Abstract
Immune-regulation strategies, such as vaccination and immunotherapy, are key to the prevention and treatment of respiratory infectious diseases. In particular, nanomedicines can be engineered and formulated to regulate host immunity in various tissues, including in the lungs. In this Review, we discuss the design of nanovaccines, including lipid-nanocarrier-based messenger RNA nanovaccines, highlighting engineering strategies for different administration routes, including nasal administration. We further discuss the engineering of immunomodulatory nanomedicines for the treatment of respiratory infectious diseases by blocking pro-inflammatory signalling pathways and virus entry, modulating stimulated immune cells and scavenging reactive oxygen species. In addition, we examine the funding situation for research on respiratory infectious diseases before and after the COVID-19 pandemic. Finally, we summarize future opportunities, challenges and global trends for immunoregulatory nanomedicine for the treatment of respiratory infections.
Key points
-
Nanomedicines can be designed to optimize the physical and chemical properties of immunologic agents for immune regulation in the prevention and treatment of respiratory infectious diseases.
-
Nanovaccines based on lipid and polymeric nanoparticles can deliver mRNA, overcome the physiological barriers of nasal mucosal immunity and improve the efficiency of antigen presentation.
-
Nanotherapeutics can be engineered to regulate the immune microenvironment in respiratory infectious diseases by blocking pro-inflammatory signalling pathways and virus entry, modulating stimulated immune cells and scavenging inflammatory cytokines and reactive oxygen species.
-
Research funding for respiratory infectious diseases has increased after the COVID-19 outbreak.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$99.00 per year
only $8.25 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Dowell, S. F. & Ho, M. S. Seasonality of infectious diseases and severe acute respiratory syndrome—what we don’t know can hurt us. Lancet Infect. Dis. 4, 704–708 (2004).
Bygbjerg, I. C. Double burden of noncommunicable and infectious diseases in developing countries. Science 337, 1499–1501 (2012).
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20, 193–205 (2022).
Dong, E., Du, H. & Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 20, 533–534 (2020).
Mosier, D. A. Bacterial pneumonia. Vet. Clin. North. Am. Food Anim. Pract. 13, 483–493 (1997).
Bradley, B. T. & Bryan, A. Emerging respiratory infections: the infectious disease pathology of SARS, MERS, pandemic influenza, and Legionella. Semin. Diagn. Pathol. 36, 152–159 (2019).
Shao, X. et al. An innate immune system cell is a major determinant of species-related susceptibility differences to fungal pneumonia. J. Immunol. 175, 3244–3251 (2005).
Zhou, P. & Shi, Z.-L. SARS-CoV-2 spillover events. Science 371, 120–122 (2021).
Abraham, E. et al. Consensus conference definitions for sepsis, septic shock, acute lung injury, and acute respiratory distress syndrome: time for a reevaluation. Crit. Care Med. 28, 232–235 (2000).
DiSilvio, B. et al. Complications and outcomes of acute respiratory distress syndrome. Crit. Care Med. 42, 349–361 (2019).
Li, K. et al. Middle East respiratory syndrome coronavirus causes multiple organ damage and lethal disease in mice transgenic for human dipeptidyl peptidase 4. J. Infect. Dis. 213, 712–722 (2016).
Singh, A. Eliciting B cell immunity against infectious diseases using nanovaccines. Nat. Nanotechnol. 16, 16–24 (2021).
Saunders, K. O. et al. Neutralizing antibody vaccine for pandemic and pre-emergent coronaviruses. Nature 594, 553–559 (2021).
Su, Z. et al. Bioresponsive nano-antibacterials for H2S-sensitized hyperthermia and immunomodulation against refractory implant-related infections. Sci. Adv. 8, eabn1701 (2022).
Chaudhary, N., Weissman, D. & Whitehead, K. A. mRNA vaccines for infectious diseases: principles, delivery and clinical translation. Nat. Rev. Drug. Discov. 20, 817–838 (2021).
Wareing, M. D. & Tannock, G. A. Live attenuated vaccines against influenza; an historical review. Vaccine 19, 3320–3330 (2001).
Skountzou, I. et al. Salmonella flagellins are potent adjuvants for intranasally administered whole inactivated influenza vaccine. Vaccine 28, 4103–4112 (2010).
