Key Points
-
Suggests that within the referral criteria set, a minor oral surgery service can be provided from an NHS practice setting.
-
Patient satisfaction was high, with short waiting times and low complication rates.
-
Further evaluation is required on other aspects of service quality, particularly efficiency, equity and accessibility.
-
A flexible, collaborative approach between service provider and commissioner is essential.
Abstract
Objectives To evaluate a pilot specialist practice-based minor oral surgery service.
Methods Service monitoring data were analysed to evaluate activity, waiting times and outcomes. Patient satisfaction was assessed by a modified version of the Dental Visit Satisfaction Scale.
Results Of 705 treatment appointments, 12.7% were not attended and treatment was not provided in another 11.6%. Mean waiting time from referral receipt to treatment was 6.8 weeks. Treatment provided included surgical removal of third molars, surgical removal of non-third molars and surgical endodontics (26.7%, 60.4% and 4.9% of cases, respectively). Antibiotics were prescribed in 15.0% of treatment cases and 2.3% of treatment cases required appointments for postoperative complications. The response rate for the satisfaction survey was 81%. All participants reported overall satisfaction and strongly agreed/agreed with positive attitudinal statements about the oral surgeon's communication/information giving, technical competence and understanding/acceptance. 77.8% were seen on time and 22.2% within 15 minutes of their appointment. Overall 74.1% felt the standard of service was better than they would expect from a hospital and none felt it was worse.
Conclusion The findings of the evaluation suggest that specialist minor oral surgery can be successfully provided in dental practice and is acceptable to patients.
Similar content being viewed by others
Introduction
The provision of specialist services in a primary care setting has been increasingly emphasised in health policy1,2,3 and dental modernisation documents.4,5 The new contract for primary dental care in England and Wales introduced opportunities for primary care organisations (PCOs) to locally commission primary care services, including specialist services,6 to meet the needs of their population. The rationale for shifting care from secondary to primary care is to increase its efficiency and accessibility while maintaining other aspects of service quality.
There are relatively few UK data on oral surgery provided in primary care. Those that exist suggest comparable patient outcomes with secondary care,7 reduced waiting times, better accessibility and lower costs.8,9,10 In addition, patients reported satisfaction with such services, citing convenience and familiarity with the surroundings as reasons for this.8,9 However, it is questionable whether these data can be generalised to contemporary NHS services as some were from private practice8 and others were provided by non-specialists or when NHS dentistry was arranged and financed differently.7,9,10 Although specialist primary care oral surgery has been established for some time in mainland Europe, North America and elsewhere, a search of the literature was unable to identify any international data comparing services in primary and secondary care.
As part of the primary care trust's (PCT) commissioning strategy to manage referrals to secondary care and to meet the needs of its population, a pilot primary care oral surgery service was established in Doncaster, South Yorkshire. One of the pilot requirements was to undertake a service evaluation comprising an audit of activity and patient satisfaction. The aim of this paper is to report the findings of the service evaluation of an NHS practice-based specialist minor oral surgery service.
Method
The intervention
All dental practices in the PCT were sent a referral pack which included the case-mix suitable for referral to the service, referral forms, and medical history sheets for completion and signing by the patient. In addition, an information booklet was sent explaining what the patient should expect when attending for surgery, a map of the location of the practice, what to expect following surgery and postoperative instructions. Patients were also asked to sign to confirm that they had read the booklet. With few exceptions, only patients referred using the standard referral forms were accepted for treatment. Where incomplete referrals were received, the referring practitioner was contacted and asked to forward the missing documentation.
On receipt of a referral, the patient was contacted by mail and invited to contact the practice to arrange an appointment. If the patient did not contact the practice within two weeks, a further letter was sent. If after a further four weeks the patient had still not contacted the practice, the referral and radiographs were returned to the referring practitioner.
Most patients were not seen for pre-assessment. The specialist assessed all referrals and a decision to appoint for surgery or assessment was made at that stage. Assessment appointments were requested when there was doubt about the diagnosis or treatment plan. With the exception of endodontic surgery, patients were not routinely reviewed.
