Key Points
-
Stresses that carcinogenic products use among the South Asian population in the UK is a substantial burden on healthcare.
-
Suggests that this community is not homogenous and requires a further study of risk behaviour, beliefs and knowledge levels in the different subgroups.
-
Highlights that primary prevention of oral cancer is both feasible and practical in helping to reduce oral cancer morbidity and mortality.
Abstract
Objectives To determine any differences in oral cancer risk factor awareness and behaviour among first and second generation Gujarati muslims and to investigate the impact of a community-based health education programme on oral cancer risk factor awareness.
Design Respondents completed a confidential, bilingual questionnaire in English and Gujarati regarding alcohol, tobacco, paan, sopari, paan masala and gutka use before and after a community-based health education programme on oral cancer risk factors.
Setting Community Health Fair. Indian Muslim Welfare Association, Batley, West Yorkshire.
Subjects Ninety-six male and female Gujarati muslims aged 16 to 81 years.
Main outcome measures Quantitative results on oral cancer risk factor awareness before and after a health education programme. Quantitative figures obtained from the questionnaire with regards to alcohol, tobacco, paan, sopari, paan masala and gutka usage.
Results There were very low levels of alcohol consumption among Gujarati muslims. First generation Gujarati males consumed significantly more tobacco than second generation Gujarati males, difference in proportion 0.30 (0.03 to 0.56, p = 0.03). There was complete absence of paan use among Gujarati females. First generation Gujarati males consumed significantly higher amounts of sopari compared with their male counterparts in the second generation (p = 0.003). There were very low rates of paan masala use. Only first generation Gujarati males consumed gutka. Significantly more first generation males and females correctly identified all oral cancer risk factors after the health education intervention compared with baseline (difference 0.40, 95% CI 0.23 to 0.57, p = <0.001). Significantly more second generation males and females correctly identified all oral cancer risk factors after the health education intervention compared with baseline (difference 0.45, 95% CI 0.28 to 0.61, p = <0.001).
Conclusion Our study demonstrated significant differences in oral cancer risk factor awareness and practices among first and second generation Gujarati muslims and that a local community-based health education programme was effective in raising awareness.
Similar content being viewed by others
Introduction
In the United Kingdom, oral cancer accounts for 2% of all new cancer cases per year with major risk factors including tobacco, alcohol, betel quid and areca nut use.1 Areca nut chewing is common and is carried out by approximately 20% of the world's population.2 Due to its frequent use in the Indian subcontinent, oral cancer is the commonest incident cancer in this region accounting for approximately 40% of all cancers.3 Betel quid ('paan') is the most popular cultural product used among South Asian immigrants in the UK and usually consists of a mixture of areca nut with or without tobacco, slaked lime, catechu and a number of condiments enclosed within a betel leaf. When areca nut is combined with tobacco it can cause premalignant lesions.4 Chewing betel quid is an independent risk factor for oral cancer.5 Betel quid chewing in combination with alcohol and tobacco use increases the relative risk of oral cancer by approximately 11-fold.6
South Asian migrants carry their native oral cancer risk factors to their new settlements.7 Rising UK immigration from South Asia suggests that this group will present a serious oral cancer public health challenge. Betel quid and smokeless tobacco consumption are common practices among certain subgroups of South Asian immigrants who have products such as areca nut and gutka readily available to them.8,9 UK and US studies have reported the continuation of areca nut chewing habits in South Asian immigrants leading to increased rates of oral cancer in host communities.2,8,10 In comparison to the indigenous population, South Asian immigrants in the UK have a higher cancer mortality rate including cancer of the mouth and pharynx.11 Studies have also demonstrated differences in the rate of coronary heart disease and type 2 diabetes between first and second generation migrants due to acculturation to host country risk factor practices.12,13
Although oral cancer is a potentially preventable disease due to its association with well-established risk factors, awareness of such risk factors is found to be generally poor among the UK South Asian community.14,15
Our study is the first to explore oral cancer risk awareness and behaviour among first and second generation muslim Gujaratis in the UK. It is also the first to assess the impact of a brief structured community-based health education programme in raising the awareness of oral cancer within an ethnic community.
