Key Points
-
Outlines a staged approach to endodontic access through extensively restored teeth.
-
Outlines a staged approach in removing gutta-percha from obturated root canals
-
Familiarises practitioners to Gates Glidden burs, Hedstrom files, K-files and endodontic solvents and the design features that make them ideal for gutta-percha removal.
Abstract
Endodontic retreatment can be a challenging task that can result in many complications if not approached cautiously. Many of these difficulties revolve around regaining access to the pulp chamber through extensive coronal restorations and removing residual root filling material, the commonest being gutta-percha (GP), from within obturated canals. This can often be an untidy, time consuming process that places teeth at a greater risk of iatrogenic injury and inhibits the operator achieving the necessary chemical disinfection required to eliminate the persistent apical disease. Therefore the following article aims to aid practitioners, particularly those who are unfamiliar, with accessing and removing GP from endodontically treated teeth. The outlined systematic approach is accessible in general practice, where the vast majority of endodontic treatment is conducted, requires basic equipment and with the correct experience can be applied to both straight and curved canals. By overcoming this initial stage of retreatment, subsequent chemical disinfection, which is critical to success, can be carried out to a higher standard reducing risks of re-infection.
Similar content being viewed by others
Introduction
The Restorative Index of Treatment Need (RIOTN) recognises endodontic retreatment as being in a higher category of complexity than primary endodontic therapy.1 This is reflected by reduced success rates in some but not all studies, and that achieving a predictable outcome can be challenging by even experienced practitioners.2 The demanding process of regaining access through extensive coronal restorations and debriding the contents of obturated root canals, the commonest filling being gutta-percha (GP), certainly contribute to this difficulty.3,4 It can be an untidy and time consuming process that places teeth at a greater risk of iatrogenic injury and inhibits thorough chemical disinfection.
Therefore, the following article aims to aid practitioners, particularly those who are unfamiliar, in accessing and removing GP from endodontically treated teeth. The outlined systematic approach is accessible in general practice, where the vast majority of endodontic treatment is conducted, requires basic equipment and with the correct experience can be applied to both straight and curved canals. By overcoming this initial stage of retreatment, subsequent chemical disinfection, which is critical to success, can be carried out to a higher standard reducing risks of re-infection.
Indications for retreatment
The aim of non-surgical endodontic retreatment is to relieve patient symptoms and re-establish healthy periapical tissues following failure of initial therapy by removing materials from the root canal space, chemically disinfecting canals and if present, addressing deficiencies of pathological or iatrogenic origin.5 It is indicated in teeth with radiological findings of persisting apical periodontitis, with or without symptoms, in the presence of an inadequate root filling or coronal seal.6 Additionally, if the initial obturation permits coronal leakage (that is, voids), elective retreatment may be necessary before non-vital bleaching to minimise risks of root resorption.6,7
The associated complications are similar to those of primary endodontic therapy, however, reinfection can still persist if GP is not adequately removed as it presents a barrier to chemical disinfection.2 Teeth are also more vulnerable to iatrogenic injuries such as perforation, file separation or irreversible damage to a coronal restoration the patient has become accustomed to.2 It is therefore important to discuss these details with the patient in order to gain informed consent.8
Persistent apical infections
Intra-radicular sources
GP length and condensation, although giving no information on previously employed irrigant regimes, hold prognostic values and are considered features that help determine if initial treatment was completed to a satisfactory standard.6,9Root fillings that are poorly condensed or do not extend to the apex can still harbour residual bacteria that escaped initial chemo-mechanical debridement.10 This lack of disinfection, which is critical to success, tends to be the commonest cause of persistent apical disease following initial root therapy.10
Apical periodontitis can still persist even after thorough debridement and satisfactory obturation, while those completed to poorer standards can have outcomes greater than expected.11 This phenomenon has been directly associated with the quality of the coronal seal, which is consistently demonstrated to be a prognostic factor in both primary and secondary root treatment.2,9,10,11,12 The evidence demonstrates robust coronal restorations, which prevent oral bacterial and salivary ingress, can lead to favourable endodontic outcomes regardless of the obturation quality.11 If compromised, the endodontic space may become re-contaminated via sealer dissolution and salivary percolation resulting in a new infection.12
If apical disease persists in the presence of a reliable coronal seal and adequate obturation, resistant microorganisms may occupy the canal space. The most common is the gram positive, facultative anaerobic coccus, E. Faecalis.13,14 Its ability to survive in extreme conditions and poor nutrient environments, resist medications and irrigants and adhere to dentinal collagen makes it difficult to remove from within the canal using conventional disinfection regimes.13
Extra-radicular sources
Extrusions of root filling material into periapical tissues reduces the prognosis of endodontic treatment.2,15 The short term toxic nature of root canal sealers is commonly implicated however; this toxicity generally reduces after the setting reaction has completed.16,17 It is more likely that aggressive instrumentation, associated with over filling, transports infected debris into the peri-radicular tissues where displaced microbes proliferate and impair healing following thorough chemical disinfection.15 On rare occasions extra-radicular microorganisms that evade host defences induce persistent apical infections.18 Actinomyces spp. and Propionibacterium species have been found to be the most prevalent in root treated teeth and contribute to the formation of impenetrable extra-radicular biofilms.18
In these circumstances the inability of retreatment to overcome peri-radicular biofilms, extruded filling materials or resistant extra-radicular microorganisms would result in failure while peri-radicular surgery would be a more viable option.
