Abstract
Study design:
Prospective, observational study.
Objectives:
To determine the proportion of patients with non-traumatic spinal cord injury (NTSCI) who regain the ability to walk and to describe walking outcomes with reference to three commonly used clinical measures of walking capacity.
Setting:
Spinal Rehabilitation Unit specializing in NTSCI, Melbourne, Australia.
Methods:
Demographic, clinical and mobility data collected from a consecutive cohort of patients admitted to the spinal rehabilitation unit between March 2006 and December 2007. Main outcome measures were the Timed Up And Go (TUG), the 10-m walk test (10 mWT) and the 6-min walk test (6MWT). Logistic regression analysis was conducted to explore predictors of walking ability after NTSCI.
Results:
Of 62 patients, 30 (48%) regained some capacity to walk during inpatient rehabilitation. Initial ASIA grade was the strongest predictor of walking. Twenty-seven patients regained the ability to perform functional tests (TUG, 10 mWT and 6MWT) of walking at ∼2 months after injury. Their performance at discharge remained low compared with normal scores but were similar to those measured in some studies of subjects with traumatic spinal cord injury (TSCI).
Conclusion:
Three simple clinical tests of walking suggest that half of all NTSCI patients are able to walk at discharge from inpatient rehabilitation. Their gait speed, however, remained impaired and not compatible with safe and efficient community walking.
Similar content being viewed by others
Introduction
Recovery of walking is a patient priority after spinal cord injury (SCI).1 Walking ability during rehabilitation determines patient goals and affects costly equipment required for discharge, such as wheelchairs and home modifications.2, 3 A number of studies have investigated walking outcomes after traumatic SCI (TSCI)2, 3, 4, 5, 6, 7, 8, 9 but have either excluded or not described the walking outcomes of patients with non-traumatic spinal cord injury (NTSCI). One study in NTSCI patients reported that 58% regained the ability to walk 10 m or better at discharge from inpatient rehabilitation.10 To date, however, more detailed information regarding functional walking ability has not been available in this population.
Studies of NTSCI patient outcomes are important because the incidence of NTSCI is reported to be greater than that of TSCI, and it is predicted to increase further as the population ages.11 There may also be differences in walking outcomes in this patient group compared with those with TSCI. Individuals with NTSCI are, on average, older, have more comorbidities, are more likely to have an incomplete SCI and are more likely to be paraplegic, when compared with those with a TSCI.10, 12, 13 These factors may all affect ambulatory outcomes.
The primary aims of this study were to determine the proportion of patients with NTSCI who regain some capacity to walk and to describe their walking outcomes with reference to three commonly used clinical measures of walking ability: the Timed Up And Go (TUG),14 the 10-m walk test (10 mWT)15 and the 6-min walk test (6MWT).16 The secondary aims were to explore the predictors of walking, the time frames for the achievement of functional walking and compare the walking outcomes with normal age-adjusted values.
Methods
Data were collected prospectively from consecutive inpatients admitted to the SCI rehabilitation unit at Caulfield Hospital between March 2006 and December 2007. This unit in Melbourne, Australia, is a 10-bed sub-acute inpatient rehabilitation unit located within a public hospital that is funded by the state government. The unit provides specialist interdisciplinary rehabilitation for patients with SCI, but predominantly to adults with NTSCI. Patients are usually residents of metropolitan Melbourne, but patients who live elsewhere in the State of Victoria are also accepted.
Patients are referred from either public or private hospitals after acute medical or surgical treatments of their NTSCI. Patients are admitted into the unit when they are medically stable enough to be managed in the sub-acute ward. Admission decisions are based on the perceived ability of patients to benefit from and participate in the programme. Discharge decisions are made with the involvement of the patient and family. No third-party payment source has influence over LOS (length of stay) or discharge destination. The team aims for the shortest LOS that will allow patients to be discharged to an appropriate, safe environment, with necessary equipment and modifications for safe functioning. The unit aims to achieve controlled faecal continence, optimal bladder management and necessary patient and carer education as part of the discharge process.
