Abstract
Study design:
Cross-sectional study.
Objectives:
To assess the importance of proprioceptive and vision information on different types of wheelchair seats with regard to postural control in paraplegic individuals during static posture.
Setting:
Centre of Rehabilitation at the University Hospital/FMRP–USP and Rehabilitation Outpatient Clinic at University Hospital/UNICAMP, Brazil.
Methods:
This study involved 11 individuals with paraplegia. All individuals were submitted to an evaluation of static balance with their eyes open and closed in three different types of seats: wheelchair seat, foam seat and gel seat. Balance evaluation was performed by using the Polhemus system, in which body displacements and anteroposterior and mediolateral speeds were assessed in a static seated position in the different types of seats. Data were analyzed using analysis of variance. The differences were considered at P<0.05.
Results:
No statistical differences were found between the three types of seats in terms of displacements and anteroposterior and mediolateral speeds, or between seats with individuals keeping their eyes open or closed (P>0.05). However, it was observed that body displacements were more prominent toward an anteroposterior than a mediolateral direction.
Conclusion:
This study suggests that individuals with paraplegia tend to exhibit a more anteroposterior body displacement than a mediolateral one, with no significant differences between the types of seats in both situations of eyes open and closed.
Similar content being viewed by others
Introduction
Postural control is crucial for performing daily activities, maintaining independence, interacting with the environment and for avoiding respiratory complications and emergence of deformities in individuals with spinal cord injury (SCI).1
Thoracic SCI impairs postural control, depending on both the level and type of lesion. Besides the balance deficits, other factors such as backrest, wheelchair inclination, foot support and seat cushion also influence the correct maintenance of seated posture.
Individuals with thoracic SCI, both high (T2–T8) and low spinal cord injury (T9–T12), have difficulty in maintaining their seated position without compensation and misalignment of their skeletal structure, as the muscle group responsible for posture maintenance2, 3, 4 and pelvic stability5 is lost. Impairment of postural control has been associated with a greater anterior displacement of the trunk during static balance and scapular protraction during dynamic situations.5
Koo et al.6 have demonstrated that patients with paraplegia tend to move their pelvis backward and incline their trunk forward, thus adopting a relaxed posture when sitting on foam seat, whereas wheelchair air seat (Roho cushion) seems to help in maintaining a correct posture. However, Aissaoui et al.7 noted that generic contoured foam promoted greater stability during a reaching task than flat foam and Roho cushion.
Nevertheless, a few studies have been conducted to evaluate the interference of these cushions on the postural control of individuals with SCI in a static seated position.
The objective of this study was to evaluate the influence of different types of wheelchair seats on the postural control of individuals with paraplegia during static posture. Velocities and anteroposterior and mediolateral displacements were assessed during static seated position using six different postures.
Subjects and methods
This study involved patients (male and female; n=11; mean age of 35±10 years) with traumatic SCI at thoracic levels from T2 to T12 (with complete and incomplete lesions, more than 12 months). This study was approved by the Research Ethics Committee of the Ribeirao Preto School of Medicine (FMRP-USP), Brazil. The exclusion criteria were presence of cardiorespiratory diseases, history of cranial-encephalic trauma associated with medullary lesion, vestibulopathies, depression and diabetes mellitus.
Evaluations were performed at the Center of Rehabilitation—CER, Clinical Hospital of Ribeirão Preto, and at the Spinal Cord Injury Rehabilitation Outpatient Clinic, University Hospital of the State University of Campinas, Brazil.
Neurological examination was performed according to the ASIA protocol. The procedure was performed by the same physician who was familiar with the examination.
Demographic characteristics and lesion levels of patients are summarized in Table 1.
Evaluation of static balance was performed using the Polhemus system (POLHEMS 3 SPACE ISOTRAK II, Colchester, Ontario, Canada). This system is based on emission and detection of the magnetic field generated by three perpendicular coils connected to an amplifier. Orientation angles and x, y and z coordination are obtained through signals generated by the three sensory coils. Therefore, the Polhemus system allows the measurement of deviations in the ‘x’ (anteroposterior), ‘y’ (mediolateral) and ‘z’ (vertical) planes. For evaluation, the transmitting coil was positioned next to the patient at a distance of 60 cm, and the sensory coils were attached to the seventh cervical vertebra and first sacral vertebra.
Static balance was evaluated with the patients in a seated position with regard to three types of seats: wheelchair seat (individual seated directly on the wheelchair seat), foam seat (eggcrate seat cushion with cover, 45 × 45 cm, 10 cm thick; 28 g dm–3 density) and gel seat (viscous gel, 40 × 45 cm; 10 cm thick). Static balance was evaluated by means of a protocol previously established for measuring anteroposterior and mediolateral displacements and velocities, with the patient in an upright position as much as possible, away from the backrest, with arms crossed over the chest in six situations: (1) seated on the wheelchair with eyes open for 60 s; (2) seated on the wheelchair with eyes closed for 60 s; (3) seated on a foam cushion with eyes open for 60 s; (4) seated on a foam cushion with eyes closed for 60 s; (5) seated on a gel cushion with eyes open for 60 s; and (6) seated on a gel cushion with eyes closed for 60 s. In the eyes-open situations, patients were asked to stare at a target placed 1.50 m away from them. A 3-min rest interval was allowed between each test.
Statistical analysis
Data were analyzed using analysis of variance. Differences were considered at P<0.05.
