Abstract
Aims To report the oral surgery referral to treatment waiting times in hospitals in England and to identify any trends in the percentage of patients seen within 18 weeks.
Materials and methods Data published by the NHS statistics team was analysed from 2016-2020.
Results Pre-COVID-19, the best performing month was February 2016, with 91.5% of patients seen within 18 weeks. The worst performing month was September 2019, with 79.3% of patients seen within 18 weeks. Oral surgery was the worst performing speciality for 8% of months (4/50). Post-COVID-19, oral surgery was the worst performing speciality for 70% of months (7/10). In July 2020, the percentage of patients seen within 18 weeks of an oral surgery referral dropped to 24%.
Discussion Over the last five years, there has been a steady decline in the number of patients who have been seen within 18 weeks of their oral surgery referral. There has also been an increase in oral surgery referrals to secondary care which needs to be addressed.
Conclusion Improvements to undergraduate and postgraduate training, combined with enhanced commissioning of primary care services, is required.
Key points
-
An assessment of trends with respect to oral surgery wait times over a five-year period.
-
Considerations to reduce oral surgery wait times in secondary care.
-
To raise awareness of NHS dental wait times in secondary care for general dental practitioners.
Similar content being viewed by others
Introduction
In the NHS Constitution for England and its accompanying Handbook, emphasis is placed on patients having the right to start their consultant-led treatment within a maximum of 18 weeks of a referral for non-urgent conditions.1 On a daily basis, general dental practitioners (GDPs) refer their patients through this 18-week pathway. This provides access to secondary care experts in numerous fields, including but not limited to: oral and maxillofacial surgery (OMFS), restorative dentistry, paediatric dentistry and oral surgery.
Operationally, the NHS expects that 92% of those on a waiting list at any point in time should have been waiting for less than 18 weeks.2 Throughout the NHS, this 92% target has not been met since March 2016 and with an increasing number of people on the waiting list for treatment, an inspection of dental waiting times is required.
The NHS statistics team publishes monthly data on consultant-led referral to treatment (RTT) waiting times in hospitals in England.3 The RTT data allows measurement of waiting times (by % of patients seen within 18 weeks) from the referral date to the start of the first definitive treatment appointment at treatment speciality level. Measuring this data allows the NHS to evaluate access to services and see whether high quality elective care is provided without delay.
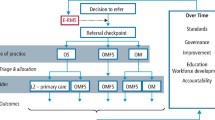
Currently within dentistry, oral surgery is the only speciality for which consultant-led RTT data is collected and then defined within its own Treatment Function Code. Due to the overlapping nature, some OMFS coding falls within the oral surgery Treatment Function Code. It is important to note that data is collected for other specialties such as OMFS, restorative dentistry and paediatric dentistry. However, these are banded together, with numerous other medical sub-specialties in the 'other' Treatment Function Code, as shown in Table 1. The RTT pathway can also be started if a patient is referred to a 'referral management service', where they can be seen by a practitioner with a specialist interest.4
The aim of this study was to carry out an analysis of oral surgery RTT waiting times in all hospitals in England and to identify any trends in the percentage of patients seen within 18 weeks.
Materials and methods
This study was a five-year retrospective data analysis of oral surgery RTT waiting times in England between January 2016 and December 2020.
The span of the study was influenced by the Guide for commissioning oral surgery and oral medicine which was published in September 2015 and describes the routes to commissioning dental specialist services.5 In order to allow for the implementation of new commissioning practices, a five-year period was chosen starting from January 2016.
Data was collected retrospectively, using online monthly published figures from the NHS statistics team.6,7,8,9,10,11 For each month, the 'Incomplete Commissioner' Excel spreadsheet files were downloaded and the following data was extracted:
-
The percentage (%) of patients seen within 18 weeks in oral surgery
-
Whether oral surgery was the worst-performing speciality from all of the specialties listed in Table 1. The worst performing speciality was defined as 'the speciality which had the lowest percentage of patients seen within 18 weeks, on any particular month'.
Note, some hospitals in England do not contribute to the RTT data and this information can be found within the published files.
