Abstract
Study design:
Case report and review of literature.
Objectives:
To report a case of a woman with paraplegia who had ruptured ectopic pregnancy but presented with minimal non-specific symptoms and no clinical signs. A trans-vaginal scan confirmed the diagnosis and an emergency laprotomy was performed to save the patient's life.
Setting:
Regional spinal injury unit in North West England.
Conclusion:
The diagnosis of ruptured ectopic in spinal cord injury woman can be difficult due to the lack of classical signs and symptoms. Awareness and constant vigilance is required to detect the early signs. Clinicians looking after such women should have sound knowledge of nervous system diseases and their pathophysiology. There should be a high index of suspicion when managing such cases and a prompt surgical treatment should be initiated.
Similar content being viewed by others
Introduction
Ectopic pregnancy remains a serious cause of maternal morbidity and mortality.1 Despite advances in the diagnosis and treatment of the tubal pregnancy, rupture remains a significant problem.2 The diagnosis of ruptured ectopic pregnancy has traditionally been made on clinical grounds: sudden abdominal pain, acute abdomen, cervical tenderness at physical examination, heamodynamic instability and dropping hematocrit.
Diagnosing ruptured ectopic in a paraplegic patient poses an extraordinary challenge. The lack of typical symptoms and signs of acute abdomen in a paraplegic patient makes it difficult for the clinician to make an accurate diagnosis, which may result in delayed surgery associated with a mortality rate of 10–15%.3 We present herein the case of a spinal cord injury (SCI) patient who had a ruptured ectopic pregnancy. We describe our management to help other gynaecologist make an appropriate diagnosis and initiate early surgical treatment.
Case report
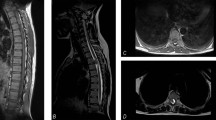
Our patient is a 35-year-old woman who has complete paraplegia below the level of T10 due to previous T10–T11 SCI. She presented with 6 weeks of amenorrhoea and feeling generally unwell. She gave a history of palpitation and having symptoms of ‘food poisoning’ for about 1 week. She was seen in a walk-in centre for these symptoms and was treated for urinary tract infection. She had had an early miscarriage 3 years earlier.
In the clinic she was found to be pale and sweating. On physical examination she was tachycardic with a pulse rate of 140 per min and BP of 110/40 mm Hg. Abdominal examination revealed mild distension, but no signs of peritoneal irritation such as tenderness, muscular rigidity or rebound pain. A trans-vaginal scan (TVS) was performed that showed irregular endometrium and collection (10 × 10 cm) in pouch of Douglas. We suspected ruptured ectopic pregnancy and an emergency laprotomy was arranged. An expert anaesthetist with special interest in SCI patients managed her during the intraoperative and immediate postoperative period. Urgent blood investigations showed a preoperative haemoglobin (Hb) of 8.8 g per 100 ml. On the way to operating theatre, she was given intravenous fluids to correct hypo-volumic shock. The abdomen was opened through a sub-umbilical midline incision. Blood clots of about 600 ml were removed from the pelvis and the site of ruptured ectopic pregnancy identified. We performed a left-sided salpingectomy after assessing the other tube, which appeared healthy. Mass closure of the abdomen was performed. Postoperative Hb was 6.5 g per 100 ml and she was transfused three units of blood. Low molecular weight heparin was stared for thromboprophylaxis. She was transferred to the regional spinal injury unit for postoperative care. After 6 weeks she was well when seen in our follow-up clinic. Histology report of the fallopian tube removed during the operation confirmed the diagnosis of ectopic pregnancy.
Discussion
There has been continued improvement in the care of patients with SCI during the past few decades. Most women live beyond child-bearing age that makes it likely that obstetricians are required to manage more of such pregnancies.4 These patients present specific problems that can be life threatening during their pregnancies. In order to meet their diagnostic challenge, the surgeon must know the exact level of the SC lesion and whether it is complete or incomplete. The pathophysiological changes caused by the SCI must be kept in mind while evaluating the patient.
