Abstract
Background:
Disability scales do not enable the transmission of concise, meaningful and daily function description for clinical purposes.
Study design:
Cross-sectional statistical analysis of 328 patients’ Spinal Cord Independence Measure (SCIM) III item scores (SIS).
Objective:
To develop a concise and clinically interpretable data-based characterization of daily task accomplishment for patients with spinal cord lesions (SCLs).
Setting:
Multi-center study at 13 spinal units in 6 countries.
Methods:
Patients were grouped into clusters characterized by smaller differences between the patients’ SIS within the clusters than between their centers, using the k-medoides algorithm. The number of clusters (k) was chosen according to the percent of SIS variation they explained and the clinical distinction between them.
Results:
Analysis showed that k=8 SIS clusters offer a good description of the patient population. The eight functional clusters were designated as A–H, each cluster (grade) representing a combination of task accomplishments. Higher grades were usually (but not always) associated with patients implementing more difficult tasks. Throughout rehabilitation, the patients’ functional grade improved and the distribution of patients with similar functional grades within the total SCIM III score deciles remained stable.
Conclusions:
A new classification based on SIS clusters enables a concise description of overall functioning and task accomplishment distribution in patients with SCL. A software tool is used to identify the patients’ functional grade. Findings support the stability and utility of the grades for characterizing the patients’ functional status.
Similar content being viewed by others
Introduction
Easy and concise transmission of information about daily task accomplishment, essential for effective use of functional assessment during care and rehabilitation after spinal cord lesions (SCLs), requires an instrument that describes the patients’ functional status concisely. Such an instrument may resemble the combination of lesion level and American Spinal Injury Association impairment scale (AIS) grade, which describes briefly the neurological status and provides abundant information on neurological deficit, its distribution and its prognosis.1
A similarly concise description of function after SCL may not be feasible because of the large number of possible combinations of task scores. But these combinations are not random, and patterns can be identified. Different tasks have varying levels of difficulty, and patients with higher overall functionality tend to show better accomplishments in the more difficult tasks.2, 3, 4 This made possible the investigation of the functional significance of the total Functional Independence Measure motor score using ordinal logistic modeling of its relationship with the independence level of single motor-Functional Independence Measure items in patients with hemiplegia after stroke.4 It also allowed developing a staging system, based on Functional Independence Measure, for functional independence across the activities of daily living for various types of disabily.5 The same patterns may also facilitate a concise description of functionality after SCL.
The total score of disability rating scales, including those used for patients with SCL, has been frequently used for the brief description of overall capacity or task accomplishment in daily activities.6 In many of these scales, however, the total score is computed by summation of the scores of scale items, which are not weighted for their relative contribution to overall functioning. It is not clear, therefore, to what extent the total score represents overall capacity or task accomplishment.
In some disability scales used with patients with SCL, such as the Barthel Index, the Quadriplegia Index of Function and the Spinal Cord Independence Measure (SCIM), item scores are weighted for their relative contribution to the total score, which improves the significance of the total score.7 But even for these scales, the functional significance of the total score is not obvious. Although higher scores represent higher functionality, and a patient with a total score below a minimal value (which is the sum of the minimal item scores representing independent functioning—70 for SCIM III) is not totally independent: identical cumulative scores can reflect the summation of different item scores, and patients with similar total scores may present different combinations of task accomplishment.
The present study was designed to develop a grading instrument that describes (a) the actual combination of daily task accomplishment in patients with SCL and (b) overall patient functionality. To this end, we further analyzed data of patients who participated in the study for the international validation of SCIM III.2, 8
Methods
Patients
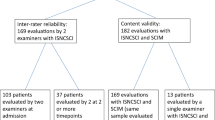
A total of 425 patients with SCL undergoing rehabilitation in 13 SCL centers in six countries in North America, Europe and the Middle-East were included in the international SCIM III study.2, 8 Thirty-seven patients were excluded because they lacked full SCIM III scores at admission, and 61 additional patients were excluded because they lacked data at discharge. A total of 328 patients had sufficient data for this analysis. Inclusion criteria were a SCL (AIS A, B, C or D) and age ⩾18 years. Patients with concomitant impairments, such as brain injury or mental disease, or any other condition that might influence their everyday function were excluded.
