Abstract
Objectives:
We have shown previously that administration of quercetin after spinal cord injury in a rat model induced significant recovery of motor function. In the same model for spinal cord compression injury, we now have correlated the treatment duration with the extent to which motor function is recovered.
Methods:
Seventy-four male Wistar rats were assigned to eight experimental groups. Mid-thoracic spinal cord injury was produced in the animals of seven groups. Quercetin was administered intraperitoneally in individual doses of 25 μmol kg−1. Treatment onset was 1 h after the injury. The length of treatment ranged from one single injection to 10 days, with injection frequencies of two or three times daily. BBB (Basso, Beattie and Bresnahan) scores were obtained and tissue preservation at the site of injury was analyzed.
Results:
None of the untreated control animals recovered motor function sufficient to walk. When quercetin was administered twice daily over a period of either 3 or 10 days, about 50% of the animals recovered sufficient motor function to walk. Stepping/walking (BBB ⩾10) were seen in two of six animals receiving only a single injection and in one of the six animal receiving three injections. Surprisingly, none of the animals that received quercetin injections three times daily recovered the ability to walk (all BBB ⩽9).
Conclusion:
Quercetin administration results in preservation of tissue bridges at the site of injury. Treatment success depends on frequency of administration and overall dose.
Similar content being viewed by others
Introduction
As shown previously in two animal models of central nervous system trauma, the administration of quercetin can be beneficial for the prevention of secondary injury after spinal cord trauma.1, 2 The term secondary injury is used to distinguish the tissue damage caused by the primary injury, describing the original mechanical impact, from the damage caused by subsequent changes in the extracellular milieu. Secondary injury is caused by a complex of pathological processes, which include oxidative stress inflammatory processes, edema, ischemia, apoptosis and tissue necrosis.3, 4, 5, 6, 7, 8 Scar tissue formation, a major obstacle to functional recovery after central nervous system trauma is believed to be, at least partially, driven by oxidative stress and inflammatory processes. Within the first few days after a trauma, activated neutrophils and macrophages invade the traumatized tissue in which they release a multitude of oxidant species and hydrolases into the extracellular space. These oxidizing species and hydrolases react with healthy tissue structures, thereby increasing the volume of tissue injury.9, 10 Thus, a compound acting as anti-oxidative and anti-inflammatory, such as quercetin, should be considered a potentially useful therapeutic agent in the acute phase after central nervous system trauma.
We have previously demonstrated that twice daily administration of 25 μmol kg−1 quercetin supports significant recovery of motor function in the animal model of spinal cord compression injury when treatment was started 1 h after injury.1 We have now chosen to use the same model of spinal cord compression injury for another set of experiments because it closely simulates an injury mechanism and the extensive mechanical damage seen in human spinal cord injury. The model has been well established in our laboratory for several years. In this study, we correlate the duration and dosage of treatment with the degree of post-traumatic recovery of motor function.
Materials and methods
Our animals were housed and cared for in a temperature-regulated animal facility exposed to a 12-h light/dark cycle in accordance with the guidelines of the Canadian Council on Animal Care after the appropriate permission had been obtained from the Animal Ethics Committee at the University of Saskatchewan. A total of 71 adult male Wistar rats (9–10 weeks of age, 285–340 g; Charles River, Canada) were subjected to standardized mid-thoracic spinal cord compression injury at level T7 as described by Rivlin and Tator.11 Anesthesia was maintained with 2–2.5% halothane in oxygen at a flow rate of 1.5 l min−1. Animals were pre-medicated with a subcutaneous injection of 0.05 mg buprenorphine per kg and received tapered doses in 12-h intervals for 3 days of post-operative analgesia. A vertical midline incision was carried out over the spinous processes T5–T7 and a catheter (butterfly-23 with cut-off needle) was tunneled subcutaneously towards the abdomen and implanted intraperitoneally. It is our experience that these catheters significantly ease repeated intraperitoneal drug administration. Laminectomy was carried out at T6 and T7 levels, and the spinal cord was exposed without opening the dura mater. An aneurysm clip (Kerr–Lougheed clip, Walsh Manufacturing, Oakville, Ontario, Canada) with a calibrated closing force of 50 g was closed around the spinal cord for 5 s, which rendered all animals completely paraplegic. The muscles were re-approximated with absorbable suture and the skin was stapled. The injection adapter of the catheter was secured with tape and sutured to the skin.
