Abstract
Study design:
Serum levels of interleukin-1β (IL-1β) and tumour necrosis factor-α (TNF-α) were measured over a 12-week period in 23 patients with spinal cord injury (SCI) with and without neurological improvement.
Objectives:
To determine the course of IL-1β and TNF-α in patients with SCI and observe a possible relationship between improvements in neurological functioning and cytokine levels.
Setting:
All patients were treated at the BG Trauma Centre, Ludwigshafen, Germany. All lab work was done at the University Hospital, Heidelberg.
Methods:
Spinal cord injury was classified according to the American Spinal Injury Association (ASIA) impairment scale (AIS) in 23 patients. TNF-α and IL-1β levels were measured upon arrival at the hospital, after 4 h, 9 h and 12 h, on days 1 and 3 and at the end of weeks 1, 2, 4, 8 and 12.
Results:
Temporal changes in TNF-α and IL-1β in SCI patients were seen. Patients with AIS improvement (Group 1) had significantly lower TNF-α levels at 9 h compared with patients without AIS improvement (Group 2; P<0.01). The course of IL-1β fluctuated greatly between 4 h and week 1 in the groups; however, between 2 and 12 weeks post trauma, there was an overall decline in both groups.
Conclusion:
Measuring serum levels of TNF-α and IL-1β over time could be useful in tracking the course of SCI. Our data show differences in measured cytokines over a 12-week period for SCI patients with and without neurological improvement.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a debilitating disorder often leading to lifelong care and rehabilitation and severe social and economic consequences for patients and their families. Although rehabilitation and treatment of SCI has progressed over the years, there are still no effective, curative strategies for treating SCI.1 In recent years, researchers have also investigated limiting damage directly after injury by targeting cytokines believed to be a cause of cellular damage.2, 3 This study provides data on two potential targets for therapy, interleukin-1β (IL-1β) and tumour necrosis factor-α (TNF-α), as a first step toward improving the clinical outcome following acute and chronic SCI.
In general, SCI has a primary phase and secondary phase of injury following traumatic injury to the spinal cord. The primary phase is marked by necrosis due to mechanical trauma such as laceration, contusion, compression or concussion. The initial lesion is often small, but cell destruction mediated by calcium influx, NO and oxidative stress spreads to surrounding tissue within minutes to hours. Pro-inflammatory cytokines such as IL-1β and TNF-α may exacerbate this process and are linked to a longer process of secondary injury that continues in the weeks following injury.4 Secondary injury is believed to be the continuation of cellular destruction brought on by processes such as oedema, inflammation, excitotoxicity and apoptosis1 leading to neuronal cell death and axonal loss in regions not affected by the initial damage.5 Although primary damage cannot be effectively treated, stopping secondary damage could halt neuronal degeneration and improve the clinical outcome of SCI.
Despite treatment attempts on animals showing success in limiting SCI, further studies are needed to show the efficacy and safety of such therapy in SCI patients.6 In the literature, there have been few measurements of targeted cytokines in SCI patients. Research has shown that temporal cytokine responses can be used as objective predictors of wound healing and aid surgeons contemplating procedure selection and timing.7, 8 This raises the question of whether cytokine levels would yield similar revelations and perhaps improve the treatment of SCI. Temporal cytokine levels after SCI have not been adequately assessed; to fill this gap, we recently measured sCD95L in nine SCI patients.9 The present study is an extension of our previous study and involves a larger patient pool and two other cytokines of interest, IL-1β and TNF-α. We believe that these data will be useful to researchers investigating new procedures or improving current strategies in limiting neuronal damage post SCI.
Materials and methods
Data were obtained from 23 patients (16 males and 7 females) suffering from acute traumatic SCI who were admitted from 2009 to 2012 to the BG Trauma Centre (Berufsgenossenschaftlische Unfallklinik Ludwigshafen). Their ages ranged from 18 to 86 years. Fifteen (65.2%) patients were paraplegic, and eight (34.8%) patients were tetraplegic. American Spinal Injury Association (ASIA) impairment scale (AIS) grades (A–E) were evaluated according to the guidelines of the International Standards for Neurological Classification of Spinal Cord Injury.10 Patients were divided into two groups (group 1, improved AIS grade; and group 2, no improvement in AIS grade) in our analysis. Demographic and clinical patient profiles are shown in Table 1. Patients received neither methylprednisolone sodium succinate nor nonsteroidal antiphlogistics. Oxycodone hydrochloride (Oxygesic) was given for pain management.
