Abstract
There is long-standing controversy as to whether suicide risk in those who have survived a traumatic event is highest when the severity of the survivors’ psychiatric condition is worst or when they begin to recover. To tackle this problem, we extracted psychiatric conditions from an online cohort of Japanese participants during the COVID-19 pandemic, at five time points (T1–T5). For 12,578 responses from 3,815 participants (mean age 47.1 years; 46.8% women), 3,508 psychiatric conditions were extracted in T1, 2,680 in T2, 2,562 in T3, 2,022 in T4 and 1,806 in T5. We then investigated whether extracted conditions could predict suicide rates in the full Japanese population in a time-specific manner. We found that COVID-19-related PTSD symptoms are associated with increased suicide rates (P = 3.0 × 10−6, Bayesian information criterion (BIC) = −23.69), and are of greater concern than depression (P = 7.6 × 10−4, BIC = −13.19) and anxiety symptoms (P = 5.9 × 10−3, BIC = −9.35). Furthermore, associations of psychiatric states with increased suicide rates are time specific (P = 0.011), suggesting that a population shows higher suicide risk when symptom severity is high. Event-related PTSD symptoms may help to identify groups at high risk of suicide and improve prevention policies.
Similar content being viewed by others
Main
Over 70% of all people confront a hazardous event, such as an earthquake, hurricane, violence, childhood abuse, war, traffic accident or pandemic, at some point in their lives1,2,3. An imperative in the context of hazardous events is suicide prevention. In 1893, suicide rates in England and Wales increased to 8.5 per 100,000, a 25% increase from baseline, during the Russian influenza4,5. Similarly, the severe acute respiratory syndrome outbreak in 2003 led to suicide rates of 37.46 per 100,000 among older adults in Hong Kong, a 32% increase from baseline6,7. In addition, after the 2011 Tohoku earthquake and tsunami, standardized suicide rates in 2014 increased to 24.5 per 100,000 in Fukushima Prefecture, a 14.3% increase from baseline8. These statistics suggest that between 1.7 and 9.1 individuals per 100,000 resort to suicide as a result of such events, underscoring the need to identify population groups at risk for suicide. However, analyzing risk factors in variables of this magnitude requires a large sample size, and this challenge becomes even more pronounced when attempting to capture short-term changes in such variables.
In contrast to most hazardous events, the coronavirus disease 2019 (COVID-19) pandemic affected mental health worldwide9. If this pandemic affected suicidal tendencies in a manner similar to that of previous hazardous events, we would have witnessed a large number of suicides. In the early phase of the pandemic, many experts suggested that an increase in suicides was likely10,11,12. In the real world, however, empirical data on suicides were more nuanced than expected. Some countries experienced an increase in suicides during the COVID-19 pandemic10,11,13,14,15. Others reported no increases or even decreases in suicides10,11,13,14,15. Even within the same country or region, increases or decreases in suicides varied among demographic groups16,17,18,19. Furthermore, despite population heterogeneity, temporal heterogeneity is equally important. As has been observed with previous disasters20,21, such as the 2011 Tohoku earthquake and tsunami8, there may be a delayed increase in suicides10,20. A delayed trend may be more pronounced in pandemics like COVID-19 because although the majority of people return to their normal lives as the pandemic wanes, some may be left behind, continuing to adhere to lifestyles altered by the pandemic. Such divergence can cause tremendous suffering for those left behind and, in extreme cases, result in suicide. Even in countries or populations that so far have shown no obvious increase in suicides during the COVID-19 pandemic10,15, suicide prevention remains a critical public health priority12. As heterogeneity in suicidal tendencies across populations cannot be explained by mere infection or mortality rates caused by the pandemic14,15, it is essential to understand the underlying mechanisms linking hazardous events to suicides for effective suicide prevention.
Over 90% of those who die by suicide have a psychiatric disorder at their time of death22,23,24,25,26,27. Psychiatric states, such as depression, anxiety and post-traumatic stress disorder (PTSD)12, are therefore likely to be key factors linking hazardous events to suicides12,28,29,30. Psychiatric conditions may be more informative for predicting suicide than suicidal ideation given that more than 60–70% of people who have died by suicide reported no suicidal ideation in assessments delivered within 30 days to 1 year of their deaths31.