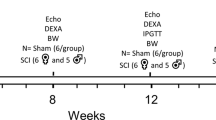
Animals in the treatment groups received weight-adjusted doses of 25 μmol quercetin per kg (quercetin dihydrate, Sigma, St Louis, MO, USA). This dose had been established as optimal for use in the acute phase after spinal cord trauma in our earlier studies.1 Animals in the control groups received normal saline, the vehicle used for quercetin suspension. Therapy onset was 1 h after spinal cord compression injury. Animals were assigned to eight experimental groups in two experimental cycles.
First experimental cycle
The first experimental cycle included six groups. Animals in Groups 1–4 (n=6 per group) received intraperitoneal injections of quercetin either as single injection (Group 1), three injections at 1, 12 and 23 h after the injury (Group 2) or at 12 h intervals for 72 h (Group 3) or for 10 days (Group 4). The animals in Group 5a (n=12) and Group 6 (n=3) served as controls. Animals in Group 5a received saline injections only. Animals in Group 6 underwent laminectomy, but no spinal cord injury was produced in order to determine whether our laminectomy technique alone caused impairment of motor function. Animals subjected to a spinal cord injury were assigned randomly to experimental groups 1–5. All animals were euthanized six weeks after injury by pericardiac perfusion under inhalation anesthesia with halothane.
Second experimental cycle
The experiments described for Groups 3 and 4 were repeated (n=6 per group) to validate the earlier results. Furthermore, we added two groups (Groups 7 and 8) in which the protocol was identical to that used in Groups 3 and 4 except that the frequency of quercetin administration was increased from twice to thrice daily (every 8 h). The objective was to test whether additional doses of quercetin would result in even better functional recovery. Another 11 animals were used as saline controls (Group 5b). Surgery for all experiments described in this report was carried out by the same researcher.
Seven animals of Group 4 and six saline controls (Group 5) were allowed to recover for a total of 12 weeks after injury to assess whether the improvement of motor function would extend beyond the 6 week recovery period in the animals receiving quercetin and whether there would be late spontaneous recovery in animals that received saline only. A summary of the experimental protocols is provided in Table 1.
For our assessment of functional recovery in the hind limbs, BBB (Basso, Beattie and Bresnahan) scores were used. With the BBB scoring system, motor function is rated from the aspects of both strength in and positioning of the hind limbs in an open field test.12 Points on a scale from 0 to 21 are awarded to describe motor function of the hind limbs, with 0 denoting no noticeable movement, whereas 21 describes a perfectly healthy, walking animal. It has been shown in a multi-center study that the inter-observer difference amounts to no more than two points.13 From a clinical aspect, the range of BBB scores can be divided into three fundamentally distinct groups, designating walking animals, animals that cannot walk but do support weight and those animals that can neither walk nor support weight. Statistical analysis of the mean BBB scores was carried out using the non-parametric Mann–Whitney test (t-test assuming non-Gaussian distribution of data).
Histological image analysis was conducted on animals from groups 4 (10 days of quercetin treatment, twice daily) and 5 (saline controls) sacrificed at 6 weeks after spinal cord injury. The animals were perfused with normal saline (to wash erythrocytes out of the tissue) followed by 10% phosphate-buffered formalin (for preservation), after which the spinal cords were dissected. A piece of spinal cord containing levels T6–T8, with the injured level T7 in the middle, was embedded in OCT (optimal cutting temperature) and frozen sections of 20 μm thickness were prepared. A total of 10 sections per animal were stained with Luxol Fast Blue (LFB)–cresyl violet stain to determine the damage to the myelin sheaths. Axial sections revealed that, at the site of injury, almost all gray matter had disintegrated and only a small rim of tissue was preserved. For our analysis, we choose sections that showed well myelinated tracts above and below the site of injury. Sections were scanned at 600 dpi and loaded into Image J. In each section, we outlined and measured the total areas lacking the LFB stain typical for intact myelin sheaths and the areas devoid of either LFB or cresyl violet staining nuclei and Nissl substance of the remaining tissue (holes). Finally, we divided the value for the area lacking LFB stain (but partially containing tissue stained with cresyl violet) by the area values for holes, resulting in the tissue bridge-to-tissue void ratio.