Method
Muslim Gujarati participants aged 16 years or over were voluntarily recruited at an annual health fair organised by a community welfare group in West Yorkshire. The health fair was advertised in local community centres, places of worship and the community magazine. Potential participants were invited during registration to take part in the study and those that provided written consent completed an anonymous bilingual questionnaire written in English and Gujarati before the start of an oral cancer awareness education programme. The structured questionnaire covered information on participant demographics including age, gender, ethnicity, place of birth, citizenship and religious belief along with use of tobacco, alcohol, paan, areca nut, paan masala and gutka. Dental registration status and knowledge of oral cancer risk factors were also explored. The questionnaires were collected before commencement of a health education programme on oral cancer risk factor awareness and an identical questionnaire was completed two hours later, immediately after the end of the programme. The health education programme consisted of short lectures, poster board presentations and workshops delivered by UK trained general dental practitioners, general medical practitioners and hospital doctors.
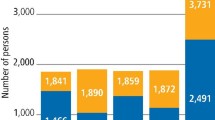
Study eligibility criteria included muslim Gujarati males and females aged 16 years or above. No potential participants refused consent to participate in the study. All 96 participants fully completed the questionnaires and were recruited into the study. The information obtained from the questionnaires was manually processed and data entered into tables. Double entry and validation was used to guard against incorrect data entry error. The main study group divisions were based upon gender and generation status. First generation Asians were classified as foreign born citizens or residents who have immigrated and been naturalised in the UK. Second generation Asians were classified as the second generation of a family to inhabit but the first to be naturally born in the UK. No data were stored electronically. The age and community structure of the participants can be seen in Table 1.
Statistical analysis
Differences in proportions were calculated, together with 95% confidence intervals, using the normal approximation to the binomial distribution. P-values were derived from the associated standard normal deviates.
Results
As anticipated due to religious prohibition, Gujarati muslims have very low declared alcohol consumption levels. Ninety-eight percent of first generation and 91% of second generation Gujarati muslims denied alcohol intake. The difference in the level of alcohol consumption between the first and second generation was 0.03 (95% CI 0.11 to 0.05, p = 0.44) and between males and females was 0.04 (0.04 to 0.12, p = 0.36). Neither was statistically significant (Table 2).
The difference in the proportions reporting tobacco consumption in first generation muslim Gujarati males (54%) compared with second generation males (26%) was 0.30 (0.03 to 0.56, p = 0.03) which was statistically significant. The difference in the proportions reporting tobacco use among second generation males (26%) compared with second generation females (14%) was 0.09 (0.15 to 0.34, p = 0.44). There was no regular tobacco use among first generation females (Table 3).
There was a slightly greater proportion of first generation Gujarati muslim males using paan regularly (12%) compared to second generation males (4%) but this was not statistically significant (p = 0.25). There was no regular paan use among Gujarati muslim females (Table 4).
First generation Gujarati muslim males had the highest proportion of regular sopari users (33%), which was greater than their female counterparts (12%; p = 0.11) and significantly greater than males in the second generation (4%; p = 0.003). Second generation Gujarati muslim females had the lowest sopari consumption at (3%). But there was no statistical difference compared with second generation males (p = 0.07) (Table 5). There was very low rate of paan masala use among the Gujarati muslim respondents. Only 8% of first generation males claimed to use paan masala regularly (Table 6).
There was complete absence of regular Gutka use in Gujarati muslims except among first generation males (42%). After tobacco, Gutka consumption was the most common habit among this group of respondents (Table 7).
Before the health education intervention, 69% of second generation Gujarati muslim females had already heard of oral cancer, which was higher than first generation females (56%) although the difference (0.13, 95% CI 0.17 to 0.42) was not statistically significant (p = 0.40). Sixty-three percent of second generation males had heard of oral cancer, which was higher than first generation males (50%), difference 0.13 (95% CI 0.14 to 0.40, p = 0.35) who were the least likely to have heard of oral cancer. Female respondents were more likely to have heard of oral cancer compared to males in their generation. Overall, more female respondents (64%) had heard of oral cancer compared to males (57%), difference 0.08 95% CI 0.12 to 0.27 (p = 0.45) although this difference was not statistically significant. Gutka and tobacco were the most correctly identified risk factors among first generation males (38%). Gutka was the most correctly identified risk factor among first generation females (50%) and second generation males and females (63% and 69% respectively). In identifying all oral cancer risk factors correctly, there was no significant difference between first generation males (8%) and females (6%) (difference 0.12, 95% CI 0.14 to 0.18, p = 0.80). There was also no significant difference between second generation males (30%) and females (31%) (difference 0.01, 95% CI 0.25 to 0.23, p = 0.91). However, there was a significant difference in correct responses between first and second generation corresponding genders (p = 0.002), difference 0.22 (95% CI 0.08 to 0.36). Alcohol was the risk factor least identified by all subgroups.
