointestinal tract. Peptides. 23, 531–536 (2002).
Wellendorph, P. et al. Deorphanization of GPRC6A: a promiscuous L-alpha-amino acid receptor with preference for basic amino acids. Mol. Pharmacol. 67, 589–597 (2005).
Christiansen, B., Hansen, K. B., Wellendorph, P. & Brauner-Osborne, H. Pharmacological characterization of mouse GPRC6A, an L-alpha-amino-acid receptor modulated by divalent cations. Br. J. Pharmacol. 150, 798–807 (2007).
Adibi, S. A. & Mercer, D. W. Protein digestion in human intestine as reflected in luminal, mucosal and plasma amino acid concentrations after meals. J. Clin. Invest. 52, 1586–1594 (1973).
Daly, K. et al. Sensing of amino acids by the gut-expressed taste receptor T1R1-T1R3 stimulates CCK secretion. Am. J. Physiol. Gastrointest. Liver Physiol. 304, G271–282 (2013).
Yasumatsu, K. et al. Umami taste in mice uses multiple receptors and transduction pathways. J. Physiol. 590, 1155–1170 (2012).
Feng, J. et al. Calcium-sensing receptor is a physiologic multimodal chemosensor regulating gastric G-cell growth and gastrin secretion. Proc. Natl. Acad. Sci. USA 107, 17791–17796 (2010).
Hira, T., Nakajima, S., Eto, Y. & Hara, H. Calcium-sensing receptor mediates phenylalanine-induced cholecystokinin secretion in enteroendocrine STC-1 cells. FEBS J. 275, 4620–4626 (2008).
Ballinger, A. B. & Clark, M. L. L-phenylalanine releases cholecystokinin (CCK) and is associated with reduced food intake in humans: evidence for a physiological role of CCK in control of eating. Metabolism. 43, 735–738 (1994).
Mace, O. J., Schindler, M. & Patel, S. The regulation of K- and L-cell activity by GLUT2 and the calcium-sensing receptor CasR in rat small intestine. J. Physiol. 590, 2917–2936 (2012).
Engelstoft, M. S. et al. Seven transmembrane G protein-coupled receptor repertoire of gastric ghrelin cells. Mol. Metab. 2, 376–392 (2013).
Oya, M. et al. The G protein-coupled receptor family C group 6 subtype A (GPRC6A) receptor is involved in amino acid-induced glucagon-like peptide-1 secretion from GLUTag cells. J. Biol. Chem. 288, 4513–4521 (2013).
Sigoillot, M., Brockhoff, A., Meyerhof, W. & Briand, L. Sweet-taste-suppressing compounds: current knowledge and perspectives of application. Appl. Microbiol. Biotechnol. 96, 619–630 (2012).
Taylor-Burds, C. C., Westburg, A. M., Wifall, T. C. & Delay, E. R. Behavioral comparisons of the tastes of L-alanine and monosodium glutamate in rats. Chem. Senses. 29, 807–814 (2004).
Conigrave, A. D. et al. L-amino acids regulate parathyroid hormone secretion. J. Biol. Chem. 279, 38151–38159 (2004).
Brennan, S. C., Davies, T. S., Schepelmann, M. & Riccardi, D. Emerging roles of the extracellular calcium-sensing receptor in nutrient sensing: control of taste modulation and intestinal hormone secretion. Br. J. Nutr. 111 Suppl 1, S16–22 (2014).
Yasuo, T., Kusuhara, Y., Yasumatsu, K. & Ninomiya, Y. Multiple receptor systems for glutamate detection in the taste organ. Biol. Pharm. Bull. 31, 1833–1837 (2008).
Davey, A. E. et al. Positive and negative allosteric modulators promote biased signaling at the calcium-sensing receptor. Endocrinology. 153, 1232–1241 (2012).
Mamillapalli, R. & Wysolmerski, J. The calcium-sensing receptor couples to Galpha(s) and regulates PTHrP and ACTH secretion in pituitary cells. J. Endocrinol. 204, 287–297 (2010).
Calbet, J. A. & Holst, J. J. Gastric emptying, gastric secretion and enterogastrone response after administration of milk proteins or their peptide hydrolysates in humans. Eur. J. Nutr. 43, 127–139 (2004).
Chayvialle, J. A., Miyata, M., Rayford, P. L. & Thompson, J. C. Effects of test meal, intragastric nutrients and intraduodenal bile on plasma concentrations of immunoreactive somatostatin and vasoactive intestinal peptide in dogs. Gastroenterology. 79, 844–852 (1980).