Results
None of the three animals that underwent laminectomy only (Group 6) showed any neurological impairment and they achieved BBB scores of 21 at every testing session. Means±s.d. values of the BBB scores in all treatment groups are presented in Figure 1, whereas Figure 2 illustrates the differences between the groups with a focus on weight bearing in stance and locomotion.
BBB (Basso, Beattie and Bresnahan) scores of all animals in groups 1–5 at 6 weeks after spinal cord compression injury (error bars show means±s.d. values). Although a trend towards improved motor function was seen in all quercetin-treated groups, the difference in mean BBB scores to those in the saline control group was statistically significant only in Group 5 (P<0.01; signified by the asterisk).
Overview of the percentage of animals in the experimental groups that recovered motor function sufficiently to support weight (BBB (Basso, Beattie and Bresnahan) 9) and to step/walk (BBB⩾10). This figure represents the same groups of animals as those in Figure 1, but with emphasis on weight support and locomotion rather than group means for BBB scores. None of the saline controls recovered motor function sufficiently to walk and only a very small percentage (4.8%) was able to support weight in stance. Functional recovery was better in virtually all of the quercetin-treated groups, even though none of the animals treated thrice daily recovered sufficiently to walk. Best recovery of motor function was seen in the groups that received quercetin for 3 days (58.3% walking) and 10 days (50% walking).
Of the 23 animals used as saline controls (Group 5), one animal had to be euthanized because of excessive self-inflicted abdominal wounds (excessive gnawing) and one animal died during week 2 from unexplained causes. The remaining 21 animals at 6 weeks achieved an average BBB score of 5.4 (±2.9 s.d.) with only one of the animals (4.75%) able to support weight in stance (BBB score of 9). No correlation between duration of saline injection and BBB scores was observed. Therefore, we will present all saline-treated animals as one single group. No significant spontaneous late recovery was seen in any of the animals that received saline only in the group with extended post-traumatic observation time of 12 weeks. Neither was any loss of function noted in the quercetin-treated animals with an extended observation period (Figure 3). Although there were no statistically significant differences between quercetin-treated and control animals at week 1 after injury (P=0.1584), the differences between the two groups were statistically significant from week 2 (P=0.0426) until the end of the observation period at 12 weeks after injury (P=0.0464). The most significant difference between the two groups was seen at 3 weeks after injury (P=0.015), followed by 4 weeks (P=0.0329) and 6 weeks (P=0.0367). It seems that there is still a subtle trend for recovery of function within both quercetin-treated animals and saline controls at 12 weeks after injury.
Recovery of motor function in the animals of group 4 (quercetin treatment for 10 days, twice daily; n=7) and group 5 (saline controls; n=6) that were observed for 12 weeks. The differences between the mean values for BBB (Basso, Beattie and Bresnahan) score of quercetin-treated animals and saline controls were statistically significant from week 2 until the end of the testing period. No significant changes in BBB score means, within the groups, were seen after week 4, although a subtle trend for further recovery of motor function was noted (error bars show means±s.d. values).
Animals that received one injection of quercetin, achieved a BBB score of 6.0±3.9. Of these 6 animals, two were stepping/walking at the end of the 6 weeks observation period (BBB scores of 10 and 11). Animals that received three injections (24 h of treatment) achieved a BBB score of 6.5±3.1. One animal out of these 6 achieved a BBB score of 10. BBB scores for animals in groups 1 and 2 are not statistically significantly different from those for the saline-treated controls.
Twelve animals that received 3 days of quercetin treatment every 12 h achieved a mean BBB score of 8.3±3.4. Although the BBB scores were not significantly different from those for the saline vehicle-treated animals, 7 of the 12 animals achieved a BBB score of 10 or better (up to a score of 12), whereas one animal could support weight in stance (BBB score of 9). Thus, from a clinical perspective, the difference in outcome between animals receiving 3 days of treatment and the saline controls (no animal walking or stepping) is very significant.