The mean age of the 328 patients was 47.6 years (s.d.=18.2). Overall 70% were men. Of all 46% had tetraplegia and 53.9% had paraplegia. AIS grade was A in 34.4% of the patients, B in 14.7%, C in 20.9% and D in 29.8%. Lesion etiology was traumatic in 59.5% of patients and non-traumatic in 40.5%. The non-traumatic etiologies were disc protrusion in 14.3%, benign tumor in 19.5%, spinal stenosis in 14.3%, myelopathy of unknown origin in 11.3%, vascular impairment in 6.8%, syringomyelia in 3.0%, decompression sickness in 2.3%, multiple sclerosis in 1.5%, congenital anomaly in 1.5%, spinal abscess in 1.5%, metastatic disease in 1.5% and other in 22.6%.2, 7
The mean time interval from injury or SCL onset (the earliest event related to SCL in a patient's hospital records) to admission was 217.8 days (s.d.= 914.8), and between admission to rehabilitation and discharge it was 133.7 days (s.d.=88.1).
Scoring procedure
All patients were evaluated with the SCIM III questionnaire within a week following admission to a rehabilitation program and within a week before program discharge. SCIM III items were scored by direct observation, by expert professionals selected at each centre (a physician, nurses, occupational therapists or physiotherapists). In exceptional cases, as for example in the case of bowel habits for which direct rater observation was troublesome, some tasks were scored based on information obtained from a staff member who observed the patient during routine care. Patient data and SCIM III scores were collected at each participating centre and pooled for analysis.
Analysis
To identify functional grades that can describe concisely the functional status of SCL patients, we clustered patients according to their SCIM III item score (SIS) profiles obtained during the first week of rehabilitation. For cluster analysis we used the k-medoides algorithm, as implemented in the ‘PAM’ package of R software (2010).9
For each possible number of clusters k, patients were divided into k clusters, each cluster having its own center. The division minimized the average distance between patients’ SIS profiles and their assigned-cluster center relative to the average distances between the cluster centers and the overall center of all patients.
For the clustering we used both the Euclidean distance, where the mean and s.d. serve as summaries, and the sum of absolute deviation distances (l1 distance), where the median and the average absolute deviation serve the same purposes. The results were quite similar. We chose to report the l1 distance for three reasons: (a) the distance reflects correctly both the relative weight of the items in the total daily function and the fact that the total SCIM III assessment of the degree of task implementation is approximately linear; (b) the resulting cluster centers were not sensitive to the initial values used in the algorithm and (c) calculations for future patients are relatively easy to perform.
The appropriate number of grades was chosen in two steps. First we studied the relationship between the number of clusters and the percent of SIS variation explained by them. In the second step, physicians examined the clinical significance of each possible set of clusters in the range suggested by the relationship in the first step.
The relationship between functional grades and total SCIM III scores (TSSs) was analyzed using a conditional distribution of patients within TSS deciles among the grades, as well as by Spearman's correlation between the grades and TSS.
Spearman's correlation was also used to assess the correlation of the functional grades with the AIS grades and the SCL level, and the differences between the paraplegia and tetraplegia distribution among grades were examined using a χ2 test.
SIS distribution among TSS deciles, and their distribution within the identified functional grades were determined at admission to rehabilitation and compared with those at discharge, using the Fisher exact test, to infer about the effect of rehabilitation on the functional grading and its relationship with the TSS. Both tests were adjusted for multiplicity using the false discovery rate. Patients at discharge were assigned to the nearest cluster, using their SCIM score at discharge.
Identifying an individual's functional grade
The centers of the clusters, identified by the analysis and the k-medoides algorithm, were entered into a software tool called ‘SCIMgradesoft.’ The tool, available at http://www.scimscore.com, was designed to identify individuals’ functional grades based on their SIS. The software calculates the distances from the centers of the predetermined clusters and identifies the nearest cluster center, thereby indicating the individual's functional grade.
Results
After generating k=3,4,…,20 clusters, we observed an increase in the percent of SIS variation explained by the clusters, which was almost linearly related to k when k⩽7, and a reduction in that increase when k>7, with an elbow effect when k=7–10 (Figure 1). Eight clusters explained 76.2% of the variation between individual SIS, and their centers were found to reflect distinct meaningful clinical states better than did a larger number of clusters. We concluded, therefore, that eight SIS clusters identified by the analysis can serve as functional grades, called ‘SCIM III grades.’
Table 1 presents the centers of the clusters. A center is the set of scores (one for each item) chosen to minimize the sum of the absolute deviations of all item values of patients in the cluster. Each curve in Figure 2 contains the item scores profile of the center of each cluster (or SCIM III grade), showing the median TSS for each center. The eight clusters were assigned the letters A–H, according to the TSS ranking. Despite this convention, the correlation coefficient between the grade and the TTS is only 0.65.
SCIM III item scores for the centers )the set of scores minimizing the sum of the absolute deviations of all item values of patients in the cluster( of the eight clusters (grades) a–h, presented by the dark lines. The median total score of each cluster is shown on the right. The light lines in the background represent score profiles of individual patients in each cluster.
