Abstract
Study design:
Retrospective chart review.
Objectives:
This study was performed to compare the outcome, especially the mortality rate, in patients with and without spinal cord injury (SCI) and necrotizing fasciitis (NF).
Setting:
Division of Spinal Cord Injury and Department of Plastic and Hand Surgery, BG-University Hospital Bergmannsheil Bochum, Ruhr-University Bochum, Germany.
Methods:
Twenty-five patients with SCI and thirty patients without SCI treated with NF were included in the study. Mean length of hospital stay, mean age, mean laboratory risk indicator for necrotizing fasciitis (LRINEC) score, mean number of surgical debridements, co-morbidity factors and mortality rate were compared between both groups.
Results:
There were no differences for the mean LRINEC score (P=0.07), mean number of surgical debridements (P=0.18) and co-morbidities (odds ratio=2.32; 95% confidence interval =0.78–6.92) between both groups. Patients with SCI were significantly younger than patients without SCI (P=0.02). Patients without SCI had a higher mortality risk rate (n=9) than patients with SCI (n=2) (relative risk=1.71; 95% confidence interval =1.13–2.6).
Conclusions:
In conclusion, SCI patients have a lower mortality rate than patients without SCI. Age may influence the mortality rate. Nevertheless, we believe that further unknown risk factors might influence the mortality, especially in patients with SCI.
Similar content being viewed by others
Introduction
Necrotizing fasciitis (NF) is a life-threatening infection characterized by fulminant destruction of tissue with associated systemic signs of sepsis and toxicity, with an overall mortality rate of 25–30%.1, 2 It initially affects the fascia followed by the subcutaneous tissue and muscle. Several factors can influence the associated mortality rate. Early diagnosis and radical surgical treatment are pivotal, and have been recognized to alter the prognosis of the disease.1, 2
NF frequently arises from minor skin lesions.3 Cunningham et al.4 reported the first case of necrotizing-soft tissue infection from a pressure sore in a spinal cord injury (SCI) patient, with extension into the spinal canal and spinal cord. In a recent study, the case of a paraplegic patient who developed NF after negative pressure wound therapy in the treatment of a fourth grade pressure sore was described.5 Citak et al.6 found a significantly increased risk of developing NF in patients with SCI, and grade three and four pressure sores. However, until now, there is a lack of data analyzing the outcome after NF in patients with SCI. The present study was performed to compare the clinical outcome, with special focus on the mortality rate of NF, in patients with and without SCI.
Material and methods
All patients who were surgically treated for NF at our hospital between April 2000 and December 2009 were enrolled in the study. Patients without a SCI and NF, who were treated at the Plastic Surgery Department of our clinic, were also included in the study. All patients under the age of 18 and those with Fournier's gangrene were excluded. The medical records were analyzed and following parameters were assessed: age, gender, pre-existing medical conditions, anatomical localization and etiology of NF, number of surgical debridements, length of hospital stay, complication and mortality rate.
The clinical diagnosis of NF was made by attending surgical physicians and was confirmed histologically. In addition, the laboratory risk indicator for necrotizing fasciitis (LRINEC) score was calculated in all patients on admission. The LRINEC score is a numerical score based on the rapidly available laboratory parameters; glucose level, C-reactive protein level, leukocyte count, sodium level, creatinine level, hemoglobin and others. The maximum score is 13, a score ⩾6 is suspicious for NF and a score ⩾8 strongly predictive for NF.7, 8, 9
Aggressive physiological fluid resuscitation, correction of electrolyte imbalances, extensive operative debridement, antiseptic wound-dressing changes using sterile gauzes and wide-spectrum antibiotic therapy were the therapeutic strategy used in all patients. Radical surgical debridement was required in almost every case before soft tissue closure.
Outcome measures
Patients were divided into two groups: (1) NF with SCI and (2) NF without SCI. There were 25 SCI patients and 30 patients without a SCI treated for NF at the authors’ institution during the observation period. Mean length of hospital stay, mean age, mean LRINEC score, mean number of surgical debridements, co-morbidity factors, complication and mortality rate were compared between both groups.