Twelve animals that received 10 days of quercetin treatment every 12 h achieved a BBB score of 10.0±2.8 which was significantly different (P<0.01) from the saline vehicle-treated animals. In this group, 6 of the 12 animals achieved a BBB score of 10 or greater (up to 14), whereas one animal could support weight in stance (BBB score of 9). BBB scores continually increased for the first 4 weeks and then reached a plateau.
Changing the treatment schedule to three instead of two daily injections did not improve the recovery of function. On the contrary, none of the animals injected three times daily was able to achieve a BBB score of 10 or higher at the end of the six-week recovery period. Animals treated thrice daily for a period of 3 days achieved a BBB score of 5.5±2.1, whereas animals treated for a period of 10 days achieved a BBB score of 8.2±1.2. None of the animals that were treated thrice daily for 3 days could bear weight in stance (BBB score of 9), whereas 3 of the 6 animals treated thrice daily for 10 days achieved a BBB score of 9. There were no differences in the mean BBB scores between these two groups and the saline vehicle-treated group. Recovery of motor function for the animals in the various treatment protocols has been summarized in Table 2.
At 6 weeks after the spinal cord injury, the measurements for areas lacking LFB stain (that is, destruction of myelin sheaths) were 0.436 cm2 (s.e.m.±0.023) for quercetin-treated animals and 0.346 cm2 (s.e.m.±0.042) for saline controls. The area measurements for holes (lack of either LFB or cresyl violet stain) were 0.077 cm2 (s.e.m.±0.012) for quercetin-treated animals and 0.117 cm2 (s.e.m.±0.0264) for saline controls. In other words, in spinal cords of quercetin-treated animals, more tissue bridges existed in areas that lacked intact myelin sheaths than in spinal cords of saline controls (Figure 4). This was reflected in higher tissue bridge-to-tissue void (hole) ratios in quercetin-treated animals. With ratios of 8.024 (s.e.m.±2.529) for quercetin-treated animals vs 3.528 (s.e.m.±0.8895) for saline controls, the difference between the two groups was almost, but not quite, statistically significant (P=0.0556). The difference between the two groups was not statistically significant for either the area size lacking intact myelin sheaths (P=0.1508) or the area size of the holes (P=0.2222).
Scans of longitudinal spinal cord sections, levels T6–T8, with compression injury at T7. Sections of 20 μm thickness were obtained at 6 weeks after injury and stained with LFB–Cresyl violet (Luxol fast blue–cresyl violet). The blue LFB stain is typical for intact myelin sheaths. Cresyl violet stains nuclei and Nissl substance of the remaining tissue bridges. Animals A and B were saline controls and achieved BBB (Basso, Beattie and Bresnahan) scores of 3 and 8, respectively. Animals C and D were treated with quercetin and reached BBB scores of 11 (after 3 days of treatment) and 12 (after 10 days of treatment). The tissue bridge-to-tissue void (hole) ratio was 1.62 for animal A, 3.24 for animal B, 5.1 for animal C and 6.0 for animal D.
Discussion
In our earlier experiments, 67% of initially paraplegic animals recovered sufficient hind limb function to walk, that is, they attained a BBB score of 10 or greater.1 For this series of experiments, an identical experimental protocol was used to create the spinal cord injury, except that the calibrated closing force of the aneurysm clip was now 50 g instead of 40 g. In only two of the treatment protocols we could achieve similar results: treatment twice daily with quercetin for 3 days enabled 58.3% of the animals to achieve BBB scores of 10 or greater with mean BBB score of 8.3, whereas twice daily treatment for 10 days allowed 50% of the animals to achieve BBB scores of 10 or greater with mean BBB scores of 10.0. In the latter group, 3 of the animals achieved a BBB score of 12, whereas two animals achieved a BBB score of 14. In the former group, only one of the animals could achieve a BBB score of 12 and none achieved a BBB score of 14. This suggests that the longer treatment has benefits over the shorter treatment as is indicated by the statistical analysis of the mean BBB scores. The fact that in this study a lower proportion of animals treated for 10 days achieved a BBB score of 10 or greater indicates, not surprisingly, that the efficacy of quercetin after acute traumatic spinal cord injury depends on the severity of the trauma. The fact that some of the animals achieved a BBB score of 10 or better with the shorter time periods (1 dose or 3 doses of quercetin) of treatment indicates that even brief exposure to quercetin has some neuroprotective effect. The fact that not all animals in a given treatment group respond uniformly to the treatment might be explained by a variety of factors. Although genetic differences between inbred animals, such as Wistar rats, are considerably lower than would be expected between human patients, they might be sufficient to cause variations in the degree by which these animals respond both to initial injury and to treatment. Furthermore, the combination of minor anatomical variations (that is, the angle at which a spinal root exits, making it more or less prone to injury caused by the clip application) and minor differences in size and position of the laminectomy may cause differences in the extent of the primary injury. It should be noted, however, that despite all these potential causes for differences in overall recovery, only a minor percentage of animals in the saline control group recovered sufficient motor function to support weight in stance and none of them was able to walk. Stepping and walking were seen only in quercetin-treated animals. The higher group average of tissue bridge-to-tissue void ratios at the site of injury in quercetin-treated animals reflects the structural preservation as a consequence of the treatment.
