Key Points
-
Describes evidence to only performing invasive procedures where justified.
-
Increasing the fiscal and temporal efficiency of procedures by removing unnecessary steps.
-
Provides clarity and reducing risks using complete, consistent and coherent history taking.
-
Provides improved patient care and pain management through effective history taking.
Abstract
Objective To evaluate the current practice of pre-oral surgery haematological investigation in patients with disclosed regular and prolonged high alcohol consumption above the national recommendation for coagulopathy due to potential alcohol induced liver impairment.
Design Retrospective analysis of data.
Setting University of Bristol Dental Hospital, United Kingdom, 2013.
Subjects Adults (over 16 years old) with a reported high alcohol intake with no history of non-alcohol-related liver impairment or pre-existing coagulopathy.
Main outcome measures Alcohol and bleeding history recorded, haematology test requested with results and actions for abnormal results.
Results From a sample size of 58 patients, 75.9% of cases had their alcohol intake recorded; only 10.3% of cases had the duration of drinking recorded. Bleeding history was recorded in 82.9% of cases to which 6.9% of cases had a positive bleeding history. The most common combination of tests requested was full blood count, coagulation screen and liver function test. In 46.6% of cases, results were out of range – in all cases but 1, the patients abnormal haematology results were not followed up further.
Conclusion It was found that 1.7% of cases met the locally agreed standard (from best available evidence) that haematology requests, including full blood count and coagulation screen, should only be undertaken in those with disclosed high alcohol intake and positive bleeding history. A consistent bleeding history and alcohol intake should always be documented thoroughly.
Similar content being viewed by others
Introduction and background
Concerns over coagulation occurs for practitioners when patients attending University of Bristol Dental Hospital for invasive oral surgery procedures, such as a soft tissue biopsy or dental extraction under local anaesthesia, report an alcohol consumption that is above the national daily recommendation for their sex demographic. These patients will usually have the following pre-operative haematology tests performed in an attempt to exclude any coagulopathy caused by alcohol-induced liver impairment that might predict an increased risk of bleeding: FBC (Full Blood Count), LFT (Liver Function Test) and CS (Coagulation Screen). The bloods will be sent urgently if the procedure is to be performed on the same day.
The haemorrhage potential for dental extractions is considered as low because non vital organs are involved, it is an open procedure, there is limited surgical dissection and local haemostatic measures are likely to be effective.1,2
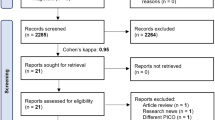
Following a literature search of AMED, EMBASE, HMIC, MEDLINE, BNI, CINAHL and the COCHRANE library, (using the search criteria 'alcohol*', 'oral*' and 'dent*'), there were minimal evidence-based guidelines found for the management of this group of dental patients specifically. There are, however, non-dental related guidelines available.
NICE (National Institute for Health and Care Excellence)3 found that over 24% of the English adult population consume alcohol in a way that is potentially or actually harmful to their health or well-being. The Department of Health recommends that men and women should drink no more than 21 and 14 units per week respectively. The NHS identifies those at high risk of developing serious types of alcohol liver disease as: men and women who drink more than 35 and 28 units of alcohol a week respectively for 10 years or more. One unit of alcohol is defined as containing 8 g of ethanol. One unit is typically half a pint of beer or lager, a 25 ml measure of spirit, and half a small glass of wine (87.5 ml).
The parameter in a full blood count which is relevant to alcohol-induced impaired coagulation is the platelet count. Platelets' role in coagulation is to maintain haemostasis. Chronic alcoholism can cause thrombocytopenia (low platelet numbers) and thrombocytopathy (impaired platelet function). A full blood count will identify thrombocytopenia but not thrombocytopathy. Alcohol-related thrombocytopenia is generally transient and platelet counts usually return to normal range within one week of abstinence.4
MCV (mean corpuscular volume) in a full blood count increases (macrocytosis) within 4–8 weeks of the onset of heavy drinking. However, although it may be an indicator of excessive alcohol consumption, it is not related to coagulation. Usually, it returns to normal range within 2 to 4 months of abstinence.4
Similarly, the parameters in a liver function test may exhibit change in excessive alcohol consumption but this does not determine coagulopathy. The parameters included in a coagulation screen are: PT (Prothrombin Time), INR (International Normalised Ratio), APTT (Activated Partial Thromboplastin time) and APPT ratio.