Patients were included if they were undergoing their first admission for rehabilitation after the onset of NTSCI. NTSCI was defined as the onset of paralysis secondary to any conditions causing damage to the spinal cord, including the cauda equina, not because of trauma. Typically, this included diagnoses such as tumours (primary and secondary); infections such as epidural abscesses; vascular events such as spinal cord ischaemia or haemorrhage; degeneration of the spinal column causing canal stenosis or osteoporosis-related fractures; and inflammatory conditions such as transverse myelitis. All patients consecutively admitted to the unit during the study period were considered for the study; however, patients who sustained a TSCI or who had a pre-existing SCI were excluded. The demographic and clinical details were recorded for each subject. These included: age, gender, cause of NTSCI, neurological level, admission ASIA score and date of onset of SCI. Patients were considered ‘walkers’ if, at any time during their admission, they were able to take consecutive steps with minimal assistance of one physiotherapist in a set of parallel bars 5 m long. Any patient requiring more than minimal assistance of one physiotherapist to walk (in or out of parallel bars) was defined as a ‘non-walker’. Minimal assistance was defined as the patient requiring physical assistance, where the physiotherapist was providing no more than 25% of the effort.
The TUG, 10 mWT and 6MWT were undertaken in all patients who were able to do so on the basis of protocols described previously.14, 15, 16 The TUG measurements included the time taken to complete the test and the seat height. The 10 mWT measurements included the time taken to complete the test and the number of steps taken. A digital stopwatch was used to time the subjects as they walked in a straight line between two markers 10 m apart within a 14 m course. Subjects began walking at a point 2 m before crossing the first marker and continued walking for 2 m beyond the second marker. For both the TUG and 10 mWT, patients were instructed to walk at a comfortable and safe speed.
The 6MWT measurements included the distance the subject could complete in 6 min and the number of rests during testing. Patient instructions were based on the American Thoracic Society Statement (2002).16 The 6MWT course consisted of a long internal hallway with ‘start’ and ‘turn’ markers 60 m apart. Subjects could rest during the test by either leaning against the wall or sitting down. Timing commenced once the subject began walking from the ‘start’ marker until the end of the 6-min time period.
Initial testing took place as soon as a patient was considered physically capable of completing the test. Patients were deemed able to perform these tests when they required no physical assistance throughout the testing procedures; however, close supervision from a physiotherapist may have been required for safety reasons. The tests were repeated within 72 hours before discharge from rehabilitation. All tests were conducted by physiotherapists according to standardised testing procedures. Tests were conducted with patients in comfortable appropriate footwear. The gait aid used for each test was noted, as were any orthoses the patients may have needed.
Length of stay in rehabilitation and discharge destination were recorded. LOS was defined as the total number of days the subjects spent in rehabilitation excluding any days spent at an acute hospital because of readmission for medical complications.
Data were analysed using SPSS version 14.0 (SPSS Inc.; Chicago, IL, USA). Differences in baseline demographic characteristics between walkers and non-walkers were examined using the χ2-test for categorical variables and the Mann–Whitney test for continuous variables. Logistic regression analysis was conducted to explore predictors of walking ability after NTSCI. It was determined a priori that independent variables with P⩽0.1 on univariate analysis were included in the model. The Hosmer and Lemeshow test was used to evaluate the model fit.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Seventy patients were admitted and completed their rehabilitation during the study period. Eight patients had SCI of traumatic cause and were excluded from the study. The remaining 62 patients met the inclusion criteria. Of these patients, 29 (47%) were male. The median age (interquartile (IQR) range) of the group was 67 (55–78) years. Demographic characteristics of the study sample are presented in Table 1. The most common causes of NTSCI were tumours and degenerative conditions, accounting for over 65% of cases. A thoracic level of SCI was present in over half of the cases and only 15% of subjects were tetraplegic. On admission, the majority of patients were classified as either ASIA C or ASIA D. The median LOS in rehabilitation was 52 days (IQR 35–91). There was a median of 35 days from the onset of the patients' NTSCI to admission to the rehabilitation unit (IQR 22–63 days).
During their inpatient admission, 30 (48%) patients regained some capacity to walk. There was no significant influence of the following on the likelihood of regaining walking ability: age (P=0.47), gender (P=0.12), length of inpatient stay (P=0.48) or the number of days from injury to rehabilitation (P=0.24).