Curiously, treatment with quercetin thrice daily resulted in no animals achieving a BBB score greater than 9. At first glance, one might consider that this is a dose issue with quercetin concentrations in blood or/and tissue rising to levels that negate the protective effects. However, in our previous study, we administered quercetin doses up to 100 μmoles kg−1 every 12 h and found little difference in the outcome when compared with the administration of 25 μmoles kg−1.1 Using a dose of 100 μmoles kg−1 twice daily, one would anticipate that plasma quercetin levels would peak at higher levels than when a dose of 25 μmoles kg−1 was administered thrice daily. It is known that quercetin, in solution administered intravenously in the rat, has a biphasic plasma clearance with a rapid drop in concentration followed by a slower drop with a half-life of 111 min with an intrinsic mean residence time within peripheral tissues of just over 3 h.14 In our investigations, quercetin is administered intraperitoneally in the form of a suspension in saline. The work of Khaled and colleagues14 has demonstrated that quercetin administered as a suspension takes 50% longer time to enter plasma than quercetin administered in solution; hence, one might anticipate a longer quercetin residence time in tissues that may affect therapeutic efficacy. The pharmacokinetics of quercetin and its breakdown products need to be investigated further to better understand the observed effects.
Quercetin inhibits many protein kinases with a half maximal inhibitory concentration in the low micromolar range.15 In other experiments, we have demonstrated that spinal cord injury results in increased activation of mitogen-activated protein (MAP) kinases (p38 MAPK, extracellular signal-regulated kinase and c-Jun N-terminal kinase) in the spinal cord immediately adjacent to the site of injury and that administration of quercetin twice daily normalizes the MAP kinase activation state (Juurlink, unpublished observations). This suggests that sufficient quercetin reaches the tissues to inhibit MAP kinase activation. It may be that thrice daily administration of quercetin maintains tissue quercetin levels at sufficiently high levels to suppress normal levels of MAP kinase activation, thus interfering with repair processes. This clearly needs to be investigated further.
Although the specific pathways through which quercetin results in neuroprotection still require further investigation, the results of our studies strongly suggest that administration of quercetin after spinal cord trauma supports functional recovery when the right treatment protocol is chosen. Quercetin has been a significant component of the diet during human evolution and, not surprisingly, is well tolerated in humans even when administered intravenously.16 A less invasive route of administering quercetin is orally. Oral intake of 250 mg quercetin four times daily has resulted in a fasting plasma level of 1.5 μM,17 suggesting that peak plasma levels may well attain 5 μM, within the therapeutic range we have previously shown in spinal cord-injured rat.1
Conflict of interest
The authors declare no conflict of interest.
References
Schültke E, Kendall E, Kamencic H, Ghong Z, Griebel RW, Juurlink BHJ . Quercetin promotes recovery from acute spinal cord injury: an MRI supported efficacious dose determination. J Neurotrauma 2003; 20: 583–591.
Schültke E, Kamencic H, Zhao M, Tian G-F, Baker AJ, Griebel RW et al. Neuroprotection following fluid percussion brain trauma. A pilot study using quercetin. J Neurotrauma 2005; 22: 1475–1484.