Ellebedy, A. H. et al. Contemporary seasonal influenza A (H1N1) virus infection primes for a more robust response to split inactivated pandemic influenza A (H1N1) virus vaccination in ferrets. Clin. Vaccine Immunol. 17, 1998–2006 (2010).
Ninomiya, A. Intranasal administration of a synthetic peptide vaccine encapsulated in liposome together with an anti-CD40 antibody induces protective immunity against influenza A virus in mice. Vaccine 20, 3123–3129 (2002).
Roy, S. et al. Viral vector and route of administration determine the ILC and DC profiles responsible for downstream vaccine-specific immune outcomes. Vaccine 37, 1266–1276 (2019).
Mielcarek, N., Alonso, S. & Locht, C. Nasal vaccination using live bacterial vectors. Adv. Drug. Deliv. Rev. 51, 55–69 (2001).
Wu, Y. et al. A recombinant spike protein subunit vaccine confers protective immunity against SARS-CoV-2 infection and transmission in hamsters. Sci. Transl. Med. 13, eabg1143 (2021).
Smith, T. R. F. et al. Immunogenicity of a DNA vaccine candidate for COVID-19. Nat. Commun. 11, 2601 (2020).
Narasimhan, M. et al. Serological response in lung transplant recipients after two doses of SARS-CoV-2 mRNA vaccines. Vaccines 9, 708 (2021).
Berkhout, B., Verhoef, K., van Wamel, J. L. B. & Back, N. K. T. Genetic instability of live, attenuated human immunodeficiency virus type 1 vaccine strains. J. Virol. 73, 1138–1145 (1999).
Cevik, M. COVID-19 vaccines: keeping pace with SARS-CoV-2 variants. Cell 184, 5077–5081 (2021).
Khalaj‐Hedayati, A., Chua, C. L. L., Smooker, P. & Lee, K. W. Nanoparticles in influenza subunit vaccine development: immunogenicity enhancement. Influenza Other Resp. Vir. 14, 92–101 (2020).
Kim, C. G., Kye, Y.-C. & Yun, C.-H. The role of nanovaccine in cross-presentation of antigen-presenting cells for the activation of CD8+ T cell responses. Pharmaceutics 11, 612 (2019).
Silva, A. L., Soema, P. C., Slütter, B., Ossendorp, F. & Jiskoot, W. PLGA particulate delivery systems for subunit vaccines: linking particle properties to immunogenicity. Hum. Vaccines Immunother. 12, 1056–1069 (2016).
Huang, J. et al. Nasal nanovaccines for SARS-CoV-2 to address COVID-19. Vaccines 10, 405 (2022).
Hussain, A. et al. mRNA vaccines for COVID-19 and diverse diseases. J. Control. Rel. 345, 314–333 (2022).
Meng, Q. et al. Capturing cytokines with advanced materials: a potential strategy to tackle COVID‐19 cytokine storm. Adv. Mater. 33, 2100012 (2021).
Hotchkiss, R. S., Coopersmith, C. M., McDunn, J. E. & Ferguson, T. A. The sepsis seesaw: tilting toward immunosuppression. Nat. Med. 15, 496–497 (2009).
van de Veerdonk, F. L. et al. A guide to immunotherapy for COVID-19. Nat. Med. 28, 39–50 (2022).
Wykes, M. N. & Lewin, S. R. Immune checkpoint blockade in infectious diseases. Nat. Rev. Immunol. 18, 91–104 (2018).
Florindo, H. F. et al. Immune-mediated approaches against COVID-19. Nat. Nanotechnol. 15, 630–645 (2020).
Jiang, S., Zhang, X., Yang, Y., Hotez, P. J. & Du, L. Neutralizing antibodies for the treatment of COVID-19. Nat. Biomed. Eng. 4, 1134–1139 (2020).
Nasiruddin, M., Neyaz, Md. K. & Das, S. Nanotechnology-based approach in tuberculosis treatment. Tuberc. Res. Treat. 2017, 1–12 (2017).
Abani, O. et al. Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 397, 1637–1645 (2021).
The REMAP-CAP Investigators. Interleukin-6 receptor antagonists in critically ill patients with Covid-19. N. Engl. J. Med. 384, 1491–1502 (2021).