The surgical team consisted of a specialist oral surgeon and a dedicated dental nurse (who also dealt with the associated administration). Pre-set, sterilised, basic surgical trays were used. These trays were supplemented with sterile instruments as appropriate (eg forceps, elevators and equipment for surgical endodontics). Before vacuum sterilisation, instruments were washer-disinfected. Non-sterile, latex surgical gloves, disposable drapes and fine suction tips were used. All surfaces were cleaned with alcohol wipes between patients. These procedures were in accordance with infection control and health and safety guidelines at that time.11
Standard straight surgical handpieces with surgical round burs were used with sterile water for irrigation. With the exception of surgical endodontics, antibiotics were not prescribed routinely. The decision to prescribe was based on the clinical judgment of the oral surgeon. Intermediate restorative material was used routinely for retrograde root fillings; however amalgam was used in exceptional circumstances. When required, polyglactin resorbable sutures (Vicryl®) were used.
In addition to pre- and postoperative instructions received before treatment, all patients received verbal and written post-operative instructions at their appointment. These included the practice telephone number in case of post-operative complications. Discharge letters were sent for all patients within one week of treatment and details of any particular follow-up required was also provided.
When specimens were submitted for histopathological examination, patients were informed of the outcome at a review appointment or by telephone when review was not possible and the referring dentist was also informed in writing.
Activity data analysis
Anonymised activity data routinely collected as part of the pilot requirements were analysed for the period of April 2007 to March 2008. Data collected included referring dentist, date of referral, date referral received, date of treatment, number of appointments required for treatment, procedure performed, reasons for non-treatment, failed attendance, antibiotics prescription, and whether a review appointment was arranged or a postoperative complication occurred.
The dataset was imported into Statistical Package for Social Sciences (SPSS) version 15.0 (SPSS Inc., Chicago, USA). Data were cleaned and validated with the service provider and analysed using descriptive statistics.
Patient satisfaction survey
A postal survey of 100 consecutive patients was undertaken using a 16 item questionnaire adapted from the 10 item Dental Visit Satisfaction Scale (DVSS)12 developed by the service provider and the PCT commissioner. Areas of enquiry included patients' perceptions of access, waiting times and interaction with the oral surgeon (including information/communication, understanding/acceptance and technical competence).12 As patients were not routinely assessed before treatment, an additional item was included to ensure that patients perceived they had sufficient time to ask questions about their treatment. A global question on patient satisfaction was included. Finally, a free-text section allowing participants to comment on matters not covered by the questionnaire was provided.
A draft of the questionnaire was piloted prospectively with five participants and re-piloted with a further 20 patients after minor amendments. Both pilots used purposive samples to obtain a broad range of views. The dental team expressed concerns that patients were less likely to be critical immediately after their appointment and that the knowledge that a satisfaction survey was being undertaken may affect their behaviour. Consequently, it was decided to survey retrospectively. To balance feasibility and affordability, a sample size of 100 was agreed between the provider and the commissioner.
Methods identified as maximising response rates from surveys were followed.13 All questionnaires were mailed with a personalised covering letter and a postage paid reply envelope to the University of Sheffield. Mailing was in three stages between November 2007 and January 2008. Questionnaire data were transferred to a spreadsheet for analysis. Ten percent of entries were checked against the source questionnaire for accuracy of transcription. Returned questionnaires with responses for less than 90% of items were excluded from the analysis. Where single items were missing, the response was excluded for that item. Any question answered by less than 90% of respondents was excluded from the analysis. All survey administration including data transfer and analysis was undertaken by researchers independent of the specialist service dental team.
Results
A. Service activity
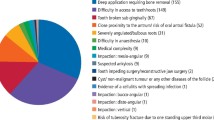
Referrals were received from 51 dentists, with approximately 70% of referrals originating from nine dentists. In total 705 treatment appointments were arranged, of which 12.7% were not attended. Of those attending, 11.6% did not proceed to treatment at the first visit. A further 3.2% of arranged appointments were planned assessments before treatment (Table 1).