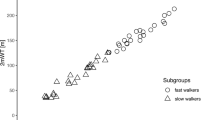
The relationship between baseline demographic characteristics and walking ability is seen in Table 1 and Figures 1 and 2. Patients with a degenerative cause of their SCI were more likely to walk than those with other causes (P=0.04, Table 1). Patients with ASIA D grade on admission were more likely to walk (P<0.001), with 15 out of 16 patients in this category achieving ambulation (Figure 1). Those with a lumbar spine level injury were more likely to walk than those with thoracic or cervical injuries (P=0.02, Figure 2). In a logistic regression model that included the cause of NTSCI, the admission ASIA grade and the level of injury, only the admission ASIA grade was a significant predictor of walking (Table 2). Patients classified as ASIA C had a 92% reduction in the odds of walking compared with those classified as ASIA D. Patients classified as ASIA B had a 97% reduction in the odds of walking compared with those classified as ASIA C. This model explained 58% of the variance in walking ability. The Hosmer and Lemeshow test indicated good model fit (χ2=4.69, P=0.79).
Of the 30 patients who regained some capacity to walk, 27 (90%) were able to perform the TUG and the 10 mWT. The three subjects unable to perform these tests were able to walk between parallel bars but required more than minimal assistance from a physiotherapist to take steps and maintain balance. Those who could perform the TUG did so at a median of 18 days after admission to rehabilitation (IQR 4–71), and at a median of 67 days (IQR 35–126) from their injury. There was a significant improvement in the TUG scores from admission to discharge (P<0.001, Table 3). The discharge results, however, still remained significantly reduced compared with the values seen in community-dwelling elderly.14
The 27 patients able to perform the 10 mWT did so at a median of 20 days (IQR 4–62) into their inpatient rehabilitation stay and 68 days (IQR 34–123) from the onset of their SCI. There was a significant improvement in this test of gait speed over the course of the admission (P<0.001, Table 3) as well as a significant reduction in the mean number of steps taken (37–27, P<0.001). Walking speed at discharge averaged 0.33 m s−1. This was considerably below the 1.29–1.35 m s−1 reported in healthy adults aged in their sixties.17
Only 20 patients were able to perform the 6MWT. They were able to perform this test at a median of 13 days (IQR 6–53) into their rehabilitation stay, and at a median of 57 days (IQR 28–132) after injury. The 6MWT distance increased significantly over the course of admission (P<0.001, Table 3); however, the walking distance at discharge remained well below that of normals.18
On the initial tests, the most commonly used gait aids were gutter-frames, two wheel-frames, pick-up (Zimmer) frames or walking sticks. At discharge, more patients were using four-wheel-frames (37%), forearm crutches (15%) or no gait aid (15%) to ambulate, whereas 7% used walking sticks, 22% were using two wheel-frames and one patient walked with a pick-up frame. Six subjects required one ankle-foot orthosis at initial testing and five of these same patients required an ankle-foot orthosis at discharge. No patient used a reciprocal gait orthosis or a knee-ankle-foot orthosis to perform the tests.
Those patients who were able to walk during inpatient rehabilitation were more likely to be discharged home. Seventy-seven percent of walkers were discharged home, compared with 52% of non-walkers (P=0.04). The remaining discharge destinations were low-level care (7% walkers and 0 non-walkers), high-level care (7% walkers and 19% non-walkers), other rehabilitation facilities (7% walkers and 3% non-walkers), acute hospitals (3% walkers and 22% non-walkers) and other (0 walkers and 3% non-walkers).
Discussion
To our knowledge, this is the first study to quantify, using three common clinical tests, the walking capacity of NTSCI patients at discharge from inpatient rehabilitation. We have described time frames for the commencement of walking and shown that although half the patients regain some ability to walk, their functional performance remained well below normal age-adjusted values.17, 18
Our study is also the first that we know of to report the time frames in which patients with NTSCI can perform functional measures of walking. Our results suggest that patients who were able to perform these tests did so at a median of ∼2 months after injury. This information may prove especially relevant for the multidisciplinary team faced with the challenge of predicting functional outcomes and time frames for patient goals during inpatient rehabilitation.19
Prediction of walking capacity is an important issue during rehabilitation after SCI.2 Initial ASIA grade has been reported elsewhere as a major predictor of gait in SCI patients.20, 21 Our study supports this with 58% of the variance in walking outcome being explained by a logistic regression model that included initial ASIA grade. The level of injury in our study was also related to walking, which is supported by other authors.20
The demographic characteristics of our sample are similar to those of an earlier cohort from our centre10 and other publications detailing the demographic characteristics of NTSCI patients.22, 23 This increases the generalisability of our findings.