Pre-treatment evaluation
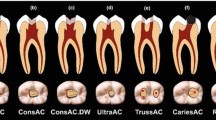
Evaluating difficulty in access
The ease of gaining access to the GP needs to be clinically and radiographically evaluated. Initially, the type and quality of the coronal restoration should be carefully examined.19 A robust coronal seal will inherently make it difficult to gain access to the pulp chamber, and extra-coronal or large intra-coronal restorations, particularly cores, can make it difficult to orient the bur correctly due to significant loss of natural anatomical landmarks. These restorations can often create a crown-root malalignment and obscure underlying pathology warranting complete coronal disassembly and thorough clinical and radiographic evaluation of tooth anatomy.20
The presence of posts significantly increases risk of iatrogenic injury (that is, vertical root fractures and perforations) rendering teeth unrestorable.19,20,21Discussion on the types of posts and their removal is outside the scope of this article but more than often a referral is required.
Evaluating difficulty of GP removal
On radiographic examination, the standard of the primary root filling needs to be evaluated with particular attention paid to the condensation and length.6,10,19 In the experience of the authors, GP is easier to retrieve when obturation is completed to a technically poorer standard, a common occurrence, than when it is well-condensed and to the appropriate length.22,23 This may be because voids allow instruments to pass more easily into the canal and GP that is not to length means there is less overall filling to remove. However, in well-obturated canals, a second opinion should be sought for the need of a retrograde approach.
Iatrogenic injuries created during primary root treatment such as ledges, separated files and perforations, as well as atypical and curved root morphology, impede instruments removing GP. The image enhancing tools of digital radiographic systems can aid in detecting these complications at lower doses, however, it is important to be wary of their presence throughout retreatment if nothing abnormal is detected on initial assessment.24
Case selection
The authors recommend that unfamiliar practitioners select case-appropriate teeth to begin with (that is, straight canals with no intra-pulpal obstructions) and refer to more experienced colleagues appropriately. The RIOTN may be a useful tool to help determine the complexity of treatment and make this decision (Table 1).1
Gaining access
An ideal access cavity provides for a stable coronal seal, maintains a reservoir of irrigants, allows good visibility and facilitates straight line access to each orifice.4,6,25 These principles still apply throughout endodontic retreatment and so any prior coronal pathology needs to be stabilised, defective restorations replaced and the tooth made ready for isolation.4
The operator will need to pre-operatively decide whether to access through the existing restoration or replace it entirely. Accessing through crowns may be justified with sound margins and no posts, however, complete coronal disassembly is often favoured as it is more accurate to assess overall restorability and underlying caries and cracks.4,20 Cooled fine diamond burs are useful to cut through ceramic and tungsten carbide burs for cast metal.25 If the crown is to be preserved, copious water spray is essential to prevent porcelain fractures, however, patients should still have prior warning that existing restorations may need replacing.25
Upon stabilisation, the occlusal position of the access cavity should be determined by examining tooth morphology.25 Attention needs to be paid to the cemento-enamel junction (CEJ) as Krasner and Rankow found this to be the most consistently reliable anatomical landmark to occlusally determine the position of the pulp chamber.25,26 Their 'Law of Centrality' dictates the chamber lies in the centre of this imaginary circumference at the level of the CEJ (Fig. 1[A]).26 It is therefore advised to examine the perimeter of the tooth on this plane with a Williams probe, keeping a mental note of its occlusal position. The access cavity should then be created centrally within this circumference and the 'Law of Concentricity' employed to ensure its dimensions mimic that of the external tooth surface at the height of the CEJ and not the occlusal surface (Fig. 1[B]).26 The operator may find this position to be significantly different to what would have been dictated by the artificial occlusal topography in a tooth that is extensively restored, rotated or angulated.25,26
