Abstract
Study design:
This was an observational, descriptive case-series study. The magnitude and direction of diaphragm movement during tidal and maximal inspiratory breaths in tetraplegic subjects were measured using B-mode sonography on a single occasion. Data were tabulated for descriptive analysis.
Objective:
There is a paucity of literature reporting dynamic movements of the paralyzed diaphragm. The aim of this pilot study was to investigate and record diaphragm movement in subjects with a cervical spinal cord injury (C1–C5), which had resulted in tetraplegia with partial or complete diaphragm paralysis. Subjects were patients of the Royal Adelaide Hospital in South Australia.
Results:
Three subjects participated in the study. The magnitude of diaphragm movement was small in two subjects and approached normal in one subject. During tidal inspiratory and maximal inspiratory breaths, the diaphragm moved in a caudal direction in two subjects. In the other subject, the diaphragm moved in a cephalad direction during a maximal inspiratory breath.
Conclusion:
Imaging of diaphragm movement was well tolerated by three subjects with cervical spinal cord injury. The difference in magnitude of diaphragm movement was not fully explained by the level of injury and the American Spinal Injury Association classification.
Similar content being viewed by others
Introduction
Cervical spinal cord injury is a common cause of chronic ventilatory failure and the degree of diaphragm paralysis is an important determinant of long-term respiratory support. We found only one study, which had measured the magnitude and direction of cephalocaudal diaphragm movement in subjects with diaphragm paralysis.1 Ultrasound is a well tolerated and reliable instrument for measuring diaphragm movement.2 The aim of our study was to use ultrasound to measure diaphragm movement in a group of subjects with C1–C5 cervical spinal cord injury.
Materials and methods
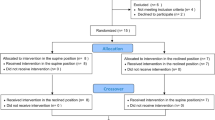
Subject recruitment was undertaken by the Medical Director at Hampstead Rehabilitation Centre in Adelaide. Subjects were included if they were over 18 years of age, had a spinal cord injury between C1 and C5 with an American Spinal Injury Association (ASIA) A, B or C classification and could spontaneously ventilate for 10 min. Subjects were excluded if they had any other past medical history, which could have affected their diaphragm function.
A Siemens Sonoline Antares ultrasound system (Siemens Sonoline Antares, Issaquah, WA, USA) was used to measure diaphragm movement. This system is reported to be accurate to within 0.5 mm on the basis of measurements against a phantom distance marker. Patients were positioned as upright as possible in their wheelchair or in bed. The 3.5-MHz abdominal probe was placed below the right subcostal margin between the mid-axillary and mid-clavicular line following the method described by the earlier authors.2, 3, 4
After five tidal breaths the sonographer froze the screen at the end of passive expiration and the leading edge of the diaphragm was marked on the screen using a single electronic marker. This was considered to be the position of the diaphragm at functional residual capacity. The position of the diaphragm at the end of inspiration was then marked electronically and the distance between markers was measured using inbuilt electronic calipers. The direction of the diaphragm movement from functional residual capacity was recorded for each breath. Three measurements were taken for tidal inspiration and three for maximal inspiration. Data were tabulated for descriptive analysis. The reliability of this test protocol was established (r2=0.85) using ten healthy subjects in a test retest study, which found no significant difference between average measures of diaphragm movement across the two testing days (P=0.457) or within the two test days (P=0.834) (Table 2).
We certify that all applicable institution and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Three male subjects were tested (Table 1). Subjects 1 and 3 had reduced diaphragm movement for tidal breaths (Table 1) compared with values for normal subjects (Table 2). The magnitude of movement for maximal breaths was also reduced in these two subjects compared with earlier reported values for healthy adults in the upright sitting position (53±16 mm4).
Discussion
The diaphragm moved in a caudal direction during all inspiratory breaths except during a maximal inspiratory breath in Subject 3.
Subject 1 (ASIA A C4/5)
The caudal direction of movement may have been because of residual innervation of the diaphragm. The small magnitude of movement may have been because of the partial paralysis of the diaphragm along with the relative recency of injury and therefore more compliant rib cage.
Subject 2 (ASIA C C3/4)
This subject had an incomplete spinal cord injury; therefore, the diaphragm was likely to be receiving innervation from the phrenic nucleus. The high magnitude of caudal movement suggests that the diaphragm was compensating for the dennervation of other respiratory muscles, whereas the chronicity of injury, with a stiffer rib cage, may have increased the piston effect of the diaphragm.
Subject 3 (ASIA A C2/3)
Subject 3 could only to be positioned at a 20-degree incline in bed on the day of testing. This position may have caused some lengthening of the diaphragm assisting diaphragm action.5 There was caudal displacement of the diaphragm during tidal breaths, which may have been because of some residual innervation and there was paradoxical (cephalad) diaphragm movement during maximal breaths. This was considered to be because of the generation of sufficient negative intra-thoracic pressure by the remaining accessory muscles during maximal breaths to overcome the minimally active diaphragm. The small magnitude of the cephalad movement was likely to be because of the chronically altered length of the diaphragm.
Conclusion
In this study of three tetraplegic subjects, imaging of diaphragm movement using B-mode ultrasound was well tolerated and able to measure both direction and magnitude of diaphragm movement during tidal and maximal inspiratory breaths. The difference in magnitude of diaphragm movement was not fully explained by the level of injury and ASIA classification and may have been because of some residual innervation of the diaphragm, time since injury, or subject position.
References
Froese A, Bryan C . Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 1974; 41: 242–255.
Blaney F, Sawyer T . Sonographic measurement of diaphragmatic motion after upper abdominal surgery: a comparison of three breathing manoeuvres. Physiother Theory Pract 1997; 13: 207–215.
Fedullo A, Lerner R, Gibson J, Shayne D . Sonographic measurement of diaphragmatic motion after coronary artery bypass surgery. Chest 1992; 102: 1683–1686.
Houston J, Morris A, Howie C, Reid J, McMillan N . Technical report: quantitative assessment of diaphragmatic movement—A reproducible method using ultrasound. Clin Radiol 1992; 46: 405–407.
Winslow C, Rozovsky J . Effect of spinal cord injury on the respiratory system. Am J Phys Med Rehabil 2003; 82: 803–814.
Acknowledgements
We would like to thank Dr Ruth Marshall, Medical Director of Hampstead Rehabilitation Centre for her assistance with subject recruitment for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hardy, F., Walker, J. & Sawyer, T. Sonographic measurement of diaphragm movement in patients with tetraplegia. Spinal Cord 47, 832–834 (2009). https://doi.org/10.1038/sc.2009.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.45
Keywords
This article is cited by
-
Evaluation of diaphragm thickening by diaphragm ultrasonography: a reproducibility and a repeatability study
Journal of Ultrasound (2021)
-
Diaphragm ultrasonography and pulmonary function tests in patients with spinal cord injury
Spinal Cord (2019)
-
Application of Ultrasound Image Tracking Algorithm for Real-Time Diaphragmatic Excursion Measurement
Journal of Medical and Biological Engineering (2018)
-
Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications
Intensive Care Medicine (2013)