PT measures the extrinsic and common pathway of coagulation. The associated clotting factors decrease first in liver disease. In alcoholic liver disease, PT can be prolonged due to reduced synthesis of coagulation proteins. INR is calculated from PT. However, INR is used to monitor patients taking vitamin K antagonists such as warfarin. In patients with alcohol-induced liver disease, the changes to vitamin K dependant and vitamin K independent clotting factors vary differently. APTT measures the intrinsic and common pathway of coagulation. APTT usually remains normal in mild liver disease but can be prolonged as liver disease progresses. An increase in APTT may indicate underlying coagulopathy. It is often only when clotting factor levels fall by 60–70% from normal do the coagulation tests not remain normal.5
The British Committee for Standards in Haematology6 found that coagulation tests have considerable limitations due to the physiology of coagulation being complex and in vitro laboratory tests that require the addition of varying exogenous reagents with differing sensitivities cannot accurately reproduce the in vivo haemostatic response. Erroneous results can be caused by sample collection, such as prolonged tourniquet placement, difficult or traumatic phlebotomy, lack of adequate sample volume and prolonged storage. Interestingly, the guideline also found that postoperative bleeding rates in patients both with and without a prolonged clotting time were similar and that 30–95% of unexpected results from screening tests were not documented or pursued further.
Although not relating to coagulopathy specifically, both NICE guideline (CG115)3 and the SIGN (Scottish Intercollegiate Guidelines Network) guideline (no. 74)6 give guidance on haematology tests in harmful alcohol misuse. They recommend blood tests for monitoring an established alcohol-related problem, but not for routine screening. They found that biochemical markers are neither sensitive nor specific for diagnosing an alcohol problem. NICE found that simple biological measures such as liver function tests are poor indicators of the presence of harmful or dependent drinking.
It is important to note that in patients with alcoholic liver disease, coagulation screens do not always predict bleeding risk.7,8 Therefore, it is most important to document a thorough bleeding history. If there is a clear bleeding history in this group of patients, then a CS and FBC may be warranted.
It was therefore locally agreed as a standard and protocol that in this group of patients, alcohol, and bleeding history should be thoroughly documented, and only if the patient has a positive bleeding history should a FBC and CS be undertaken.
Objectives
To evaluate the current procedure of pre-oral surgery haematology investigations for patients who disclose a high alcohol intake (above the national recommendation), at the University of Bristol Dental Hospital, against the locally agreed standard by retrospectively assessing information recorded in patients' notes.
Method
Approval was sought from the clinical effectiveness audit committee to assess current practice against the agreed local standard and protocol. The electronic test request system was accessed to retrospectively identify all patients where one or a combination of FBC/LFT/CS tests had been requested for patients who consumed over the recommended alcohol allowance and were to have an oral surgery procedure. The period covered was 39 months as this was when the electronic request system was implemented in the hospital. Patients with non-alcohol-related liver impairment, medical histories associated to pre-existing coagulopathy or other non-alcohol-related reasons for haematological tests were excluded from the data. All patients were over 16 years of age.
The following information was collected:
gender, alcohol intake and duration of intake, bleeding history, any pre-existing alcohol-related liver disease, treatment required, the type of haematology test requested, why the tests were requested, the test results and if any action was required to achieve haemostasis. If the haematology results were abnormal, information was obtained on if any action was taken or if the patient was followed up.
Results
Over a period of 39 months, 58 patients had haematology tests undertaken due to reported high alcohol intake. In 84.5% (49/58) of cases the patients were male.
The majority of patients required routine dental extractions (range 1–18 teeth), two patients required a planned surgical dental extraction and two patients required a soft tissue biopsy. Operator level ranged from undergraduate students under supervision to specialist staff who all used the same local anaesthetic and haemostatic agents if required.
In 75.9% (44/58) of cases alcohol intake was recorded (range 10–231 units per week) with the duration of drinking being recorded in 10.3% (6/58) of cases. Bleeding history was recorded in 82.8% (48/58) of cases and 8.3% (4/48) of these cases had a positive bleeding history. Therefore, 93.1% (54/58) of cases had haematology tests regardless of bleeding history.
The most common combination of tests requested was FBC/LFT/CS (70.7%). Other combinations of tests included: FBC/CS, FBC/CS/LFT/INR, FBC/CS/LFT/Haematinics, FBC/CS/INR, and FBC/LFT/INR.