Kozlov, M. Omicron overpowers key COVID antibody treatments in early tests. Nature https://doi.org/10.1038/d41586-021-03829-0 (2021).
Roback, J. D. & Guarner, J. Convalescent plasma to treat COVID-19: possibilities and challenges. JAMA 323, 1561–1562 (2020).
Nguyen, P. T. N., Nho Van Le, Nguyen Dinh, H. M., Nguyen, B. Q. P. & Nguyen, T. V. A. Lung penetration and pneumococcal target binding of antibiotics in lower respiratory tract infection. Curr. Med. Res. Opin. 38, 2085–2095 (2022).
Qiao, Q. et al. Nanomedicine for acute respiratory distress syndrome: the latest application, targeting strategy, and rational design. Acta Pharm. Sin. B 11, 3060–3091 (2021).
Duan, Y., Wang, S., Zhang, Q., Gao, W. & Zhang, L. Nanoparticle approaches against SARS-CoV-2 infection. Curr. Opin. Solid. State Mater. Sci. 25, 100964 (2021).
Doroudian, M., MacLoughlin, R., Poynton, F., Prina-Mello, A. & Donnelly, S. C. Nanotechnology based therapeutics for lung disease. Thorax 74, 965–976 (2019).
Yang, H. et al. Amino acid-dependent attenuation of Toll-like receptor signalling by peptide-gold nanoparticle hybrids. ACS Nano 9, 6774–6784 (2015).
Gao, Y., Dai, W., Ouyang, Z., Shen, M. & Shi, X. Dendrimer-mediated intracellular delivery of fibronectin guides macrophage polarization to alleviate acute lung injury. Biomacromolecules 24, 886–895 (2023).
Liu, F.-C. et al. Use of cilomilast-loaded phosphatiosomes to suppress neutrophilic inflammation for attenuating acute lung injury: the effect of nanovesicular surface charge. J. Nanobiotechnol. 16, 35 (2018).
Kou, M. et al. Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool? Cell Death Dis. 13, 580 (2022).
Liu, W. et al. Recent advances of cell membrane-coated nanomaterials for biomedical applications. Adv. Funct. Mater. 30, 2003559 (2020).
Brahmakshatriya, V. et al. IL-6 production by TLR-activated APC broadly enhances aged cognate CD4 helper and B cell antibody responses in vivo. J. Immunol. 198, 2819–2833 (2017).
Hong, S. et al. B cells are the dominant antigen-presenting cells that activate naive CD4+ T cells upon immunization with a virus-derived nanoparticle antigen. Immunity 49, 695–708 (2018).
Denzel, A. et al. Basophils enhance immunological memory responses. Nat. Immunol. 9, 733–742 (2008).
Kim, J. et al. Self-assembled mRNA vaccines. Adv. Drug. Deliv. Rev. 170, 83–112 (2021).
Nakahashi-Ouchida, R., Fujihashi, K., Kurashima, Y., Yuki, Y. & Kiyono, H. Nasal vaccines: solutions for respiratory infectious diseases. Trends Mol. Med. 29, 124–140 (2023).
Soema, P. C., Kompier, R., Amorij, J.-P. & Kersten, G. F. A. Current and next generation influenza vaccines: formulation and production strategies. Eur. J. Pharm. Biopharm. 94, 251–263 (2015).
Nemes, E. et al. Prevention of M. tuberculosis infection with H4:IC31 vaccine or BCG revaccination. N. Engl. J. Med. 379, 138–149 (2018).
Al-Halifa, S., Gauthier, L., Arpin, D., Bourgault, S. & Archambault, D. Nanoparticle-based vaccines against respiratory viruses. Front. Immunol. 10, 22 (2019).
Li, M. et al. COVID-19 vaccine development: milestones, lessons and prospects. Signal. Transduct. Target. Ther. 7, 146 (2022).
Tiboni, M., Casettari, L. & Illum, L. Nasal vaccination against SARS-CoV-2: synergistic or alternative to intramuscular vaccines? Int. J. Pharm. 603, 120686 (2021).
Weng, Y. et al. The challenge and prospect of mRNA therapeutics landscape. Biotechnol. Adv. 40, 107534 (2020).
Guo, S. et al. Membrane‐destabilizing ionizable lipid empowered imaging‐guided siRNA delivery and cancer treatment. Exploration 1, 35–49 (2021).