The appropriate angulation and depth now needs to be established by aligning the bur parallel to the long axis of the tooth and radiographically measuring the distance between the point of access and the floor of the pulp chamber. The operator must be mindful that in the presence of core restorations, the bur does not characteristically drop into the pulp chamber but instead directly meets the floor. Therefore, gentle pressure should be applied for each stroke of the bur, followed by careful inspection under magnification and illumination to avoid furcal perforation. The 'Law of Colour Change' can help identify when the bur has reached the correct distance as the pulpal floor appears darker than the surrounding restoration (Fig. 1[C]).26 The use of round ended burs are advised to avoid forming ledges and when the restoration-pulp floor interface has been breached, a safe ended bur can then be used for lateral cutting. Rubber dam placement can also be delayed until entering the pulp chamber to aid bur orientation.4
When at the pulp floor the 'Laws of Orifice Location' can guide exploration and discovery of treated and overlooked root canals, keeping in mind orifices are located at the vertices of the floor-wall junction (Fig. 1[D & E]).26 When one canal is located, the remainder can be traced using the anatomical map located on the floor of the pulp chamber and in mandibular molars, the 'Laws of Symmetry' (Fig. 2).26 In cases where there is loss of anatomy, through former overzealous use of burs, appropriate magnification and illumination can help locate the orifice. Obturated canals, which are more visible due to the bright orange colour of the GP, should be identified first.
With a robust coronal seal, accurate occlusal positioning and correct bur alignment, access to the initial root filling can be conservatively gained. Krasner and Rankows' laws of access, that primarily apply to untreated teeth, can also be a useful guide for achieving this during retreatment cases (Table 2).26
Removing gutta-percha
Step 1: Gross coronal GP removal
Upon achieving straight line access, a sequence of Gates Glidden (GG) burs should be used to remove the core trunk of GP from within the coronal one to two thirds of root canals, depending on curvature, under rubber dam. The bur's blunted tip and lateral cutting design of the elliptical shaped head make it a safe and time efficient instrument for GP removal (Fig. 3).27 However unlike their nickel-titanium counterparts, the steel is more rigid and prone to fracture on flexion, limiting use to straight segments of the canal.27,28 Although separation is almost always at the latch end of the bur, excessive torsional forces can still cause fractures further down the shank.27,28 Fortunately, these burs are relatively inexpensive and they are manufactured in six different sizes of increasing diameters and lengths in either stainless or carbon steel, the latter of which fractures more readily.28 For this stage it is recommended stainless steel GG3–4 burs are used in narrow canals and GG4–5 in wider canals.
A pre-operative radiograph should be used to calculate the estimated working length (EWL) of the GP in only the straight segment of the obturated root canal (Fig. 4a). This length should not exceed the bend in curved canals or apical third in straight canals. With the GG set to this measurement, the tip of the bur should then be rested directly above the centre of the orifice with the shank oriented parallel to the long axis of the respective root (Fig. 4b). At this stage no apical pressure is necessary as frictional heat generated from the bur, rotating at full speed, plasticises the GP. Simultaneously, the weight of the hand-piece 'alone' passively engages the cutting flutes into the root filling causing the bur to migrate apically into the canal, removing GP along its path.25 Further apical pressure may be necessary when GP is well-condensed or 'in' canals that have been mechanically underprepared. This additional pressure should be very gentle to prevent ledge formation, perforation or file separation and if upon application resistance is felt while being short of the desired length, withdraw and reassess root morphology and bur angulation.
The lateral cutting action of the flutes creates significant debris and often condenses GP laterally against canal walls (Fig. 4c). These remnants can be picked away using a DG16 endodontic probe and then removed through frequent irrigation and circumferential brushing strokes of the GG to leave an unobstructed straight path to the apical segment of the GP (Figs 4d and 4e).