In those with a positive bleeding history, 25% (1/4) of cases had a CS and FBC undertaken. The other three cases had FBC/LFT/CS. No patients with a positive bleeding history had abnormal haematology results that would indicate coagulopathy.
In 27/58 of cases (46.6%), results were out of range. In all cases apart from one, no follow-up arrangement was made. It was also noted that there was a lack of documentation regarding whether or not patients had been informed of their results.
No patients had platelet counts below 50 × 109/L. 10.3% (6/58) had platelet counts below 150 × 109/L, of which two cases were below 100 × 109/L. Of these six cases, three had pack and suture as a precautionary measure, and three had no intervention. No adverse events were reported.
One patient did experience a postoperative bleed which required pack and suture of the socket along with biting on tranexamic acid-soaked gauze to achieve haemostasis. This patient required extraction of four teeth, drank up to 60 units per week, had no positive bleeding history and no abnormal haematology results that would indicate coagulopathy.
Discussion
It is important that a consistent medical and social history be undertaken. Alcohol intake was widely recorded in the patient's notes – however, there was a lack of detail and consistency to the recordings. Measurements of alcohol were recorded in litres/bottles/cans/pints/units – which can vary depending on the type of alcohol being consumed and the size of bottles/cans. Measurements were recorded either per day or per week. The duration of drinking is important to identify risks of developing serious types of alcoholic liver disease and because alcohol-related thrombocytopenia is generally transient where platelet counts usually return to normal within one week of abstinence.3 However, 87.9% (51/58) of cases had not had the duration of drinking recorded. Therefore, if a patient gives a previous history of short-term, high alcohol intake and does not have a diagnosed liver impairment or bleeding history, there may not be an indication to undertake haematology tests.
In 8.6% (5/58) of cases, the recorded alcohol intake was below the maximum weekly recommended alcohol intake for their sex demographic and there was no other reason documented for the investigations apart from alcohol intake. Therefore, these cases underwent unnecessary haematology investigations. This may be due to practitioners not knowing what the recommended maximum weekly alcohol intake is.
A thorough bleeding history is very important and should always be documented due to all oral surgery procedures carrying a bleeding risk – especially in those with reported high alcohol intake. The results showed that there was little documentation of details regarding bleeding history, such as family history, bruising easily and post-traumatic/postsurgical bleeding. It is important that practitioners always undertake a consistent medical and social history and be able to assess the importance of individual questions. Performing phlebotomy on a patient where a positive bleeding history has not been identified can be considered as an unnecessary invasive procedure and causes loss of time to the patient. Resources and practitioner time could also be better allocated.
The dental notes were accompanied by a medical and social history sheet, which included a basic alcohol history and bleeding disorder question. These sheets are thorough and work well to get an accurate medical history and act as a prompt to the practitioner to ask further questions regarding alcohol history or bleeding if required. However, these sheets were often not used by practitioners or were used but not followed up with further alcohol or bleeding related questions. A bleeding history may have been undertaken verbally within this process but as it was not documented there is no evidence that it was undertaken. Examples of questions regarding bleeding history can be found in Table 1.
In a non-hospital setting, patients are often given a medical and social history form to fill out themselves. The form usually asks for units of alcohol intake per week but not the duration of intake. Patients may not always fill this out as they may not think it is relevant towards dental treatment, may not wish to disclose their intake (especially if it's at a high level) or do not know what a unit is and how to work out how much they drink. If the practitioner does not pursue the question, or ask further questions regarding bleeding, this is left unanswered and is a potential risk to the patient.
There was a wide range of haematology requests. NICE guideline CG115 found that simple biological measures, such as liver function tests, are poor indicators of the presence of harmful or dependent drinking. Therefore, with regards to screening for impaired coagulation prior to an oral surgery procedure, a LFT is of little value. If LFTs were taken to screen for alcohol-induced liver disease, then abnormal results should be followed up. In 25.9% (15/58) of cases, LFTs were out of range. However, none of these cases were followed up.