In short, we hypothesize that people or groups with severe psychiatric conditions will show higher suicidal tendencies. However, patients with psychiatric disorders have historically been thought to show a heightened risk of suicide as they begin to recover, when their energy and motivation return, rather than when their symptom severities are the greatest32,33. Emil Kraepelin, professor of psychiatry at the University of Heidelberg, wrote in 1896, ‘Often, I saw precisely at that moment, suicide attempts that previously were not undertaken because of the lack of volition, despite great tedium of life’32,34. Our understanding of the temporal specificity of the association between psychiatric conditions and suicides is limited due to the difficulty in capturing short-term fluctuations in suicide rates, forcing previous studies to use suicidal ideation and incomplete suicide as proxy indicators, or to adopt cross-sectional designs35,36. Previous studies have not examined the temporal covariation between psychiatric states and suicidal tendencies during a single, large-scale, stressful event.
We hypothesized that event-related psychiatric states reliably predict increased suicide rates with high time specificity. Under this hypothesis, this study examined whether psychiatric states can reliably predict increased suicide rates and, if so, which psychiatric states can be used for such a prediction. Furthermore, we examined whether such predictability is temporally generalizable or time specific.
Results
Participants
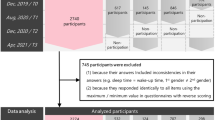
After excluding participants with inconsistencies in their answers (Fig. 1), the current analyses included 3,815 responders at T0 (data before the pandemic; December 2019), 3,508 responders at T1 (first data during the pandemic; August 2020), 2,680 responders at T2 (second data during the pandemic; December 2020), 2,562 responders at T3 (third data during the pandemic; April 2021), 2,022 responders at T4 (fourth data during the pandemic; August 2021) and 1,806 responders at T5 (fifth data during the pandemic; December 2021) (Table 1).
The procedures were decided based on the original survey (at T0 (*)). At that time, we aimed to collect data from enough individuals with high scores in PS use for a detailed survey. To do so, we performed a screening test (where participants reported demographics and PS scores). A total of 99,156 participants were enrolled in this screening test. These 99,156 participants were screened to include approximately equal numbers of individuals in each quintile relative to their PS score (assessed by the Japanese version of the Smartphone Addiction Scale Short Version). We also measured the Autism Spectrum Quotient (AQ) to capture participants’ autistic characteristics. Because CES-D, STAI and AQ include reversed questions, individuals were excluded if they responded identically to all items using only the maximum or minimum values in the questionnaires. As a result, we extracted 5,955 participants from the screening population. The data at T0 were not analysed in this study.
Descriptive and outcome data
Table 1 shows the information on severity and prevalence of PTSD, depression and anxiety in each age–sex group from the online participants at each time point, along with information on the actual and estimated suicide rate increase. The actual suicide rate increase of each group was based on the full population from which this sample was drawn (full population of Japan). The estimated suicide rate increase of each group was calculated based on the prevalence of PTSD in the same group.
Main results
Effects of psychiatric states on the suicide rate
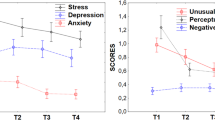
We first examined whether psychiatric states can predict increased suicide rates (and, if so, which psychiatric states can predict suicide rates) during a stressful event, the COVID-19 pandemic. These analyses were performed using severities of psychiatric scores (PTSD, depression and anxiety) for (1) T1 data, (2) T2–T5 data and (3) T1–T5 data, both at the individual and group level. In T1 data, our mixed-effect model analyses showed that the model based on PTSD scores had the smallest Bayesian information criterion (BIC) both in individual and group-level analyses compared with models based on depression or anxiety scores (Supplementary Fig. 1a,b; also see Supplementary Table 1 for the full statistics). We confirmed that adding depression scores and/or anxiety scores to PTSD scores (the psychiatric state that best predicted increased suicide rates in the T1 data) did not improve the model’s goodness of fit. These findings held in T2–T5 data (Supplementary Fig. 1c,d) and in T1–T5 data (at the group level, for the main effect of psychiatric scores for PTSD alone, beta coefficient (β) = 0.04, t-statistics (t) = 5.29, degrees of freedom (df) = 48, P = 3.0 × 10−6, BIC = −23.69; for depression alone, β = 0.04, t = 3.59, df = 48, P = 7.6 × 10−4, BIC = −13.19; for anxiety alone, β = 0.03, t = 2.88, df = 48, P = 5.9 × 10−3, BIC = −9.35; Fig. 2, see Supplementary Fig. 1e for the individual-level analysis). The difference in BIC (ΔBIC) was larger than 10 (PTSD versus depression, ΔBIC = 10.5; PTSD versus anxiety, ΔBIC = 14.3), signifying a very strong difference. Although data were taken from the same group, group-level psychiatric severities were highly coherent across independent cohorts (see ‘Other analyses’). Taken together, these findings attest to the robustness of the association of PTSD scores with suicide rate. In these models, neither confounder effects of depression nor those of anxiety can fully explain the association between PTSD and suicide increase.