All patients with TBI, severe chest injuries, traumatic amputations of the extremities and severe intra-abdominal injuries were excluded from our study.
Sample acquisition
Venous blood was collected (7.5 ml monovette, Sarstedt, Germany) following admission to the hospital at specific time points: upon arrival, at 4, 9 and 12 h, and at 1, 2, 4, 8 and 12 weeks after injury. Following 20 min of coagulation, blood was centrifuged at 3000 r.p.m. for 10 min and the serum supernatant obtained from serum samples was alliquoted and stored at −80 °C until analysis of IL-1β and TNF-α.
Measurement of IL-1β and TNF-α
The Quantikine Human Immunoassay (R&D Systems, Inc, Minneapolis, MN, USA) for IL-1β and TNF-α measurement was used. The lab technician performing the test was blinded to all patient and clinical information. Enzyme-linked immunosorbent assay analyses were performed twice for each patient at each time point. Lab work was done in the lab of the Heidelberg Trauma Research Group at the Heidelberg University Hospital.
Data analysis
Data analysis was supported by the Institute for Medical Biometrics and IT at the University of Heidelberg, Germany. Comparison of cytokine levels (IL-1β and TNF-α) between different groups was made with the Mann–Whitney U-Test. Comparison of cytokine levels within a group was made with the Wilcoxon signed-rank test. Continuous data were expressed as means and s.d., and categorical data were expressed with absolute and relative rates. Figures were illustrated in terms of means and s.e.m.
Results were deemed statistically significant if P<0.05. Statistical analyses were conducted with SPSS Software (Deutschland GmbH, Ehningen, Germany). Graphs were created with Sigmaplot Software (Systat Software Inc., San Jose, CA, USA).
Statement of ethics
The study was approved by the Ethics Commission of the Landesärztekammer Rheinland-Pfalz (No. 837.266.09) and Ethics Commission of the University of Heidelberg (No S- 514.2011). All participants provided written informed consent prior to enrolment.
Results
Age, gender, level of lesion and initial and final ASIA impairment scale (AIS) grades for patients with and without AIS improvement are shown in Table 1.
In the entire collective, there were 23 patients: 16 male and 7 female. The average age was 42.9±21.8 years. Thirteen injuries (56.5%) were due to falls, 9 (39.1%) due to traffic accidents and 1 (4.4%) due to another cause. There were eight cervical lesions (34.8%), nine thoracic lesions (39.1%) and six lumbar lesions (26.1%). The initial AIS scores were as follows: 13 A injuries (56.5%), 1 B injury (4.3%), 4 C injuries (17.4%) and 5 D injuries (21.8%). The final AIS scores were as follows: 11 A injuries (47.9%), 1 B injury (4.3%), 2 C injuries (8.7%), 8 D injuries (34.8%) and 1 E injury (4.3%).
There were 7 patients with AIS improvement and 16 with no improvement. Among the patients with improvement, the average age was 50.14±24.78 years. There were six females (85.7%) and one male (14.3%). Injuries included five falls (71.4%) and two traffic accidents (28.6%). There were three cervical lesions (42.9%), one thoracic lesion (14.2%) and three lumbar lesions (42.9%). Initial AIS injuries included two A injuries (28.5%), one B injury (14.3%), three C injuries (42.9%) and one D injury (14.3%). Final AIS scores were as follows: one B (14.3%), one C (14.3%), four D (57.1%) and one E (14.3%).
Among patients with no AIS improvement, the average age was 39.75±20.39 years. There were 15 males (93.8%) and 1 female (6.2%). Injuries included 8 falls (50.0%), 7 traffic accidents (43.8%) and 1 other (6.2%). There were 5 cervical lesions (31.2%), 8 thoracic lesions (50.0%) and 3 lumbar lesions (18.8%). Initial AIS injuries included 11 A injuries (68.8%), 1 C injury (6.2%) and 4 D injuries (14.3%). Final AIS scores were as follows: 11 A (68.8%), 1 C (6.2%) and 4 D (25.0%).
TNF-α
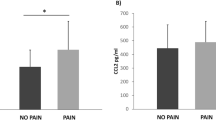
Temporal changes in TNF-α in both groups are best seen in Figures 1a and b.
(a) The course of TNF-α serum levels from week (W) 1 to W 12 in spinal cord-injured (SCI) patients with (group 1) and without (group 2) improvement in the ASIA impairment scale (AIS) is shown. The course during the first 72 h is shown in b. Significant differences in comparison with initial values are indicated by an asterisk (*) in patients with AIS improvement. (b) The course of TNF-α serum levels in both groups in the first 72 h after SCI. Significant differences in comparison with initial values are indicated by an asterisk (*) or by a cross (+) according to AIS group, respectively. Two asterisks indicate significant difference between groups.