Step 2: Gross apical GP removal
Stainless steel Hedstrom files should now be used to retrieve the remaining core trunk of GP from within the apical segment of the root canal. Their use, although time consuming, produces less residual debris than contemporary rotary techniques.29,30The screw like cutting flutes, machined from round blanks, are angled at almost 90 degrees to the long axis with a 2% taper giving them a vertical cutting action during longitudinal filing motions that is ideal for retrieving GP (Fig. 5).31 Inappropriate rotary motions are discouraged as the file's relatively reduced cross sectional diameter decreases its torsional limit increasing risks of separation.31,32Additionally, the machining process can lead to significant variations in efficacy between different Hedstrom brands and therefore, only International Standards Organisation (ISO) approved files are recommended.31
Set all instruments to the EWL of the full GP length and not the whole root canal. Increasing this measurement to 0.5–1 mm beyond the radiographic apex can help remove overextended fillings averting the need for a retrograde approach.33 To create an initial glide path for the Hedstrom file, a sequence of ISO Kfiles should be used in a quarter turning motion. The inability of GP to form a hermetic seal within the canal often assists this process (Fig. 6a).34 The subsequent longitudinal space, which exists laterally between the canal walls and root filling, should be expanded to an ISO size 25 to reduce risks of file fracture during GP removal. A sufficiently sized Hedstrom, that resists bending (that is, ISO size ≥25), can then be engaged into the glide path by applying adequate apical pressure during a longitudinal stroke (Fig. 6b). The operator may notice increasing resistance to insertion and if unable to reach within 2 mm of the EWL with an ISO size 25, the glide path may need to be re-established.
When at the correct length, the Hedstrom should be tilted approximately 30 degrees away from the root filling and simultaneously withdrawn under resistance (Fig. 6c). Altering the path of withdrawal in this manner intimately engages the cutting flutes into the GP, providing greater retention for its displacement and eventual extraction. If the file readily releases a larger size may be required and vice versa. It may take several attempts with a gradually increasing sequence of Hedstrom files to achieve this. In most cases this apical segment can be quickly removed as one complete unit, however, if the GP has been exposed to light or air for long periods of time, it can become brittle making retrieval more fragmented.35
Upon removing the apical segment, the tip of the GP should be inspected for a rounded appearance which would signify retrieval of the master apical cone and progression to the next stage (Fig. 6d). However, if there is an irregular terminal appearance or tactile feedback within the canal indicates otherwise, further instrumentation may be required. In wider canals with stubborn GP it can sometimes be useful to braid two Hedstrom files gently around the GP point. Usually ISO sizes 15 and 20 work well for this process; however, caution is needed to prevent separation (Fig. 7).
Step 3: Fine GP removal
Although irrigation removes gross debris throughout retrieval, fine GP remnants often remain particularly in the apical third of curved canals.29,36 Endodontic solvents can be a useful option to dissolve, shrink and retrieve this residual debris if it is otherwise difficult to remove mechanically. Fortunately GP is soluble to a wide range of organic solvents including chloroform, tetrachloroethylene, xylene, halothane and eucalyptol, turpentine and orange oils.37 Solvents are best reserved for this stage as use during gross removal frequently leads to inconvenient residues of GP painted across the length of the canal walls.
Over the years, chloroform has been the solvent of choice due to its ability to rapidly dissolve GP into a thin liquid, however, there has been renewed interest to find alternatives due to its potential carcinogenic properties.38,39,40,41 Additionally, the hepatotoxic side effects of halothane deters its use also, and the failure of turpentine oils to dissolve GP at room temperatures make it impractical for chair-side application.42,43 Of the remaining, tetrachloroethylene, xylene and eucalyptol, and orange oils have shown to be the most biocompatible while also possessing useful solvency properties at 37°C.41 Unfortunately, the lack of a standard research model makes it difficult to conclude superiority, with current studies producing conflicting results. However, the most recognisable may be the tetrachloroethylene solvent, which is commercially available as EndosolvE.
A side vented 27 gauge needle should be placed passively into the canal to deliver solvent into each root canal. A flushing action is advised as repeated irrigation and aspiration creates turbulent pressures that promote removal of filling materials. Additionally, the volume deposited should saturate the root canal up to the floor of the pulp chamber. The solvent should then be agitated using hand files and the largest fitting paper points inserted into the canal to absorb the now dissolved root filling material (Fig. 8a). Upon withdrawal, the presence of residual GP will be clearly indicated by an orange shade on the tip of the soaked paper point. This 'wicking' should be repeated circumferentially until no further discolouration is witnessed in the presence of a saturated canal (Fig. 8b).
