Abstract
Study design:
A retrospective study.
Objectives:
The objectives of the study were to investigate the predictors for hyponatraemia in patients with cervical spinal cord injuries (CSCIs) and to define the relationship between magnetic resonance imaging (MRI) scans and hyponatraemia.
Setting:
The study was carried out at The First Affiliated Hospital of Anhui Medical University.
Methods:
A total of 292 patients with CSCIs were retrospectively reviewed to determine the predictors of hyponatraemia. Fourteen variables were extracted from the medical records: age, sex, blood pressure (BP), tracheostomy, serum potassium, serum chloride, serum bicarbonate, serum albumin, intravenous fluid intake and urine volume for 24 h, haematocrit, haemoglobin, neurological assessment and four MRI signal patterns. Univariate and multivariate analyses were used to determine the effect of each variable on hyponatraemia.
Results:
Eighty-two of the 270 patients (30%) developed hyponatraemia. Univariate analyses indicated that the following variables were significant predictors of hyponatraemia: tracheostomy; the initial American Spinal Injury Association (ASIA) Impairment Scale (AIS) A assessment; and haemorrhage changes on T2-weighted MRI scans, and low BP. Multivariate regression analyses revealed two variables were significant predictors of hyponatraemia: haemorrhage changes on T2-weighted MRI scans and low BP.
Conclusions:
Haemorrhage changes on MRI scans were closely associated with the onset of hyponatremia and could provide objective data for forecasting hyponatraemia in CSCI patients. Low BP was also a reasonable predictor of hyponatremia.
Similar content being viewed by others
Introduction
In addition to motor and sensory deficits, hyponatraemia, which is defined as a serum sodium concentration <135 mmol l−1, is frequently seen in patients suffering from a cervical spinal cord injuries (CSCI),1, 2 and the occurrence is 29–86% according to previous studies.3, 4, 5, 6 Many studies have detailed how hyponatraemia can lead to a variety of signs and symptoms including nausea, vomiting, disorientation, headaches and even potential physiological changes.4, 7 Severe hyponatraemia is a life-threatening condition that has long been known to be closely associated with increased mortality in CSCI patients.4, 7, 8
Hyponatraemia after a CSCI may result from autonomic nervous system (ANS) dysfunction. Impairment of the ANS decreases the peripheral vascular resistance and results in chronic hypotension, which may stimulate the secretion of antidiuretic hormone (ADH). Thus, water is retained in the body after CSCIs.3, 9, 10 In addition to inappropriate secretion of ADH, dysfunction of the ANS also impacts kidney function. When the renal sympathetic innervation of the kidney is impaired, tubular secretion of angiotensin II, which controls renal blood flow, and the renin production through the juxtaglomerular granular cells are damaged, which reduces tubular reabsorption of both Na+ and water.8 Therefore, impairment of the central nervous system may lead to either water retention, salt wasting or a combination of the two.5, 11
Previous studies have reported certain risk factors for hyponatraemia in CSCI patients, including low BP, severe paralysis, other electrolyte disturbances (serum potassium, serum chloride) and excessive water intake.4, 7 However, these factors might have many confounders. For example, BP could be easily affected by lots of factors such as pain, haemorrhagic shock, history of renal disease and/or hypertension. The occurrence of electrolyte disturbances might not always be present either before hyponatremia or in the acute phase of a spinal cord injury (SCI). Daily fluid intake might be difficult to calculate precisely due to difficulties in gathering precise collection numbers from patients. Therefore, a method that could provide objective data for forecasting hyponatraemia in the early stages of an SCI is needed.
Magnetic resonance imaging (MRI) is now frequently used in SCI cases.12, 13, 14, 15, 16, 17 It allows for better visualisation of soft tissues, such as the spinal cord, discs and ligaments, when compared with either radiographs or computerised tomography scans. It can also help determine both the CSCI mechanism and the extent of neurological damage. In patients with CSCI, signal changes on MRI scans suggest injury to the spinal cord and these changes are not easily affected by other factors. Notably, the data found on MRI are achievable in the early stages of a CSIC. Previous studies have reported that the different signal changes on MRI are associated with quite different prognoses. Moreover, recent studies have found that the presence of hypointensities in T2-weighted MRI scans (haemorrhage changes) to be closely associated with respiratory complications, which is another frequent complication of CSCIs.18 Therefore, we hypothesise that the haemorrhage changes on MRI scans may have a relationship with hyponatremia in patients with CSCI. This study proposes to determine both the predictors of hyponatraemia and to define the relationship, if any, between MRI results and hyponatraemia.