Statistical analysis
All variables were expressed in terms of mean and ±s.d. of the mean. The t test was performed when the data were distributed normally; otherwise the Mann-Whitney test was used. The Shapiro-Wilk normality test was performed to test the null hypothesis that the data had a normal distribution. For all tests, P<0.05 was considered statistically significant. The mortality rate was compared between both groups using relative risk ratio. Number of co-morbidities was compared between patients with SCI and patients without SCI using odds ratio. Statistical analysis was carried out using a statistical software package (GraphPad Prism Version 4.1, GraphPad Software Inc., La Jolla, CA, USA).
Results
There were 25 (9 female and 16 male patients) patients with SCI and 30 patients (17 female and 13 male patients) without SCI treated for NF at the authors’ institution. In patients without SCI, the infection was localized at the lower extremity in 15 cases, followed by the upper extremity in 13 cases and trunk in 2 cases. In the majority of patients with SCI (n=18), the infection was in the lower extremity, followed by the sacral region with six cases. The musculus erector trunci was affected only in 1 case.
Outcome measures
There were no statistically significant differences for the mean LRINEC score (P=0.07) and the mean number of surgical debridements (P=0.18) between both groups. The mean LRINEC score was 7.3 (range 2.0–10.0; s.d.=2.2) for patients without a SCI and 6.6 (range 3.0–10.0; s.d.=1.8) for patients with a SCI. A mean of 4 (range 0–10 operations; s.d. 2.7) surgical interventions were necessary during the treatment period for patients without a SCI, whereas patients with a SCI required a mean of 3.6 (range 1–22 operations; s.d.=5.0) surgical interventions.
Patients with a SCI were significantly younger (47 years ±13.3) than patients without a SCI (55.0 years ±14.6) (P=0.02). The mean length of hospital stay for patients without SCI was 28 days (s.d.=19.4), significantly shorter compared with SCI patients whose mean length of hospital stay was 91.8 days (±72.8) (P<0.0001).
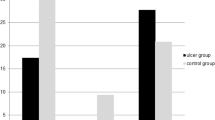
Patients without SCI had more co-morbidities with 17 cases, compared with SCI patients with 9 cases. However, there was no significant difference (odds ratio=2.32; 95% confidence interval=0.78–6.92) between both groups. The most common co-morbidity factor was diabetes mellitus with 40% in patients without SCI, whereas diabetes mellitus was registered only in 4% of SCI patients. The mortality rate in patients without SCI (n=9) was higher than in patients with SCI (n=2) (relative risk=1.71; 95% confidence interval=1.13–2.6). Detailed information is given in Table 1.
Discussion
Previous studies have analyzed specific risk factors for NF in patients without a SCI, for example. diabetes mellitus, obesity, peripheral vascular disease, age and female gender.1, 2, 10, 11 Elliott et al.1 reported on associated mortality and strategies for optimal management of NF in general. This is the first study comparing the overall outcome in patients with and without a SCI treated for NF.
We found no significant differences for the mean LRINEC score and the mean number of surgical interventions in both groups. The mean duration of hospital stay was significantly longer in patients with SCI compared with patients without SCI. However, regular check-up and examinations like urodynamic test for the urinary bladder dysfunction or optimization of the antispasticity medication in patients with SCI accounted for the prolonged hospitalization.
Interestingly, the overall mortality rate in patients with SCI and without SCI was 8% and 30%, respectively. The mortality rate in patients without SCI correlated well with the current literature.1, 2 In contrast, our results showed a significantly lower mortality rate of NF in patients with SCI compared with patients without a SCI. Su et al.7 reported that patients with a LRINEC score of ⩾6 have higher rates of mortality and amputation. This was also confirmed in our study. However, there was no statistical significant difference for the LRINEC score between both groups, although the mortality rate was higher in patients without SCI. Most of the patients in our study with SCI developed NF because of pressure sores of the pelvic trochanteric area of the body.
Several studies have shown a higher mortality rate with increasing co-morbidities and age.12, 13, 14, 15 In our study, a significant difference for co-morbidities was not found between both groups. However, SCI patients were significantly younger compared with patients without a SCI. The younger age in the SCI group may influence the mortality rate and is a potential limitation of the current study. However, we believe that there exist more unknown potential risk factors that might influence the mortality rate, especially in patients with SCI. Hume et al. found that adrenocorticotropic hormone concentration after SCI is significantly less than before the injury.16 A lower concentration of adrenocorticotropic hormone after SCI leads to lower cortisol concentration that decreases the immune reaction and might result in a higher survival rate. A low mortality rate among patients with SCI and associated bacteremia was described by Montgomerie et al.17 However, reasons for the low mortality rate remain unclear. Wang et al.18 showed the association of SCIs and a low-grade chronic inflammatory state as well as endothelial activation. However, the mortality rate was not analyzed in this study. Nevertheless, this might be a possible reason for the lower mortality rate of NF in patients with SCI. A better insight into the pathophysiology of NF in patients with SCI is needed to explain the decrease in mortality. Hence, further studies are essential to enhance the prognosis of NF both in patients with and without SCI.