Statistical tests were performed with a mixed-effects model analysis (two-tailed test). The BIC of each model is presented as a difference from the model based on PTSD symptoms alone (PTSD model). Positive values indicate that the PTSD model is superior to the model shown by each bar. ΔBIC values larger than 2 (dashed line) are considered significantly worse than the PTSD model, whereas differences larger than 10 (solid line) are considered ‘very strong’ differences. Filled bars represent models based on depression or anxiety and open bars represent models based on combinations of PTSD, depression and/or anxiety scores. This figure is based on data from T1–T5. The ΔBIC values for each bar from left to right are 10.50, 14.34, 3.85, 3.86 and 7.75.
The predictive power of estimated suicide risk
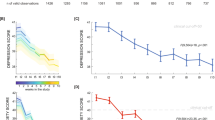
To further deepen our understanding of the association between PTSD and suicide risk, we estimated suicide risk (Srisk) based on known risk ratios for each sex (PTSDrisk of 3.96 for men and 6.74 for women)29 and PTSD prevalence based on our online survey (PTSDprev) (model specification, Srisk = (PTSDrisk − 1) × PTSDprev). These analyses were performed using the prevalences of PTSD scores for (1) T1 data, (2) T2–T5 data and (3) T1–T5 data at the group level. We performed mixed-effects regression analyses to show the association between estimated suicide risk and the actual suicide rate across each age and sex group. This showed the strong predictive power of the estimated suicide risk in the T1 data (β = 0.85, t = 6.3, df = 8, P = 2.3 × 10−4; Supplementary Fig. 2a). This effect held in T2–T5 data (β = 0.60, t = 5.5, df = 38, P = 2.8 × 10−6; Supplementary Fig. 2b) and in T1–T5 data (β = 0.63, t = 8.8, df = 48, P = 1.5 × 10−11; Supplementary Fig. 2c) (Fig. 3). Furthermore, effects of the estimated suicide risk were not compromised by adding sex, age and/or time points as mixed effects (Supplementary Fig. 2). According to the coefficient of determination (R2), 48% of the variability in the suicide rate during the pandemic across age groups and across time can be explained by variability of stress-related PTSD symptoms. These trends have also been observed in stratified analyses for each age group, suggesting that these effects were not only driven by stratified correlation (Supplementary Fig. 3). In other words, suicide risk is probably associated with psychiatric state. However, these analyses do not exclude the possibility that results in the base model are largely driven by stratified correlation, that is, the association between suicide risk and psychiatric trait in this context. In such a scenario, variability of suicide risk among groups should be explained by the variability of psychiatric conditions at any time point. There should be no time specificity in such an association.
Each circle and square represents the suicide rate increase estimated from PTSD probability (x axis) and the suicide rate increase (y axis) for each age group. Circles and squares represent female and male data, respectively. Colours represent data acquisition timing and the size of the shapes represents the number of online participants. Circles and squares of sizes representing 100, 300 and 500 individuals are shown for reference.
