Abstract
Introduction A patient requested dental implant therapy to replace his missing upper left central incisor. Pre-operative cone beam computed tomography (CBCT) imaging revealed a complex neurovascular supply to the anterior maxilla.
Discussion Imaging demonstrated accessory neurovascular canals around the nasopalatine foramen which directly communicate with canalis sinuosus. They are, therefore, most likely to carry branches of the anterior superior alveolar nerve and vessels. One of these canals was directly in the path of proposed dental implant placement. A review of the dental literature suggests that such anatomical variation is relatively common. Some authors have proposed that injury to these structures is a cause of intractable pain following dental implant placement. Following discussion with the patient, it was agreed that the provision of an adhesive bridge was a realistic alternative in this case.
Conclusion The availability of CBCT imaging in recent years has shown that complex neurovascular anatomy in the anterior maxilla is not uncommon. Evidence is lacking regarding the relevance of this to dental implant placement but it is possible that injury to these structures explains some cases of postoperative intractable pain.
Similar content being viewed by others
Key points
-
Complex neurovascular anatomy in the anterior maxilla is not uncommon.
-
Highlights that evidence is lacking regarding the relevance of this to dental implant placement.
-
Suggests it is possible that injury to these structures explains some cases of postoperative intractable pain.
Introduction
While dental implant placement in the anterior maxilla is considered to be a safe procedure, several cases of persistent pain and chronic discomfort following dental implant placement in this region have been reported.1,2,3,4,5,6 The availability of cone beam computed tomography (CBCT) technology in recent years has led to frequent three dimensional imaging of the region before dental implant placement. Along with anatomical studies, this has highlighted the variability of the neurovascular structures in the anterior maxilla.7,8,9,10,11 Neurovascular supply to the anterior maxilla arises from the nasopalatine nerves and vessels through the nasopalatine canal. The anterior superior alveolar nerves and vessels reach the anterior maxilla through the neurovascular canal, canalis sinuosus.12 Variation is common in both structures.7,8,10,11 Persistent or intractable pain following dental implant placement in the anterior maxilla has been attributed to both psychological and physical causes such as impingement on neurovascular structures.2,3,13,14 This case study presents a patient who was a candidate for dental implant placement in the upper left central incisor position. Preoperative CBCT scanning revealed a complex neurovascular supply to the area. These anatomical findings and their significance in relation to possible complications following dental implant placement are discussed. The management of this patient in light of these considerations is also presented.
Case presentation
A 49-year-old male patient presented with a missing upper left central incisor. This tooth was lost as the result of trauma followed by a failed restoration. The tooth was extracted some four years before presentation. The patient was unhappy with wearing his mucosa-supported acrylic partial denture and wished to discuss fixed alternatives, including a dental implant supported restoration.
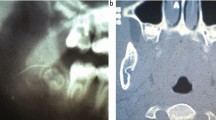
Clinical examination, periapical radiography, and ridge mapping suggested a significant labial alveolar defect and a potentially large nasopalatine foramen complicating dental implant placement (Fig. 1). Based on these findings, the available bone volume for dental implant placement was regarded as borderline. Therefore, in accordance with current guidance, a CBCT scan was prescribed to further assess the potential implant site.15,16,17,18
Anatomical findings
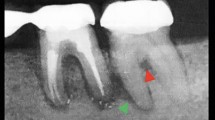
On examination of the CBCT images, complex neurovascular anatomy was observed. The nasopalatine canal begins at the floor of the nose as three distinctly separate canals (Fig. 2). More inferiorly, the three coalesce into one nasopalatine foramen. The two lateral openings of these canals into the nasopalatine foramen have been termed the foramina of Stensen and the openings of midline canals have been termed foramina of Scarpa.19 At the level of the hard palate, four additional foramina may be observed anterior and lateral to the nasopalatine foramen (Fig. 3). By tracing into the bone from these foramina on the CBCT images, it can be observed that they are the openings of accessory canals which communicate with canalis sinuosus (Figs 4 and 5).12 They are most likely, therefore, to carry branches of the anterior superior alveolar nerves. At the site of the missing upper left central incisor, a reformatted CBCT image in the sagittal plane shows one of the accessory canals longitudinally (Fig. 6). The dense cortical bone of the lateral border of the nasopalatine canal can be seen immediately posterior to the accessory canal.