Nakajima, S., Hira, T. & Hara, H. Calcium-sensing receptor mediates dietary peptide-induced CCK secretion in enteroendocrine STC-1 cells. Mol. Nutr. Food Res. 56, 753–760 (2012).
Veldhorst, M. A. et al. Dose-dependent satiating effect of whey relative to casein or soy. Physiol. Behav. 96, 675–682 (2009).
Cummings, D. E. et al. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 50, 1714–1719 (2001).
Ullrich, S. S. et al. Comparative effects of intraduodenal protein and lipid on ghrelin, peptide YY and leptin release in healthy men. Am. J. Physiol. Regul. Integr. Comp. Physiol. 308, R300–304 (2015).
Foster-Schubert, K. E. et al. Acyl and total ghrelin are suppressed strongly by ingested proteins, weakly by lipids and biphasically by carbohydrates. J. Clin. Endocrinol. Metab. 93, 1971–1979 (2008).
Jonker, J. T. et al. Effects of low doses of casein hydrolysate on post-challenge glucose and insulin levels. Eur. J. Intern. Med. 22, 245–248 (2011).
Gagnon, J. & Anini, Y. Insulin and norepinephrine regulate ghrelin secretion from a rat primary stomach cell culture. Endocrinology. 153, 3646–3656 (2012).
Iwakura, H. et al. Establishment of a novel ghrelin-producing cell line. Endocrinology. 151, 2940–2945 (2010).
Zhao, T. J. et al. Ghrelin O-acyltransferase (GOAT) is essential for growth hormone-mediated survival of calorie-restricted mice. Proc. Natl. Acad. Sci. USA 107, 7467–7472 (2010).
Sakata, I. et al. Glucose-mediated control of ghrelin release from primary cultures of gastric mucosal cells. Am. J. Physiol. Endocrinol. Metab. 302, E1300–1310 (2012).
Galligan, J. J. Ligand-gated ion channels in the enteric nervous system. Neurogastroenterol. Motil. 14, 611–623 (2002).
Neunlist, M. et al. Glycine activates myenteric neurones in adult guinea-pigs. J. Physiol. 536, 727–739 (2001).
Ruhl, A., Hoppe, S., Frey, I., Daniel, H. & Schemann, M. Functional expression of the peptide transporter PEPT2 in the mammalian enteric nervous system. J. Comp. Neurol. 490, 1–11 (2005).
Cherubini, E. & North, R. A. Actions of gamma-aminobutyric acid on neurones of guinea-pig myenteric plexus. Br. J. Pharmacol. 82, 93–100 (1984).
Liu, M. T., Rothstein, J. D., Gershon, M. D. & Kirchgessner, A. L. Glutamatergic enteric neurons. J. Neurosci. 17, 4764–4784 (1997).
Neunlist, M. & Schemann, M. Nutrient-induced changes in the phenotype and function of the enteric nervous system. J. Physiol. 592, 2959–2965 (2014).
Neal, K. B., Parry, L. J. & Bornstein, J. C. Strain-specific genetics, anatomy and function of enteric neural serotonergic pathways in inbred mice. J. Physiol. 587, 567–586 (2009).
Darcel, N. P., Liou, A. P., Tome, D. & Raybould, H. E. Activation of vagal afferents in the rat duodenum by protein digests requires PepT1. J. Nutr. 135, 1491–1495 (2005).
Jordi, J. et al. Specific amino acids inhibit food intake via the area postrema or vagal afferents. J. Physiol. 591, 5611–5621 (2013).
Niijima, A. Reflex effects of oral, gastrointestinal and hepatoportal glutamate sensors on vagal nerve activity. J. Nutr. 130, 971S–973S (2000).
Torii, K. & Niijima, A. Effect of lysine on afferent activity of the hepatic branch of the vagus nerve in normal and L-lysine-deficient rats. Physiol. Behav. 72, 685–690 (2001).
Muller, T. D. et al. Ghrelin. Mol. Metab. 4, 437–460 (2015).
Iwakura, H. et al. Oxytocin and dopamine stimulate ghrelin secretion by the ghrelin-producing cell line, MGN3-1 in vitro. Endocrinology. 152, 2619–2625 (2011).
Zhao, T. J. et al. Ghrelin secretion stimulated by {beta}1-adrenergic receptors in cultured ghrelinoma cells and in fasted mice. Proc. Natl. Acad. Sci. USA 107, 15868–15873 (2010).