Methods
Study data
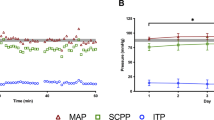
This study’s subjects included 292 patients who underwent medical treatment in the Department of Spinal Surgery of The First Affiliated Hospital of Anhui Medical University, in Hefei, China, from 1 January 2013 to 31 May 2016. The inclusion criteria were a serum sodium level below the limit of 135 mmol l−1 at any time during treatment in the department. The exclusion criteria included the following: (1) other polytrauma; (2) history of renal diseases; (3) neurological diseases that could lead to autonomic dysfunction (Parkinsonism, Shy–Drager syndrome) and (4) patients who did not undergo an MRI scan within days of injury. Demographic data included age and sex. In the current study, BP was measured and recorded at least five times per day before the occurrence of hyponatremia and the average systolic BP on each day was calculated, respectively. Following previous studies, an average systolic BP below 90 mm Hg or the need for intravenous administration of crystalloids and vasopressors was defined as low BP.3, 8 Both intravenous fluid intake and urine volume were collected for 24 h before the onset of hyponatraemia and the mean daily data of these volumes were calculated, respectively. Blood parameters (electrolyte, albumin, haematocrit and haemoglobin) were collected every day before the onset of hyponatraemia and the minimum of these data were recorded (Table 1). To prevent laboratory errors, we repeated the blood tests immediately on the same day to negate the occurrence of any abnormal blood data.
Patients were routinely discharged after the medical treatment in the department. The patients visited the outpatient clinic at 3, 6, 9 and 12 weeks post SCI and then twice per year after that. This study was approved by the Ethics Committee of The First Affiliated Hospital of Anhui Medical University.
Neurological examination
Using the American Spinal Injury Association (ASIA) impairment scale (AIS), two neurosurgeons examined patients to determine their initial neurological impairment at the time of admission ('the initial AIS grade'). To evaluate their neurological improvements, we also reassessed the AIS grade 4 weeks after the CSCI ('the final AIS grade'). The 4-week timeframe selected to reassess the AIS grade was based on the end of spinal shock, which was interpreted as the recovery of deep tendon and bulbocavernosus reflexes.19 In addition, the neurological level of injury (NLI) in patients with a CSCI was examined upon admission. The NLI was the most caudal segment where both sensory function and motor function were intact.
Radiological data
All patients underwent an MRI scan within 3 days of their injuries. On the basis of previous studies, there were four signal patterns on the T2-weighted MRI that could describe nearly all the entire spectrum of spinal cord injuries.12 They were normal cord, single-level oedema, multi-level oedema and haemorrhage (Figure 1). One radiologist and one neurosurgeon assessed the CSCI patients’ MRI signal patterns and determined each spinal cord injury level (IL) and the highest MRI signal change level (HL) according to the following rules: (1) when signal changes on MRI scans were absent, the IL and HL were determined according to the segment of spinal instability, bone fracture and cervical disc injury; (2) for single-level oedema (indicated as a hyperintense core in a T2-weighted image), the centre of the hyperintense core was selected as the CSCI IL and the HL on the MRI; (3) for multi-level oedema, the centre of a wider-ranging hyperintensity area was selected as the IL and the highest segment of the hyperintensity as the HL; and (4) when haemorrhage and oedema were both present on the MRI, which was observed as a hypointense core surrounding a wider-ranging hyperintensity area, the hypointense core was selected as the IL and the highest segment as the HL on the MRI (Figure 1).
Four signal patterns and the level of injury on MRI. (a) C3 fracture without signal changes on MRI. (b) Single-oedema (C6-7). (c) Multi-oedema from C2/3 to C6 with ossification of posterior longitudinal ligament. The injury level on MRI images was 'C4,' and the highest signal changes were at C2/3. (d) Haemorrhage surrounded by oedema at C4 with a C4/5 disc injury. The injury level on MRI images was 'C4,' and the highest signal changes were at C3. A full colour version of this figure is available at the Spinal Cord journal online.