Time specificity of estimated suicide risk
To examine the time specificity of the estimated suicide risk, we performed cross-lagged relationship analyses using the above base model. Specifically, we examined associations of the estimated suicide risk with the ‘past’ or ‘future’, in addition to the ‘current’ suicide rate. This analysis was performed using prevalences of PTSD scores for T1–T5 data at the group level. The mixed-effect model analysis showed that the model predicting current suicide increase had the smallest BIC compared with those predicting past or future suicide increases (Supplementary Fig. 4). The ΔBIC was larger than 2, which is a statistically meaningful difference. Therefore, the estimated suicide risk best predicted the suicide rate in the same month from which the scores were extracted, rather than in a past or future month. Interestingly, the association between estimated suicide risk and actual suicidal tendency appeared to decrease sharply moving back in time, but more gradually moving forward (Fig. 4). This qualitative view was statistically supported by the generalized linear model. Specifically, including the interaction between time distance and direction (toward the future or the past) in the model significantly improved the prediction of the Pearson correlation (distance, β = −0.038, t = −2.3, df = 10, P = 0.047; interaction term, β = −0.063, t = −4.2, df = 10, P = 0.002, BIC = −12.1) compared with the prediction obtained without the interaction term (β = −0.07, t = −3.0, df = 11, P = 0.011, BIC = −3.7). The ΔBIC was larger than 2 (ΔBIC = 8.4), signifying a statistically meaningful difference. According to these analyses, the Pearson correlation shows a monthly decline of 0.10 when moving toward the past and declines by 0.038 when moving toward the future. This indicates that the Pearson correlation declines 2.65 times more rapidly toward the past than toward the future. This finding supports the idea that the increase in suicide rate at the population level does not precede exacerbations of psychiatric conditions; rather, the suicide rate increases in response to such exacerbations. Furthermore, it also suggests that effects of exacerbated psychiatric conditions on suicide are not instantaneous, but persist for several months.
The x axis denotes the month from which the actual suicide rate increase was extracted. The estimated increase in the suicide rate in the nth month was compared with the actual increase in the suicide rate in the n + xth month. The y axis represents Pearson correlation coefficients between estimated and actual suicide rate increases. Circles and squares represent female and male data, respectively. The black line indicates male and female data combined. The green (red) line represents the fitted line from the generalized linear models (two-tailed test) used to predict past (future) increases in the suicide rate. The solid (coloured dashed) line represents the fitted line based on the generalized linear model (two-tailed test) with (without) the interaction between distance and direction toward future and past.
Other analyses
In the test of selection bias based on our criteria, the estimated increase in the suicide rate showed a strong positive correlation between the screened and excluded populations (Pearson’s r = 0.89, P = 2.1 × 10−14; Supplementary Fig. 5a), indicating selection bias was unlikely to account for our results. In the test of the effect of residence, the estimated increase in the suicide rate showed a strong positive correlation between a population from Osaka and those from locations other than Osaka (Pearson’s r = 0.95, P = 4.5 × 10−21; Supplementary Fig. 5b), indicating that our findings are unrelated to residence.
Discussion
Key results
We showed that nearly half of the variability in suicide rate, regardless of age and sex, can be explained by a combination of COVID-19-related PTSD symptoms and previously reported sex differences in the suicide risk of PTSD. We further showed that the effects at T1 also held at T2–T5. Compared with other psychiatric symptoms, event-related PTSD symptoms appear to be reliable surrogate endpoints for increased suicide, outperforming depression or anxiety scores in predicting concurrent suicide risk. The most important finding was the strong temporal specificity of the association between symptoms and the suicide rate. This suggests, at least at a group level, that the population shows higher suicide risk when PTSD severity is higher. This finding provides a new avenue in research and prevention of suicide risk at the population level.
Interpretation
The high temporal specificity of the association found here indicates that reducing event-related PTSD symptoms could help prevent event-related suicides. Thus, event-related PTSD symptoms may work as a surrogate endpoint for suicide. Such a surrogate endpoint is beneficial for suicide prevention given the extremely low prevalence of suicides, usually less than 0.003% per month37. It is not realistic, or even possible, to observe such a large sample size in populations at risk, such as those who lost their jobs during the pandemic, those who got divorced during the pandemic and so on. Our data, however, suggest that measuring PTSD symptoms might be sufficient to identify populations at greater risk of suicide. If our findings apply to other traumatic events, we may be able to estimate the risk of suicide increase in other trauma-exposed populations (such as populations who witness genocide or who have experienced abuse) at given time points, that is, soon after the trauma, 1 year after trauma and so on. Policies and efforts to reduce PTSD severity within populations, or for individuals, are expected to reduce the overall suicide risk. Although further clarifications are needed to draw definitive conclusions, individuals at risk of suicide might be identifiable based on validated questionnaires in various settings, such as clinics, agencies and online consultations. Individuals identified through these channels should be guided to official clinical settings and given empirically validated treatments focused on PTSD, such as early intervention strategies38.
