Key Points
-
Describes a case report of a life threatening complication that should be brought to the attention of all practitioners involved in the placement of osseo-integrated implants.
-
The aetiology of the complication, principles of management and preventative/precautionary measures are discussed.
Abstract
The floor of the mouth is a very vascular area. Should perforation of the lingual cortex of the mandible occur during the placement of an osseo-integrated implant, significant haemorrhage may result. We present the case of a patient who attended our unit with acute airway obstruction. Although life threatening haematoma following the placement of osseo-integrated implants in the interforaminal area of the mandible is known to occur, there continue to be sporadic reports in the literature.1,2,3,4 This shows that some practitioners are unaware of the risks involved and place implants of the wrong size and orientation.
Similar content being viewed by others
Case report
A 71-year-old man was referred from a dental implant practice to the maxillofacial service at Wythenshawe Hospital, South Manchester. Two implants had been placed in the anterior mandible together with some implants in the maxilla under local analgesia. Swelling of the floor of the mouth was noticed immediately after the insertion of the mandibular implants. It enlarged gradually during the first two postoperative hours to a point where the patient was unable to talk.
He was examined in the resuscitation area of the Accident and Emergency department where he was kept sitting upright. His oxygen saturation was 95% on air and the respiratory rate was 15 breaths/minute. He was tachycardic (120 beats/minute) and hypertensive (268/150 mmHg). Intravenous access was secured and blood specimens were sent for haematological investigations and cross match.
There was evidence of a large haematoma involving the sublingual, submental and submandibular spaces bilaterally. The tongue was displaced superiorly, pressed firmly against the palate and protruded extraorally (Fig. 1). There was neither bleeding nor any signs of haematoma at the sites of the maxillary implants and the nasopharyngeal airway was patent.
His medical history included hypertension and he was on bendroflumethiazide, lisinopril and aspirin which had not been discontinued prior to the surgical procedure.
Consent was obtained and the patient was taken immediately to the emergency theatre. The airway was secured by awake fibre-optic intubation undertaken in the partially reclining position which was technically difficult. General anaesthesia was induced and tracheostomy was undertaken. An attempt to release the haematoma via a midline incision in the floor of the mouth and limited dissection of the sublingual space proved unrewarding. Antibiotic prophylaxis was administered intravenously and continued into the post-operative period. The patient was also given intravenous steroids (Dexamethasone 8 mg) after the induction of general anaesthetic and two further doses post-operatively at eight hourly intervals. The hypertension was managed with labetalol infusion and later atenolol.
He was subsequently transferred to the Intensive Care Unit. He was extensively investigated as to whether he might have an underlying coagulopathy but this was found not to be the case. The tracheostomy was removed the second post-operative day and the site was dressed with an airtight dressing and healed spontaneously. The patient was discharged home on the fifth post-operative day. He made a full recovery and progressed to completion of his implant retained dentures.
Discussion
The anterior floor of mouth is a very vascular area. It is supplied by the sublingual branch of the lingual artery which anastomoses with the submental artery, a branch of the facial artery, and the incisive arteries which are branches of the inferior alveolar artery.4 This rich anastomosing plexus lies very close to the interforaminal lingual cortical plate of the mandible and can give rise to extensive bleeding.2,4
Severe haemorrhage from these vessels has been reported as a complication of dental and surgical procedures involving perforation of the lingual cortex and/ or laceration of the adjacent soft tissues, as well as a result of malignant invasion, radionecrosis, trauma and anticoagulant treatment.2,3,4
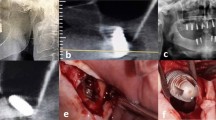
In our patient the cause of the haematoma was perforation of the lingual cortex prior to placement of osseo-integrated implants (Fig. 2) possibly compounded by aspirin treatment which has a well known anti-platelet action.
Significant haemorrhage into the sublingual space is likely to lead to dissecting sublingual, submandibular and submental haematomas4 with elevation of the tongue and airway obstruction similar to Ludwig's angina. The treatment of this complication depends on the extent and the progress of the haematoma. The principles of management are airway preservation, drainage of haematoma and haemostasis together with correction of any cardiovascular or coagulation disorders. The tissues of the floor of the mouth are lax and haemorrhage results in diffuse haematoma rather than a discrete collection which would be easy to drain. Surgical drainage and identification of the bleeding vessel should, however, be attempted. In a comprehensive review of the literature Kalpidis and Setayesh4 found that tamponade and digital compression were helpful in controlling the haemorrhage in only few cases. The majority of patients required drainage of the haematoma and haemostasis via an intraoral or extraoral approach.
This case demonstrates the need for appropriate information to be given to patients during the consent procedure. Preventative/precautionary measures to avoid perforation of the lingual cortex should be taken. It is vital to appreciate the shape of the lingual cortex and to select carefully the correct implant length and angulation. Imaging techniques that assess the mandibular anatomy in a sagittal plain such as lateral cephalometric radiographs and computed tomograms (CT) as well as surgical stents may be an advantage. In high risk cases, elevation of a lingual mucoperiosteal flap to assess the mandibular contour intra-operatively and to protect the sublingual soft tissues and vasculature may prevent this complication. This surgical manoeuver, however, carries itself a risk of haemorrhage within the anterior floor of mouth and requires care. Practitioners involved in implant placement should be trained and well equipped in their practice environment to deal with such emergencies. Skills in the management of compromised airway are imperative.
References
Mordenfeld A, Andersson L, Bergström B. Hemorrhage in the floor of the mouth during implant placement in the edentulous mandible: a case report. Int J Oral Maxillofac Implants 1997; 12: 558–561.
Hofschneider U, Tepper G, Gahleitner A, Ulm C. Assessment of the blood supply to the mental region for reduction of bleeding complications during implant surgery in the interforaminal region. Int J Oral Maxillofac Implants 1999; 14: 379–383.
Niamtu J III . Near-fatal airway obstruction after routine implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 597–600.
Kalpidis C D, Setayesh R M. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 2004; 75: 631–645.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Pigadas, N., Simoes, P. & Tuffin, J. Massive sublingual haematoma following osseo-integrated implant placement in the anterior mandible. Br Dent J 206, 67–68 (2009). https://doi.org/10.1038/sj.bdj.2009.2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.2
This article is cited by
-
Mental foramen and lingual vascular canals of mandible on MDCT images: anatomical study and review of the literature
Anatomical Science International (2018)
-
Massive sublingual hematoma secondary to anticoagulant therapy complicated by a traumatic denture: a case report
Journal of Medical Case Reports (2012)
-
Are we respecting the anatomy of the jaws?
Oral Radiology (2010)