Abstract
Aim To determine the prevalence of restoration overhangs in a general dental practice and investigate if these are associated with an increase in the rate of alveolar bone loss locally.
Methods Historical dental records were randomly and anonymously selected from the records of patients in a general dental practice. The most recent bitewing radiographs were examined and any overhangs were recorded along with location. Sequential bitewing radiographs were examined so that the restored tooth with an overhang could be compared over time with a similar but unrestored tooth which acted as a control.
Results A total of 111 dental records were audited and an overhang was observed in 67 cases. The prevalence of overhangs was greatest on upper molar teeth. Bone loss was calculated from 35 historical sets of bitewing radiographs over a period of up to 25 years. The mean bone loss on the unrestored control teeth was 0.06 mm/year and on the teeth adjacent to the overhangs it was 0.16 mm/year. This difference of 0.1 mm/year was statistically significant (paired t-test, P = 0.01). There was no significant difference between males and females. The mean size of the overhang was 0.9 mm (range 0.4-2.0 mm) with the bigger overhangs being associated with greater bone loss; however, not all ledges were associated in bone loss.
Conclusions Restoration overhangs can be associated with increased bone loss and larger overhangs may be most problematic, although other factors are involved as not all ledges caused bone loss.
Similar content being viewed by others
Key points
-
Suggests restoration ledges can significantly increase the rate of bone loss.
-
Highlights that ledges do not cause increased bone loss in all patients.
-
Argues consideration needs to be given to ledge removal or maximising oral hygiene measures while monitoring bone loss.
Introduction
Following placement of proximal restorations, access to the margins is usually limited; therefore, it is often difficult to place, check and modify or polish the interproximal margin. This can result in the production of a restoration overhang (Fig. 1) which has been defined as 'an extension of restorative material beyond the confines of a cavity preparation'.1 Prevalence is reported to be between 25% and 76% of restored surfaces.1 Overhangs may occur on any tooth surface although restorations involving the proximal surfaces of posterior teeth with concavities in the cervical area are particularly at risk.2 Techniques to limit overhangs with both indirect restorations and amalgam are well known and may be effective if well executed, although the risk of overhang increases where the restoration margin is subgingival.2,3 However, with an increasing move towards adhesive dentistry and increasing restrictions on the use of amalgam, the issue of eliminating overhangs in relation to composite resin restorations is more challenging. Where composite resin restorations are used in class II situations, there are difficulties with both contact tightness and the production of overhangs.4,5,6 Therefore, the prevalence of restoration overhangs may increase with wider adoption of composite resin restorations.
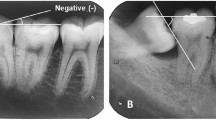
A case selected from the historical records in general practice. The bitewing radiographs were taken on the dates indicated. The overhangs at the 35 distal and the 36 distal can be observed and the adjacent bone level assessed. In this case there does not appear to be any associated bone loss: a) 1990; b) 1993; c) 1994; d) 1999; e) 2001
There is some evidence that the presence of a proximal restoration per se is sufficient to induce an inflammatory reaction in the adjacent periodontal tissues7,8 and that this effect is intensified when the restoration margin is placed subgingivally.9 Encroachment on the interproximal space by an overhang is thought to cause:
Local irritation of the gingiva and periodontal tissues
Plaque/debris retention
Reduced ability of the patient to clean the interproximal area
Changes in the periodontal microflora.
There is a need for longitudinal studies to monitor the impact of restoration overhangs on the surrounding tissues in order to guide clinicians as to the optimal treatment. Specifically, the decision to remove an overhang (accepting the risks such as tissue damage and cavity enlargement) or monitoring the overhang (with increased oral hygiene measures) should be guided by an evidence base.
Using measurements taken from serial, paralleling technique bitewing radiographs, this longitudinal analysis aims to describe the prevalence of restoration overhangs within a general practice population, and to evaluate the relationship between overhangs and changes in alveolar bone height over time.
Methods
An audit was planned using existing patient records. No patients were contacted or examined and the record analysis was carried out anonymously. The online NHS research tool indicated that this anonymous analysis of historical records did not require ethical approval. Clinical records of patients from a private general practice were randomly sampled by a person not involved in the study from the practice record storage room, and bitewing radiographs, where present, were examined for the presence of overhanging restoration margins. Records without bitewing radiographs were returned and further records were examined until sufficient records with bitewing radiographs were obtained. The initial analysis was aimed at determining the number and location of restoration overhangs from the historical records. The most recent bitewing radiographs were used from the dental records in each case. From this pool of records, a further analysis of suitable records was carried out to analyse bone levels over time.