Setting aside the accessory canal, the site may otherwise be regarded as having satisfactory bone volume for placement of a dental implant, avoiding the nasopalatine canal. Nevertheless, the presence of these accessory canals raised concerns. Impingement on the accessory canal at the potential implant site seemed unavoidable. The risks of excessive haemorrhage appeared minor, given the small size of the canal. A more serious concern, however, was the potential for peripheral nerve injury and neuropathic pain.
Case management
This case was discussed between the general dental practitioner, who was providing treatment, a specialist in prosthodontics, a professor of maxillofacial imaging, and a professor of oral and maxillofacial surgery. A neurovascular canal was very clearly visible at the site of the potential implant placement (Fig. 6). While evidence is lacking on this issue, it was felt that nerve damage and subsequent intractable pain was a significant risk and could not be ruled out if a dental implant was to be placed. These findings, the outcome of our deliberations and options for replacement of the missing upper left central incisor were then discussed with the patient.
In this case, it was felt that there was a realistic fixed alternative, an adhesive cantilever bridge supported by the intact upper right central incisor. This also had the advantage of very low risk, rapidity of production and low cost. The patient's occlusion was also acceptable for an adhesive restoration. The patient's smile line was favourable and so the contact of the pontic with the defect in the alveolar ridge was hidden during normal function. On balance, therefore, it was felt that this was a realistic alternative to potentially damaging implant therapy. The patient accepted this proposal and was very satisfied with the result (Fig. 7).
Discussion
Figure 8 is a diagrammatic representation of the course of canalis sinuosus, from where it leaves the infraorbital canal in the floor of the orbit. The canal reaches the anterior margin of the orbit lateral to the infra-orbital foramen, before turning inferiorly and medially in the anterior wall of the maxillary sinus. It curves inferiorly to the infraorbital foramen before reaching and then curving around the nasal opening. Its termination in the nasal septum is termed 'foramen septale'. The two accessory neurovascular canals found on the left side in this case are shown branching inferiorly towards the edentulous ridge at the site of the upper left central incisor.
Several cases of intractable pain following dental implant placement in the anterior maxilla have been reported. In 2017, McCrea drew attention to the presence of branches of canalis sinuosus in the alveolar bone of the upper incisor region and reported a case in which dental implant placement had led to persistent pain.2 The author attributed this to 'invasion of the nasopalatine duct together with the unidentified injury to an aberrant neurovascular canal inferior to the canalis sinuosus'. It is reported that the patient's symptoms resolved following removal of the implant and repair of the site with particulate xenograft material.
In 2017 Politis et al. published a case series of 26 patients referred to a tertiary centre because of neuropathic pain, following dental implant placement.4 Six patients with implants placed in the anterior maxilla were included in the study. Pain was attributed to nerve injury in three of these six patients. The authors draw attention to canalis sinuosus possibly being traumatised during implant placement and present a CBCT image showing a dental implant in close relationship to this canal.
Rodriguez-Lozano et al. in 2010 reported a case in which eight maxillary implants were placed.5 At the time of surgery, a sharp pain was felt during placement of the implant in the upper left canine position. Pain persisted many months postoperatively. While there is some confusion over the diagnosis, the authors attribute this, at least in part, to the position of the dental implants. In the upper left canine region, trauma to the anterior superior alveolar nerve in canalis sinuosus cannot be ruled out.12
In 2015, Shaeffer reported a case of intractable pain following implant placement in the upper left first premolar position but which was impinging on the root of the adjacent canine.6 The pain did not subside following removal of the implant, or of the canine, and the diagnosis remained unclear.