Results
Data for the percentage of patients seen within 18 weeks following an oral surgery referral was collected for all 60 months. This was broken down into pre-COVID-19 and post COVID-19 data, as shown in Figure 1.
Pre-COVID-19 was the period from January 2016 up to and including February 2020; a total of 50 months. The best performing month was February 2016, with 91.5% of patients seen within 18 weeks. The worst performing month was September 2019, with 79.3% of patients seen within 18 weeks. Between July 2018 and October 2018, for four consecutive months, oral surgery was the worst-performing speciality. This accounted for 8% of months (4/50).
The post COVID-19 period was from March 2020 to December 2020, a total of ten months. During this time, 70% of months (7/10), showed oral surgery to be the worst performing speciality. In July 2020, the percentage of patients seen within 18 weeks of an oral surgery referral dropped down to 24%.
Overall, of the 19 specialties, only four contributed to having the lowest percentage of patients seen within 18 weeks on any given month. Neurosurgery was the worst performing speciality in 55% of months (33/60) followed by plastic surgery, which was the worst performing in 25% of months (15/60). Oral surgery was the worst-performing speciality in 18.33% of months (11/60) and ear, nose and throat (ENT) was the worst performing in 1.66% of months (1/60).
For any given month, the data collected for oral surgery showed a consistent 5-year decline in the percentage of patients seen within 18 weeks (see Figure 2).
Discussion
This review shows that in the four-year period from January 2016 to December 2019, there was a noticeable decline in the percentage of patients seen within 18 weeks in oral surgery. In early 2016, over 90% of patients were regularly seen within 18 weeks, compared to the end of 2019, where less than 80% were seen within the same timeframe. While the reason for this downward trend cannot be attributed to a single cause, there has been an increase in oral surgery referrals from primary care to secondary care.12 Jadun et al. proposed a number of reasons for this increase, including: a larger UK population; patients keeping their teeth longer and requiring treatment when they have more complex medical needs; and an increase in litigation resulting in defensive referrals.
In March 2020, the entirety of the UK went into lockdown due to COVID-19. In the same month, the British Association of Oral and Maxillofacial Surgeons and the British Association of Oral Surgeons released joint guidance on treating patients during this difficult time.13 They stressed the importance of using appropriate personal protective equipment, which included FFP3 masks for all oral examinations and aerosol generating procedures. Furthermore, their recommendation was to only treat emergency/urgent cases and to triage patients appropriately, providing advice, analgesia and antibiotics if necessary. All of these factors inevitably led to the percentage of patients seen within 18 weeks in oral surgery during the pandemic to plummet.
Access
Interestingly, throughout this 5-year period, all specialties saw a gradual decline in the percentage of patients seen within 18 weeks. In January 2016, the average for all specialties was 92%. Towards the end of 2019 and before COVID-19 was a factor, the average for all specialties was below 84%. With a record number of patients on waiting lists for routine operations and procedures, the entire NHS is facing a patient access problem which has been exacerbated by COVID-19.14
A recent Healthwatch report has shown that patients continue to struggle to access NHS dental treatment.15 This has worsened since COVID-19 and the proportion of positive feedback regarding dentistry has fallen. One recommendation from this report is the need for rapid and radical reform in the way NHS dentistry is commissioned, which would allow for greater patient access.
Oral surgery and commissioning
Oral surgery is one of the 13 General Dental Council-recognised dental specialties.16 In August 2019, when the number of specialists in dentistry was reviewed, there were 741 specialist oral surgeons in the UK.17 This was the second highest figure among specialties, with orthodontics having 1,384 registrants on the specialist list. For the same year, in England, oral surgery had the highest number of hospital appointments of any dental speciality, with 956,286 appointments.18
The previously mentioned Guide for commissioning oral surgery and oral medicine describes the three different complexity levels in oral surgery. Level 1 procedures are those that can be carried out by foundation dentists and GDPs. Level 2 procedures require clinicians to have enhanced skills and these clinicians may or may not be on the specialist list. For those not on the specialist list, enhanced skills are acquired through dental core training posts or postgraduate study. Finally, Level 3 procedures are those which require management by a specialist or consultant.5
The commissioning guide states that most Level 1 and Level 2 procedures can be carried out in primary care. This has led to the creation of Tier 2 minor oral surgery (MOS) contracts which offer Level 2 procedures, including intravenous sedation and specialist care in general practice.