Our approach is agnostic as to whether COVID-19-related PTSD symptoms are the primary reason for suicides of those who resorted to suicide due to the pandemic. Risk factors for suicide typically act additively or synergistically, that is, patient risk levels increase with the number of risk factors33. In such a scenario, even if suicides in a given population increased in proportion to the severity of COVID-19-related PTSD symptoms in that population, it is possible that COVID-19-related PTSD symptoms were not the primary reason for the suicides. These symptoms may have raised the likelihood of suicidal decision-making depending on other primary reasons, such as economic strain, social isolation and physical disorders. Regardless of the primary reason, it is possible that decreasing severe PTSD symptoms (a candidate warning sign of potential suicide susceptibility) may reduce suicide risk.
Limitations
Several limitations should be considered. First, PTSD scores based on online surveys are sometimes higher than those observed in other types of surveys19,39, which may also explain the relatively high prevalence of COVID-19-related PTSD diagnoses in our online populations (5.3–34.6%) and in previous online research (7–35.6%)40,41. Consequently, estimated numbers of suicides based on PTSD scores are higher than actual numbers. It is important to note that although our data support the reliability of estimated numbers of suicides as ratio scales, raw values are likely to be overestimated. Second, we relied on self-report measures to evaluate psychiatric conditions from participants online, which have lower accuracy compared with clinician-administered diagnostic interviews. In particular, depression and anxiety were assessed with less-validated questionnaires compared with that used for PTSD. This may explain why these questionnaires did not capture more variance in suicide rates than was obtained from the questionnaire about PTSD symptoms. Third, our correlational approach prevents us from drawing conclusions about causality. It is possible that an unmodeled external factor could explain the strong correlation between COVID-19-related PTSD symptoms. Further clarification must be obtained on replicability and causality of the reported associations and whether these group-level findings can be applied at the individual level.
Generalizability
Global surveys with similar approaches could help to better explain reasons behind differences in suicide rate changes across countries, leading to more effective prevention of suicide worldwide. It may be possible to generalize these findings to other large-scale, long-lasting, stressful events.
In summary, we found that COVID-19-related PTSD symptoms at given points in time can predict concurrent suicide increases. Importantly, the associations between PTSD symptoms and suicide decrease only gradually with time, making it possible to take action for identified groups at risk of suicide. Further research based on our findings may help governments and agencies to focus prevention resources on groups at high risk of suicide, especially groups showing higher PTSD symptoms.
Methods
Study design
This study examined the association between psychiatric states and changes in suicide rates during the COVID-19 pandemic in Japan, which experienced a tremendous increase in suicide that varied greatly across gender and age groups14,42. Cross-sectional psychiatric states at multiple points in time were estimated through online questionnaires. Specifically, we performed real-time, online monitoring of a large online cohort immediately before the pandemic and at five time points during the COVID-19 pandemic. The online surveys were conducted six times with the same population: once before the pandemic (December 2019; T0) and five times during the pandemic (T1 in August 2020, T2 in December 2020, T3 in April 2021, T4 in August 2021 and T5 in December 2021). Note that, for the purpose of this article, only time points during the pandemic (T1–T5) were analysed.
Setting
This work is part of a larger online survey on problematic smartphone (PS) use, which was approved by the Ethics Committee of the Advanced Telecommunications Research Institute International. Details of trajectories of psychiatric states and demographic data have been previously published43,44. The study was originally planned in 2019 before the COVID-19 pandemic, and was later expanded to examine the psychiatric impact of COVID-19. Given the real-time aspect of the pandemic, we compared three psychiatric conditions in their predictability of suicide increase using the T1 data as soon as they were collected (also see ref. 45) Then, for all subsequent analyses using T2–T5 data, we included in the model only the psychiatric condition with the highest predictability. This approach ensured the model was fixed with the initial T1 data during the pandemic and T2–T5 data points could be considered as real-time data (T2–T5). Therefore, all analyses were performed on T1 and T2–T5 separately and T1–T5 combined. The exception to this is the analyses of time specificity of the predictive power of estimated suicide risk because this analysis could not be done with T1 data alone.
