Abstract
Study design:
A cross-sectional study.
Objectives:
To study prevalence of pressure ulcers (PrUs), quality of life (QoL) and effect of wheelchair cushions used by Thai wheelchair users with chronic spinal cord injury (SCI).
Setting:
Maharaj Hospital, Chiang Mai, Thailand.
Methods:
Thai chronic SCI wheelchair users, aged over 18 years and non-ambulatory with ASIA impairment scale A, B or C were recruited. They completed the PrUs questionnaire and rated the EuroQoL-5D and their health status with a visual analog scale (VAS). Demographic data of each participant were extracted from medical records. The EQ-5D health states were transformed to utility scores by using the Thai algorithm and the prevalence of PrUs was reported. The EQ-5D, the utility scores and the health status VAS were compared between those with and without current PrUs and between those participants using foam and air-filled cushions.
Results:
Of 129 participants, 26.4% had current PrUs at the time of the study, 27.9% had healed PrUs and 45.7% never had PrUs. The median VAS score for health status was 70 (Q1=50, Q3=80). Based on the EQ-5D, only one dimension (anxiety/depression) was significantly different between those with and those without current PrUs (P=0.015). Those using an air-filled cushions had a mean utility score four times higher than of those using a foam cushion (0.131 vs 0.032, P=0.089) but not statistically significant.
Conclusions:
PrUs are still prevalent among Thai wheelchair users with chronic SCI. Anxiety/depression is associated with current ulcers.
Similar content being viewed by others
Introduction
Pressure ulcer (PrU) is one of the main secondary health outcomes of spinal cord injury (SCI) that has a significant impact on health, functions and quality of life (QoL), especially in the case of non-ambulatory individuals, either bed-bound patients or wheelchair users,1 and may occur at any phase after injury.2 According to a recent review on PrUs in people with SCI in developing countries (2014), PrUs are especially prevalent. During acute hospitalization, PrU prevalence ranged from 2.7% in China to 42.5% in Brazil; during rehabilitation, the prevalence ranged from 5.9% in Sri Lanka to 29.9% in South India; and in the chronic phase, it ranged from 26.7% in Brazil to 46.2% in China.3
According to our cross-sectional survey conducted in Chiang Mai in 2003,4 80% of 142 individuals with chronic SCI living in communities reported having an occurrence of PrU at least once in their lives, but during the survey, 28% had current PrUs, similar to the prevalence reported in developing and developed countries.3 In addition, it was observed that the severity of SCI, and the duration after injury were significantly associated with PrUs among Thais with chronic SCI.4
To have better PrU prevention outcomes, we began implementation of the Consortium for Spinal Cord Medicine clinical practice guidelines PrU prevention and treatment following SCI (2000). For example, we began applying pillows and cushions to bridge contacting tissues and unloading bony prominences, conducting daily visual and tactile skin inspections, providing a wheelchair pressure-reducing cushion and so on.2 Before the implementation of the universal health coverage scheme in 2002, only government employees, retirees and dependants under the civil servant medical benefit scheme and private sector employees under the social security scheme received free health services. At present, about 75% of the Thai population as well as people with disabilities receive coverage under this universal health scheme, which provides them free basic health services.5 Although the budget for medical rehabilitation including services and necessary equipment has increased, it is still limited.5 We therefore, provided every SCI wheelchair user a foam cushion (made of medium-soft foam of 5.0–7.5 cm thickness on top and hard foam of 2.5 cm thickness below, at a cost of about US $10). These were either flat or contoured based on pressure mapping, and with the old cushions being replaced yearly with new ones.
From our observation, the foam cushions seemed to be a cost-effective means for maintaining skin integrity. However, some clients at risk of PrU might have been better off with air-filled cushions, which cost approximately 500 US dollars, or 50 times more expensive than the cost of the foam cushion. Preliminary data regarding cost-effectiveness were needed to discern how to make an air-filled cushion available for those at risk so that the National Health Service Office could make a decision. Therefore, the purpose of this study was to report the prevalence of PrUs and their impact on the QoL in Thais with chronic SCI. In addition, a comparison was made between the outcomes for those with PrUs and those without PrUs and between those using foam cushions and those using air-filled cushions.