Yang, T. et al. Efficient hepatic delivery and protein expression enabled by optimized mRNA and ionizable lipid nanoparticle. Bioact. Mater. 5, 1053–1061 (2020).
Zhang, H. et al. Aerosolizable lipid nanoparticles for pulmonary delivery of mRNA through design of experiments. Pharmaceutics 12, 1042 (2020).
Lokugamage, M. P. et al. Optimization of lipid nanoparticles for the delivery of nebulized therapeutic mRNA to the lungs. Nat. Biomed. Eng. 5, 1059–1068 (2021).
Cheng, Q. et al. Selective organ targeting (SORT) nanoparticles for tissue-specific mRNA delivery and CRISPR–Cas gene editing. Nat. Nanotechnol. 15, 313–320 (2020).
Dilliard, S. A., Cheng, Q. & Siegwart, D. J. On the mechanism of tissue-specific mRNA delivery by selective organ targeting nanoparticles. Proc. Natl Acad. Sci. USA 118, e2109256118 (2021).
Dong, Y. et al. Poly(glycoamidoamine) brushes formulated nanomaterials for systemic siRNA and mRNA delivery in vivo. Nano Lett. 16, 842–848 (2016).
Kaczmarek, J. C. et al. Polymer–lipid nanoparticles for systemic delivery of mRNA to the lungs. Angew. Chem. Int. Edn 55, 13808–13812 (2016).
Kaczmarek, J. C. et al. Optimization of a degradable polymer–lipid nanoparticle for potent systemic delivery of mRNA to the lung endothelium and immune cells. Nano Lett. 18, 6449–6454 (2018).
Capasso Palmiero, U. et al. Poly(beta-amino ester)-co-poly(caprolactone) terpolymers as nonviral vectors for mRNA delivery in vitro and in vivo. Adv. Healthc. Mater. 7, 1800249 (2018).
Patel, A. K. et al. Inhaled nanoformulated mRNA polyplexes for protein production in lung epithelium. Adv. Mater. 31, 1805116 (2019).
Kaczmarek, J. C. et al. Systemic delivery of mRNA and DNA to the lung using polymer-lipid nanoparticles. Biomaterials 275, 120966 (2021).
Higuchi, A. et al. Material design for next-generation mRNA vaccines using lipid nanoparticles. Polym. Rev. 63, 394–436 (2023).
Tseng, H. F. et al. Effectiveness of mRNA-1273 against SARS-CoV-2 omicron and delta variants. Nat. Med. 28, 1063–1071 (2022).
Andrews, N. et al. Covid-19 vaccine effectiveness against the omicron (B.1.1.529) variant. N. Engl. J. Med. 386, 1532–1546 (2022).
Wang, K. et al. Transmission characteristics and inactivated vaccine effectiveness against transmission of SARS-CoV-2 omicron BA.5 variants in Urumqi, China. JAMA Netw. Open. 6, e235755 (2023).
Low, J. G. et al. A phase I/II randomized, double-blinded, placebo-controlled trial of a self-amplifying Covid-19 mRNA vaccine. npj Vaccines 7, 161 (2022).
Annual R&D day. Moderna https://investors.modernatx.com/events-and-presentations/events/event-details/2022/Annual-RD-Day-2022/default.aspx (2022).
Bahl, K. et al. Preclinical and clinical demonstration of immunogenicity by mRNA vaccines against H10N8 and H7N9 influenza viruses. Mol. Ther. 25, 1316–1327 (2017).
Arevalo, C. P. et al. A multivalent nucleoside-modified mRNA vaccine against all known influenza virus subtypes. Science 378, 899–904 (2022).
Miao, L., Zhang, Y. & Huang, L. mRNA vaccine for cancer immunotherapy. Mol. Cancer 20, 41 (2021).
Shim, B. S. et al. Intranasal immunization with plasmid DNA encoding spike protein of SARS-coronavirus/polyethylenimine nanoparticles elicits antigen-specific humoral and cellular immune responses. BMC Immunol. 11, 65 (2010).
Stemirna Therapeutics. Vaccine agent for treating or preventing coronavirus disease. WO2021159985A1 (World Intellectual Property Organization, 2021).