Conclusions:
In conclusion, patients with SCI have a lower mortality rate than patients without SCI. LRINEC score can be helpful in the early detection of NF. Age may influence the mortality rate. Nevertheless, we believe that additional unknown risk factors might influence the mortality, especially in patients with SCI. Therefore, further clinical and experimental studies are warranted.
References
Elliott DC, Kufera JA, Myers RA . Necrotizing soft tissue infections. Risk factors for mortality and strategies for management. Ann Surg 1996; 224: 672–683.
McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA . Determinants of mortality for necrotizing soft-tissue infections. Ann Surg 1995; 221: 558–563.
Freeman HP, Oluwole SF, Ganepola GA, Dy E . Necrotizing fasciitis. Am J Surg 1981; 142: 377–383.
Cunningham SC, Napolitano LM . Necrotizing soft tissue infection from decubitus ulcer after spinal cord injury. Spine (Phila Pa 1976) 2004; 29: E172–4.
Citak M, Backhaus M, Meindl R, Muhr G, Fehmer T . Rare complication after VAC-therapy in the treatment of deep sore ulcers in a paraplegic patient. Arch Orthop Trauma Surg 2010; 130: 1511–1514.
Citak M, Backhaus M, Tilkorn DJ, O’Loughlin PF, Meindl R, G et al. Necrotizing Fasciitis in Patients with Spinal Cord Injury: An Analysis of 25 Patients. Spine (Phila Pa 1976) 2011; 36: 1225–1229.
Su YC, Chen HW, Hong YC, Chen CT, Hsiao CT, Chen IC . Laboratory risk indicator for necrotizing fasciitis score and the outcomes. ANZ J Surg 2008; 78: 968–972.
Wong CH, Khin LW . Clinical relevance of the LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score for assessment of early necrotizing fasciitis. Crit Care Med 2005; 33: 1677.
Wong CH, Khin LW, Heng KS, Tan KC, Low CO . The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004; 32: 1535–1541.
Asfar SK, Baraka A, Juma T, Ma’Rafie A, Aladeen T, al Sayer H . Necrotizing fasciitis. Br J Surg 1991; 78: 838–840.
Hung CC, Chang SC, Lin SF, Fang CT, Chen YC, Hsieh WC . Clinical manifestations, microbiology and prognosis of 42 patients with necrotizing fasciitis. J Formos Med Assoc 1996; 95: 917–922.
Dellinger EP . Severe necrotizing soft-tissue infections. Multiple disease entities requiring a common approach. Jama 1981; 246: 1717–1721.
Janevicius RV, Hann SE, Batt MD . Necrotizing fasciitis. Surg Gynecol Obstet 1982; 154: 97–102.
Paty R, Smith AD . Gangrene and Fournier's gangrene. Urol Clin North Am 1992; 19: 149–162.
Pessa ME, Howard RJ . Necrotizing fasciitis. Surg Gynecol Obstet 1985; 161: 357–361.
Hume DM, Bell CC, Bartter F . Direct measurement of adrenal secretion during operative trauma and convalescence. Surgery 1962; 52: 174–187.
Montgomerie JZ, Chan E, Gilmore DS, Canawati HN, Sapico FL . Low mortality among patients with spinal cord injury and bacteremia. Rev Infect Dis 1991; 13: 867–871.
Wang TD, Wang YH, Huang TS, Su TC, Pan SL, Chen SY . Circulating levels of markers of inflammation and endothelial activation are increased in men with chronic spinal cord injury. J Formos Med Assoc 2007; 106: 919–928.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Citak, M., Fehmer, T., Backhaus, M. et al. Does spinal cord injury influence the mortality rate in patients with necrotizing fasciitis?. Spinal Cord 50, 338–340 (2012). https://doi.org/10.1038/sc.2011.108
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.108