Records were required to have readable pairs of bitewings of left and right sides of suitable angulation. From these records, the bitewings were assessed by one of the authors and required to have a restoration with an overhang on one tooth with an intact and unrestored similar tooth such as the same tooth on the other side of the arch. The total number of records analysed with suitable bitewing radiographs was 111 and these were used in the analysis to determine the prevalence and location of the overhangs.
The prevalence of overhanging restorations was recorded along with restoration site and restoration type. The only patient data recorded were gender and age at the time of sampling. From these records only those with sequential bitewing radiographs over time of readable quality were included in the analysis. This enabled the measurement of bone levels and any change over time. Sequential sets of bitewings were examined using a standard light box and 2.5 x magnification. Measurements were made by a single examiner using a digital calliper with a stated accuracy to 0.01 mm.
Alveolar bone height was measured at sites adjacent to overhanging restorations and at homologous sites which were either unrestored or satisfactorily restored (no overhang was identified). Points of reference were the most inferior part of the overhang for the subject tooth, and the cement-enamel junction (CEJ) or the most inferior part of the restoration for the control tooth. The bone level was determined to be the most superior point of the alveolar crest. A linear estimate of the horizontal extent of the overhang was also recorded. An example of a case with sequential bitewing radiographs is shown in Figure 1.
A repeatability analysis was carried out to ensure accuracy in the readings. For each case the bitewing radiograph was measured three times and the average was used in the calculations. The average difference in film measurements was 0.6% so the reliability was considered to be good.
Inclusion criteria
The inclusion criteria for the audit required the patient to be aged 18 years or older with an overhanging restoration visible on a bitewing radiograph. For the bone-level assessment, the inclusion criteria also required two or more sets of comparable film bitewing radiographs taken with a beam-aiming device, where there was a suitable control tooth with at least 2 mm of visible alveolar bone and no edentulous space adjacent to the overhanging restoration or control tooth.
The records were anonymised and an analysis was carried out once all the data had been collected. A comparison was made to measure the bone loss on the left and right sides. This enabled a direct comparison between the unrestored control tooth and the restored tooth with an overhang. The amount of bone loss on the overhang tooth and control tooth was compared using the student's t-test.
Results
A total of 111 patient records were randomly sampled. The sample comprised 42 males and 69 females. The average age at the time of sampling was 52.8 years (range 18-86). In these bitewing radiographs 98 teeth were restored and of those, 39 had radiographic evidence of a one or more restoration overhang (40%). The average number of overhangs per patient was 1.6 (range 1-5). The total number of overhangs identified in the 111 records was 67 involving 55 amalgam restorations and 12 crowns. No overhangs involving composite restorations were identified during this audit. Given these numbers an analysis of the type of restoration and the effect of this on bone level change was not possible.
The most common site for overhangs was the upper left first molar with eight (six distal, two mesial). Overall the most common site for overhangs was upper molars followed by lower molars then upper premolars and lastly lower premolars.
Bone-level assessment
The radiographs of 35 patients with 39 overhanging restorations and control teeth were assessed and 4 cases were excluded due to poor film quality. It is important to note that this was not a random sample because of the inclusion criteria. The average length of observation was 11.4 years (range 2-24 years, median 12 years).
Overhangs involving amalgam restorations were the most common (85%) with others being crowns. The average bone-level reduction per year for the subject and control teeth was calculated for each case and compared. The variance was similar; therefore, parametric analysis was conducted using student's t-test. Table 1 shows a summary of the data.
Based on the radiographic assessment, the average bone loss per year for the subject teeth was 0.16 mm (range 0.06-0.77 mm) while the average bone loss per year for the control teeth was 0.06 mm (range 0.025-0.33 mm). The average difference between the subject and control groups was 0.98 (confidence interval 0.092). The P-value was 0.01, indicating that the result was statistically significant. When comparing the rate of bone loss of male and female patients, no statistically significant difference was identified (p = 0.7).