Additional markers of completion include gaining apical patency using pre-curved ISO size 6–8 Kfiles. This will allow the operator to attain a zero reading with an electric apex locator, establish a glide path for shaping and facilitate chemo-mechanical disinfection.44 Common obstructions can be a result of residual GP, debris plugs, ledge formation or file separation which would require a combination of mechanical (that is, pre-curving files, ultrasonics) and chemical means (that is, solvents, chelating agents and lubricants) to overcome with magnification.
Subsequently, the remainder of the root canal should be reshaped using the preferred preparation technique, thoroughly disinfected and then obturated after a penultimate rinse of 17% ethylenediaminetetraacetic acid (EDTA) followed by NaOCl.45 This irrigant regime has been demonstrated to improve periapical healing in retreatment cases with a possible explanation being that it removes the remaining smear layer, containing infected organic and inorganic matter, solvents and filling material that is created throughout endodontic retreatment.45
Conclusion
The strategy proposed above is one of many that aim to aid practitioners in overcoming difficult aspects of retreatment which often revolve around gaining access and removing old GP. Other methods of GP removal include the Protaper D series, reciprocating file systems and the use of heat. However, it is important to note that the subsequent chemical disinfection with NaOCl is the key stage that eliminates and prevents further infection and it is the adequate GP removal that facilitates this process.
References
Falcon H C, Richardson P, Shaw M J, Bulman J S, Smith B G N . Restorative dentistry: Developing an index of restorative dental treatment need. Br Dent J 2001; 190: 479–486.
Ng YL, Mann V, Gulabivala K . Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J 2008; 41: 1026–1046.
Carrotte P . Endodontics: Part 5 Basic instruments and materials for root canal treatment. Br Dent J 2004; 197: 479–486.
Carrotte P . Endodontics: Part 6 Rubber dam and access cavities. Br Dent J 2004; 197: 527–534.
Ruddle C J . Ch. 25, Nonsurgical endodontic retreatment. In Cohen S, Burns RC (eds) Pathways of the Pulp. 8th ed. 875–929. Elsevier: Mosby, St. Louis, 2002.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921–930.
Zimmerli B, Jeger F, Lussi A . Bleaching of nonvital teeth. A clinically relevant literature review. Schweiz Monatsschr Zahnmed 2010; 120: 306–320.
Main B G, Adair R L . The changing face of informed consent. Br Dent J 2015; 219: 325–327.
Ng Y L, Mann V, Rahbaran S, Lewsey J, Gulabivala K . Outcome of primary root canal treatment: systematic review of the literature Part 2. Influence of clinical factors. Int Endod J 2008; 41: 6–31.
Siqueira J F . Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J 2001; 34: 1–10.
Gillen B M, Looney S W, Gu L S et al. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod 2011; 37: 895–902.
Siqueira J F Jr, Rôças I N, Lopes H P, Uzeda M . Coronal leakage of two root canal sealers containing calcium hydroxide after exposure to human saliva. J Endod 1999; 25: 14–16.
Love R M . Enterococcus faecalisa mechanism for its role in endodontic failure. Int Endod J 2001; 34: 399–405.
Gopikrishna A V, Kandaswamy D, Jeyavel R K . Comparative evaluation of the antimicrobial efficacy of five endodontic root canal sealers against Enterococcus faecalis and Candida albicans. J Conserv Dent 2006; 9: 2–12.
Yusuf H . The significance of the presence of foreign material periapically as a cause of failure of root treatment. Oral Surg Oral Med Oral Pathol 1982; 54: 566–574.
Lodiene G, Morisbak E, Bruzell E, Ørstavik D . Toxicity evaluation of root canal sealers in vitro. Int Endod J 2008; 41: 72–77.
Barbosa S V, Araki K, Spangberg L S W . Cytotoxicity of some modified root canal sealers and their leachable components. Oral Surg, Oral Med, Oral Pathol, Oral Radiol, Endod 1993; 75: 357–361.
Wang J, Jiang Y, Chen W, Zhu C, Liang J . Bacterial flora and extraradicular biofilm associated with the apical segment of teeth with post-treatment apical periodontitis. J Endod 2012; 38: 954–959.
Tait C M E, Ricketts D N J, Higgins A J . Restoration of the root-filled tooth: pre-operative assessment. Br Dent J 2005; 198: 395–404.