First generation Gujarati muslims who had heard of oral cancer stated relatives (43%), dentists (33%) and media oral cancer awareness campaigns (24%) as their primary source of information. Second generation Gujarati muslims named media oral cancer awareness campaigns (57%), relatives (27%) and dentists (16%) as their primary source of information. 63% of first generation and 42% of second generation Guajarati muslims who stated they had not heard of oral cancer were registered with a dentist at the time of the study (Table 8).
After health education, tobacco was the risk factor most correctly identified by first generation Gujarati muslim males and females (75% and 81% respectively). Paan was the risk factor most correctly identified by second generation males (88%). Paan, tobacco and gutka were the risk factors most correctly identified by second generation females (93%). Across all subgroups, awareness of all oral cancer risk factors increased from baseline. Significantly, more first generation males (42%) and females (56%) correctly identified all oral cancer risk factors after health education compared to baseline knowledge (8% and 6% respectively) (difference 0.40, 95% CI 0.23 to 0.57, p = <0.001). Significantly, more second generation males (66%) and females (83%) correctly identified all oral cancer risk factors after health education compared to baseline knowledge (30% and 31% respectively) (difference 0.45, 95% CI 0.28 to 0.61, p = <0.001). Overall, oral cancer risk factor awareness after health education increased in females in greater proportion than males in both the first and second generations (50% and 52% increased awareness in females compared with 34% and 36% increased awareness in males; p = 0.02). After health education, alcohol still remained the least correctly identified risk factor across most subgroups (Table 9).
Discussion
The use of carcinogenic products in the UK South Asian population presents a substantial burden on healthcare and risks psychological dependency.2 Recently, relatively cheap and increasingly popular commercially produced sachets of betel quid substitutes called gutka have become available. These carry greater carcinogenic potential compared with conventional betel quid due to the dangerous combination of tobacco and areca nut.16 By adulthood, most users are addicted to the habit and it therefore persists after immigration.17 Regular use of betel quid and gutka is a strong risk factor for oral cancer.18,19
Vora et al. in their study of oral cancer risk behaviour practices among Asian males in Leicester found variation in practice based upon religious and generation grounds.14 This highlights that the South Asian community in the UK is not homogenous and the need to study risk behaviour, beliefs and knowledge levels in the different subgroups of this population with a view for prevention. Appropriate public health measures and early detection of oral lesions is required to influence the cancer mortality rate in this high risk population.20
Betel quid is widely used among UK Indian Gujarati speakers.21 At present, Bangladeshi adults are the predominant South Asian subgroup still retaining the chewing habits in the UK.22 However, there is evidence that chewing practices have extended to subsequent generations of Asians born in the UK.14
A study in the United States (US) investigating paan and gutka use in Indian-Gujarati immigrants9 found 5% of the study sample consuming paan and 77% consuming gutka regularly with no regular gutka consumption among the female respondents. Our study showed similar findings in the rate of paan consumption (4%) but a lower proportion of gutka users (10%). Our study also revealed the complete absence of regular gutka use among Indian-Gujarati women. Forty-eight percent of the Indian-Gujarati immigrants correctly identified paan as a risk factor for oral cancer, which was similar to the findings of 43% in our sample group. However, 93% of respondents in their study correctly identified gutka as a risk factor for oral cancer compared with only 56% of respondents in our study. The differences in the results may be explained by our study consisting of a restricted religious sample. A study investigating oral cancer risk awareness and practices among a South Asian male community in the UK found 23% of muslim respondents chewing paan regularly but there was no data on gutka use.21 Forty-six percent of their first generation muslim respondents had heard of oral cancer compared to a similar proportion of 50% in our study. However, only 43% of their second generation muslim respondents had heard of oral cancer compared to 63% in our study.