Statistical analysis
The following variables were evaluated retrospectively by univariate logistic regression analysis: (1) age, (2) sex, (3) BP, (4) tracheostomy, (5) serum potassium, (6) serum chloride, (7) serum bicarbonate, (8) serum albumin, (9) intravenous intake and urine volume for 24 h, (10) haematocrit, (11) haemoglobin and the neurological assessment and radiological parameters stated above. To prevent missing potential predictors, P<0.10 was considered statistically significant in the univariate logistic regression analyses. Multiple logistic regression analyses were used to calculate the adjusted estimates of the relationship between hyponatraemia and each variable, which showed significant differences from the univariate analyses. For all variables used in the logistic regression, both the data type and coding methods are presented in Table 2. The Pearson correlation coefficient was used to test the correlation between these two variables. The accuracy of the predictors of hyponatraemia (sensitivity, specificity and accuracy rate) was also calculated.
Statistical analyses were performed using SPSS 16.0 software (Chicago, IL, USA) and P<0.05 was considered statistically significant. Estimates of the relationship were described as odds ratios with 95% confidence intervals.
Results
In total, 270 patients (214 males and 56 females) with CSCIs were treated at our hospital over a 3-year period. The range of serum sodium was from 109.2 to 134.5 mmol l−1 (mean, 127.6 mmol l−1). The times to occurrence of hyponatraemia ranged from 0 to 27 days after CSCI (mean 5.7 days). Patient characteristics are summarised in Table 1.
The extent of neurological impairment upon admission was graded as AIS A in 58 patients (22%), AIS B in 25 patients (9%), AIS C in 73 patients (27%), AIS D in 71 patients (26%) and AIS E in 43 patients (16%), respectively. The final grade was AIS A in 46 patients (17%), AIS B in 24 patients (9%), AIS C in 65 patients (24%), AIS D in 84 patients (31%) and AIS E in 51 patients (19%). These data showed that improvement varied in patients with CSCIs. There were 72 patients (26%) with an NLI above C4 and of these patients 31(43%) patients developed hyponatraemia. NLI was assessed as below C4 in 198 patients, (73%) and of these patients 51 patients (26%) developed hyponatremia.
The four signal patterns found on MRI scans were normal cord in 49 patients (18%), single-level oedema in 80 patients (30%), multi-level oedema in 110 patients (41%) and haemorrhage in 31 patients (12%). The hyponatraemia rate was 4% in normal cord, 33% in single-level oedema, 28% in multi-level oedema and 80% in haemorrhage patients, respectively. In addition, the observation of neurological changes in haemorrhage patients showed that of a total of 31 patients 25 (81%) were graded as AIS A upon admission; among these, 24 (96%) remained AIS A at follow-up. One patient improved to AIS B. Of the 53 patients who had an SCI level above C3/4 26% developed hyponatraemia. Of the 83 patients who had an HL on their MRI was above C3/4 30% developed hyponatraemia.
A correlation between haemorrhage changes on the MRI and the initial AIS A was observed (coefficient value=0.293; P-value<0.001). This indicated that the initial AIS A and haemorrhage change might carry either the same or similar information (severe damage to the spinal cord).
Univariate analyses of the risk factors for hyponatraemia showed significant differences in four variables: low BP, tracheostomy, haemorrhage on the MRI and initial AIS A (Table 2). Multivariate logistic regression showed significant differences in low blood pressure and haemorrhage changes on the MRI (Table 2). Therefore we considered these variables to be risk factors for forecasting hyponatremia in patients with a CSCI.
The number of false positives and negatives, sensitivity, specificity and accuracy rate are presented in Table 3. The results showed that haemorrhage changes on the MRI had a high specificity but a rather low sensitivity, which indicated that these changes on MRI might not occur frequently in patients with a CSCI. However, once these signal changes are found, special attention should be paid to the occurrence of hyponatremia. The result also showed that haemorrhage changes on MRI scans had both higher specificity and sensitivity levels than those of low BP, which indicated that haemorrhage changes on MRI scans are more reliable than low BP in forecasting the onset of hyponatremia in patients with CSCI.