Broer, S. Amino acid transport across mammalian intestinal and renal epithelia. Physiol. Rev. 88, 249–286 (2008).
Sigoillot, M. et al. Optimization of the production of gurmarin, a sweet-taste-suppressing protein, secreted by the methylotrophic yeast Pichia pastoris. Appl. Microbiol. Biotechnol. 96, 1253–1263 (2012).
Nemeth, E. F. et al. Pharmacodynamics of the type II calcimimetic compound cinacalcet HCl. J. Pharmacol. Exp. Ther. 308, 627–635 (2004).
Petrel, C. et al. Modeling and mutagenesis of the binding site of Calhex 231, a novel negative allosteric modulator of the extracellular Ca(2+)-sensing receptor. J. Biol. Chem. 278, 49487–49494 (2003).
Faure, H. et al. Molecular determinants of non-competitive antagonist binding to the mouse GPRC6A receptor. Cell calcium. 46, 323–332 (2009).
Bleasdale, J. E. et al. Selective inhibition of receptor-coupled phospholipase C-dependent processes in human platelets and polymorphonuclear neutrophils. J. Pharmacol. Exp. Ther. 255, 756–768 (1990).
Davidson, G. A. & Varhol, R. J. Kinetics of thapsigargin-Ca(2+)-ATPase (sarcoplasmic reticulum) interaction reveals a two-step binding mechanism and picomolar inhibition. J. Biol. Chem. 270, 11731–11734 (1995).
Young, S. H., Rey, O., Sternini, C. & Rozengurt, E. Amino acid sensing by enteroendocrine STC-1 cells: role of the Na+-coupled neutral amino acid transporter 2. Am. J. Physiol. Cell Physiol. 298, C1401–1413 (2010).
Granata, R. et al. Obestatin promotes survival of pancreatic beta-cells and human islets and induces expression of genes involved in the regulation of beta-cell mass and function. Diabetes. 57, 967–979 (2008).
Thorens, B. et al. Cloning and functional expression of the human islet GLP-1 receptor. Demonstration that exendin-4 is an agonist and exendin-(9-39) an antagonist of the receptor. Diabetes. 42, 1678–1682 (1993).
Carrillo, J., Agra, N., Fernandez, N., Pestana, A. & Alonso, J. Devazepide, a nonpeptide antagonist of CCK receptors, induces apoptosis and inhibits Ewing tumor growth. Anti-cancer drugs. 20, 527–533 (2009).
Chang, R. S. & Lotti, V. J. Biochemical and pharmacological characterization of an extremely potent and selective nonpeptide cholecystokinin antagonist. Proc. Natl. Acad. Sci. USA 83, 4923–4926 (1986).
Tulipano, G. et al. Characterization of new selective somatostatin receptor subtype-2 (sst2) antagonists, BIM-23627 and BIM-23454. Effects of BIM-23627 on GH release in anesthetized male rats after short-term high-dose dexamethasone treatment. Endocrinology. 143, 1218–1224 (2002).
Verhulst, P. J. et al. Role of ghrelin in the relationship between hyperphagia and accelerated gastric emptying in diabetic mice. Gastroenterology. 135, 1267–1276 (2008).
Acknowledgements
This work was supported by a Methusalem grant from the University of Leuven for research on “The Brain-Gut Axis in Health and Disease: from Mucosal Integrity to Cortical Processing”. Sandra Steensels is holder of a PhD grant from the Agency for Innovation by Science and Technology (IWT). The authors would like to thank Anneleen Geuzens and Linda Nys for their skilful technical assistance.
Author information
Authors and Affiliations
Contributions
J.T. and I.D. conceived and designed the experiments. L.V., T.V.D.B., T.T. and S.S. performed the experiments. L.B. contributed to the reagents tools. L.V., T.V.D.B., T.T. and I.D. analysed the results. L.V. and I.D. wrote the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Vancleef, L., Van Den Broeck, T., Thijs, T. et al. Chemosensory signalling pathways involved in sensing of amino acids by the ghrelin cell. Sci Rep 5, 15725 (2015). https://doi.org/10.1038/srep15725
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep15725
This article is cited by
-
Ghrelin Response to Acute and Chronic Exercise: Insights and Implications from a Systematic Review of the Literature
Sports Medicine (2021)
-
Therapeutic potential of ectopic olfactory and taste receptors
Nature Reviews Drug Discovery (2019)
-
Deregulation of transcription factors controlling intestinal epithelial cell differentiation; a predisposing factor for reduced enteroendocrine cell number in morbidly obese individuals
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.