Improving oral surgery services
Based on current oral surgery capacity, decline in patients being seen within 18 weeks and commissioning recommendations, the following are suggestions made to help improve waiting times.
More exposure to oral surgery during undergraduate training
Oliver et al.19 found that, of their 649 respondents, the most common skill deficiency at undergraduate level was in oral surgery. They also reported that more recent graduates were less satisfied with undergraduate teaching of surgical extractions when compared to established practitioners. When looking at undergraduate experience in oral surgery, Brown et al.20 also found that students showed a lack of confidence in surgical extractions. Students noted that more clinical experience at university would have better prepared them for oral surgery in practice.
Implementing a higher number of performed and assisted non-surgical and surgical extractions, at a variety of difficulty levels, as well as increasing the time spent in oral surgery hospital placements, would help improve training.
More accessible postgraduate training in oral surgery
Firstly, dental foundation trainees (DFTs) should have access to multiple oral surgery study days with specialist oral surgeons, where they can develop their existing skills. This would allow DFTs to have the confidence to be able to carry out simple surgical extractions independently, something which not all DFTs currently have the opportunity to do.21
Secondly, developing more oral surgery-specific dental core training posts would increase the number of clinicians with enhanced skills. Improving access and offering part-funding for postgraduate certificates and diplomas in oral surgery or conscious sedation would also allow more clinicians to work at a higher competency level and thus reduce referrals into secondary care.
Increasing oral surgery speciality training posts
In 2015, the commissioning guide stated that there were 755 registered oral surgeons. Four years later, in 2019, the GDC's report Principle of specialist listing stated that there were 741 specialists.17
The number of specialists has remained fairly static. With more patients being referred for oral surgery services and a decline in the number of patients seen within 18 weeks, a well-planned increase in the number of posts now may help alleviate this pressure.
Utilising Tier 2 minor oral surgery services
Hospital outpatient clinic capacity and theatre space have always been limiting factors for service provision. This has resulted in Tier 2 services for some specialties, including oral surgery and endodontics. Thomas et al.22 found that of 401 referrals to an NHS Tier 2 service for endodontics, nearly all referrals could have been dealt with by Tier 2 practitioners, with only 3.5% of patients requiring additional consultant input.
The National Institute for Health Research suggest that with an advanced oral surgery service in primary care, two-thirds of patients could be treated in practice rather than hospital.23 Benefits of this would include cost savings when compared to secondary care treatment and shortened waiting times for patients.
Expansion of local Tier 2 MOS services would be the most practical recommendation to implement, as current Tier 2 MOS services are found in the heart of communities and treatment is provided by a highly skilled workforce. This would appropriately redirect many patients destined for secondary care to more local and economical services.
Limitations
Using secondary data from the NHS limits the scope of what can be investigated. Ideally, RTT data from oral surgery would be compared to data from other dental specialities, which we do not have. Furthermore, there was no control over how data was input at the source. This data is an amalgamation of hundreds of different clinicians subjectively coding their treatment outcomes. This may result in some patients being inappropriately coded into oral surgery rather than OMFS and vice versa.
Further research is required and the dataset published by the NHS statistics team can be further analysed by regional performance.
Conclusion
There has been a steady decline in the percentage of patients seen within 18 weeks of an oral surgery referral, from over 90% in 2016, to below 80% in 2019. COVID-19 has presented additional challenges and there is an increased backlog of patients requiring oral surgery services. Further education and training of dentists, along with novel approaches to service management, are required to bring levels back up to 2016 standards.
References
Public Health England. Handbook to the NHS Constitution for England. 2021. Available at https://www.gov.uk/government/publications/supplements-to-the-nhs-constitution-for-england/the-handbook-to-the-nhs-constitution-for-england (accessed March 2021).
House of Commons Library. NHS Key Statistics: England, February 2020. 2020. Available at http://allcatsrgrey.org.uk/wp/download/health_services/CBP-7281_2.pdf (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times. 2021. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/ (accessed March 2021).