Yang, R. et al. A core–shell structured COVID-19 mRNA vaccine with favorable biodistribution pattern and promising immunity. Signal. Transduct. Target. Ther. 6, 213 (2021).
Yan, Y. et al. Systemic mRNA delivery to the lungs by functional polyester-based carriers. Biomacromolecules 18, 4307–4315 (2017).
Suberi, A. et al. Polymer nanoparticles deliver mRNA to the lung for mucosal vaccination. Sci. Transl. Med. 15, eabq0603 (2023).
McKinlay, C. J. et al. Charge-altering releasable transporters (CARTs) for the delivery and release of mRNA in living animals. Proc. Natl. Acad. Sci. USA 114, 448–456 (2017).
Haabeth, O. A. W. et al. mRNA vaccination with charge-altering releasable transporters elicits human T cell responses and cures established tumors in mice. Proc. Natl. Acad. Sci. USA 115, E9153–E9161 (2018).
Petsch, B. et al. Protective efficacy of in vitro synthesized, specific mRNA vaccines against influenza A virus infection. Nat. Biotechnol. 30, 1210–1216 (2012).
Qiu, Y. et al. Effective mRNA pulmonary delivery by dry powder formulation of PEGylated synthetic KL4 peptide. J. Control. Rel. 314, 102–115 (2019).
Lou, B. et al. Preparation of mRNA polyplexes with post-conjugated endosome-disruptive peptides. Methods Mol. Biol. 2355, 275–286 (2021).
Yeom, J. H. et al. Inhibition of xenograft tumor growth by gold nanoparticle-DNA oligonucleotide conjugates-assisted delivery of BAX mRNA. PLoS One 8, 75369 (2013).
Sun, P. et al. Transcellular delivery of messenger RNA payloads by a cationic supramolecular MOF platform. Chem. Commun. 54, 11304–11307 (2018).
Tsai, S. J. et al. Exosome-mediated mRNA delivery in vivo is safe and can be used to induce SARS-CoV-2 immunity. J. Biol. Chem. 297, 101266 (2021).
Zhitnyuk, Y. et al. Efficient mRNA delivery system utilizing chimeric VSVG-L7Ae virus-like particles. Biochem. Biophys. Res. Commun. 505, 1097–1102 (2018).
Tacchi, L. et al. Nasal immunity is an ancient arm of the mucosal immune system of vertebrates. Nat. Commun. 5, 5205 (2014).
Strugnell, R. A. & Wijburg, O. L. The role of secretory antibodies in infection immunity. Nat. Rev. Microbiol. 8, 656–667 (2010).
Jansen, E. M. et al. Are inhaled mRNA vaccines safe and effective? A review of preclinical studies. Expert. Opin. Drug. Deliv. 19, 1471–1485 (2022).
Mao, T. et al. Unadjuvanted intranasal spike vaccine elicits protective mucosal immunity against sarbecoviruses. Science 378, eabo2523 (2022).
Hartwell, B. L. et al. Intranasal vaccination with lipid-conjugated immunogens promotes antigen transmucosal uptake to drive mucosal and systemic immunity. Sci. Transl. Med. 14, eabn1413 (2022).
Wang, J. et al. Pulmonary surfactant-biomimetic nanoparticles potentiate heterosubtypic influenza immunity. Science 367, 869 (2020).
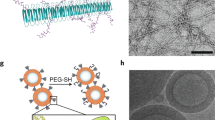
Zheng, B. et al. Inhalable nanovaccine with biomimetic coronavirus structure to trigger mucosal immunity of respiratory tract against COVID-19. Chem. Eng. J. 418, 129392 (2021).
Popowski, K. D. et al. Inhalable dry powder mRNA vaccines based on extracellular vesicles. Matter 5, 2960–2974 (2022).
Bessa, J. et al. Efficient induction of mucosal and systemic immune responses by virus-like particles administered intranasally: implications for vaccine design. Eur. J. Immunol. 38, 114–126 (2008).
Schuster, S. J. et al. Chimeric antigen receptor T cells in refractory B-cell lymphomas. N. Engl. J. Med. 377, 2545–2554 (2017).
Koppolu, B. & Zaharoff, D. A. The effect of antigen encapsulation in chitosan particles on uptake, activation and presentation by antigen presenting cells. Biomaterials 34, 2359–2369 (2013).