The SCIM III grade also showed a significant but weaker correlations with the AIS grade and with the SCL level (r=0.446, 0.25; P<0.001). The distribution of patients across the functional grades was different for tetraplegia and paraplegia (P<0.001): patients with tetraplegia were the majority in the grades A and B, and a minority in C and E. In the other grades the difference in paraplegia or tetraplegia frequency was nonsignificant.
The functional grades of patients who participated in the SCIM III international study changed during rehabilitation, as shown in Table 2 (in percentages of the initial number of patients with each grade). Of the patients admitted with grade A, 37.0 were discharged with grade B and 7.4% with H, whereas 34.5% of the patients admitted with grade F, and 47.6% of those admitted with grade G, achieved grade H at discharge.
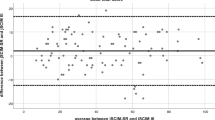
The functional grade distribution for each total SCIM III decile range, at admission and at discharge, is shown in detail in Figure 3. Patients with a TSS in the same decile may have one of up to five different functional grades. Similarly, some clusters extend over a range of up to four deciles of TSS. The distribution of patients within each TSS deciles between the functional grades is similar at admission to rehabilitation and at discharge, except in the lowest and third deciles. For the third decile, the difference is statistically significant for each test individually (P=0.024 and 0.016) but not after adjusting for multiplicity.
SCL patients with a functional grade of A–F are likely to require some assistance in carrying out some daily activities. Patients with the highest grade, H, can probably carry out all SCIM III tasks without assistance. Table 3 shows examples of the likely task accomplishment level of patients in each of the eight functional grade clusters.
When a patient's SISs are known, the functional grade can be obtained by (a) adding the absolute differences between all the scores of each item and the value of that item in the center of the grade, for each grade and (b) choosing the grade for which that value is the smallest. The SCIMgradesoft application can be used to calculate a patient's functional grade automatically. When a patient's SISs are not known but the functional grade (A–H) is known, a reasonably accurate assessment of the patient's level of accomplishment on various daily tasks can be derived from the information presented in Figure 2.
Discussion
This study is the first attempt to classify SCL patients based on a functional grading that describes the composition of SCIM III task accomplishment. Patients in the study were algorithmically clustered into eight groups by functional level, and characteristic activity patterns were described for each group, reflecting achievements in each domain of daily function.
Grouping enabled classification of the functional level into eight SCIM III grades, in a manner similar to that of Frankel and AIS grading of neurological impairment.10, 11 Grouping also provided a tool that can demonstrate the functional meaning of the TSS, as reflected in the accomplishment of various daily tasks. Functional score combinations with distinct clinical significance allowed the delineation of patterns of activity level that have a fair chance of being predicted by the SCIM III grade in clinical settings.
Higher SCIM III grades tend to indicate better execution of more difficult tasks. Conversely, lower grades tend to indicate that a higher amount of assistance is required (Table 1, Figure 2, Appendix). However, the different grades indicate not so much the general level of task execution as a different composition of abilities. The relatively low correlation between the grade and the TTS, as well as the mismatch between the functional grades (each one including patients with similar SIS score composition) and the TSS deciles confirm that the classification of patients with SCL into the eight functional grades is not a mere reflection of the sum of the patient's scores across items. These findings support the notion that unlike the TSS, the grades are appropriate for characterization of the patient's complex task accomplishment profile.
The significant but weak correlations of the SCIM III grade with the AIS grade and with the SCL level is compatible with the tendency of functionality to reflect SCL severity and level to some extent, depending on the combination of severity and level.
Rehabilitation had a considerable and positive effect on the functional grade attainment of patients in our sample. The vast majority of patients progressed to higher functional grades during rehabilitation, which supports the validity of the suggested functional classification. Of patients with a SCIM III grade of A on admission, 70.4% achieved a higher functional grade at discharge from rehabilitation, as did 80.5% of patients with an initial grade of B, 89.8% with C, 80.3% with D, 76.9% with E and 62.1% with F. Only in the group of patients with an initial grade of G, fewer than half the patients (47.6%) improved their functional level, which may be attributed to a ceiling effect. This may also explain the decline in functional grade progress from grade D onward (Table 3). It would appear that patients with a SCIM III grade of C have the highest potential for functional improvement, which parallels the highest potential for neurological improvement of patients with Frankel C SCL.12, 13
Seven patients with initial functional grades D–H deteriorated to lower functional grades at discharge. The most prominent deteriorations were in bladder and bowel management, which may reflect either a loss of abilities that were initially preserved or misinterpretation of the initial functional condition.
The general similarity in the distribution of the patients with the same functional grades within TSS deciles at admission and at discharge indicates that changes in rehabilitation stage and patient condition do not affect the relationship between the grades and the overall functional status. This observed relationship supports the reliability and usefulness of the classification, although a larger multi-center study could potentially provide additional data to further validate the stability of the grades.