Patients with improved AIS (group 1) showed a decrease in TNF-α concentrations after 9 h (1.62 pg ml−1), which was followed by significant increases at 72 h and week 1 in comparison with initial values (3.51 pg ml−1 and 3.93 pg ml−1, P=0.043 and 0.046, respectively). After 4 weeks and after 8 weeks there was a significant increase in levels (4.59 pg ml−1 and 5.38 pg ml−1, P=0.028 and 0.043, respectively), and a decrease thereafter up until week 12 (4.93 pg ml−1) (Figures 1a and b).
Patients without AIS improvement (group 2) showed a significant decrease in TNF-α levels at 4 h compared with the initial value (3.46 pg ml−1; P=0.026). Concentration levels fluctuated during week 1 and fell after week 2 (4.18 pg ml−1 and 3.62 pg ml−1, respectively). Levels then increased up until week 12 (5.54 pg ml−1).
There was a significantly lower concentration in group 1 than in group 2 at 9 h (P<0.01) (Figures 1a and b).
IL-1β
Temporal changes can be seen in Figures 2a and b. From 4 h to week 1, cytokine levels fluctuated greatly in the AIS groups. Levels declined after week 2 in both groups with a plateau between weeks 4 and 8. There were no significant differences over the course of the first week relative to initial values in groups 1 and 2. However, group 2 showed a significant fall in IL-1β levels between weeks 1 and 4 (P=0.017) (Figure 2a). There were no significant differences between AIS groups over the entire course of the study.
(a) The course of IL-1β serum levels from week 1 to week 12 in SCI patients with and without AIS improvement is shown. The course in the first 72 h is shown in b. A significant fall in comparison with the maximum value at week 1 is indicated by a cross (+) in patients with no AIS improvement. (b) The course of IL-1β serum levels in both groups within the first week (W) after SCI. There were no significant differences in comparison with initial values.
Discussion
In this study, we documented distinct, temporal cytokine profiles for IL-1β and TNF-α. We found that IL-1β levels were significantly elevated in SCI patients directly after accident and at all time points in the study. The TNF-α levels were significantly elevated following an initial decrease in concentration in the first 12 h after injury. Although studies have shown increased IL-1β and TNF-α after SCI,11, 12 this was the first study to have taken repeated measurements over time to generate a temporal cytokine profile for IL-1β and TNF-α in humans. Because of the not especially large patient collective (n=23), there were associated differences in absolute values with a high and variable s.d. Nevertheless, some significant absolute values for IL-1β and TNF-α were recorded.
One of the most comprehensive studies on cytokine profiles post SCI was conducted by Davies et al.12 Authors documented cytokine profiles after SCI and showed significantly higher levels of TNF-α in SCI patients, similar to our results, but showed no detectable differences in IL-1β. Unlike our study, cytokine measurements were taken only once and patients were in different stages of SCI: 23 patients were in the sub-acute phase of SCI (2–52 weeks) and the remaining 34 had chronic SCI (>52 weeks). Most measurements were probably taken at a much later time point than in our study, as Davies et al.12 reported TNF-α serum levels, almost 10 times higher than ours, and IL-1β levels were undetectable. This could be explained by the fact that TNF-α increased steadily in our patients, peaking at our last measurement at week 12. Perhaps levels would have continued to increase, reaching a maximum level weeks or months later similar to that in the study by Davies et al.12 With regard to absolute IL-1β levels, they peaked after 1 week and decreased steadily thereafter, which could explain undetectable measurements in the study by Davies et al.12 (if IL-1β measurements were taken months after injury).
The discussion of cytokine profiles is by no means limited to research on SCI. Measurement of cytokines has also focused the interest of researchers in traumatic injury on other organs.7 Of particular interest to our discussion on injury to the central nervous system is the recent study by LaPar et al.13 on cytokine profiles in patients with no traumatic and traumatic head injuries. This study involved 1,022 patients over 5 years, making it one of the largest retrospective studies on cytokine profiles. Various cytokines were measured within 72 h of admission, including TNF-α and IL-1β. There appeared to be little differences in IL-1β between groups; however, TNF-α was shown to be significantly higher in patients with no traumatic head injury.13 This study raised the question of whether the severity of injury to the head (assessed with the Head Injury Severity Score) affected cytokine profiles, or, more broadly speaking, whether there is a correlation between cytokine profiles and the level of damage to the central nervous system. In extending this question, they also examined whether prognosis can somehow be reflected by cytokine levels. Researchers grouped patients according to mortality or survival, but concluded that there were no significant differences between IL-1β and TNF-α with regard to prognosis.