Wilson, J. T. et al. Enhancement of MHC-I antigen presentation via architectural control of pH-responsive, endosomolytic polymer nanoparticles. AAPS J. 17, 358–369 (2015).
Xing, Y. et al. Synthesis of poly(acyclic orthoester)s: acid-sensitive biomaterials for enhancing immune responses of protein. Vaccine. Angew. Chem. Int. Edn. 59, 7235–7239 (2020).
Cai, H. et al. Multivalent antigen presentation enhances the immunogenicity of a synthetic three-component HIV-1 V3 glycopeptide vaccine. ACS Cent. Sci. 4, 582–589 (2018).
Zhang, F., Lu, Y. J. & Malley, R. Multiple antigen-presenting system (MAPS) to induce comprehensive B- and T-cell immunity. Proc. Natl. Acad. Sci. USA 110, 13564–13569 (2013).
Wang, C. et al. Bioengineering of artificial antigen presenting cells and lymphoid organs. Theranostics 7, 3504–3516 (2017).
Steenblock, E. R. & Fahmy, T. M. A comprehensive platform for ex vivo T-cell expansion based on biodegradable polymeric artificial antigen-presenting cells. Mol. Ther. 16, 765–772 (2008).
Joshi, N., Walter, J. M. & Misharin, A. V. Alveolar macrophages. Cell. Immunol. 330, 86–90 (2018).
Allard, B., Panariti, A. & Martin, J. G. Alveolar macrophages in the resolution of inflammation, tissue repair, and tolerance to infection. Front. Immunol. 9, 1777 (2018).
Chuquimia, O. D. et al. The role of alveolar epithelial cells in initiating and shaping pulmonary immune responses: communication between innate and adaptive immune systems. PLoS One 7, e32125 (2012).
Mantovani, A. et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 25, 677–686 (2004).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395, 1054–1062 (2020).
Quinton, L. J., Walkey, A. J. & Mizgerd, J. P. Integrative physiology of pneumonia. Physiol. Rev. 98, 1417–1464 (2018).
Muhammad, W., Zhai, Z., Wang, S. & Gao, C. Inflammation‐modulating nanoparticles for pneumonia therapy. Wiley Interdisc. Rev. Nanomed. Nanobiotechnol. 14, e1763 (2022).
Ohbayashi, H. Matrix metalloproteinases in lung diseases. Curr. Protein Pept. Sci. 3, 409–421 (2002).
van den Brand, J. M. A., Haagmans, B. L., van Riel, D., Osterhaus, A. D. M. E. & Kuiken, T. The pathology and pathogenesis of experimental severe acute respiratory syndrome and influenza in animal models. J. Comp. Pathol. 151, 83–112 (2014).
Wang, P. et al. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature 593, 130–135 (2021).
Renn, A., Fu, Y., Hu, X., Hall, M. D. & Simeonov, A. Fruitful neutralizing antibody pipeline brings hope to defeat SARS-Cov-2. Trends Pharmacol. Sci. 41, 815–829 (2020).
Jiang, D., Liang, J., Li, Y. & Noble, P. W. The role of Toll-like receptors in non-infectious lung injury. Cell Res. 16, 693–701 (2006).
Gao, W. et al. Size-dependent anti-inflammatory activity of a peptide-gold nanoparticle hybrid in vitro and in a mouse model of acute lung injury. Acta Biomater. 85, 203–217 (2019).
Okutani, D., Lodyga, M., Han, B. & Liu, M. Src protein tyrosine kinase family and acute inflammatory responses. Am. J. Physiol. Lung Cell. Mol. Physiol. 291, L129–L141 (2006).
Hanke, J. H. et al. Discovery of a novel, potent, and Src family-selective tyrosine kinase inhibitor. J. Biol. Chem. 271, 695–701 (1996).
Fung, S.-Y. et al. The potential of nanoscale combinations of self-assembling peptides and amino acids of the Src tyrosine kinase inhibitor in acute lung injury therapy. Biomaterials 32, 4000–4008 (2011).
Zhang, C. Y. et al. pH-responsive nanoparticles targeted to lungs for improved therapy of acute lung inflammation/injury. ACS Appl. Mater. Interf. 11, 16380–16390 (2019).