Comparison to traumatic SCI
Compared with one study in TSCI, a greater proportion of our NTSCI patients with initial ASIA B, C or D grades regained some capacity to walk at discharge from rehabilitation. It has been reported that 0.9% of TSCI subjects with an ASIA A or B initial grade of SCI walked at rehabilitation discharge, whereas 28.3% of ASIA C and 47.2% of ASIA D diagnosed subjects regained some capacity to walk.2 This compares with 18% (ASIA B), 48% (ASIA C) and 94% (ASIA D) in our NTSCI patients. In contrast to this study and our results, a recent multicentre randomised trial, investigating the effects of overground training versus body-weight supported treadmill training (in addition to routine physical therapy) after TSCI, reported that 92% of ASIA C and 100% of ASIA D patients achieved minimal assisted ambulation at ∼16 weeks after SCI.9 It is possible that the additional physical intervention in this trial accounted for the improved result in patients with ASIA C and D grades of SCI.
An age of greater than 50 years has been reported to have a negative effect on the likelihood of walking in TSCI,2 and one study22 that included both TSCI and NTSCI patients also found that age affects the independence and performance of gait. However, an earlier study in NTSCI found that age had no effect on walking outcomes,24 and this study supports this finding. Although these findings should be confirmed in a larger cohort, currently available data also suggest that the provision of rehabilitation should not be influenced by age at the onset of NTSCI.
Our patients' walking outcomes at discharge were similar to those reported in two studies predominantly involving traumatic SCI populations.6, 25 However, these studies included subjects who were at least 1 year after injury. Few studies have examined walking outcomes after early rehabilitation. Our patients' results are lower compared with one study of mostly TSCI subjects in which their 10 mWT and 6MWT results at 12 weeks after injury were 8 s and 473 m, respectively.26 Similarly, in a large multicentre study,9 10 mWT speeds reported in subjects with ASIA C and D at ∼3 months after TSCI (∼11 s or 0.85 m s−1) exceeded our patients' mean score at discharge. The inclusion of two ASIA B patients in our results may explain the lower mean scores in our study. Interestingly, this same study9 reported 6MWT scores of 250 m, which is comparable to our NTSCI group's mean result (220 m). Further research is required to clarify these differences and the long-term walking outcomes after NTSCI.
Comparison to normals
Although there were significant improvements during inpatient rehabilitation in the TUG, 10 mWT and 6MWT scores in our patients, the functional performance at discharge remained poor compared with normal age-adjusted scores. The average TUG at discharge (33.25 s) of our subjects is more than twice as slow as that reported in community-dwelling older people.27 Gait speed at discharge from inpatient rehabilitation was one-fifth to one-quarter of normal scores.17 Given that the safe negotiation of pedestrian crossings has been calculated at a walking speed of 1.22 m s−1,28 the patients in our study, on average, would be unlikely to safely negotiate community environments. The 6MWT at discharge (mean 220 m) was less than a third of that reported in normal subjects aged 55–75 years,18 and thus reduced endurance could also be a significant barrier to practical community ambulation after NTSCI. Taken together, these results suggest that the rehabilitation team should use caution in describing NTSCI patients as ‘community walkers’ after rehabilitation, and access to manual and power wheelchairs may remain a priority for aiding community access for these patients. These results also suggest that NTSCI patients may require access to ongoing outpatient therapy services to address goals of improving gait speed and endurance related to community mobility.
Utility of the TUG, 10 mWT and 6MWT
These tests of walking capacity have good test-retest and interobserver reliability29 and have established concurrent validity in a traumatic and ischaemic SCI population.25 The 10 mWT and 6MWT also have good construct validity and responsiveness when used in SCI populations. They are clinically simple to conduct and require minimal equipment.15, 30 The tests could be performed in 27 out of 30 of our walking patients, suggesting that they are also highly feasible to conduct in an NTSCI population.