In 3.4% (2/58) of cases the platelet levels were below 100 × 109/L (both were above 50 × 109/L which is the minimum blood platelet level required before an oral surgery procedure).9 These two patients both proceeded to undergo dental extractions with precautionary pack and suture and there was no adverse post-operative hemorrhage reported. Although the patients' medical histories did not indicate an alternative cause for thrombocytopenia apart from high alcohol consumption, it is important that the patients are referred to be followed up by a medical professional to address the thrombocytopenia and examine for other possible undiagnosed causes of thrombocytopenia.
The total costs of materials and processing of blood samples, not including time to the patient and staff members, was 20 times more than that which was actually required over 39 months. This was because 54/58 cases did not require any tests to be undertaken and there were only four patients with reported high alcohol intake who had a positive bleeding history that would have warranted a FBC and CS.
It is important to remember that often commonly a patient attends requiring a dental extraction due to acute dental pain. Thus, in examples of where the protocol has not been followed the patients who did not disclose a positive bleeding history underwent unnecessary investigations, thereby prolonging the time that the patient is experiencing acute pain. Therefore, with consistent medical and social history taking, we should able to identify those without a positive bleeding history as not requiring further investigations and focus on our primary concern on managing the patients' acute dental pain. Our secondary concern of postoperative bleeding in this group of patients, should it occur, can be managed with local haemostatic measures which are likely to be effective due to the haemorrhage potential of the procedure being low.
Conclusion
It is important for practitioners involved in invasive procedures, which involve a bleeding risk, to be familiar with the recommended maximum weekly alcohol intake. Alcohol intake should be documented in units per week and duration of intake. Focus should be placed on consistent medical and social history taking. Although haematology tests have a range of limitations, a FBC and CS may be warranted if there is a positive bleeding history. A LFT is not required as it will not be able to indicate coagulopathy. Any abnormal results should be followed up with the patient's general medical practitioner or onward referral to haematology. From the results of this audit, haematological investigations for patients who exceed the recommended weekly alcohol intake, in the absence of a positive bleeding history, are not indicated. If prolonged bleeding occurs, this can be successfully managed with local haemostatic measures.
References
Francis C W, Kaplan K L . Hematologic problems in the surgical patient: Bleeding and thrombosis. In Hoffman R, Benz E J, Shattil S et al. (ed) Hematology: basic principles and practice. 3rd ed. pp 2381. New York: Churchill Livingstone, 2000.
Seligsohn U, Coller B . Classification, clinical manifestations and evaluation of disorders of hemostasis. In Beutler E, Lichtman M A, Coller B S et al. (ed) Williams' hematology. 6th ed. pp 1471. New York: McGraw-Hill, 2001.
National Institute for Health and Care Excellence. Alcohol dependence and harmful alcohol use]. [CG115]. London: National Institute for Health and Care Excellence, 2011.
Ballard S . The hematological complications of alcoholism. Alcohol Health Res World 1997; 21: 42–52.
DeSancho M, Pastores S . The liver and coagulation. In Rodés J, Benhamou J, Blei A, Reichen J, Rizzetto M (ed) The textbook of hepatology: From basic science to clinical practice. 3rd ed. pp 260. Oxford: Blackwell publishing Ltd, 2007.
Chee Y L, Crawford J C, Watson H G, Greaves M . Guidelines on the assessment of bleeding risk prior to surgery or invasive procedures. Br J Haematol 2008; 140: 496–504.
Scottish Intercollegiate Guidelines network (SIGN). The management of harmful drinking and alcohol dependence in primary care. SIGN publication no.74. Edinburgh: SIGN, 2003. Online guidelines available at http://www.sign.ac.uk (accessed July 2015).
Tripodi A, Salerno F, Chantarangkul V et al. Evidence of normal thrombin generation in cirrhosis despite abnormal conventional coagulation tests. Hepatology 2005; 41: 553–558.
Tripodi A, Mannucci P M . The coagulopathy of chronic liver disease. N Engl J Med 2011; 365: 147.
Gupta A, Epstein J B, Cabay R J . Bleeding disorders of importance in dental care and related patient management. J Can Dent Assoc 2007; 73: 77–83.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Quach, S., Brooke, A., Clark, A. et al. Blood investigations prior to oral surgery for suspected alcohol-induced coagulopathy. Are they necessary?. Br Dent J 219, 121–123 (2015). https://doi.org/10.1038/sj.bdj.2015.593
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.593
This article is cited by
-
The relevance of alcohol to dental practice
BDJ Team (2018)
-
The relevance of alcohol to dental practice
British Dental Journal (2017)