The size of the overhang was measured as the distance of the furthest extent of the restoration ledge from the tooth surface, perpendicular to the long-axis of the tooth, at the base of the restoration. The average overhang width was 0.9 mm (range 0.4-2 mm). Figure 2 shows a case from the analysis comparing bone levels adjacent to an overhang and a control tooth. The chart in Figure 3 shows that the average difference in bone loss between the two groups increases with the size of the overhang.
In this case the historical records provided bitewing radiographs as shown above and were taken on the dates indicated. The restoration overhang being studied was the mesial overhang at the 47. The control site was the mesial surface of the 46. The mean change per year for the subject tooth with the overhang was 0.26 mm compared with 0.025 mm for the control tooth: a) 2001; b) 2005; c) 2006; d) 2009; e) 2012; f) 2013
The rate of bone loss adjacent to an overhang related to the size of the overhang. The control site showed little change in each case as expected. The chart shows the bone level change related to the size of the overhang: for an increased overhang size, towards the right of the chart the rate of bone loss per year is increased
Discussion
This study appears to be unique in that it examined bone loss in relation to overhangs from radiographs of patients in a general practice over a prolonged period. This enabled longitudinal bitewing radiographs to be retrospectively analysed. No patients were examined or contacted as part of this audit of historical dental records and so ethical approval was not required. The rate of bone loss calculated from the control teeth in this survey was 0.06 mm/year which compares with data from other studies such as 0.07 mm/year in a similar study of sequential radiographs on dental school patients.10 This similarity suggests that the population in this paper compares with other groups.
The prevalence of overhangs in the present study was 40% of proximal restorations. This shows that they are common findings on bitewing radiographs and compares with results from other studies, 25-76%1 and 50%,2 although the findings in the present audit may differ from contemporary practice as less amalgam is now in use. Use of composite resin may result in a different prevalence of overhangs. Furthermore, there is greater use of sectional bands, particularly with composite which could alter the cervical fit of the matrix.
The site of overhangs determined from this analysis indicated that upper molars have more overhangs than other teeth. This may be due to the more complex anatomy because of the root anatomy and position of the trifurcation in relation to the mesial and distal surfaces, unlike on the lower molars. It may also be that the marginal fit of the matrix band is more difficult to see and check for when restoring upper teeth.
The greater average rate of bone loss of 0.16 mm/year detected adjacent to the overhang suggests that the increased stagnation and impaired access for good oral hygiene results in increased plaque accumulation, leading to increased bone loss in susceptible patients. There may also represent a direct effect of the restorative material on the periodontal tissues. It was interesting to observe that not all ledges resulted in increased bone loss. This suggests that it is not the ledge that causes the bone loss directly and other factors are involved. This would include patient factors such as the susceptibility to periodontal bone loss. Nevertheless, larger overhangs typically resulted in more bone loss than smaller ledges. This may be due to the increased plaque accumulation. Given that the overhang size is relevant, this suggests that reducing the overhang would help reduce the rate of bone loss and also that complete overhang removal may not be essential. Sorensen et al.11 investigated crevicular fluid flow adjacent to interproximal subgingival marginal discrepancies of full coverage restorations. Small defects of <0.05 mm were associated with significantly less fluid flow and bone loss than larger defects. The present data is in agreement with this finding that overhang size is relevant.
When an overhang is detected then it may be appropriate to assess the patient and overall risk factors and susceptibility to periodontal bone loss. Leaving it unmonitored or a policy of removal of all overhangs may not be in the best interests of each individual patient. In some cases, where there is a known risk of bone loss, perhaps from longitudinal BPE scores or pocket charting from other sites within the mouth, a decision to remove the overhang may be best. This can sometimes be achieved by reducing the ledge with interproximal instruments including finishing strips, ultrasonic scaler tips, dental burs and special cutting tips held in a non-rotary, reciprocating handpiece.
The results of the present analysis indicate that even if the ledge is reduced and not entirely removed it may have a beneficial effect. Where there is no evidence of bone loss, an option is to optimise the oral hygiene and monitor the overhang and adjacent alveolar bone height over time. This could include flossing under the overhang or the use of suitably-sized interproximal cleaning brushes. Clearly, taking maximum care to avoid the creating of an overhang remains paramount. Somewhat in contrast to the opinions of prior researchers, the authors would argue that while overhangs and inflammation are undesirable, if the rate of bone loss is unlikely to compromise the lifespan of the tooth within an individual patient's lifetime, it allows operators to decide the merits of overhang removal, restoration replacement perhaps with repositioning of restoration margins, against leaving a restoration until it requires replacement due to failure by other means. It must be borne in mind that individual patient risk factors are not necessarily constant and should be reassessed at each examination.
