Abstract
Study design:
Spinal tuberculosis as all other osteoarticular tuberculosis occurs as a result of hematogenous dissemination of Mycobacterium tuberculosis from a primarily infected visceral focus mainly lungs, but Pott’s paraplegia occurring secondarily to Scrofuloderma has not been reported till date.
Purpose:
To document such an association of Pott’s paraplegia and Scrofuloderma.
Methods:
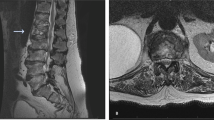
A 29-year-old female presented to us with low backache and paraplegia of 1 month duration. Clinical examination showed multiple healed Scrofuloderma lesions over sterum and neck (Figure 1). Magnetic resonance imaging (Figure 4), computed tomography (Figure 3) and X-ray (Figure 2) showed Pott’s spine involving dorsal vertebrae (D8–10) with pre and paravetebral abscess with intraspinal extension. She was treated by minimally invasive surgery to drain pus and granulation tissue by resecting transverse process of D9 vertebra. Drained material was sent for histopathological examination, Zielh-neelsen (ZN) staining, culture and sensitivity for M. tuberculosis. Patient completely recovered neurologically after 1 month of surgery.

Clinical photographs showing multiple healed Scrofuloderma lesions over neck and sternum.

X-ray dorso lumbar spine antero-posterior view showing lateral translation of D9 over D10 vertebra.
Results:
Patient completely recovered neurologically after surgery and is presently on multidrug chemotherapy and spinal brace.
Conclusions:
Pott’s paraplegia can occur secondary to Scrofuloderma and it can be managed by multidrug antitubercular therapy and minimally invasive surgical procedure.
Similar content being viewed by others
Introduction
Extrapulmonary tuberculosis constitutes 15–20% of all cases of tuberculosis. Osteoarticular tuberculosis accounts for 1–3% of all tuberculosis patients,1 while skin tuberculosis constitutes 1–2% of all extrapulmonary tuberculosis.2 Scrofuloderma is one type of skin tuberculosis, which occurs due to direct involvement and breakdown of skin from contiguous tubercular foci–like-infected lymph node or bone. It is uncommon to have another site of active tuberculosis far away from the one responsible for Scrofuloderma. A single case report on two occasions has been published showing association between Scrofuloderma, Psoas abscess and caries spine of lumbar vertebrae without neurological deficit.3, 4 We present a case of pott’s paraplegia involving D8–10 vertebrae 5 years after Scrofuloderma lesions over neck and sternum.
Case report
A 29-year-old female presented to us with history of low backache and inability to walk for last 1 month. Pain was insidious in onset, dull aching in character, non-radiating and aggravated by coughing, sneezing and attempted movement of trunk. She had history of loss of appetite and weight loss. She had no history of trauma, chronic cough, hemoptysis, altered bowel and bladder habits and history of immunodeficiency virus (HIV) contact. There was past history of multiple Scrofuloderma lesions over neck and sternum (Figure 1) 5 years back, which was proved by biopsy. Patient was given multidrug chemotherapy for 9 months and the lesions healed completely. General physical examination was insignificant with no lymphadenopathy or organomegaly. Patient had spastic paraplegia in extension and no voluntary control of both lower limbs. Spinal examination revealed tenderness over D8–10 vertebrae with paravertebral muscle spasm. There was no sensory and bowel bladder involvement. On examination, knee and ankle jerks were brisk, patellar ankle clonus were present and bilateral plantar reflexes were up going. There were multiple healed skin lesions due to Scrofuloderma in neck and sternal region (Figure 1). Hematological and biochemical investigations revealed erythrocyte sedimentation rate (62 mm/1st h), montoux test showed induration of 24 × 26 mm, hemoglobin 11 mg dl−1 and total leukocyte count 8400 mm−3, hepatitis B surface antigen was negative, enzyme immunoassays for human HIV infection was negative. Ultrasound abdomen showed no organomegaly and lymphadenopathy. Urine routine microscopy was within normal limits. X-ray showed paradiscal destruction of D9–D10 vertebrae with diminished disc space and lateral translation of D9 over D10 vertebrae (Figure 2). Computed tomography (Figure 3) further revealed destruction of lamina and pedicle of D9 vertebrae and posterior part of 9th rib. It also showed anterior scalloping of D7 and D8 vertebrae with pre and paravertebral abscess with intraspinal extension. Computed tomography of chest indicated no fresh or healed tubercular lesions and hilar lymphadenopathy. Magnetic resonance imaging (Figure 4) in addition showed multiloculated pre and paravertebral collection causing scalloping of anterior aspect of vertebrae seen at D7–D11 vertebrae, with extension into neural foramina at D8/D9, D9/D10 with ventral epidural component compressing thecal sac with cord edema at the same level. There was no evidence of myelomalacia or syrinx formation. Patient was diagnosed clinicoradiologically as a case of Pott’s paraplegia. Keeping in view of neurological deficit and lateral translation of involved vertebrae with involvement of pedicle and laminae of D9 vertebra treatment initially thought of was spinal decompression and stabilization, but as it was a case of recurrence, we suspected resistant infection and did minimally invasive transversectomy of D9 vertebrae to attain material (granulation tissue and pus), which was subjected for histopathological and microbiological examination and indirectly decompressing the tense abscess. Patient was put on multidrug antitubercular therapy with complete bed rest. Patient showed early motor recovery within first 24 h, leading to complete motor recovery within 1 month. Histopathological examination showed tubercular granuloma and on ZN stain no acid fast bacilli. Culture revealed M. tuberculosis sensitive to all first-line antitubercular drugs. Patient was mobilized on Taylor’s spinal brace support and was started on gradual back extension exercise 3 months after surgery.
Discussion
Cutaneous tuberculosis is a well-known entity prevalent in temperate and tropical climates, but due to global increase in HIV infection the incidence of cutaneous tuberculosis is raising worldwide.5 A single case report on two occasions has been published showing association between Scrofuloderma, psoas abscess and lumbar vertebral caries spine without neurological deficit,3, 4 our case highlights paraplegia due to tuberculosis of spine involving dorsal vertebrae secondary to multiple healed Scrofuloderma lesion at cervical and sternal region, which has not been reported in literature up till date and being managed by minimally invasive decompression leading to full neurological recovery. Although such rare cases may present without multidrug resistant (MDR) tuberculosis or HIV infection, which can be managed on multiple lines of treatment: minimal invasive to radical debridement and spinal fixation.
References
Tuli SM . Tuberculosis of the Skeletal System (Bones, Joints, Spine and Bursal Sheaths) Second ed. Jaypee Brothers Medical Publishers (P) Ltd: New Delhi. 1991 pp 3–122.
Sethuraman G, Ramesh V . Cutaneous tuberculosis in children. Pediatr Dermatol. 2013; 30: 7–16.
Sehgal VN, Chander R, Garg VK, Karmakar S . Scrofuloderma of the scalp, psoas abscess, and caries spine: an unusual association. J Dermatol 1994; 21: 42–45.
Sehgal VN, Jain S, Thappa DM, Logani K . Scrofuloderma and caries spine. Int J Dermatol 1992; 31: 505–506.
Dye C . Global epidemiology of tuberculosis. Lancet 2006; 367: 938–940.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kanojia, R., Kalra, M., Sareen, A. et al. Pott’s paraplegia secondary to Scrofuloderma is a rare association. Spinal Cord 51, 931–933 (2013). https://doi.org/10.1038/sc.2013.101
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2013.101