Lo Cicero, A., Stahl, P. D. & Raposo, G. Extracellular vesicles shuffling intercellular messages: for good or for bad. Curr. Opin. Cell Biol. 35, 69–77 (2015).
Inal, J. M. Decoy ACE2-expressing extracellular vesicles that competitively bind SARS-CoV-2 as a possible COVID-19 therapy. Clin. Sci. 134, 1301–1304 (2020).
Xie, F. et al. Engineering extracellular vesicles enriched with palmitoylated ACE2 as COVID‐19 therapy. Adv. Mater. 33, 2103471 (2021).
Huang, X. et al. Nanotechnology-based strategies against SARS-CoV-2 variants. Nat. Nanotechnol. 17, 1027–1037 (2022).
Rao, L., Tian, R. & Chen, X. Cell-membrane-mimicking nanodecoys against infectious diseases. ACS Nano 14, 2569–2574 (2020).
Wang, C. et al. Membrane nanoparticles derived from ACE2-rich cells block SARS-CoV-2 infection. ACS Nano 15, 6340–6351 (2021).
Zhang, Q. et al. Cellular nanosponges inhibit SARS-CoV-2 infectivity. Nano Lett. 20, 5570–5574 (2020).
Lin, C. H., Chang, S. H. & Fang, J. Y. Recent advances using phosphodiesterase 4 (PDE4) inhibitors to treat inflammatory disorders: animal and clinical studies. Curr. Drug. Ther. 11, 21–40 (2016).
Yu, H.-P. et al. Oleic acid-based nanosystems for mitigating acute respiratory distress syndrome in mice through neutrophil suppression: how the particulate size affects therapeutic efficiency. J. Nanobiotechnol. 18, 25 (2020).
Wang, Z., Li, J., Cho, J. & Malik, A. B. Prevention of vascular inflammation by nanoparticle targeting of adherent neutrophils. Nat. Nanotechnol. 9, 204–210 (2014).
Okeke, E. B. et al. Inhibition of neutrophil elastase prevents neutrophil extracellular trap formation and rescues mice from endotoxic shock. Biomaterials 238, 119836 (2020).
Logie, C., Van Schaik, T., Pompe, T. & Pietsch, K. Fibronectin-functionalization of 3D collagen networks supports immune tolerance and inflammation suppression in human monocyte-derived macrophages. Biomaterials 268, 120498 (2021).
Yin, H., Fang, J., Liao, L., Nakamura, H. & Maeda, H. Styrene-maleic acid copolymer-encapsulated CORM2, a water-soluble carbon monoxide (CO) donor with a constant CO-releasing property, exhibits therapeutic potential for inflammatory bowel disease. J. Controlled Rel. 187, 14–21 (2014).
Guo, J. et al. Cyclodextrin-derived intrinsically bioactive nanoparticles for treatment of acute and chronic inflammatory diseases. Adv. Mater. 31, 1904607 (2019).
Rao, L. et al. Decoy nanoparticles protect against COVID-19 by concurrently adsorbing viruses and inflammatory cytokines. Proc. Natl. Acad. Sci. USA 117, 27141–27147 (2020).
Zhang, H. et al. Inhalable nanocatchers for SARS-CoV-2 inhibition. Proc. Natl. Acad. Sci. USA 118, e2102957118 (2021).
Li, Y. et al. Dual-mode nanoprobes for reactive oxygen species scavenging and treatment of acute lung injury. Appl. Surf. Sci. 610, 155458 (2023).
Zhu, Y. et al. Porous Se@SiO2 nanospheres treated paraquat-induced acute lung injury by resisting oxidative stress. Int. J. Nanomed. 12, 7143–7152 (2017).
Bhattacharjee, A., Basu, A., Biswas, J. & Bhattacharya, S. Nano-Se attenuates cyclophosphamide-induced pulmonary injury through modulation of oxidative stress and DNA damage in Swiss albino mice. Mol. Cell. Biochem. 405, 243–256 (2015).
Zhou, Y. et al. Inhalable gadofullerenol/[70] fullerenol as high-efficiency ROS scavengers for pulmonary fibrosis therapy. Nanomed. Nanotechnol. Biol. Med. 14, 1361–1369 (2018).