In attempting to evaluate a similar type of question, we investigated whether improvements in AIS grades over the course of the study reflected different cytokine profiles—in other words, whether a distinct cytokine expression pattern could be detected in patients with a better prognosis. Patients were grouped into two groups, improved AIS or not improved. Overall, we saw that there was significant relationship between improved AIS grades and a fall in TNF-α after 9 h and an increase after 72 h and at later time points in this study. Lower levels of TNF-α were seen in patients with improved AIS in the first week after injury and significantly higher levels of TNF-α were seen in these patients thereafter. IL-1β levels were highly variable in both groups during the first week, and appeared to decline after the second week. Regarding TNF-α specifically, our data do not suggest that high levels of TNF-α after 72 h contribute to a worsening in neurological prognosis. Interestingly, Vidal et al.14 suppressed TNF-α after 14 days in SCI mice and concluded that TNF-α has no influence on neurological remission during the early chronic phase of SCI (2–3 weeks post SCI). Our results are consistent with this study in showing that higher TNF-α levels were found in patients after 2 weeks who had improved AIS grades, suggesting that TNF-α does not necessarily exacerbate neurological damage in this early chronic phase of injury and TNF-α-blockers would not improve prognosis so late after injury (Figures 1a and b). On the other hand, our data do not discount the fact that acute blockage of TNF-α could have some therapeutic benefit. Pearse et al.15 observed that cyclic AMP given acutely reduced TNF-α levels in mice greatly, which could have been one of the mechanisms leading to functional recovery after SCI. In our study, neurological improvement appeared to be reflected by lower levels of TNF-α in the first week, especially in the first 72 h, suggesting that reducing TNF-α in this early phase of injury could have some benefit for the patient. Other studies have shown that there are other relevant factors not investigated in this study associated with changes in cytokines. For example, authors have shown that cytokine concentrations after injury appear to be highest in injured tissue and there are differences in systemic and local measurements.16 There also appears to be a correlation between cytokine levels and distance from the lesion.7 Understanding this spatial and temporal relationship of cytokine levels could be beneficial in targeting cytokines in the process of tissue repair and regeneration 17 and would be of interest in investigating SCI. Because of the obvious problems in extraction of tissue samples from the spinal cord, we were only able to use venous blood as our medium. We were able to show a temporal cytokine expression pattern for IL-1β and TNF-α in serum, but we do not know whether the results reflect temporal differences at the site of the lesion. This would be an interesting question to evaluate in a further study. Further limitations to this study were the small sample size and the differences in the demographics and AIS grades of groups (Table 1). Further stratification of the data based on AIS grade was not meaningful because of the small size of the collective, making the value of cytokine expression as a prognostic marker unclear. A much larger patient collective would perhaps remove baseline differences in groups and produce more conclusive results. It is also worth noting that there is some concern that the AIS classification is limited in assessing neurological improvement.18 Spontaneous AIS conversions following SCI have been documented in the literature,19 and this possible source of error should be considered in future studies investigating similar questions. In addition, there is evidence in the literature that cytokine production is influenced by circadian rhythms. Authors have shown that macrophages secrete cytokines based on a circadian clock in mice.20 A circadian-dependent secretion could have influenced the levels found in SCI patients and account for the variability of our results, although more investigation of this topic in humans is needed.
Our study and others suggest that the observation of peripheral cytokines could present a method for tracking the course of SCI and for better understanding this process. Although we were not able to show the prognostic value of our methods because of the limited size of our collective, our results imply that measuring cytokine expression patterns after SCI is meaningful to explore and potentially useful in developing innovative approaches for treating acute and sub-acute SCI.
DATA ARCHIVING
All patient data were archived anonymously according to guidelines set forth by the ethics committee, and serum was frozen at −80° for future study.
References
Fehlings MG, Baptiste DC . Current status of clinical trials for acute spinal cord injury. Injury 2005; 36: B113–B122.
Rowland JW, Hawryluk GW, Kwon B, Fehlings MG . Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 2008; 25: E2.
Beattie MS, Hermann GE, Rogers RC, Bresnahan JC . Cell death in models of spinal cord injury. Prog Brain Res 2002; 137: 37–47.
Beattie MS . Inflammation and apoptosis: linked therapeutic targets in spinal cord injury. Trends Mol Med 2004; 10: 580–583.