Abbott P V . Assessing restored teeth with pulp and periapical diseases for the presence of cracks, caries and marginal breakdown. Aust Dent J 2004; 49: 33–39.
Tsesis I, Fuss Z . Diagnosis and treatment of accidental root perforations. Endod Top 2006; 13: 95–107.
Filippo G D, Sidhu S K, Chong B S . Apical periodontitis and the technical quality of root canal treatment in an adult sub-population in London Br Dent J 2014; 216: E22.
Lynch CD, Burke FM . Quality of root canal fillings performed by undergraduate dental students on single-rooted teeth. Eur J Dent Educ 2006; 10: 67–72.
Van Der Stelt PF . Better imaging: the advantages of digital radiography. J Am Dent Assoc 2008; 139: 7S13S.
Patel S, Rhodes J . A practical guide to endodontic access cavity preparation in molar teeth. Br Dent J 2007; 203: 133–140.
Krasner P, Rankow H J . Anatomy of the pulp chamber floor. J Endod 2004; 30: 5.
Hülsmann M, Stotz S . Efficacy, cleaning ability and safety of different devices for gutta-percha removal in root canal retreatment. Int Endod J 1997; 30: 227–233.
Lausten L L, Luebke N H, Brantley W A . Bending and metallurgical properties of rotary endodontic instruments. IV. Gates Glidden and Peeso drills. J Endod 1993; 19: 440–447.
Reddy N, Admala SR, Dinapadu S, Pasari S, Reddy MP, Rao MS . Comparative analysis of efficacy and cleaning ability of hand and rotary devices for gutta-percha removal in root canal retreatment: an in vitro study. J Contemp Dent Pract 2013; 14: 635–643.
Yürüker S, Görduysus M, Küçükkaya S et al. Efficacy of Combined Use of Different Nickel-Titanium Files on Removing Root Canal Filling Materials. J Endod 2016; 42: 487–492.
D'Souza J E, Walton R E, Maixner D . Cross-sectional configuration of endodontic files compared with manufacturers' design. J Endod 1995; 21: 599–602.
Walton R E, Torabinejad M . Principles and practice of endodontics. 4th edition. Philadelphia: Saunders; 2008.
Metzger Z, Ben-Amar A . Removal of overextended gutta-percha root canal fillings in endodontic failure cases. J Endod 1995; 21: 287–288.
American Association of Endodontists. Obturation of Root Canal Systems. Available online at https://www.aae.org/uploadedfiles/publications_and_research/endodontics_colleagues_for_excellence_newsletter/fall09ecfe.pdf (accessed June 2016).
Wong M, Peters D D, Lorton L, Bernier W E . Comparison of gutta-percha filling techniques: three chloroformguttapercha filling techniques, part 2. J Endod 1982; 8: 4–9.
Friedman S, Moshonov J, Trope. Efficacy of removing glass ionomer cement, zinc oxide eugenol, and epoxy resin sealers from retreated root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1992; 73: 609–612.
Wong R . Conventional endodontic failure and retreatment. Dent Clin N Am 2004; 48: 265–289.
Tamse A, Unger U, Metzger Z, Rosenberg M . Gutta percha solvents a comparative study. J Endod 1986; 12: 337–339.
Whitworth J M, Boursin E M . Dissolution of root canal sealer cements in volatile solvents. Int Endod J 2000; 33:: 19–24.
Schafer E, Zandbiglari T . A comparison of the effectiveness of chloroform and eucalyptus oil in dissolving root canal sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 611–616.
Wourms J D, Campbell A D, Hicks M L, Pelleu G B . Alternative solvents to chloroform for gutta-percha removal. J Endod 1990; 16: 224–226.
Chutich M J, Kaminski EJ, Miller DA, Lautenschlager EP Risk assessment of the toxicity of solvents of gutta-percha used in endodontic retreatment. J Endod. 1998; 24: 213–216.
Kaplowitz G J . Effect of temperature on rectified turpentine oil as a gutta-percha solvent. J Endod 1994; 20: 173.
Souza R A . The importance of apical patency and cleaning of the apical foramen on root canal preparation. Braz Dent J 2006; 17: 6–9.
Mann V, Gulabivala K . A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011; 44: 583–609.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Virdee, S., Thomas, M. A practitioner's guide to gutta-percha removal during endodontic retreatment. Br Dent J 222, 251–257 (2017). https://doi.org/10.1038/sj.bdj.2017.166
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.166