This study used convenience sampling, which limits its generalisability because we cannot be sure that we had a representative sample. This is compounded by the relatively small sample size leading to lower statistical power. Another potential issue is multiple significance testing, which increases the likelihood of some of the small significant differences we found in our study being due to chance. Population selection bias is self-evident. Health education interventions delivered to communities may promote cancer awareness and early presentation but the evidence is limited.23
Our study demonstrated that a local community-based health education programme was effective in raising at least short-term awareness of oral cancer risk factors in a Gujarati South Asian community. It also emphasises that the public require information and education in matters relating to risk factors associated with oral cancer and that the need to develop a health promotion strategy to prevent cancers should include oral cancer as a priority. This is consistent with findings in other studies.24,25
There is evidence that at present, there are inadequate strategies and policies for primary prevention, health promotion and education related to oral cancer control.25 A large population-based prospective intervention study demonstrated that primary prevention of oral cancer is both feasible and practical.26 Morbidity and mortality associated with oral cancer can be reduced by primary prevention and early detection.27
Conclusion
We provided an overview of oral cancer risk factor awareness and practices among a UK adult muslim Gujarati population. Our study has highlighted particularly concerning poor awareness of gutka as a risk factor for oral cancer despite it being one of the most common habits among first generation Gujarati muslim males and one of the most carcinogenic.
A health education programme proved to be effective in raising short-term awareness of oral cancer risk factors among the muslim Gujarati community. The likelihood of long-term retention of oral cancer risk factor knowledge or whether this increased awareness of risk factors will translate to desirable behavioural change requires further research.
References
Cancer Research UK. Oral cancer incidence statistics. Cancer Research UK, 2013. Online statistics available at http://www.cancerresearchuk.org/cancer-info/cancerstats/types/oral/incidence/uk-oral-cancer-incidence-statistics#By (accessed July 2013).
Warnakulasuriya S . Areca nut use following migration and its consequences. Addict Biol 2000; 7: 127–132.
Parkin D M, Pisani P, Ferlay J . Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 1999; 80: 827–841.
Chitropa P K, Shah J T, Katti G, Ghali S . A correlative study of smokeless tobacco induced lesions and smoke induced leukoplakia in various aspects. Journal of Indian Academy of Oral Medicine and Radiology 2011; 23: 86–91.
Jacob B J, Straif K, Thomas G et al. Betel quid without tobacco as a risk factor for oral precancers. Oral Oncol 2004; 40: 697–704.
Subapriya R, Thangavelu A, Mathavan B, Ramachandran C R, Nagini S . Assessment of risk factors for oral squamous cell carcinoma in Chidambaram, southern India: a case control study. Eur J Cancer Prev 2007; 16: 251–256.
Warnakulasuriya S . Ethnicity, race and oral cancer. In Bedi R, Bahl V, Rayan R R (eds) Dentists, patients and ethnic minorities. pp 57–65. London: The Royal College of Surgeons, 1996.
Changrani J, Gany F M, Cruz G, Kerr R, Katz R . Paan and gutka use in the United States: a pilot study in Bangladeshi and Indian Guajarati immigrants in New York city. J Immigr Refug Stud 2006; 4: 99–110.
Auluck A, Hislop G, Poh C, Zhang L, Rosin M P . Areca nut and betel quid chewing among South Asian immigrants to western countries and its implications for oral cancer screening. Rural Remote Health 2009; 9: 1118.
Changrani J, Gany F M . Paan and gutka use in the United States: an emerging threat. Journal of Immigrant Health 2005; 7: 103–108.
Balarajan R, Bulusu L, Adelstein A M, Shukla V . Patterns of mortality among migrants to England and Wales from the Indian subcontinent. BMJ 1984; 289: 1185–1187.
Worth R M, Kato H, Rhoads G G, Kagan A, Syme S L . Epidemiological studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: mortality. Am J Epidemiol 1975; 102: 481–490.