Materials and methods
This study is part of a cross-sectional study on ‘cost-effectiveness evaluation of an air-alternating overlay on preventing of PrUs in persons with chronic traumatic SCI,’ approved by the Research Ethics Committee of the Faculty of Medicine, Chiang Mai University (Research ID: 1440/Study code: REH-13-1440-Ex). It was conducted from 1 January 2013 to 31 December 2013, at the Maharaj Hospital, Chiang Mai, Thailand.
Data on wheelchair users with chronic traumatic SCI were obtained from the above-mentioned study. Inclusion criteria were as follows: age >18 years, 1+ years post-SCI, ability to communicate and provide information, and use a wheelchair. Respondents with ASIA impairment scale D were excluded. The demographic data were collected based on the international SCI core data set.6 The participants were asked to complete a questionnaire regarding PrUs and related factors, and to rate the EuroQoL-5 dimensions (EQ-5D) and the visual analog scale (VAS) to assess their health status, with ‘0’ representing ‘worst health’ and ‘100’ representing ‘best health’.7, 8
The EQ-5D is a generic health-related QoL measure that has been widely used as a means for valuing different health states and assessing the cost-effectiveness of alternative health technologies.7, 8, 9 According to a review on preference-based health-related QoL questionnaires in SCI research,8 the EQ-5D was used in 10 studies. It consisted of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each of these dimensions has three levels of response (1: no problem; 2: some problems and 3: confined to bed for mobility, unable to wash or dress oneself for self-care, unable to perform one’s day-to-day usual activities, extreme pain and discomfort, and extreme anxiety and depression).7, 8, 9 When combined levels were rated from the five domains, there were 243 health states, that is, ‘11111’ stands for ‘best imaginable health,’…, ‘33333’ stands for ‘worst imaginable health.’7, 8, 9 Then, the EQ-5D health states were transformed to utility scores by using the Thai algorithm.10 For example, a paraplegic wheelchair user (2) had no problem with self-care (1), some problems with doing usual activities (2), no pain (1) and no anxiety/depression (1), his EQ-5D health state was 21211; when using the Thai algorithm, its utility score was 0.618.10
Owing to marked socioeconomic and cultural differences between countries, a study of EQ-5D was done to derive the EQ-5D health state values or the utility scores from the Thai general population that could be used in evaluating health intervention in Thailand.10 The Thai algorithm is as follows: the Thai utility score=1-0.202-(0.121*mo)-(0.121*sc)-(0.059*ua)-(0.072*pd)-(0.032*ad)-(0.190*m2)-(0.065*p2)-(0.046*a2)-(0.139*N3); mo: mobility; sc: self-care; us: usual activities; pd: pain/discomfort and ad: anxiety/depression. The variable ‘mo’ is 1 if mobility is level 2, 2 if mobility is level 3 and 0 otherwise; the variable ‘sc’ is 1 if self-care is level 2, 2 if self-care is level 3 and 0 otherwise; the variable ‘us’ is 1 if usual activity is level 2, 2 if usual activity is level 3 and 0 otherwise; the variable ‘pd’ is 1 if pain/discomfort is 2, 2 if pain and discomfort is 3, and 0 otherwise; the variable ‘ad’ is 1 if anxiety/depression is 2, 2 if anxiety/depression is 3 and 0 otherwise; the variable ‘m2’ is 1 if mobility is level 3 and 0 otherwise; the variable ‘p2’ is 1 if pain/discomfort is level 3 and 0 otherwise; the variable ‘a2’ is 1 if anxiety/depression is level 3 and 0 otherwise; and the variable ‘N3’ is 1 if any dimension is level 3 and 0 otherwise.10
Statistical analysis
Descriptive analyses were conducted. Prevalence of PrUs was reported as percentage of Thai wheelchair users. The demographic data, disability based on the EQ-5D dimensions and the health state VAS scores were compared between those with current PrUs and those without current PrUs. Sites and reported causes were compared between those with current PrUs and those with healed PrUs. The utility scores were compared between those using the foam cushions and those using the air-filled cushions. χ2 test or Fisher’s exact test was used for categorical data and Student's t-test or Mann–Whitney U-test was used for continuous data.
Results
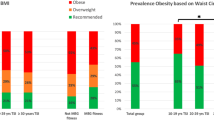
Of the 129 participants, 34 (26.4%) had current PrUs, 36 (27.9%) had healed PrUs and 59 (45.7%) never had PrUs. Table 1 shows the demographic data: 62% had a complete SCI and 72.9% were paraplegic. Demographic data, such as gender, age group, duration after injury, impairment level, completeness of SCI, educational level and having employment, were not related to the presence of current PrUs.
