Key Points
-
Suggests a general understanding of fixed retainers and space maintainers and their application is essential for patient safety as discussed in the paper.
-
Notes that fixed retainers require regular monitoring to ensure caries does not occur unnoticed, thus preventing catastrophic damage as shown.
-
Highlights that molar bands are used during orthodontic treatment, which if left unsupervised can cause excessive damage.
Abstract
Lingual arches are fixed space maintainers utilised for the preservation of leeway space in cases of mild mandibular crowding. They are normally bonded using glass-ionomer cement applied to the internal surface of molar bands. As with any fixed appliance/retainer, if molar bands are not sufficiently monitored they have the potential to pose a significant threat to an individual's dental health. Unconventionally, in our example a lingual arch was used as a long-term fixed retainer with harmful consequence to one of the banded first permanent molars. A general understanding of molar bands and fixed retainers is important for patients' general dental health by the prevention of discrete caries progression.
Similar content being viewed by others
Introduction
A lingual arch is a custom made, passive, fixed-space maintaining device composed of molar bands conventionally cemented onto the mandibular first permanent molar teeth. Stainless steel wire (usually 0.9 mm) is soldered to the lingual surface of these bands, and extends anteriorly following the arch shape onto the lingual surfaces of the lower incisors. It is used to prevent both the mesial movement of the banded molar teeth and lingual collapse of the lower incisors.1 By preventing these movements, a lingual arch can also be used to preserve the leeway space, avoiding or reducing the likelihood of requiring extractions in the treatment of mild crowding. Studies that have looked at the effects of lingual arches have shown that they are effective in reducing arch perimeter loss, but this is partly by mandibular incisor proclination.2
Case report
In the case that we present, a 13-year-old male initially attended his orthodontist with a marked Class II division I malocclusion, on a severe skeletal II base, with a significantly increased overjet at 13 mm. He was treated with a functional appliance for twelve months, had favourable growth, and then proceeded to have upper and lower fixed appliances on a non-extraction basis. His treatment was completed in two and a half years and the appliances were debonded when he was 16 years of age. He was provided with a Hawley retainer for the upper arch, and unconventionally a lingual arch in the lower arch. After a routine period of one year's supervised retention, he was discharged to the general care of his dentist.
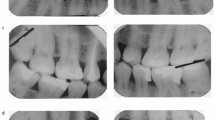
We first examined the patient ten years post removal of his fixed appliances, at the age of 26 years. He self-referred to our emergency department for the removal of the lingual arch due to pain and discomfort from his left mandibular first permanent molar (36). The band on this side was loose and a large cavity was evident where the disto-buccal cusp once was (Fig. 1). The lingual arch was carefully removed and the extent of the very large cavity evident.
A periapical radiograph taken to assess root morphology and apical pathology associated with 36 (Fig. 2) clearly demonstrates supra-crestal caries distally, and apical pathology associated with the distal root.
Unfortunately, irreversible pulpal damage had occurred necessitating root canal treatment for the tooth to be saved. This was carried out and the tooth restored in preparation for a lab-made coronal restoration for optimal coronal seal (Figs 3 and 4).
Discussion
Retention can be defined as 'the holding of teeth following orthodontic treatment in the treated position for the period of time necessary for the maintenance of the result,'3 be it via fixed or removable methods. The success of a retainer can be judged in relation to four different outcomes: survival of the retainer; assessment of tooth stability; adverse effects on oral health; and patient satisfaction. In our example, the fixed lingual arch had failed in one out of these four – adverse effects on oral health. The iatrogenic damage shown in this example was the result of unsupervised retention of an unconventional fixed retainer. It is now well accepted that long-term retention is the suggested method of maintaining alignment of teeth, however, it is very unusual to have a lingual arch incorporating molar bands acting as a long term fixed retainer, as per our example.
Orthodontic bands are normally cemented using a glass-ionomer cement (GIC) lute. The GIC is mixed so that the viscosity is low, enabling good flow around the circumference of the tooth for improved bonding and seal, whilst also reducing the risk of voids. The internal surface of bands are frequently sandblasted to further improve the bond strength. Some benefits of using GIC are its fluoride leaching properties and moisture tolerance, given the inherent moisture control difficulties associated with the mandibular molar teeth. The most significant risk of using a GIC lute, however, is the dissolution of the material prior to complete curing. This can create voids that are difficult to clean, within which food packs; if left untreated this can result in progressive decalcification (white spot lesions, advancing to brown spot lesions, followed by cavitation) with catastrophic consequences as our example demonstrates. Ten years ago when the lingual arch in our example was placed, GIC lute would still have been the material of choice for the cementation of bands; whilst it resiliently remained bonded on one side for this extended period of time, it failed on the other. When fitting bands, it is not a case of one size fits all. They are available in a multitude of sizes and the fit should be the tightest that still enables ideal positioning. If a poor size is selected, the band will inevitably work its way loose due to the biting pressures acting on it like a fulcrum. Loose bands are frequently unnoticed by the patient and can subsequently cause caries as discussed, or migrate apically causing irritation to the gingival sulcus and periodontal tissues with potential for acute periodontal infections. Due to these risks, it is important that the bands are reviewed regularly, as would be the case during a course of orthodontic fixed appliance treatment.
The prescription and placement of fixed retainers should only be performed with a fully informed patient and mostly in specific situations, as they have potential long term implications on oral health, such as periodontal disease and caries. There are many features of malocclusions with well-established indications for fixed retainers, such as the closure of midline diastemas, corrected rotations, or proclination of the labial segments for example. Contemporary fixed retainers are typically composed of a multi-strand stainless steel wire of 0.0175 inch diameter, or chain-link (dimension: height 0.0158 × width 0.0383 inches) of 14 karat white gold or stainless steel, that are bonded lingually to each tooth and allow physiologic mobility (Fig. 5). Composite resin is the bonding material of choice for conventional fixed retainers due to its high bond strength and ability to command cure. The small amount of mobility reduces the risk of attachments debonding as the teeth move naturally within the periodontal ligament. Debonded attachments (like voids with molar bands) create a food trap and an incredibly difficult site to clean, usually with the patient unaware allowing caries to progress unnoticed. For molar bands, the relatively short duration that they are in situ over the course of treatment with regular monitoring makes iatrogenic damage an easily preventable situation.
Conclusion
It is imperative that any appliance is regularly reviewed by a trained dental clinician. This is particularly important with fixed retainers and any appliance incorporating molar bands as they can hinder oral hygiene practice causing irreversible damage to the tooth crown, root and gingivae as discussed in this article.
For further scientific information on retention visit the following online Cochrane review article which included 15 randomised control studies: Littlewood S J et al. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev 2016; 25: CD0022834.
References
Gianelly A A . Leeway space and the resolution of crowding in the mixed dentition. Semin Orthod 1995; 1: 188–194.
Rebellato J, Lindauer S J, Rubenstein L K, Isaacson R J, Davidovitch M, Vroom K . Lower arch perimeter preservation using the lingual arch. Am J Orthod Dentofacial Orthop 1997; 112: 449–453.
Moyers R E . Handbook of orthodontics for the student and general practitioner, 3rd edition. Year Book Medical Publishers: Michigan, 1973.
Littlewood S J, Millett D T, Doubleday B, Bearn D R, Worthington H V . Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev 2016; 25: CD002283
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hemmings, N., Noar, J. Case report: long term lingual arch – preventable iatrogenic damage. Br Dent J 222, 19–20 (2017). https://doi.org/10.1038/sj.bdj.2017.24
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.24