Maidstone and Tunbridge Wells NHS Trust. Patient Access to Treatment Policy and Procedure (RTT 18 weeks). 2016. Available at https://www.mtw.nhs.uk/wp-content/uploads/2015/08/Patient_access_RTT_18_weeks.pdf (accessed June 2021).
NHS England. Guide for Commissioning Oral Surgery and Oral Medicine. 2015. Available at https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/09/guid-comms-oral.pdf (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2015-16. 2016. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2015-16/ (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2016-17. 2017. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2016-17/ (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2017-18. 2018. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2017-18/ (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2018-19. 2019. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2018-19/ (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2019-20. 2020. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2019-20/ (accessed March 2021).
NHS England. Consultant-led Referral to Treatment Waiting Times Data 2020-21. 2021. Available at https://www.england.nhs.uk/statistics/statistical-work-areas/rtt-waiting-times/rtt-data-2020-21/ (accessed March 2021).
Jadun S, Syed N, Drabu T, Yates J. Patient awareness and quality of oral surgery referrals to specialist practice. Oral Surg 2019; 13: 99-107.
British Association of Oral and Maxillofacial Surgeons and British Association of Oral Surgeons. Guidance PPE for patients with emergency oral problems of unknown COVID-19 Status. 2020. Available at https://www.baos.org.uk/wp-content/uploads/2020/03/no-wm-BAOMS-BAOS-COVID-Advice-Update-24-March-20191.pdf (accessed March 2021).
O'Dowd A. NHS waiting list hits 14 year record high of 4.7 million people. BMJ 2021; DOI: 10.1136/bmj.n995.
Healthwatch. What people have told us about NHS Dentistry. 2021. Available at https://www.healthwatch.co.uk/sites/healthwatch.co.uk/files/reports-library/20211014_HWE%20Dentistry%20Update%20Dec%202021.pdf (accessed July 2021).
General Dental Council. Specialist lists. 2019. Available at https://www.gdc-uk.org/registration/your-registration/specialist-lists (accessed April 2021).
General Dental Council. Principles of specialist listing: Consultation outcome report. 2019. Available at https://www.gdc-uk.org/docs/default-source/consultations-and-responses/principles-of-specialist-listing---consultation-outcome-report.pdf?sfvrsn=85d0d175_2 (accessed April 2021).
NHS Digital. Hospital Outpatient Activity 2019-20. 2020. Available at https://digital.nhs.uk/data-and-information/publications/statistical/hospital-outpatient-activity/2019-20 (accessed April 2021).
Oliver G R, Lynch C D, Chadwick B L, Santini A, Wilson N H F. What I wish I'd learned at dental school. Br Dent J 2016; 221: 187-194.
Brown J, Baker R, Moore R. An investigation into the oral surgery curriculum and undergraduate experience in a sample of DFT's in the UK. Eur J Dent Educ 2020; 25: 421-434.
Ross J, Baker S R. Perceptions of foundation dentists on minor oral surgery teaching in dental foundation training. Eur J Dent Educ 2019; 23; 405-414.
Thomas G M, Newton R, Tolley W J, Bishop K. Novel tier 2 service model for complex NHS endodontics. Br Dent J 2021; DOI: 10.1038/s41415-021-2840-3.
National Institute for Health Research. Redesigning oral surgery with enhanced primary dental care, electronic referral and triage may save overall costs. 2018. Available at https://evidence.nihr.ac.uk/alert/redesigning-oral-surgery-with-enhanced-primary-dental-care-electronic-referral-and-triage-may-save-overall-costs/ (accessed April 2021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The author declares no conflicts of interest.
Rights and permissions
About this article
Cite this article
Ehsan, O. Oral surgery wait times in NHS secondary dental care in England: a five-year review. Br Dent J (2022). https://doi.org/10.1038/s41415-022-4138-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-022-4138-5
This article is cited by
-
Addressing oral health inequities in rural communities: a call to action
British Dental Journal (2023)
-
Accreditation pathway for oral surgery
British Dental Journal (2023)