Three cases of chronic idiopathic pain following dental implant placement in the anterior maxilla were reported by Patel and Nixon in 2018.3 They report that no cause was identified for any case and that all patients continued to experience symptoms. Psychological aetiologies were proposed and treatment was prescribed accordingly. None of the implants were removed, on the basis that further surgical trauma may worsen the outcome. The authors report that CT or cone beam CT imaging was available in some cases. They considered possible sources of pain, including 'damage to the neurovascular bundle or accessory nerves', but these were excluded as possible diagnoses. An analysis of these images specifically with regard to possible accessory canals of canalis sinuosus is not reported.
Devine et al. in 2016 reported a retrospective case series of ten patients with chronic post-surgical pain following dental implant placement.1 Of these, seven patients had implants placed in the anterior maxilla. In two cases, implants had been subsequently removed but this did not result in improvement of the symptoms. In some cases, the postoperative pain began immediately after placement of the dental implants and, in others, after provision of the implant-supported prosthesis. Nine patients were treated with pharmacological and behavioural therapy, with partial improvement in five patients. One patient refused treatment. The authors were not able to identify nerve injury in these ten cases, although it is not clear if the presence of accessory neurovascular canals were specifically excluded. Understandably, in most cases, the patients were left with their prostheses in place so as not to deprive them of a functional, long-term restoration.
In 2003, Goodacre et al. carried out a review of implant complications and found that neurosensory disturbance affected 7% of patients.20 Unfortunately, the details of which of these occurred in the anterior maxilla are not available. Notwithstanding, the presence of accessory canals in the anterior maxilla is reasonably common. In an observational study of 176 CBCT images of the anterior maxilla in 2013, von Arx et al. found that there were accessory canals, at least 1 mm in diameter, in 27.87% of patients.10 Of these, 56% could be shown to communicate with canalis sinuosus. In a similar study of cone beam CT images in 2015, Wanzeler et al. found that canalis sinuosus itself was present in 88% of cases.11 This raises the question of whether these, often poorly identified, neurovascular canals might be the cause of at least some cases of intractable pain following dental implant placement in the region.
It has been suggested that three surgical scenarios are possible in relation to minor neurovascular canals and dental implant placement. The first is that the implant is placed at a safe distance and no adverse consequences arise. The second is that the drilling for the implant osteotomy passes directly through the neurovascular channel such that there is nerve discontinuity at that point. Where this is a functionally unimportant neurovascular canal, such as canalis sinuosus or its accessory branches, no adverse consequences arise. In the third scenario, however, the implant is placed such that it is compressing the nerves of the canal, causing neuropathy. This outcome is well reported in the case of the inferior dental nerve for example.21,22,23,24 This offers a possible explanation of why neuropathy following dental implant placement in the anterior maxilla does not always result if accessory canals of canalis sinuosus are present.
The question is also raised of why some patients only experience intractable pain following fitting of the prosthesis to dental implants.1 It is possible that loading a dental implant with a prosthesis increases the compression of the surrounding bone during function. Another explanation might be that clinical and laboratory procedures are sufficiently accurate to allow the fitting of a splinted prosthesis, but that the fit is not quite completely passive. Tightening the prosthesis onto the implants might then place a torque on an implant which compresses the surrounding bone sufficiently and in a way that further affects nerve tissue. Nonetheless, these are merely speculative explanations.
It seems clear that some cases of intractable pain following implant surgery are the result of psychological issues.1,3 Chronic postoperative pain can occur following other types of surgery and parallels have been drawn with the phantom pain experienced after amputation of a limb, for example.3,14 Nevertheless, patients with chronic pain often present a complex diagnostic challenge. It seems reasonable to assume that, if the accessory canals of canalis sinuosus often remain unidentified, that at least some cases in the anterior maxilla may have a physical cause which is also unidentified. In some cases, removal of the implant, which is considered to be the cause of the pain, does not resolve the problem.1,6 It might, therefore, be assumed that the implant placement was not the cause of the pain and other diagnoses considered. Nevertheless, this would appear to be an unsafe assumption. An alternative explanation might be that the preparation of the implant osteotomy and placement of an implant is the cause of neural damage which persists after removal of the implant itself.