For research purposes, the suggested classification may be suitable for grouping patients with SCL according to clinically meaningful functional grading. For clinical purposes, the classification may be used to quickly obtain a reasonable description of a patient's task accomplishment in various functional domains, using the available SCIM III grade and the information provided in Table 1. By comparison, other functional assessment instruments require addressing many items (for example, 19 in SCIM III) to obtain a meaningful picture of the patient's functional status. This may assist clinical decision processes, which involve interaction between classification and measurement of function.14 We suggest adding the SCIM III grade to the diagnoses recorded in the patient's records, for example, ‘SCIM III 60F’ (SCIM III total score=60, SCIM III grade=F).
Adding the 61 patients with missing discharge data to the cluster analysis had only a small effect on the results. New data from additional patients and centers may change the centers of the clusters slightly. Given the clinical interpretation of the current grades, however, we believe that their structure will remain stable.
Obtaining the SCIM III grades using the currently available method requires a full set of SCIM scores items. Methods for obtaining SCIM III grades with incomplete sets of scores are under development, but require further research.
It must be emphasized that information on the grades of individuals whose scores show large deviations from the center of their cluster (Figure 2) should be accompanied by details of their individual achievements on items on which their accomplishment was atypical for their assigned grade. This reservation stems from the main limitation of the classification: that although the combinations of task score distributions were not random, neither were they uniform for all patients, and the characteristic patterns of activity level may not reflect the actual task accomplishment in some patients. This limitation must be considered when assessing a specific patient, just as the limitations of AIS grading must be considered in patients with central cord or thoracic SCL. With this reservation in mind, SCIM III grading can be safely used to identify the functional status of individual patients. Furthermore, SCIM III grading can serve as an important tool for refining case-mix classification algorithms when comparing clinical departments or facilities within a country or across countries.
In conclusion, SCIM III clusters that differ in their functional significance can be used for functional grading of SCL and for clarifying the meaning of the TSS, for both clinical and research purposes. The description of characteristic activity patterns for each grade can reflect task accomplishment in each domain of daily function, and may be used to obtain a reasonable picture of a patient's task accomplishment in various functional domains. The changes in SCIM III grades and the stability of their relationship with the TSS throughout rehabilitation support the validity and the reliability of the classification.
References
Fromovich-Amit Y, Biering-Söerensen F, Baskov V, Juocevicius A, Vest-Hansen H, Gelernter I et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord 2009; 47: 597–603.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multi-center international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Prasad R, Hellawell DJ, Pentland B . Usefulness of the Functional Independence Measure (FIM), its subscales and individual items as outcome measures in Guillain Barré syndrome. Int J Rehabil Res 2001; 24: 59–64.
Tetsuo KM, Okuno T, Kazuhisa D . Relationship between independence level of single motor-FIM items and FIM-motor scores in a patient with hemiplegia after stroke: an ordinal logistic modeling study. J Rehabil Med 2006; 38: 280–286.
Stineman MG, Ross RN, Fiedler R, Granger CV, Maislin G . Functional independence staging: conceptual foundation, face validity, and empirical derivation. Arch Phys Med Rehabil 2003; 84: 29–37.
Catz A, Itzkovich M . Trends in the assessment of functional outcomes after spinal cord lesions. In: Soroker N, Ring H (eds). Advances in Physical and Rehabilitation Medicine. Monduzzi: Bologna, 2003, pp 123–127.
Anderson K, Aito S, Atkins M, Biering Sorensen F, Charlifue S, Curt A et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med 2008; 31: 133–144.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The Spinal Cord Independence Measure (SCIM) version III: Reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
R Development Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2009 ISBN 3-900051-07-0 http://www.R-project.org.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969; 7: 179–192.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Catz A, Thaleisnik M, Fishel B, Ronen J, Spasser R, Folman Y et al. Recovery of neurologic function after spinal cord injury in israel. Spine 2002; 27: 1733–1735.
Catz A, Goldin D, Fishel B, Ronen J, Bluvshtein V, Gelernter I . Recovery of neurologic function following nontraumatic spinal cord lesions in Israel. Spine 2004; 29: 2278–2282.
Tesio L . Functional assessment in rehabilitative medicine: principles and methods. Europa Medicophys 2007; 43: 515–523.
Acknowledgements
This study was supported by the Loewenstein Rehabilitation Hospital Spinal Department Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Bluvshtein, V., Front, L., Itzkovich, M. et al. A new grading for easy and concise description of functional status after spinal cord lesions. Spinal Cord 50, 42–50 (2012). https://doi.org/10.1038/sc.2011.84
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.84