Discussion
This study found a correlation between MRI images and hyponatraemia in patients with a CSCI. These results demonstrated that haemorrhagic changes on MRI images are closely associated with hyponatraemia. In addition, low BP also appears to be associated with hyponatraemia.
Neurological assessment
Various studies have reported that the severity of paralysis is closely associated with hyponatraemia.3, 4, 8 This may be because a complete injury results in severe dysfunction of the ANS. The AIS is a system used to evaluate the neurological impairment of patients with an SCI. An assessment of AIS A indicates a complete injury. However, in the current study, univariate analyses indicated that the initial AIS A was a risk factor for hyponatremia, whereas multivariate analyses found no significant differences in the initial AIS A.
Several studies have reported that the AIS grade may change over time because of the spinal shock post CSCI. Yugue et al.20 reported that 19% of patients graded AIS A upon admission had improved neurological function at a final follow-up. In the current study, 58 patients were graded as AIS A upon admission and 12 of them had improved by their final follow-up visit. Moreover, improvement was found not only in patients with AIS A, but also in those with other AIS grades. These results confirm why only univariate analyses noted significant differences, whereas no differences were noted in the multivariate analyses.
Therefore, the potential variability of AIS grades due to spinal shock should be noted because 20% of the patients with AIS A who were assessed soon after an initial CSCI showed significant improvement post-spinal shock. In addition, predicting hyponatraemia should not be merely based on the AIS A grade in the early stages of a CSCI.
Radiological data
In the acute phase of a SCI, the presence of hyperintensity on T2-weighted MRI indicated spinal cord oedema, which suggested either a contusion or injury to the spinal cord. Haemorrhage changes on an MRI were described as a hypointensity that was surrounded by a hyperintensity on a T2-weighted MRI.21 In the current study, only haemorrhage changes on the MRI were associated with the onset of hyponatraemia in patients with a CSCI.
This outcome might be due to haemorrhage changes on MRI scans that indicate a severe SCI, which would also suggest a poor neurological outcome for patients with a CSCI. Bozzo et al.12 found that 93% of patients with haemorrhage changes on sagittal T2 images were graded as AIS A upon admission. Of these, 95% remained graded AIS A at their final follow-up visit. Similarly, in the current study, 80% of patients who exhibited haemorrhage changes on MRI scans were initially graded AIS A and only one patient showed an AIS grade improvement at his final follow-up visit.
The AIS grade, which is assessed in the early phases of an injury, may change over time because of its relationship to spinal shock. By contrast, haemorrhage changes on MRI will not change as spinal shock abates and they can be observed in the acute phase of CSCI. Hence, these image changes have a greater importance factor when compared with the initial AIS A. In addition, it also explains why only univariate analyses indicated that the initial AIS A was a risk factor for the onset of hyponatremia in patients with a CSCI. Therefore, haemorrhage changes on an MRI are a more robust predictor of hyponatraemia.
Blood pressure
Like hyponatraemia, low BP frequently appeared in patients with a CSCI. Nakao et al.8 found that 45% of CSCI patients developed low BP. Popa et al.20 reported that 68% of patients with motor-complete-CSCI had low BP. This study had a 10% occurrence of low BP, which was lower in previous studies. This outcome is likely attributable to the higher proportion of patients with incomplete CSCIs in this study than in previous studies.
In the present study, univariate and multivariate analyses indicated that low BP was a risk factor for hyponatraemia; thus low BP is an appropriate predictor of hyponatraemia in patients with a CSCI. Our two hypotheses for the close association between hyponatraemia and hypotension are as follows: (1) the pathways, which correlate to mediate BP and serum sodium, are close together at the dorsal area of the lateral funiculi and (2) the occurrence of hypotension could stimulate the secretion of ADH, which would induce water retention.3, 22
Electrolyte
In addition to hypotension, other electrolyte disturbances are also frequently present in CSCI patients. Of these disturbances, previous studies have noted that serum chloride was closely associated with hyponatremia, which may be explained by two reasons: (1) most of the total body sodium (about 65%) and chloride (about 85%) are located in the extracellular fluid rather than potassium and bicarbonate. Therefore, the water retention, which is caused by inappropriate ADH secretion, might influence sodium and chloride simultaneously. (2) the accompanying anions of sodium are mainly chloride, so the changes in serum sodium concentration are typically paralleled by similar changes in chloride.23 However, this relationship between hypochloraemia and hyponatremia was not achieved in the current study. This could have been because the changes in serum chloride and sodium have previously always occurred at the same time, whereas our study only collected electrolytes before the onset of hyponatremia.