Of the 513 surgical procedures performed, the most commonly undertaken was surgical removal of non-third molar teeth (Table 2).
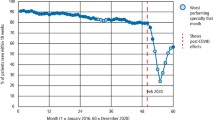
The mean waiting time from receipt of referral to first treatment appointment was 6.8 weeks. Of those treated, 77.0% were treated in one appointment. Only 4.4% of patients required more than two appointments to complete their treatment.
Antibiotics were prescribed postoperatively for 15.0% of patients, of which approximately one third were surgical endodontics cases. Of the 25 surgical endodontic procedures performed, 24 included the prescription of antibiotics (Table 3).
Thirty (5.8%) of patients were reviewed following surgery, of which 25 were for surgical endodontics. Overall, only 12 (2.3%) surgical procedures undertaken required an unscheduled appointment for postoperative complications.
B. Patient satisfaction
Eighty-one of the 100 questionnaires were returned after three mailings; 67% were returned after the first mailing and 7% after each of the second and third mailings.
Of those participating, 77.8% were seen on time and the remainder were seen within 15 minutes of their appointment. When asked about the standard of care received, 74.1% patients felt it was better and 13.5% said it was as good as they would expect from a hospital. None said it was worse.
High levels of satisfaction were reported on items adapted from the DVSS. All but three participants reported satisfaction (strongly agree/agree) with the information provided and their level of understanding of the procedure, what to expect postoperatively, the oral surgeon's affective behaviour and communication skills, and the participants' perception of the quality of care received (Table 4). All participants reported overall satisfaction with care received.
Of the 81 questionnaires returned, 33 participants provided comments on the service. Data were arranged within three themes, which were consistent with Donabedian's dimensions of quality healthcare: 'structure', 'process' and 'outcome'.14 Each will be described in turn with quotations to aid interpretation.
Structure
Two dimensions emerged from the data: accessibility, and facilities and practice environment.
Accessibility
Some participants reported that locating the practice was difficult, which was partly due to administrative oversights:
'I didn't receive a map and found the practice difficult to locate.'
Facilities and practice environment
Some negative views were expressed about specific aspects of the practice's facilities:
'The only problem I had was that the surgery did not have adequate facilities to enable to change my daughter's nappy.'
Another participant perceived that the practice environment could be improved:
'This is a bit picky, but I was surprised by the waiting room, which seemed quite dated and old fashioned compared to my dentist.'
Process
This was the predominant theme to emerge from the data, within which there were three dimensions: affective behaviour, technical competence, and efficiency of service.
Affective behaviour
Positive views were expressed on the communication skills of the oral surgeon:
'I was really nervous about the treatment I was going to have but the oral surgeon really put me at ease, I felt he genuinely cared about me as a person.'
Another commented:
'...who made me feel comfortable and secure. He was friendly and took time to discuss with me all aspects of the problem and treatment procedure.'
Equally positive views were expressed about other members of the dental team:
'The receptionist was lovely, very helpful and very good at her job.'
Technical competence
Participants perceived that the oral surgeon was technically competent:
'...in particular the skill of the oral surgeon.'
'...well-executed by a very competent surgeon.'
Efficiency of service
Participants perceived the service to be efficient:
'Excellent service. No waiting and a straightforward and successful procedure.'
However, some questioned the cost implications to the patient by being treated in primary care:
'...if I received the treatment in hospital would I have to pay for it myself?'
Another complimented the service on its approach to efficiency of delivery, even though this caused inconvenience:
'Unfortunately I was late for my first appointment and the oral surgeon advised I would have to rebook so as not to cause delays to other patients. I admire this, as he really wants to deliver the best for all patients!'
Outcome
Participants reported positive outcomes to their care:
'...Excellent treatment with no after effects ... subsequently healing nicely.'