Li, L. et al. A broad-spectrum ROS-eliminating material for prevention of inflammation and drug-induced organ toxicity. Adv. Sci. 5, 1800781 (2018).
Ji, H. et al. Inhaled pro-efferocytic nanozymes promote resolution of acute lung injury. Adv. Sci. 9, 2201696 (2022).
Head, M. G., Brown, R. J., Newell, M. L., Scott, J. A. G., Batchelor, J. & Atun, R. The allocation of US$105 billion in global funding from G20 countries for infectious disease research between 2000 and 2017: a content analysis of investments. Lancet Glob. Health. 8, e1295–e1304 (2020).
Heida, R., Hinrichs, W. & Frijlink, H. Inhaled vaccine delivery in the combat against respiratory viruses: a 2021 overview of recent developments and implications for COVID-19. Expert. Rev. Vaccines 21, 957–974 (2022).
Li, J. X. et al. Safety and immunogenicity of heterologous boost immunisation with an orally administered aerosolised Ad5-nCoV after two-dose priming with an inactivated SARS-CoV-2 vaccine in Chinese adults: a randomised, open-label, single-centre trial. Lancet Respir. Med. 10, 739–748 (2022).
Saravolatz, L. D., Depcinski, S. & Sharma, M. Molnupiravir and nirmatrelvir-ritonavir: oral COVID antiviral drugs. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciac180 (2022).
Fernandes, Q. et al. Emerging COVID-19 variants and their impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann. Med. 54, 524–540 (2022).
Forgham, H., Kakinen, A., Qiao, R. & Davis, T. P. Keeping up with the COVIDs—could siRNA-based antivirals be a part of the answer? Exploration 2, 20220012 (2022).
AminJafari, A. & Ghasemi, S. The possible of immunotherapy for COVID-19: a systematic review. Int. Immunopharmacol. 83, 106455 (2020).
Wu, Q. et al. Evaluation of the safety profile of COVID-19 vaccines: a rapid review. BMC Med. 19, 173 (2021).
Schieffelin, J. S., Norton, E. B. & Kolls, J. K. What should define a SARS-CoV-2 “breakthrough” infection? J. Clin. Invest. 131, E151186 (2021).
Beatty, G. L. & Gladney, W. L. Immune escape mechanisms as a guide for cancer immunotherapy. Clin. Cancer Res. 21, 687–692 (2015).
Acknowledgements
The authors are supported by the National Key Research and Development Program of China (grant numbers 2021YFA1201000, 2018YFE0117800, 2021YFC2302400 and 2021YFE0106900), the National Natural Science Foundation of China (NSFC) key project (grant number 32030060); the NSFC (grant numbers 31971302, 31871003 and 32171394), the NSFC international collaboration key project (grant number 51861135103), the Natural Science Foundation of Guangdong Province of China (grant number 2019A1515011597), and the joint grant between Guangzhou City and College (grant number 202102010106), The Beijing–Tianjin–Hebei Basic Research Cooperation Project (grant number 19JCZDJC64100) and the Educational Commission of Guangdong Province of China key project (grant number 2020ZDZX2001).
Author information
Authors and Affiliations
Contributions
Y.X., Y.H. and M.X. contributed equally to the preparation of this manuscript. Y.X. and X.-J.L. contributed to writing and editing of this manuscript. Y.H., M.X. and X.-J.L. researched data for the article and contributed to the discussion of content and writing. M.Y., Y.T., L.L., J.W. and X.-J.L. researched data for the article. G.X., J.L. and T.X. contributed to reviewing and editing the manuscript. Y.H., W.G. and X.-J.L. contributed to the discussions and writing, reviewing and editing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Bioengineering thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Japan Society for the Promotion of Science (JSPS): https://www.jsps.go.jp/
National Institutes of Health (NIH): https://www.nih.gov/
National Natural Science Foundation of China (NSFC): https://www.nsfc.gov.cn/
National Science Foundation (NSF): https://www.nsf.gov/
United Kingdom Research and Innovation (UKRI): https://www.ukri.org/
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, Y., Huang, Y., Xie, M. et al. Immunoregulatory nanomedicine for respiratory infections. Nat Rev Bioeng 2, 244–259 (2024). https://doi.org/10.1038/s44222-023-00131-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44222-023-00131-8