The presentation of acute abdomen in the patients with paraplegia depends on the neurological level, the completeness of the SCI and the degree of the continuity of the reflex arc below the level of injury.5 If the reflex arc below the level of injury is intact, upper motor neuron state returns with spastic paralysis of the abdominal muscles. If the reflex arc is damaged then a lower motor neurone state appears below the level of injury. Normal somatic sensation to the anterior abdominal wall originates from T7 to T11, and L1. Patients with complete cord injuries above T7 will have no abdominal wall sensation. Painful stimuli from the abdominal viscera reach the cord by way of the thoracic sympathetic, splanchnic, hypogastric or pelvic nerves. The sympathetic outflow to most of the viscera comes from the T5 level or below. The visceral sensory fibres of the rectum and bladder are carried via the S2–S4 parasympathetic system. Patients with injuries above the level of the splanchnic outflow tract at T6 are referred to as having ‘high’ cord injuries. Below that level, patients can be regarded as having ‘low’ cord injuries.6
In young healthy women with acute abdomen, the most common presenting symptom is pain, but the SCI patients may or may not have pain. Patients with high cord injuries have altered physiological response and loss of sensory, motor and reflex function. An acute intra-abdominal process may present as increased spasticity, referred shoulder tip pain, alteration in bowel function, nausea and vomiting, autonomic dysreflexia or simply a feeling that there is ‘something wrong’. Our patient had low cord lesion and presented with nausea and abdominal cramps. We emphasize the need to be aware of possible intra-abdominal disease as soon as the patient deviates from her status quo in any respect. Loss of appetite usually is the first indication that something is wrong. Symptoms like nausea and abdominal cramps, which simulate food poisoning may be a warning of impeding emergency. Our patient complained of something wrong but could not localize it and was restless. In many cases patients can localize it; the pain may be sharp or dull and referred to distant skin area of the dermatome supplying the involved viscera.3
Symptoms of autonomic dysreflexia are useful in early recognition of abdominal visceral disease. They can be in the form of sweating, increased spasticity of the limbs, sphincter or adjacent abdominal muscle. Autonomic dysreflexia is a problem unique to SCI patients with injury at the T6 level and above. In our patient these symptoms were absent.
Vital signs have been used traditionally to assess the stability of acutely ill patients. A rise in pulse rate is one of the earliest sign of hypovolumic shock and also of dysreflexia due to abdominal disease. In patients with SCI above the splanchnic outflow, temporary hypertension can occur that can be misleading. It is crucial that an experience anaesthetist, who has special interest in managing patients with SCI, be involved from an early stage.
The use of ultrasound in the diagnosis of ectopic pregnancy has been evaluated in many studies and it is now widely used for this purpose. The appearance of the adnexal mass and type and amount of intra-peritoneal fluid present have been suggested as possible predictor of tubal rupture. Free intaperitoneal fluid particularly when echogenic in appearance or substantial in volume has been suggested both as a sign of ectopic pregnancy and as a possible sign of rupture when there is an ectopic pregnancy.7
Although TVS is important in the management of ectopic pregnancy, in most of the cases clinical status of patient is the deciding factor for determining the need for the surgical intervention. The role of TVS however cannot be overemphasized in particular, when the clinical signs and symptoms are unreliable.
The operative management of the patients with SCI is the same as the patients with normal neuraxis.5 Retention sutures are used to close all abdominal wounds to handle the increased wound tension that can occur from abdominal spasticity. The postoperative care can be difficult as there can be problem with spasticity, hypertension, urinary tract infection and decubitus ulcer. These patients are best managed in spinal units where trained staff are available round the clock to deal with these problems. Our patient tolerated the surgery well and necessary measures were taken to deal with possible postoperative problems.
In conclusion, the diagnosis of ruptured ectopic in SCI woman can be difficult due to lack of classical signs and symptoms. In pregnancy an early referral in clinic for TVS is recommended in such patients. Awareness and constant vigilance is required to detect the early signs. Clinicians looking after such women should have sound knowledge of nervous system diseases and its pathophysiology. There should be a high index of suspicion when managing such cases and a prompt surgical treatment initiated.
References
Carson SA, Buster JE . Ectopic pregnancy. N Eng J Med 1993; 329: 1174–1181.
Mol BWJ, Hajenius PJ, Ankum WM, Van der Veen F, Bossuyt PMM . Screening for ectopic pregnancy in symptom free women at increased risk. Obstet Gynecol 1997; 89: 704–707.
Bar-On Z, Ohry A . The acute abdomen in spinal cord injury individuals. Paraplegia 1995; 33: 704–706.
Neumayer LA, Bull DA, Mohr JD, Putnam CW . The acutely affected abdomen in paraplegic spinal cord injury patients. Ann Surg 1990; 212: 561–566.
Charney KJ, Juler GL, Comarr AE . General surgery problems in patients with spinal cord injuries. Arch Surg 1975; 110: 1083–1088.
Juler GL, Eltoral IM . The acute abdomen in spinal cord injury patients. Paraplegia 1985; 23: 118–123.
Frates MC, Brown DL, Doubilet PM, Hornstein MD . Tubal rupture in patients with ectopic pregnancy: diagnosis with transvaginal US. Radiology 1994; 191: 769–772.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rawal, N., Sharma, S. & Soni, B. A case of silent rupture of an ectopic pregnancy. Spinal Cord 46, 758–759 (2008). https://doi.org/10.1038/sc.2008.27
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.27
Keywords
This article is cited by
-
Colonic obstruction in a tetraplegic patient: a common symptom from an uncommon cause
Spinal Cord Series and Cases (2020)