Discussion
To our knowledge, this is the first evaluation of a NHS specialist minor oral surgery service in primary care under new contractual arrangements. The findings suggest that a range of oral surgical procedures can be performed in a primary care setting with low complication rates and high levels of patient satisfaction. Although the proportion of each procedure undertaken differed, the case-mix and findings are similar to those reported earlier.7,8,9,10
Overall 12.7% patients did not attend appointments and 11.6% of those who attended were not treated after their initial appointment. Although the reasons for patients not proceeding to treatment were recorded (Table 1), nothing is known of the reasons for failed attendance. The rate of failed attendance is at the lower end of the range of that experienced in hospital outpatients departments in the UK15 and is lower than some oral surgery clinics;16 nonetheless this is still an important area of future enquiry, as the efficiency of the service would be improved if the number of patients failing to attend could be reduced. Although NHS contractual arrangements preclude charging for missed appointments, measures to minimise failed appointments were already in place. For example, patients were only offered appointments once they had contacted the practice. Other measures could include reminder telephone calls and text messaging. Although both methods are effective in general healthcare,17 their effectiveness in dentistry is unclear and would increase the administrative burden.
Stricter application of referral criteria and improved patient assessment by referring dentists could reduce the number of patients not proceeding to treatment. For example, a large proportion of those identified as inappropriate referrals or where symptoms had resolved had been referred for the removal of lower third molars and did not meet NICE guidelines. Similarly those patients who were referred to secondary care were often for reasons of dental anxiety which could have been identified by the referring practitioner. As patients referred were often irregular attenders (13.2% of all referrals were patients who had originally requested emergency appointments at the local dental access centre) who are often dentally anxious,18,19,20 assessing such patients' suitability for treatment with local anaesthesia can be problematic for referring dentists. Arguably they are also more likely to fail to attend for treatment if their symptoms resolve before their appointment.
In the light of earlier data8,21,22, postoperative review appointments were not routinely arranged. Only 12 (2.3%) patients attended with postoperative complications. As the diagnosis at the review appointment was not recorded in the database, it is not possible to directly compare these data with published complication rates. If it is assumed that all postoperative complications were alveolar osteitis ('dry socket'), the incidence would still compare favourably with those from secondary care.23,24 As the case-mix of patients would vary between sectors and patients may have sought the care of their own dentists postoperatively, these data may not be directly comparable. However, all patients treated were instructed to contact the service if complications were experienced, which was reinforced in written postoperative instructions. Furthermore, the patient satisfaction survey did not identify problems with postoperative complications.
As antibiotics have questionable effectiveness in preventing postoperative complications,25,26 they were not routinely prescribed. The decision to prescribe was based on the procedure undertaken (antibiotics were routinely prescribed postoperatively for surgical endodontics), surgical complexity, existing infection and history of complications following tooth removal. Only 15.0% of all procedures included antibiotic prescription, 31.1% of which were for surgical endodontics.
This study identified high levels of patient satisfaction with the service – approximately three quarters of participants perceived the service to be better than they would expect to receive in a hospital and all reported overall satisfaction. The findings are consistent with earlier research which reported satisfaction with oral surgery provided in primary care.8,9 Bell8 and Clark9 cited various reasons for this, including a simplified appointment process, shorter waiting times, familiarity and personal nature of the service and their geographical convenience, which are consistent with the findings reported here. However, patient satisfaction surveys often report high levels of satisfaction, even when further investigation reveals dissatisfaction with aspects of a service.27,28 Various explanations for this have been suggested, including patients' unwillingness to offend their practitioners.27,28 As the oral surgeon was not the patient's regular practitioner and the survey was undertaken retrospectively and anonymously, such risks should have been minimised. Nonetheless, as the theoretical and methodological difficulties of assessing patient satisfaction have been well documented,27,28,29 any future evaluation should include a mixed method approach to assess the acceptability of the service.29,30
All patients referred were offered appointments that were convenient for them and more than 75% were treated at their first appointment. The qualitative data suggested satisfaction with the perceived efficiency of the service, possibly as a result of patients not routinely being assessed before treatment. Coulthard et al.31 reported dissatisfaction among GDPs with hospital-based oral surgery, citing waiting times, lack of accessibility and having to attend for multiple appointments for their care as causes. As 51 out of 105 dentists in this health community referred patients to the service, many practitioners appear to be satisfied with the service. However, nothing is known of why some practitioners do not refer. Similarly, the views of dentists who do refer on the quality of the service provided are unknown. Both would be areas for future inquiry.