Tator CH, Fehlings MG . Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991; 75: 25–26.
Tator CH . Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 1995; 5: 407–413.
Tator CH, Koyanagi I . Vascular mechanisms in the pathophysiology of human spinal cord injury. J Neurosurg 1997; 86: 483–492.
Carlson SL, Parrish ME, Springer JE, Doty K, Dossett L . Acute inflammatory response in spinal cord injury following impact injury. Exp Neurol 1998; 152: 77–88.
Juurlink BHJ, Paterson PG . Review of oxidative stress in brain and spinal cord injury: suggestions for pharmacological interventions and nutritional management strategies. J Spinal Cord Med 1998; 21: 309–334.
Sekhon LHS, Fehlings MG . Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 2001; 26: S2–12.
Pincemail J, Deby C, Thirion A, De Btuyn-Dister M, Goutier R . Human myeloperoxidase activity is inhibited in vitro by quercetin. Comparison with three related compounds. Experientia 1998; 44: 450–453.
Klebanoff SJ . Oxygen metabolites from phagocytes. In: Gallin JI and Snyderman R (eds). Inflammation: basic principles and clinical correlates. Lippincott Williams & Wilkins: Philadelphia, 1999, pp 721–768.
Rivlin AS, Tator CH . Effect of duration of acute spinal cord compression in a new acute injury model in the rat. Surg Neurol 1978; 10: 38–43.
Basso DM, Beattie MS, Bresnahan JC . A sensitive and reliable locomotor rating scale for open field tests in rats. J Neurotrauma 1995; 12: 1–21.
Basso DM, Beattie MS, Bresnahan JC, Anderson DK, Faden AI, Gruner JA et al. MASCIS evaluation of open field locomotor scores: Effects of experience and teamwork on reliability. J Neurotrauma 1996; 13: 343–359.
Khaled KA, El-Sayed YM, Al-Hadiya BM . Disposition of the flavonoid quercetin in rats after single intravenous and oral doses. Drug Dev Ind Pharm 2003; 29: 397–403.
Davies SP, Reddy H, Caivano M, Cohen P . Specificity and mechanism of action of some commonly used protein kinase inhibitors. Biochem J 2000; 351: 95–105.
Gugler R, Leschik M, Dengler HJ . Disposition of quercetin in man after single oral and intravenous doses. Eur J Clin Pharmacol 1975; 9: 229–234.
Conquer JA, Maiani G, Azzini E, Raguzzini A, Holub BJ . Supplementation with quercetin markedly increases plasma quercetin concentration without effect on selected risk factors for heart disease in healthy subjects. J Nutr 1998; 128: 593–597.
Acknowledgements
We thank our technicians Mehri Herman, Arlene Drimmie and Hui Huang as well as Lloyd Jennett from RUH for technical support. We also thank Mrs Angela Damant, Mrs Michel Moroz and Mr Evan Matshes, who provided assistance with randomization, treatment and care of our animals. This study was supported by the Saskatchewan Health Research Foundation and by the Christopher Reeve Paralysis Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schültke, E., Kamencic, H., Skihar, V. et al. Quercetin in an animal model of spinal cord compression injury: correlation of treatment duration with recovery of motor function. Spinal Cord 48, 112–117 (2010). https://doi.org/10.1038/sc.2009.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.111
Keywords
This article is cited by
-
Quercetin prevents necroptosis of oligodendrocytes by inhibiting macrophages/microglia polarization to M1 phenotype after spinal cord injury in rats
Journal of Neuroinflammation (2019)
-
Quercetin suppresses NLRP3 inflammasome activation and attenuates histopathology in a rat model of spinal cord injury
Spinal Cord (2016)
-
Quercetin Promotes Neuronal and Behavioral Recovery by Suppressing Inflammatory Response and Apoptosis in a Rat Model of Intracerebral Hemorrhage
Neurochemical Research (2015)
-
Oxidative stress in spinal cord injury and antioxidant-based intervention
Spinal Cord (2012)
-
Quercetin attenuates inflammatory processes after spinal cord injury in an animal model
Spinal Cord (2010)