Table 2 shows sites and causes of PrUs reported by those with current PrUs and those with healed PrUs. The most common site of current PrUs was ischium/ischial tuberosity, whereas that of healed PrUs was the sacrococcygeal area. Very few reported having PrUs in more than one site in both groups. Both current and healed PrUs were reported to be caused by prolonged sitting and lying in bed. In addition, out of 34 medical records of those with current PrUs, 22 (64.8%) reported severity of the ulcers based on the National Pressure Ulcer Advisory Panal Scale: stage I in 1 participant, II in 11, III in 7 and IV in 3. Among them, two participants with stage II and one with stage III used air-filled cushions, the rest used foam cushions.
Table 3 shows comparisons of disability based on the EQ-5D between those with current PrUs and those without current PrUs. Limitations in mobility (walking), self-care and usual activities as well as experiencing of pain/discomfort were not associated with current PrUs; however, anxiety/depression had significant association with current PrUs, that is, the proportion of anxiety/depression was higher in those with current PrUs than those without current PrUs (79.4% vs 53.7%, P=.015). In addition, the median health status VAS score of all the participants was 70 (Q1=50, Q3=80) and that there was no difference between those having current PrUs and those not having current PrUs.
Most of the participants used foam cushions (78.3%), followed by air-filled cushions (15.5%), gel cushions (1.5%) and others (3.1%); one (0.8%) did not use a cushion. When comparing between those using foam cushions and those using air-filled cushions, the percentages of those having current PrUs were not different. However, although the utility score of those using air-filled cushions was four times higher than that of those using foam cushions, this difference was not statistically significant (0.131 vs 0.032, P=0.089; see Table 4).
Discussion
The prevalence of current PrUs in Thai wheelchair users with chronic SCI was 26.4% and the percentage of those having no PrUs was 45.7%, whereas in 2003, as we found, 28% of the chronic SCI living in communities had PrUs at the time of the survey and only 20% reported having never had PrUs.4 It needs to be noted that these two studies were a cross-sectional survey, not a cohort study; the participants recruited were chronic SCI living in the community, not the newly injured cases; but that the duration after injury was similar, about 9 years.4 The increase in percentage of those not having had PrUs since injury might be due to our effort over the past 10 years by following the clinical practice guideline–PrU prevention following SCI,2 and from our observation, a PrU occurred only in 0–1 of 70 new SCI cases during acute and post-acute rehabilitation phases each year. This decreases the risk of PrU in an early long-term phase.
Based on the health status VAS, Thai wheelchair users with chronic SCI seem to be moderately satisfied with their health. The only QoL dimension that was associated with having current PrUs was anxiety/depression. As this was a cross-sectional study, we could not conclude whether PrU caused anxiety/depression or not. Nevertheless, rehabilitation professionals should keep in mind the relationship between having PrUs and emotional states. According to an earlier study,11 it is recommended that apart from skin check and pressure relief techniques, we should help individuals with SCI realize how PrUs develop in daily living, manage stress and identify an optimal balance between living a full life and avoiding activity associated with PrUs.
As expected, the most common site of PrUs among wheelchair users was the ischial tuberosity. It is our practice to use a 7.5- to 10-cm thickness of medium-soft on top of hard foam cushion and cut or contour its top surface to lower the pressure at the ischial tuberosity12 down to 60–90 mm Hg if an interface pressure at this bony prominence is over 120 mm Hg. This cut-out/contoured foam cushion is quite similar to what has been previously reported from Japan.13 However, the prevalence of current PrUs was lower in the Japanese study than in ours (17.9% vs 26.4%).14 The higher rate in our study might be due to prolonged use, as a new cushion was replaced yearly. To have better prevention outcomes, we should remind them that the foam cushions are not durable,13 deteriorate over time even without use,15 and should be changed more frequently, for example, every 6 months instead of yearly.12 In addition, compared with a flat foam cushion, a custom-contoured foam cushion provides lower interface pressure at the bony prominences and good envelopment of the buttocks as long as there is no bottoming-out.16
In developed countries, air-filled cushions have been widely used by wheelchair users. They cost over 500 US dollars, 50 times more expensive than the foam cushions, which we have provided free of charge to our wheelchair users. Other cushions that cost more than 10 US dollars are purchased by the users or free from charitable organizations. Economic evidence is necessary to help policy makers to accept reimbursement of an air-filled cushion for those who are really in need. According to this preliminary economic evaluation carried out by transforming the ED-5Q health states to utility scores, those using air-filled cushions had four times higher utility score than those using foam cushions (0.131 vs 0.032, P=0.089). However, we still could not conclude that prescribing the air-filled cushion will be cost-effective with regard to prevention of PrUs in Thai SCI wheelchair users. A psychometric evaluation of the use of EQ-5D as a generic preference-based health-related QoL measure in individuals with SCI is still lacking,8 and a larger randomized control trial study is necessary.