Imaging guidelines
In prescribing imaging in this case, UK and European guidelines were followed and these led to the prescription of cone beam CT imaging.15,16,17,18 Nevertheless, in other cases, it is possible that these guidelines could have led to the prescription of a conventional radiograph only. For example, the guidelines of the European Association of Osseointegration state:
'If the clinical assessment of implant sites indicates that there is sufficient bone width and the conventional radiographic examination reveals the relevant anatomical boundaries and adequate bone height and space, no additional imaging is required for implant placement'.16
Therefore, if clinical examination, ridge mapping and the results of conventional radiography had suggested that the site was adequate for dental implant placement, current UK and European guidelines would not have led to the prescription of a CBCT image. These accessory canals are very unlikely to be observed on conventional periapical radiography. Nevertheless, the work of von Arx et al. suggests that accessory canals are present in approximately 28% of patients.10 Therefore, this raises the question of whether cone beam CT imaging should be routinely prescribed before implant placement in the anterior maxilla because of the possible presence of accessory neurovascular canals in the implant site. This would be the position of the American Academy of Oral and Maxillofacial Radiology; whose guidance suggests that CBCT imaging should be used for the assessment of all implant sites.25
Some authors have also recommended three dimensional imaging before dental implant placement in the anterior maxilla. In 2007, Jacobs et al. commented on the complexity of neurovascularisation in the anterior jaw bones. These authors suggested routine cross-sectional imaging, before surgical intervention, to avoid complications such as haemorrhage or sensory disturbance.8 Similarly, in a study of the anatomy of the nasopalatine canal in 2009, Liang et al. recommended preoperative planning using CBCT imaging. Nevertheless, amendment to UK and European guidance would appear to be premature, based on current evidence.
The small risks of developing cancer because of exposure to ionising radiation must be balanced against the benefits of the exposure to the patient. The significance of accessory neurovascular canals in the anterior maxilla remains unclear. Additionally, the financial costs to the patient of performing unnecessary scans has to be considered. Von Arx et al. commented in 2015 on the lack of evidence concerning the clinical significance of surgical damage to canalis sinuosus or its accessory canals.10 Further research is necessary before a change to current UK and European guidelines could be supported on this basis.
Conclusion
This case presented with an accessory neurovascular canal which was surgically unavoidable during dental implant placement and could have potentially led to persistent postoperative pain. It remains the case, however, that evidence about the significance of accessory neurovascular canals with regard to dental implant placement is very limited and we cannot know the consequences if placement had been carried out in this case. Even if there had been intractable pain following implant surgery, there would have still been doubt as to whether damage to nerves in the accessory neurovascular canals was the causative factor. There are several case reports where intractable pain following dental implant placement in the anterior maxilla has been attributed to a psychogenic origin.1,3 Nonetheless, it seems sensible, when aware of the presence of such accessory canals, to proceed with caution. It was fortunate, in this case, that a realistic alternative to implant therapy was easily available. Decision-making, therefore, was relatively straightforward. Nevertheless, this may not be the case for other patients when accessory neurovascular canals are present in the anterior maxilla.
Following the availability of cone beam computed tomography imaging, it has become clear that the neurovascular supply of the anterior maxilla is variable and often complex. Conventional radiography is unlikely to fully demonstrate this.
References
Devine M, Taylor S, Renton T. Chronic post-surgical pain following the placement of dental implants in the maxilla: A case series. Eur J Oral Implantol 2016; 9 (Spec Iss): 179-186.
McCrea S J J. Aberrations Causing Neurovascular Damage in the Anterior Maxilla during Dental Implant Placement. Case Rep Dent 2017; 2017: 5969643.
Patel J, Nixon P. Chronic idiopathic pain following implant placement in the anterior maxilla: a case series. Dent Update 2018; 45: 1043-1047.
Politis C, Agbaje J, Van Hevele J et al. Report of Neuropathic Pain After Dental Implant Placement: A Case Series. Int J Oral Maxillofac Implants 2017; 32: 439-444.
Rodriguez-Lozano F J, Sanchez-Perez A, Moya-Villaescusa M J, Rodriguez-Lozano A, Saez-Yuguero M R. Neuropathic orofacial pain after dental implant placement: review of the literature and case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: e8-e12.