It would seem prudent to remove larger overhangs (>1 mm) at the earliest opportunity, particularly in the molar regions where accelerated bone loss may lead to furcation involvement which has a significant impact on the progression of periodontal destruction.
Limitations of this study include errors due to the measurements taken from bitewing radiographs such as changes in the position of the radiograph and magnification effects. These, however, are likely to be less for bitewings than other intraoral radiographs and also as a paralleling device was in use. There will also be errors in taking measurements from radiographs. This was minimised by one operator carrying out all the measurements with a single technique under magnification. Verification and repeat measurements were carried out. However, there remains a risk of operator bias. Accurately and consistently measuring the vertical distances between the points of reference at the inferior surface of the restoration, the CEJ and the alveolar crest was challenging. All measurements were taken from analogue film with some inevitable variation in beam angulation from image to image due to the longitudinal nature of this analysis. Nowadays, film positioning and beam alignment devices are recommended,12 although a variation of ten degrees has been shown to have no effect.13 It is possible that with the shift towards digital imaging, digital subtraction comparison of images will improve image comparison and therefore the accuracy of measurements. No conclusions could be drawn regarding specific individual risk factors, such as smoking or a known diagnosis of periodontitis, from this analysis.
Conclusions
Restoration overhangs were most commonly observed on maxillary molars. Overhanging restorations were associated with increased bone loss, with larger overhangs (>1 mm) generally found to be most problematic. However, other factors are involved as not all ledges caused bone loss and significant variation was observed.
References
Brunsvold M A, Lane J J. The prevalence of overhanging dental restorations and their relationship to periodontal disease. J Clin Periodontol 1990; 17: 67-72.
Arneberg P, Sillness J, Nordbo H. Marginal fit and cervical extend of class II amalgam restorations related periodontal condition. J Periodontal Res 1980; 15: 669-677.
Leon A R. Amalgam restorations and periodontal disease. Br Dent J 1976; 140: 377-382.
Chuang S F, Su K C, Wang C H, Chang C H. Morphological analysis of proximal contacts in class II direct restorations with 3D image reconstruction. J Dent 2011; 39: 448-456.
Frankenberger R, Kramer N, Pelka M, Petschelt A. Internal adaptation and overhang formation of direct class II resin composite restorations. Clin Oral Investig 1999; 3: 208-215.
Loomans B A, Opdam N J, Roeters F J, Huysmans M C. Proximal marginal overhang of composite restorations in relation to placement technique of separation rings. Oper Dent 2012; 37: 21-27.
Broadbent JM, Williams K B, Thomson W M, Williams S M. Dental restorations: a risk factor for periodontal attachment loss? J Clin Periodontol 2006; 33: 803-810.
Pack A, Coxhead L J, McDonald B W. The prevalence of overhanging margins in posterior amalgam restorations and periodontal consequences. J Clin Periodontol 1990; 17: 145-152.
Reitemeier B, Hänsel K, Walter M H, Kastner C, Toutenburg H. Effect of posterior crown margin placement on gingival health. J Prosthet Dent 2002; 87: 167-172.
Rohner F, Cimasoni G, Vuagnat P. Longitudinal radiographical study on the rate of alveolar bone loss in patients of a dental school. J Clin Periodontol 1983; 10: 643-651.
Sorensen S E, Larsen I B, Jörgensen K D. Gingival and alveolar bone reaction to marginal fit of subgingival crown margins. Scand J Dent Res 1986; 94: 109-114.
Potter B J, Shrout M K, Harrell J C. Reproducibility of beam alignment using different bite-wing radiographic techniques. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79: 532-535.
Shrout M K, Hildebolt C F, Vannier M W. The effect of alignment errors on bitewing-based bone loss measurements. J Clin Periodontol 1991; 18: 708-712.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Millar, B., Blake, K. The influence of overhanging restoration margins on interproximal alveolar bone levels in general dental practice. Br Dent J 227, 223–227 (2019). https://doi.org/10.1038/s41415-019-0530-1
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0530-1
This article is cited by
-
Sectional matrix solutions: the distorted truth
British Dental Journal (2021)