Participants
From registrants of an online survey company (Macromill; https://monitor.macromill.com/) who were living in the Kansai region of Japan, 99,156 individuals were invited via email to participate in a screening for the original study. In that screening, participants reported their demographics and smartphone-related items, including PS use scores. The email contained information about informed consent, and completion of the questionnaire was taken to indicate participant consent. Of these 99,156 individuals, 5,955 were screened and recruited in December 2019 (T0), such that the population evenly included individuals belonging to each quintile of PS use scores. In response to the COVID-19 pandemic, we invited the volunteers to participate in follow-up online surveys containing additional questions about COVID-19-related PTSD symptoms, at T1–T5. Participants were excluded if (1) they contradicted their answers across items (for example, in one question they answered that they never drink, but in another question they answered that they sometimes drink) or across surveys (for example, age differs more than 2 years within 1 year surveys); and (2) they answered using only the maximum or minimum rating in questionnaires that include reverse items (for example, Center for Epidemiologic Studies Depression Scale (CES-D) and Form Y of the State–Trait Anxiety Inventory (STAI-Y); also see refs. 43,44). Figure 1 shows the flow diagram of the number and proportion of participants retained at each stage. In response to the findings in T1 data that PTSD symptoms are the most predictive of suicide, we collected COVID-19-related PTSD symptoms from those excluded via the above screening processes in the T2–T5 data. These data were used to examine the possibility of selection bias (see ‘Bias’).
Variables
Depression, anxiety and COVID-19-related PTSD scores were taken from the online survey, as were age and sex. Suicide numbers were extracted from the provisional database provided by the Ministry of Health, Labour and Welfare (MHLW) in Japan. Potential confounding factors include selection bias based on our criteria, effect of residence of our online participants and self-selection bias that participants were selected from online registries. Variables used in the mixed-effect analyses are listed in Supplementary Table 2.
Data sources and measurement
Following standard procedures46,47, we relied on self-administered questionnaires to measure COVID-19-related PTSD symptoms. We used the widely used 22-item Impact of Events Scale-Revised (IES-R)48 to assess PTSD symptoms. Note that in our online survey, PTSD symptoms were assessed specifically with respect to COVID-19, for example, ‘I thought about COVID-19 when I didn’t mean to.’ As is recommended48, we regarded an IES-R score >32 as probable PTSD. To assess depression symptoms, we used the CES-D49. CES-D comprises 20-items, with scores higher than 15 signifying probable depression. The STAI-S50 was used to assess state anxiety symptoms. STAI-S comprises 20 items, where scores higher than 40 or 41 denote probable anxiety disorder for men or women, respectively.
We extracted monthly suicide numbers from January 2019 to June 2022 from the provisional database provided by the MHLW in Japan (https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000140901.html; accessed 8 June 2023).
Bias
To exclude potential confounding factors due to selection bias based on our criteria, we compared the estimated increase of the suicide rate for each subgroup in the screened population (a total of 9,070 participants) with those in the excluded population (a total of 94,111 participants) in the T2–T5 data (see Fig. 1).
To test the effect of residence, the estimated increase of the suicide rate was compared for each subgroup of participants from Osaka (a total of 38,034 participants) with those from locations other than Osaka (a total of 56,077 participants) in the T2–T5 data. Of note, in August 2020, Osaka had the second-largest number of people with COVID-19 in Japan.
Study size
Due to characteristics of the observational study during the COVID-19 pandemic, study size was restricted to that of the original larger study. We conducted a post hoc power analysis using G*Power v.3.1.9.7 (Franz Faul; Kiel University) to check the adequacy of our sample size. Using the coefficient of determination in the main result based on stress-related PTSD symptoms (R2 = 0.48, α = 0.05) for a sample size of 50 (the number of age–sex groups), the statistical power (1 − probability of a type-II error) was more than 0.99.
Quantitative variables
Psychiatric variables
In the individual-level analysis, each individual had their own value for psychiatric status at each time point. In the group-level analysis, averages of depression, anxiety and COVID-19-related PTSD scores were taken from the data during the COVID-19 pandemic, that is, data from T1–T5, for each sex and age group.