It has been argued that the 6MWT and 10 mWT provide similar information about walking speed after SCI.31 However, we found that only 20 of the 27 patients able to perform the 10 mWT were also assessed using the 6MWT. In seven patients, physiotherapists did not undertake the 6MWT as they deemed it was not safe for these patients with very limited mobility, a finding that suggests that these tests do not measure identical constructs. The 6MWT may better reflect sensorimotor deficits rather than cardiovascular limitations after SCI,30 and the ability to perform this test may provide additional information that is not available from the 10MWT.
Limitations
The sample was drawn from one Australian centre and may not be representative of NTSCI in other centres and countries. Patients' gait aids were not controlled, so initial and discharge measures were taken with patients using different gait aids (for example, two wheel frame vs four wheel frame). This difference, however, reflects a clinically relevant progression and the pragmatic approach taken during this study. Although the sample size is relatively small, which may affect generalisability, the demographic and clinical characteristics compare favourably with other studies in NTSCI10, 12, 13, 23 and include patients with a similar range of aetiologies and severity. It is possible that the small sample size may have affected our ability to identify predictors of walking after NTSCI. This aspect of our study was exploratory and should be confirmed in larger samples.
Implications and further research
Although this study provides new information about walking outcomes at discharge from rehabilitation, little is known regarding the longer-term functional mobility outcomes in the NTSCI group. Given that these patients tend to be significantly older than those with a traumatic injury and have comorbidities that could affect function, it is possible these individuals continue to face significant mobility challenges over time. Further research in this area is required.
Although we have shown that the initial ASIA grade of SCI is related to walking after NTSCI, a notable amount of the variation in walking ability remains unexplained. Larger studies are required to explore other factors that may influence walking outcomes such as body anthropometry, comorbidities and patterns of recovery in muscle strength. In addition, given the relatively poor ambulation outcomes of NTSCI patients at rehabilitation discharge compared with community-living age-matched norms, research exploring the potential benefits of treatments such as functional electrical stimulation and partial body-weight-supported treadmill training on gait outcomes is warranted.
In summary, nearly half of our NTSCI patients could perform functional tests of walking at ∼2 months after injury. The results of these tests improved significantly throughout inpatient rehabilitation. Despite this improvement, the discharge outcomes for gait speed remained impaired and not compatible with safe and practical community walking. This information may inform inpatient rehabilitation teams in planning the care, equipment needs and ongoing support for this under-represented but significant subgroup of SCI individuals.
References
Ditunno PL, Patrick M, Stineman M, Ditunno JF . Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord 2008; 46: 500–506.
Kay ED, Deutsch A, Wuermser LA . Predicting walking at discharge from inpatient rehabilitation after a traumatic spinal cord injury. Arch Phys Med Rehabil 2007; 88: 745–750.
Waters RL, Yakura JS, Adkins R, Barnes G . Determinants of gait performance following spinal cord injury. Arch Phys Med Rehabil 1989; 70: 811–818.
Waters RL, Adkins R, Yakura J, Vigil D . Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994; 75: 756–760.
Wirz M, van Hedel HJ, Rupp R, Curt A, Dietz V . Muscle force and gait performance: relationships after spinal cord injury. Arch Phys Med Rehabil 2006; 87: 1218–1222.
Kim CM, Eng JJ, Whittaker MW . Level walking and ambulatory capacity in persons with incomplete spinal cord injury: relationship with muscle strength. Spinal Cord 2004; 42: 156–162.
Krawetz P, Nance P . Gait analysis of spinal cord injured subjects: effects of injury level and spasticity. Arch Phys Med Rehabil 1996; 77: 635–638.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006; 66: 484–493.
Dobkin B, Barbeau H, Deforge D, Ditunno J, Elashoff R, Apple D et al. The evolution of walking-related outcomes over the first 12 weeks of rehabilitation for incomplete traumatic spinal cord injury: the multicenter randomized spinal cord injury locomotor trial. Neurorehabil Neural Repair 2007; 21: 25–35.
New PW . Functional outcomes and disability after nontraumatic spinal cord injury rehabilitation: results from a retrospective study. Arch Phys Med Rehabil 2005; 86: 250–261.
New PW, Sundararajan V . Incidence of non-traumatic spinal cord injury in Victoria, Australia: a population-based study and literature review. Spinal Cord 2008; 46: 406.