It should be noted that the prevalence of current PrUs in those using the foam cushions in this study was still high (over 24%). Recently, Taule et al. retrospectively reviewed 80 SCI wheelchair users visiting the seating clinic at a University Hospital in Norway, and found that 26.7% had current PrUs and 62.7% used air-filled cushions.17 The results from these two studies reveal that wheelchair cushions are not the only means of preventing PrUs. Both rehabilitation professionals and SCI wheelchair users should be aware that causes of PrUs are multi-factorial.11, 18, 19, 20 Besides risk factors (duration after injury, completeness of SCI, spasticity, being underweight and history of PrUs), personal and behavioral risks (being unmarried, unemployed and less educated, daily-lifestyle and activities;11 use of tobacco, alcohol or drugs;20, 21 loss of independency and suicidal ideation)20 and equipment such as type of wheelchair and cushion used17 should be identified, explored, linked to cause, and balanced between living a full life and avoiding activities related PrUs in adults with SCI.11, 17, 18, 19, 20 In addition, to make prevention of recurrent PrUs more effective, an intensive structured patient education on healthy lifestyle, exercise and diet, and monthly follow-up contact should be provided to those having previously undergone PrU surgery by a health professional with expertise in both PrUs and SCI.17, 20, 22, 23
Limitations of this study include the use of a cross-sectional study design and a sample of chronic SCI wheelchair users who visited an out-patient rehabilitation clinic in a hospital. There might be a selection bias. According to our previous study done in 2007, 52.5% were tetraplegic and 50.8% had a complete SCI,24 whereas in this study, 75% were paraplegic wheelchair users and some ambulatory tetraplegic clients were excluded. In addition, PrUs were self-reported. Some participants might not recall the occurrence of a small, grade 1 PrU or ulcers that had already healed, and so the prevalence of PrUs reported might be lower than what it should have been. Unfortunately, only two-thirds of those having current PrUs in this survey had data on the severity of the PrUs in their medical records. Further prospective study with a larger cohort is mandatory.
In conclusion, PrUs are still prevalent among wheelchair users with chronic SCI in Thailand. Anxiety/depression is associated with having current ulcers. To achieve better prevention outcomes, rehabilitation professionals and SCI-affected wheelchair users should be aware of an appropriate wheelchair cushion that should be used, its life expectancy and multi-factorial causes of PrUs.
Data archiving
There were no data to deposit.
References
Krause JS, Reed KS, McArdle JJ . A structural analysis of health outcomes after spinal cord injury. J Spinal Cord Med 2010; 33: 22–32.
Consortium of Spinal Cord Medicine Pressure Ulcer Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health Care Professionals. Paralyzed Veterans of America: Washington DC. 2000.
Zakrasek EC, Creasey G, Crew JD . Pressure ulcers in people with spinal cord injury in developing countries. Spinal Cord 2014; 53: 7–13.
Wilekha N, Kovindha A . A study of protective behaviors and risk factors of pressure ulcers in spinal cord injured patient. J Thai Rehabil 2005; 15: 101–112.
Treerutkuarkul A (ed). Unversal Health Coverage: Case Studies from Thailand. Health System Research Institute (HSRI), Ministry of Publish Health: Nonthaburi. 2012.
DeVivo M, Biering-Sørensen F, Charlifue S, Noonan V, Post M, Stripling T et al. International Spinal Cord Injury Core Data Set. Spinal Cord 2006; 44: 535–540.
Brazier J, Roberts J, Tsuchiya A, Busschbach J . A comparison of the EQ-5D and SF-6D across seven patient groups. Health Econ 2004; 13: 873–884.
Whitehurst DGT, Noonan VK, Dvorak MFS, Bryan S . A review of preference-based health-related quality of life questionnaires in spinal cord injury research. Spinal Cord 2012; 50: 646–654.