Keane RW, Davis AR, Dietrich WD . Inflammatory and apoptotic signaling after spinal cord injury. J Neurotrauma 2006; 23: 335–344.
Silva NA, Sousa N, Reis RL, Salgado AJ . From basics to clinical: a comprehensive review on spinal cord injury. Progr Neurobiol 2013; 114: 25–57.
Currie HN, Loos MS, Vrana JA, Dragan K, Boyd JW . Spatial cytokine distribution following traumatic injury. Cytokine 2014; 66: 112–118.
Pape HC, Schmidt RE, Rice J, van Griensven M, das Gupta R, Krettek C et al. Biochemical changes after trauma and skeletal surgery of the lower extremity: quantification of the operative burden. Crit Care Med 2000; 28: 3441–3448.
Biglari B, Buchler A, Swing T, Biehl E, Roth HJ, Bruckner T et al. Increase in soluble CD95L during subacute phases after human spinal cord injury: a potential therapeutic target. Spinal Cord 2013; 51: 183–187.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Hayes KC, Hull TC, Delaney GA, Potter PJ, Sequeira KA, Campbell K et al. Elevated serum titers of proinflammatory cytokines and CNS autoantibodies in patients with chronic spinal cord injury. J Neurotrauma 2002; 19: 753–761.
Davies AL, Hayes KC, Dekaban GA . Clinical correlates of elevated serum concentrations of cytokines and autoantibodies in patients with spinal cord injury. Arch Phys Med Rehab 2007; 88: 1384–1393.
LaPar DJ, Rosenberger LH, Walters DM, Hedrick TL, Swenson BR, Young JS et al. Severe traumatic head injury affects systemic cytokine expression. J Am Coll Surg 2012; 214: 478–486 discussion 86-8.
Vidal PM, Lemmens E, Geboes L, Vangansewinkel T, Nelissen S, Hendrix S . Late blocking of peripheral TNF-alpha is ineffective after spinal cord injury in mice. Immunobiology 2013; 218: 281–284.
Pearse DD, Pereira FC, Marcillo AE, Bates ML, Berrocal YA, Filbin MT et al. cAMP and Schwann cells promote axonal growth and functional recovery after spinal cord injury. Nat Med 2004; 10: 610–616.
Hauser CJ, Zhou X, Joshi P, Cuchens MA, Kregor P, Devidas M et al. The immune microenvironment of human fracture/soft-tissue hematomas and its relationship to systemic immunity. J Trauma 1997; 42: 895–903.
Werner S, Grose R . Regulation of wound healing by growth factors and cytokines. Physiol Rev 2003; 83: 835–870.
Gundogdu I, Akyuz M, Ozturk EA, Cakci FA . Can spinal cord injury patients show a worsening in ASIA impairment scale classification despite actually having neurological improvement? The limitation of ASIA Impairment Scale Classification. Spinal cord 2014; 52: 667–670.
Spiess MR, Muller RM, Rupp R, Schuld C, Group E-SS, van Hedel HJ . Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. J Trauma 2009; 26: 2027–2036.
Keller M, Mazuch J, Abraham U, Eom GD, Herzog ED, Volk HD et al. A circadian clock in macrophages controls inflammatory immune responses. Proc Natl Acad Sci USA 2009; 106: 21407–21412.
Acknowledgements
We thank Mr Fabian Ritter of BG RCI (Insurance Association of the Chemical Industry) for providing financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Biglari, B., Swing, T., Child, C. et al. A pilot study on temporal changes in IL-1β and TNF-α serum levels after spinal cord injury: the serum level of TNF-α in acute SCI patients as a possible marker for neurological remission. Spinal Cord 53, 510–514 (2015). https://doi.org/10.1038/sc.2015.28
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.28
This article is cited by
-
Prognostic value of the systemic inflammatory index (SII) and systemic inflammatory response index (SIRI) in patients with traumatic spinal cord injury
European Spine Journal (2024)
-
Glial fibrillary acidic protein is a robust biomarker in cerebrospinal fluid and peripheral blood after traumatic spinal cord injury: a prospective pilot study
Acta Neurochirurgica (2023)
-
The Role of Tumor Necrosis Factor Following Spinal Cord Injury: A Systematic Review
Cellular and Molecular Neurobiology (2023)
-
Correlation between miRNA-124, miRNA-544a, and TNF-α levels in acute spinal cord injury
Spinal Cord (2022)
-
The inflammatory response and blood-spinal cord barrier integrity in traumatic spinal cord injury: a prospective pilot study
Acta Neurochirurgica (2022)