Intravenous fluid intake and urine volume for 24 h
Water retention was caused by inappropriate secretion of ADH after a CSCI. It has been proven that excessive fluid intake might contribute to hyponatraemia. Therefore, some studies support the opinion that fluid restriction is necessary in the acute of CSCI.24, 25, 26 However, in the current study, univariate analyses did not find significant differences in IV fluid intake. This might be because, in this study, we did not include the oral water intake due to difficulties in gathering precise collection numbers from patients.
The impairment of the ANS and inappropriate secretion of ADH after a CSCI might lead to an increased loss of serum sodium. Nakao et al.8 found that patients’ daily urine volume was associated with serum sodium, and as their urine volume increased serum the sodium levels decreased. This could have resulted from the function of sodium reabsorption being damaged after the CSCI and this damage might have led to increased wasting of sodium and water. However, for some patients, whose hyponatraemia was caused by the syndrome of inappropriate antidiuretic hormone secretion (SIADH), the urine volume might not increase after a CSCI.4, 5, 27 This may explain why no significant differences in daily urine volume were noted in this study.
Limitations
The first limitation is that this study is retrospective in nature. Second, the fluid intake estimation did not include oral fluid intake. This information may not have been precisely noted in patients’ charts and thus might impact water balance. Third, the signal changes of haemorrhages might not be revealed on MRI if it was performed within a few hours of the CSCI.28 Further, research has shown that the initial hypointensity of the haemorrhage can change into a hyperintensity after 2 weeks.29, 30 Thus, the appropriate time to perform the first MRI post-trauma requires further investigation.
This study only examined associations. We did not formally validate our model for predicting hyponatraemia. This needs to be done in a separate sample or population to verify the predictive value of our model.
Conclusion
Haemorrhage changes on T2-weighted MRI scans were closely associated with hyponatremia in patients with a CSCI. It had a high specificity (97%) for forecasting hyponatremia. In addition to haemorrhage changes, low BP was also considered a reasonable predictor of hyponatraemia.
Data archiving
There were no data to deposit.
References
Hagen EM, Lie SA, Rekand T, Gilhus NE, Gronning M . Mortality after traumatic spinal cord injury: 50 years of follow-up. J Neurol Neurosurg Psychiatry 2010; 81: 368–373.
Reines HD, Harris RC . Pulmonary complications of acute spinal cord injuries. Neurosurgery 1987; 21: 193–196.
Furlan JC, Fehlings MG . Hyponatremia in the acute stage after traumatic cervical spinal cord injury. Spine 2009; 34: 501–511.
Frisbie JH . Salt wasting, hypotension, polydipsia, and hyponatremia and the level of spinal cord injury. Spinal Cord 2007; 45: 563–568.
Palmer BF . Hyponatremia in patients with central nervous system disease: SIADH versus CSW. Trends Endocrinol Metab 2003; 14: 182–187.
Rodgers RB, Horn EM, Sonntag VKH. Acute Treatment of Patients with Spinal Cord Injury. In: Herkowitz HN (ed). The spine, 6th edn. Elsevier: Philadelphia, PA, USA. 2011, pp 1422–1435..
Ball SG . Diagnosis and treatment of hyponatraemia. Best Pract Res Clin Endocrinol Metab 2016; 30: 161–173.
Nakao Y, Suda K, Shimokawa N . Risk factor analysis for low blood pressure and hyponatremia in acutely and subacutely spinal cord injured patients. Spinal Cord 2012; 50: 285–288.
Amini A, Schmidt MH . Syndrome of inappropriate secretion of antidiuretic hormone and hyponatremia after spinal surgery. Neurosurg Focus 2004; 16: E10.
Barros AP, González QA, Pena SM, Pose RA . Syringomyelia associated with inappropriate antidiuretic hormone secretion. BMJ Case Rep 2014 doi: 10.1136/bcr-2013-202575.