The referral criteria applied to this pilot minor oral surgery service resulted in a case-mix largely restricted to dentoalveolar surgery, reflecting the commissioning needs of the local PCT. Specialist services could provide a wider range of oral surgery and oral medicine care where there is a commissioning need. Ideally all such services should operate as part of a clinical network including commissioners and clinicians from primary and secondary care.
Other NHS practice-based specialist services have been reported as being more cost-effective than those in secondary care.10 However, this study was undertaken under different contractual and remunerative arrangements. Previously, contractual constraints and lack of funding have been seen as barriers to providing such services in primary care,8,9 potentially increasing the likelihood that specialist services would be restricted to the private healthcare market. As well as increasing patient costs this could also create inequity of access. It is noteworthy that one patient inquired whether they would have to pay for treatment if it were provided in secondary rather than primary care. This implies that the patient charge levied in primary care may reduce the affordability of the service for some. Currently, secondary care services charge PCTs for treatment but there does not appear to be a consistent charging structure. Anecdotal reports suggest that tariff costs for minor oral surgery vary depending on how the hospital codes the procedures. Consequently, although shifting specialist services to primary care has the potential to improve efficiency, rigorous health economic analysis is still required.
Any service evaluation should consider all dimensions of the quality of the service. Maxwell identified six dimensions:32 effectiveness, efficiency (value for money), equity (is the service fairly applied?), social acceptability (is the service acceptable to patients and other stakeholders?), accessibility and appropriate to need. This service evaluation has covered most of these dimensions, though more emphasis could be placed on the assessment of efficiency, equity and accessibility. The areas identified for future enquiry should deliver a more comprehensive service evaluation of all aspects of quality.
Conclusion
A specialist minor oral surgery service can be successfully provided in NHS primary care. A range of procedures was provided, waiting times and complication rates were low and patient satisfaction was high. Any future evaluation should consider other aspects of quality, particularly efficiency, equity and accessibility of the service.
References
Department of Health. World class commissioning. London: Department of Health, 2007. [Available online: http://www.dh.gov.uk/en/Managingyourorganisation/Commissioning/Worldclasscommissioning/index.htm, accessed 12.02.09].
Department of Health. Commissioning a patient-led NHS. London: Department of Health, 2005. [Available online: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4116716, accessed 12.02.09].
Department of Health. The NHS plan: a plan for investment, a plan for reform. London: Department of Health, 2000. [Available online: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyandGuidance/DH_4002960, accessed 12.02.09].
Department of Health. NHS dentistry: options for change. London: Department of Health, 2002. [Available online: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4008017, accessed 12.02.09].
Department of Health. Modernising NHS dentistry: implementing the plan. London: Department of Health, 2000. [Available online: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002931, accessed 12.02.09].
Department of Health. Primary care dental services: commissioning specialist dental services. London: Department of Health, 2005. [Available online: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4123971, accessed 12.02.09].
Wood G D, Corcoran J P . Oral surgery specialisation in general practice. Br Dent J 1988; 164: 331–333.
Bell G. An audit of 600 referrals to a primary care based oral surgery service. Br Dent J 2007; 203: E6.
Clark S. The patient's view of minor oral surgery in dental practice. Br Dent J 1995; 179: 71–73.
Sadler A, Davidson M, Houpis C, Watt Smith S . Specialist practice for minor oral surgery: a comparative audit of third molar surgery. Br Dent J 1993; 174: 273–277.