Results
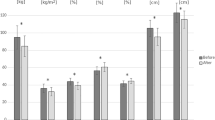
Figure 1 shows the mean values of anteroposterior and mediolateral displacements of the body for eyes both open and closed with regard to different types of seats. No significant differences were observed between the seats, both for anteroposterior and mediolateral displacements (P>0.05). Furthermore, no significant difference was observed between the seats with regard to eyes-open and eyes-closed situations (P>0.05).
However, paraplegic individuals have a more prominent body displacement in the anteroposterior sense than in the mediolateral sense (P<0.05).
Figure 2 shows mean values for body displacement velocities of anteroposterior and mediolateral positions with regard to different types of seats in both situations of eyes open and closed. There were no significant differences between seats in terms of displacement velocity (anteroposterior and mediolateral) and visual situation (eyes open and eyes closed) (P>0.05). Individuals with paraplegia had more prominent velocities for body displacements in a mediolateral sense than in an anteroposterior sense (P<0.05).
Discussion
The variety of seats allows the individuals to have options based on the one that provides the best comfort, prevents pressure ulcers and maintains optimal trunk balance.8
It is important to better understand whether the different types of seats have influence on trunk control, as manual activities depend on the stabilization and coordination between lumbar and thoracic spine.9, 10 Therefore, a seat that helps control posture in individuals with SCI sequelae can benefit them in their daily tasks.
According to Cholewicki et al.,11 reduction in static balance in the seated position is more likely to be observed in the sagittal plane (anteroposterior displacement) compared with the frontal plane (mediolateral displacement). The results from this study corroborate those found by Cholewicki et al.,11 who also observed greater anteroposterior displacement.
The protocol used in this study was aimed to assess the paraplegic individuals’ response to different levels of sensory loss, such as imprecise proprioceptive information with the use of foam and gel cushions, as well as the lack of vision by closing the eyes.
The results have shown that the presence of proprioceptive information provided by wheelchair seats or imprecise proprioceptive information generated by foam or gel cushions did not change the patients’ static balance, thus suggesting that SCI may impair the sending of sensory impulses to the central nervous system. Another explanation for the similar body displacement observed during the use of different types of seats is that foam and gel cushions did not create an imprecise sensorial feedback.
Unexpectedly, no difference in postural control was observed between the seats when static balance was compared regardless of whether the eyes were open or closed, thus suggesting that visual information did not help to control the trunk of paraplegic individuals studied. Therefore, it seems that the proprioceptive information from the neck and upper back may have interfered in postural adjustment during the static position. However, if the seating situations had created a sensorial conflict, it is also important to consider the possibility that individuals with paraplegia learnt to use the vestibular system to maintain adequate trunk control.
Because it is questionable whether the sensory conflicts were created by seating situations, additional studies must be conducted to evaluate the balance adjustments during visual and proprioceptive conflict conditions and during dynamic sitting.
Although the results obtained in this study showed that seats did not influence static balance in individuals with spinal cord injuries, the data showed a more anteroposterior body displacement than mediolateral. Moreover, the variety of seats provides options for individual comfort, relieving pressure points.
References
Minkel JL . Seating and mobility considerations for people with spinal cord injury. Phys Ther 2000; 20: 701–709.
Seelen HAM, Adam JJ, Drukker J, Spaans F, Huson A . Postural motor programming in paraplegic patients during rehabilitation. Ergonomics 1998; 41: 302–316.
Janssen-Potten YJ, Seelen HA, Drukker J, Huson T . The effect of seat tilting on pelvic position, balance control and compensatory postural muscle use in paraplegic subjects. Arch Phys Med Rehabil 2001; 82: 1393–1402.
Jassen-Potten YJ, Seelen HA, Drukker J, Spaans F, Drost M . The effect of footrests on sitting balance in paraplegic subjects. Arch Phys Med Rehabil 2002; 83: 642–648.
Sinnott KA, Milburn P, McNaughton H . Factors associated with thoracic spinal cord injury, lesion level and rotator cuff disorder. Spinal Cord 2000; 38: 748–753.
Koo TKK, Mak AFT, Lee YL . Posture effect on seating interface biomechanics: comparison between two seating cushions. Arch Phys Med Rehabil 1996; 77: 40–47.
Aissaoui R, Boucher C, Bourbonnais D, Lacoste M, Dansereau J . Effect of seat cushion on dynamic stability in sitting during a reaching task in wheelchair users with paraplegia. Arch Phys Med Rehabil 2001; 82: 274–281.
Gagnon D, Nadeau S, Noreau L, Eng JJ, Gravel D . Trunk and upper extremity kinematics during sitting pivot transfers performed by individuals with spinal cord injury. Clin Biomech 2008; 23: 279–290.
Aissaoui R, Boucher C, Bourbonnais D, Lacoste M, Dansereau J . Effect of seat cushion on dynamic stability in sitting during a reaching task in wheelchair users with paraplegia. Arch Phys Med Rehabil 2001; 82: 274–281.
Hastings JD, Fanucchi ER, Burns SP . Wheelchair configuration and postural alignment in persons with spinal cord injury. Arch Phys Med Rehabil 2003; 84: 528.
Cholewicki J, Polzhofer GK, Radebold A . Postural control of trunk during unstable sitting. J Biomech 2000; 33: 1733–1737.
Acknowledgements
The authors thank FAPESP (2007/54596-0) for the support provided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Takara, K., Gaspar, M., Metring, N. et al. Evaluation of the influence of different types of seats on postural control in individuals with paraplegia. Spinal Cord 48, 825–827 (2010). https://doi.org/10.1038/sc.2010.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.30