Brooks R . EuroQoL: the current state of play. Health Policy 1996; 37: 53–72.
Tongsiri S, Cairns J . Estimating population-based values for EQ-5D health states in Thailand. Value Health 2011; 14: 1142–1145.
Clark FA, Jackson JM, Scott MD, Carlson ME, Atkin MS, Uhles-Tanaka D et al. Data-based models of how pressure ulcers develop in daily-living contexts of adults with spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1516–1525.
Ferguson-Pell MW . Seat Cushion Selection: Choosing a Wheelchair System. J Rehabil Res Dev Clin Suppl 1990, 49–73.
Sumiya T, Kawamura K, Tokuhiro A, Takechi H, Ogata H . A survey of wheelchair use by paraplegic individuals in Japan. Part 1: characteristics of wheelchair cushions. Spinal Cord 1997; 35: 590–594.
Sumiya T, Kawamura K, Tokuhiro A, Takechi H, Ogata H . A survey of wheelchair use by paraplegic individuals in Japan. Part 2: prevalence of pressure sore. Spinal Cord 1997; 35: 595–598.
Ferguson-Pell MW, Wilkie IC, Reswick JB, Barbenel JC . Pressure sore prevention for the wheelchairbound spinal injury patient. Paraplegia 1980; 18: 42–51.
Gefen A . Tissue changes in patients following spinal cord injury and implications for wheelchair cushions and tissue loading: a literature review. Ostomy Wound Manage 2014; 60: 34–45.
Taule T, Bergfjord K, Holsvik EE, Lunde T, Stokke BH, Storlid H et al. Factors influencing optimal seating pressure after spinal cord injury. Spinal Cord 2013; 51: 273–277.
Garber SL, Rintala DH, Hart KA, Fuhrer MJ . Pressure ulcer risk in spinal cord injury: predictors of ulcer status over 3 years. Arch Phys Med Rehabil 2000; 81: 465–471.
Chen Y, DeVivo MJ, Jackson AB . Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil 2005; 86: 1208–1213.
Krause JS, Vines CL, Farley TL, Sniezek J, Coker J . An exploratory study of pressure ulcers after spinal cord injury: relationship to protective behaviors and risk factors. Arch Phys Med Rehabil 2001; 82: 107–113.
Tate DG, Forchheimer MB, Krause JS, Meade MA, Bombardier CH . Patterns of alcohol use and abuse in persons with spinal cord injury: risk factors and correlates. Arch Phys Med Rehabil 2004; 85: 1837–1847.
Rintala DH, Garber SL, Friedman JD, Holmes SA . Preventing recurrent pressure ulcers in veterans with spinal cord injury: impact of a structured education and follow-up intervention. Arch Phys Med Rehabil 2008; 89: 1429–1441.
Krause JS, Broderick L . Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset. Arch Phys Med Rehabil 2004; 85: 1257–1264.
Wongtra-Ngan N, Kovindha A, Tongprasert S, Premkomol P Measuring qualitiy of life with WHOQOL-BREF in Thai individuals with spinal cord injury. ASCON meeting 31 October 2010; Le Meridian, New Delhi.
Acknowledgements
We thank the International Health Policy Program (IHPP), Thailand, for funding this research and Chiang Mai University for funding presentation of this paper at the ISCOS meeting in Maastricht, September 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Kovindha, A., Kammuang-lue, P., Prakongsai, P. et al. Prevalence of pressure ulcers in Thai wheelchair users with chronic spinal cord injuries. Spinal Cord 53, 767–771 (2015). https://doi.org/10.1038/sc.2015.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.77
This article is cited by
-
Comparison of aloe vera gel dressing with conventional dressing on pressure ulcer pain reduction: a clinical trial
BMC Research Notes (2024)
-
Increasing employment opportunity for persons with spinal cord injury by digital working: an exampling case series from Thailand
Spinal Cord Series and Cases (2024)
-
Low-intensity pulsed ultrasound partially reversed the deleterious effects of a severe spinal cord injury-induced bone loss and osteoporotic fracture healing in paraplegic rats
Spinal Cord (2023)
-
Wireless, multimodal sensors for continuous measurement of pressure, temperature, and hydration of patients in wheelchair
npj Flexible Electronics (2023)
-
Incidence, severity and time course of pressure injuries over the first two years following discharge from hospital in people with spinal cord injuries in Bangladesh
Spinal Cord (2022)