British Dental Association. Advice sheet A12: infection control in dentistry. London: BDA, 2003.
Corah N L, O'Shea R M, Pace L F, Seyrek S K . Development of a patient measure of satisfaction with the dentist: the Dental Visit Satisfaction Scale. J Behav Med 1983; 7: 367–373.
Edwards P, Roberts I, Clarke M et al. Methods to influence response rates to postal questionnaires. Cochrane Database Syst Rev 2007; 2: MR000008.
Donabedian A. Evaluating the quality of medical care. Millbank Quart 1966; 44: 166–206.
Anon. Did not attend. Bandolier November 1999. [Available online at: http://findarticles.com/p/articles/mi_m5LWU/is_11_6/ai_n25027476/?tag=content;col1, accessed 24.11.09].
Trenmouth M J, Hough A . Reasons for broken and cancelled appointments in a British orthodontic clinic. J Clin Orthod 1991; 25: 115–120.
Traina S, MacLean C, Park G, Kahn K . Telephone reminder calls increased response rates to mailed study consent forms. J Clin Epidemiol 2005; 58: 743–746.
Wyborn C, Marshman Z, Dyer T A, Godson J, Beal J . The dental health of adults in Yorkshire and Humber 2008. York: The Yorkshire and Humber Public Health Observatory, 2009.
Kelly M, Steele J, Bradnock G et al. Adult dental health. Oral health in the United Kingdom 1998. London: The Stationery Office, 2000.
Milsom K M, Jones C, Kearney-Mitchell P, Tickle M . A comparative needs assessment of the dental health of adults attending dental access centres and general dental practices in Halton & St Helens and Warrington PCTs 2007. Br Dent J 2009; 206: 257–261.
Irvine G H, Hepangama N . Post-operative follow-up following the removal of wisdom teeth. Br Dent J 1998; 185: 565–566.
Oldham R, Boyles J . Post-operative review. Br Dent J 1999; 186: 210, 212.
Heasman P A, Jacobs D J . A clinical investigation into the incidence of dry socket. Br J Oral Maxillofac Surg 1984; 22: 115–122.
Osbourne P T, Frederickson G, Small A I, Torgerson S T . A prospective audit of complications related to mandibular third molar surgery. Br J Oral Maxillofac Surg 1985; 43: 767–769.
Lawler B, Sambrook P J, Goss A N . Antibiotic prophylaxis for dentoalveolar surgery: is it inidicated? Aust Dent J 2005; 50 (Suppl 2): S54–S59.
Monaco G, Staffolani C, Gatto M R, Checchi L . Antibiotic therapy in impacted their molar surgery. Eur J Oral Sci 1999; 107: 437–441.
Locker D, Dunt D . Theoretical and methodological issues in sociological studies of consumer satisfaction with medical care. Soc Sci Med 1978; 12: 283–292.
Calnan M. Towards a conceptual framework of lay evaluation of health care. Soc Sci Med 1988; 27: 927–933.
Sitzia J, Wood N . Patient satisfaction: a review of issues and concepts. Soc Sci Med 1997; 45: 1829–1843.
Schneider H, Palmer N . Getting to the truth? Researching user views of primary health care. Health Policy Plan 2002; 17: 32–41.
Coulthard P, Koron R, Kazakou I, Macfarlane T V . Patterns and appropriateness of referral from general dental practice to specialist oral and maxillofacial surgical services. Br J Oral Maxillofac Surg 2000; 38: 320–325.
Maxwell R J. Quality assessment in health. BMJ 1984; 288: 1470–1471.
Acknowledgements
The authors would like to thank Dr Zoe Marshman, Mr Paul Stones and Professor Peter G. Robinson for their comments on drafts of the paper. They would also like to extend thanks to Mrs Claire Cooper for administering the patient satisfaction survey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Dyer, T., Dhamija, A. Evaluation of an NHS practice-based minor oral surgery service. Br Dent J 207, 577–582 (2009). https://doi.org/10.1038/sj.bdj.2009.1136
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.1136