Zheng Y, lamoureux E L, Ikram M K et al. Impact of migration and acculturation on prevalence of type 2 diabetes and related eye complications in Indians living in a newly urbanised society. PLoS One 2012; 7: e34829.
Vora A R, Yeoman C M, Hayter J P . Alcohol, tobacco and paan use and understanding of oral cancer risk among Asian males in Leicester. Br Dent J 2000; 1888: 444–451.
Shetty K V, Johnson N W . Knowledge, attitudes and beliefs of adult South Asians living in London regarding risk factors and signs for oral cancer. Community Dent Health 1999; 16: 227–231.
Nair U, Bartsch H, Nair J . Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: a review of agents and causative mechanisms. Mutagenesis 2004; 19: 251–262.
Chandra P S, Mulla U . Areca nut: the hidden Indian 'getaway' to future tobacco use and oral cancers among youth. Indian J Med Sci 2007; 61: 319–321.
Murti P R, Bhonsle R B, Pindborg J J, Daftary D K, Gupta P C, Mehta F S . Malignant transformation rate in oral submucous fibrosis over a 17 year period. Community Dent Oral Epidemiol 1985; 13: 340–341.
International Agency for Research on Cancer. Betel quid and areca nut chewing and some areca nut related nitrosamines. Lyon: IARC monographs, 2004.
Swerdlow A J, Marmot M G, Grulich A E, Head J . Cancer mortality in Indian and British ethnic immigrants from the Indian subcontinent to England and Wales. Br J Cancer 1995; 72: 1312–1319.
Winstock A R, Trivedy C R, Warnakulasuriya K A, Peters TJ . A dependency syndrome related to areca nut use: some medical and psychological aspects among areca nut users in the Gujrat community in the UK. Addict Biol 2000; 5: 173–179.
Khan F A, Robinson P G, Warnakulasuriya K A, Newton J T, Gelbier S, Gibbons D E . Predictors of tobacco and alcohol consumption and their relevance to oral cancer control among people from minority ethnic communities in the South Thames Health Region, England. J Oral Pathol Med 2000; 29: 214–219.
Warnakulasuriya K A, Harris C K, Scarrott D M, Watt R, Gelbier S, Peters T J, Johnson N W . An alarming lack of public awareness towards oral cancer. Br Dent J 1999; 187: 319–322.
Amarasinghe H K, Usgodaarachchi U S, Johnson N W, Warnakulasuriya K A . Public awareness of oral cancer, of oral potentially malignant disorders and of their risk factors in some rural populations in Sri Lanka. Community Dent Oral Epidemiol 2010; 38: 540–548.
Chiba I . Prevention of betel quid chewers oral cancer in the Asian pacific area. Asian Pac J Cancer Prev 2001; 2: 263–269.
Gupta P C . Betel quid and oral cancer: prospects for prevention. IARC Sci Publ, 1991; (105): 466–470.
Ahluwalia K P . Assessing the oral cancer risk of South Asian immigrants in New York City. Cancer 2005; 104 (Suppl 2): 2959–2961.
Acknowledgements
We would like to thank the Indian Muslim Welfare Association of Batley, West Yorkshire for providing the venue and subjects for the study and Professor Damien McElvenny for advising on the statistical analysis of the study data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Siddique, I., Mitchell, D. The impact of a community-based health education programme on oral cancer risk factor awareness among a Gujarati community. Br Dent J 215, E7 (2013). https://doi.org/10.1038/sj.bdj.2013.829
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.829
This article is cited by
-
The UK public and healthcare professionals' awareness of mouth cancer
British Dental Journal (2023)
-
“Cancer Education on Wheels,” a Novel Cost-Effective Method in Creating Awareness in the Community: a Pilot Study
Journal of Cancer Education (2023)
-
A survey of the awareness and knowledge of oral cancer among residents in Beijing
BMC Oral Health (2022)
-
Effectiveness of Interventions to Improve Oral Cancer Knowledge: a Systematic Review
Journal of Cancer Education (2022)
-
Health and Social Care Outcomes in the Community: Review of Religious Considerations in Interventions with Muslim-Minorities in Australia, Canada, UK, and the USA
Journal of Religion and Health (2022)