Kriz J, Schuck O, Horackova M . Hyponatremia in spinal cord injury patients: new insight into differentiating between the dilution and depletion forms. Spinal Cord 2015; 53: 291–296.
Bozzo A, Marcoux J, Radhakrishna M, Pelletier J, Goulet B . The role of magnetic resonance imaging in the management of acute spinal cord injury. J Neurotrauma 2011; 28: 1401–1411.
Martirosyan NL, Bennett KM, Theodore N, Preul MC . Manganese-enhanced magnetic resonance imaging in experimental spinal cord injury: correlation between T1-weighted changes and Mn (2+) concentrations. Neurosurgery 2010; 66: 131–136.
Looby S, Flanders A . Spine trauma. Radiol Clin North Am 2011; 49: 129–163.
Goldberg AL, Kershah SM . Advances in imaging of vertebral and spinal cord injury. J Spinal Cord Med 2010; 33: 105–116.
Zohrabian VM, Flanders AE . Imaging of trauma of the spine. Handb Clin Neurol 2016; 136: 747–767.
Wolf M, Weber MA . Neuroimaging of the traumatic spine. Magn Reson Imaging Clin N Am 2016; 24: 541–561.
Jun T, Itaru Y, Keiichiro S, Maeyama A, Masatoshi N . A study of risk factors for tracheostomy in patients with a cervical spinal cord injury. Spine 2016; 41: 764–771.
Ditunno JF, Little JW, Tessler AS, Burns AS . Spinal shock revisited: a four-phase model. Spinal Cord 2004; 42: 383–395.
Yugué I, Okada S, Ueta T, Maeda T, Mori E, Kawano O et al. Analysis of the risk factors for tracheostomy in traumatic cervical spinal cord injury. Spine 2012; 37: E1633–E1638.
Pan G, Kulkarni M, Macdougall DJ, Miner ME . Traumatic epidural hematoma of the cervical spine: diagnosis with magnetic resonance imaging. Case report. J Neurosurg 1988; 68: 798–801.
Karlsson AK . Autonomic dysfunction in spinal cord injury: clinical presentation of symptoms and signs. Prog Brain Res 2006; 152: 1–8.
Giebisch G, Windhager E. Integration of Salt and Water Balance. In: Boron E, Boulpaep E (eds). Medical physiology. Elsevier Saunders: Philadelphia, PA, USA. 2005, pp 861–876..
Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med 2013; 126 (10 Suppl 1): S1–S42.
Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH . Hyponatremia treatment guidelines 2007: expert panel recommendations. Am J Med 2007; 120 (11 Suppl 1): S1–21.
Spasovski G, Vanholder R, Allolio B, Annane D, Ball S, Bichet D et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant 2014; 29 (Suppl 2): i1–i39.
Cuesta M, Garrahy A, Thompson CJ . SIAD: practical recommendations for diagnosis and management. J Endocrinol Invest 2016; 39: 991–1001.
Bradley WJ . MR appearance of hemorrhage in the brain. Radiology 1993; 189: 15–26.
Shanmuganathan K, Gullapalli RP, Zhuo J, Mirvis SE . Diffusion tensor MR imaging in cervical spine trauma. AJNR Am J Neuroradiol 2008; 29: 655–659.
Himada K, Tokioka T . Sequential MR studies of cervical cord injury: correlation with neurological damage and clinical outcome. Spinal Cord 1999; 37: 410–415.
Acknowledgements
Dr CS work has been funded by the National Natural Science Foundation of China. This study was supported by the National Natural Science Foundation of China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Song, P., Dong, F., Feng, C. et al. A study of predictors for hyponatraemia in patients with cervical spinal cord injury. Spinal Cord 56, 84–89 (2018). https://doi.org/10.1038/sc.2017.103
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2017.103
This article is cited by
-
Mechanisms of hyponatremia and diabetes insipidus after acute spinal cord injury: a critical review
Chinese Neurosurgical Journal (2023)
-
Predictive factors for irreversible motor paralysis following cervical spinal cord injury
Spinal Cord (2021)
-
Comment on ‘Correspondence to: A study of predictors for hyponatraemia in patients with cervical spinal cord injury’
Spinal Cord (2018)
-
Re: A study of predictors for hyponatraemia in patients with cervical spinal cord injury
Spinal Cord (2018)