Citterio A, Franceschini M, Spizzichino L, Reggio A, Rossi B, Stampacchia G . Nontraumatic spinal cord injury: an Italian survey. Arch Phys Med Rehabil 2004; 85: 1483–1487.
Ones K, Yilmaz E, Beydogan A, Gultekin O, Caglar N . Comparison of functional results in non-traumatic and traumatic spinal cord injury. Disabil Rehabil 2007; 29: 1185–1191.
Podsiadlo D, Richardson S . The timed ‘up and go’: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–148.
Hill K, Denisenko S, Miller K, Clements T, Batchelor F . Clinical Outcome Measurement in Adult Neurological Physiotherapy, 3rd edn. Australian Physiotherapy Association: Melbourne, Victoria, Australia, 2005.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. American Thoracic Society statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111–117.
Bohannon RW . Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing 1997; 26: 15–19.
Camarri B, Eastwood PR, Cecins NM, Thompson PJ, Jenkins S . Six minute walk distance in healthy subjects aged 55–75 years. Respir Med 2006; 100: 658–665.
Schonherr MC, Groothoff JW, Mulder GA, Eisma WH . Prediction of functional outcome after spinal cord injury: a task for the rehabilitation team and the patient. Spinal Cord 2000; 38: 185–191.
Barbeau H, Nadeau S, Garneau C . Physical determinants, emerging concepts, and training approaches in gait of individuals with spinal cord injury. J Neurotrauma 2006; 23: 571–585.
Curt A, Dietz V . Ambulatory capacity in spinal cord injury: significance of somatosensory evoked potentials and ASIA protocol in predicting outcome. Arch Phys Med Rehabil 1997; 78: 39–43.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M . Effects on age on spinal cord lesion patients' rehabilitation. Spinal Cord 2003; 41: 457–464.
McKinley WO, Seel RT, Gadi RK, Tewksbury MA . Nontraumatic vs traumatic spinal cord injury: a rehabilitation outcome comparison. Am J Phys Med Rehabil 2001; 80: 693–702.
New PW . Influence of age and gender on rehabilitation outcomes in nontraumatic spinal cord injury. J Spinal Cord Med 2007; 30: 225–237.
van Hedel HJ, Wirz M, Dietz V . Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil 2005; 86: 190–196.
van Hedel HJA, Wirz M, Curt A . Improving walking assessment in subjects with an incomplete spinal cord injury: responsiveness. Spinal Cord 2006; 44: 352–356.
Steffen TM, Hacker TA, Mollinger L . Age- and gender-related test performance in community-dwelling elderly people: six-minute walk test, Berg balance scale, timed up & go test, and gait speeds. Phys Ther 2002; 82: 128–137.
Hoxie RE, Rubenstein LZ . Are older pedestrians allowed enough time to cross intersections safely? J Am Geriatr Soc 1994; 42: 241–244.
Lam T, Noonan VK, Eng JJ . A systematic review of functional ambulation outcome measures in spinal cord injury. Spinal Cord 2008; 46: 246–254.
van Hedel HJA, Wirz M, Dietz V . Standardized assessment of walking capacity after spinal cord injury: the European network approach. Neurol Res 2008; 30: 61–73.
van Hedel HJA, Dietz V, Curt A . Assessment of walking speed and distance in subjects with an incomplete spinal cord injury. Neurorehabil Neural Repair 2007; 21: 295–301.
Acknowledgements
We acknowledge the Physiotherapy staff at Caulfield Hospital, Alfred Health, Melbourne, Australia for their contribution to this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sturt, R., Holland, A. & New, P. Walking ability at discharge from inpatient rehabilitation in a cohort of non-traumatic spinal cord injury patients. Spinal Cord 47, 763–768 (2009). https://doi.org/10.1038/sc.2009.36
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.36
Keywords
This article is cited by
-
Validation of a clinical prediction rule for ambulation outcome after non-traumatic spinal cord injury
Spinal Cord (2020)
-
Instrumenting gait assessment using the Kinect in people living with stroke: reliability and association with balance tests
Journal of NeuroEngineering and Rehabilitation (2015)
-
Validity and reliability of the 10-m walk test and the 6-min walk test in spinal cord injury patients
Spinal Cord (2011)