Shaeffer W. A case of intractable pain in the anterior maxilla following dental implant placement: Association of Dental Implantology Members' National Forum. 2015.
de Oliveira-Santos C, Rubira-Bullen I R, Monteiro S A, Leon J E, Jacobs R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin Oral Implants Res 2013; 24: 1044-1048.
Jacobs R, Lambrichts I, Liang X et al. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 683-693.
Torres M G, de Faro Valverde L, Vidal M T, Crusoe-Rebello I M. Branch of the canalis sinuosus: a rare anatomical variation - a case report. Surg Radiol Anat 2015; 37: 879-881.
von Arx T, Lozanoff S, Sendi P, Bornstein M M. Assessment of bone channels other than the nasopalatine canal in the anterior maxilla using limited cone beam computed tomography. Surg Radiol Anat 2013; 35: 783-790.
Wanzeler A M, Marinho C G, Alves Junior S M, Manzi F R, Tuji F M. Anatomical study of the canalis sinuosus in 100 cone beam computed tomography examinations. Oral Maxillofac Surg 2015; 19: 49-53.
Shelley A M, Rushton V E, Horner K. Canalis sinuosus mimicking a periapical inflammatory lesion. Br Dent J 1999; 186: 378-379.
Al-Sabbagh M, Okeson J P, Khalaf M W, Bhavsar I. Persistent pain and neurosensory disturbance after dental implant surgery: pathophysiology, aetiology, and diagnosis. Dent Clin North Am 2015; 59: 131-142.
Renton T. Persistent Pain after Dental Surgery. Rev Pain 2011; 5: 8-17.
Faculty of General Dental Practice. Selection Criteria in Dental Radiography. 3rd ed. London: Faculty of General Dental Practice, 2015.
Harris D, Horner K, Gröndahl K et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A concensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res 2012; 23: 1243-1253.
European Commission. Radiation Protection No 172: Cone beam CT for dental and maxillofacial radiologue (Evidence-based guidelines). 2012. Available at http://www.sedentexct.eu/files/radiation_protection_172.pdf (accessed April 2019).
Horner K, Islam M, Flygare L, Tsiklakis K, Whaites E. Basic principles for use of dental cone beam computed tomography: consensus guidelines of the European Academy of Dental and Maxillofacial Radiology. Dentomaxillofac Radiol 2009; 38: 187-195.
Grey H. Anatomy of the human body. 29th ed. Philadelphia: Lea & Febiger, 1973.
Goodacre C J, Bernal G, Rungcharassaeng K, Kan J Y. Clinical complications with implants and implant prostheses. J Prosthet Dent 2003; 90: 121-132.
Gregg J M. Neuropathic complications of mandibular implant surgery: review and case presentations. Ann R Australas Coll Dent Surg 2000; 15: 176-180.
Maqbool A, Sultan A A, Bottini G B, Hopper C. Pain caused by a dental implant impinging on an accessory inferior alveolar canal: a case report. Int J Prosthodont 2013; 26: 125-126.
Misch C E, Resnik R. Mandibular nerve neurosensory impairment after dental implant surgery: management and protocol. Implant Dent 2010; 19: 378-386.
Park Y T, Kim S G, Moon S Y. Indirect compressive injury to the inferior alveolar nerve caused by dental implant placement. J Oral Maxillofac Surg 2012; 70: e258-e259.
Tyndall D A, Price J B, Tetradis S et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 817-826.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shelley, A., Tinning, J., Yates, J. et al. Potential neurovascular damage as a result of dental implant placement in the anterior maxilla. Br Dent J 226, 657–661 (2019). https://doi.org/10.1038/s41415-019-0260-4
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0260-4
This article is cited by
-
Cone-beam computed tomography of accessory canals of the canalis sinuosus and analysis of the related risk factors
Surgical and Radiologic Anatomy (2024)
-
Anatomical variations and accessory structures in the maxilla in relation to implantological procedures: an observational retrospective study of 212 cases using cone-bean computed tomography
International Journal of Implant Dentistry (2022)