Suicide rates
Using the national database, we calculated suicide rates during the COVID-19 pandemic (that is, 2020, 2021 and 2022) for each sex and age group (10 year bins) compared with suicide numbers a year before the pandemic (that is, 2019). Specifically, the suicide rate for each group in a specific month was defined as follows: the number of suicides in that group in the specific month of 2019 subtracted from that in the same month in 2020, 2021 or 2022 divided by the number of suicides in 2019. Suicide numbers were adjusted based on the corresponding population at that time. Each value was calculated for each group and was therefore used as if it were in the group-level analysis. In the individual-level analysis, each online participant was assigned one value of suicide rate corresponding to their age and sex. This value was used to explain across-participant heterogeneity.
Estimated suicide risk
The suicide risk in a given population was estimated from the prevalence of probable PTSD, according to the following equation:
where PTSDrisk is the risk ratio of suicide (PTSD:healthy)29 (3.96 for men and 6.74 for women) and PTSDprev is the frequency of probable PTSD diagnosis from our samples in a given population, that is, the rate at which the threshold, IES-R >32, was exceeded. This model was designed before acquisition of T2–T5 data45.
Statistical methods
Effects of psychiatric states on the suicide rate
To show associations between psychiatric states and suicide rate, we used psychiatric state data from an online survey (N = 3,508; T1 data). Specifically, we compared how well these different measures predict the impact of COVID-19 on suicide rate throughout the entire Japanese population (population of 125.9 million). We used mixed-effects models to test whether each of three psychiatric conditions could predict the suicide rate. In all models, psychiatric state, that is, PTSD, depression or anxiety, was considered a fixed effect, whereas sex was classified as a random effect (the model was specified as ‘Suicide Increase ~ 1 + PsychiatricScore + (1 | sex)’, where ‘~’ indicates the relation between the response and predictor variables). We used the BIC to compare model goodness of fit, with smaller values indicating better models. Traditionally, a ΔBIC value larger than 2 is considered a significant difference between models, whereas a difference larger than 10 is considered a very strong difference51. Among the three psychiatric states examined, we extracted the best psychiatric state with the highest performance in predicting the suicide rate in the T1 data. We further examined whether adding other psychiatric state(s) to the best psychiatric state improved the model goodness of fit. Finally, applying each state to the equation above, six models were examined for T1 data. With these models, we performed individual-level analysis and group-level analysis. In the group-level analyses, the number of online participants in each group was included as weight term. These analyses were first applied to data from the T1 epoch and to-be-examined models were defined. We then examined whether effects for T1 data held for T2–T5 data.
Testing the predictive power of estimated suicide risk
We performed mixed-effects regression analyses to show the association between estimated suicide risk and the actual suicide rate across each age and sex group. Analyses were weighted by the online population size at a given time point, that is, for each group. This model was defined as the ‘base model.’ Again, these analyses were applied to (1) T1 data, (2) T2–T5 data and (3) T1–T5 data. We examined whether addition of age, sex and time point in analyses (2) and (3) to the base model as random effects compromised the results of the analysis on the base model.
Time specificity of estimated suicide risk
To examine the time specificity of the estimated suicide risk, we performed cross-lagged relationship analyses using the above base model for T1–T5 data. Specifically, we examined associations of the estimated suicide risk with the past or future, instead of the current suicide rate. The past was defined as the previous x months from current time point (−5, …, −1), and future was defined as x months following the current time point (+1, …, +5). For example, for the estimated suicide risk for August 2020, the actual suicide rates in July, August and September 2020 were respectively defined as past (−1), present and future (+1) suicide rates. We also calculated the Pearson correlation to examine estimation accuracy for demonstration purposes. Our subsequent investigation sought to determine any disparity in the correlation trend toward past or future time points. Using generalized linear models, we examined whether temporal distance from the present could effectively forecast the Pearson correlation. The primary objective of this analysis was to evaluate whether incorporating an interaction term across time distance and direction for future versus past enhanced the model’s performance or remained inconsequential (model specification was Pearson correlation ~ 1 + distance + distance : direction). The main effect of direction was not included in the model because doing so differentiated the intercepts across the fitted lines toward the past and toward the future. Our focus was on examining the differential slopes across these directions while keeping the intercept, that is, the fitted value for the current time point, the same. Therefore, we only included direction as an interaction term in the model. We regarded the difference as statistically meaningful when the ΔBIC exceeded 2. Statistical analyses were performed using MATLAB v.R2019b.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The main summary statistics that support the findings of this study are available in the Supplementary Information. Owing to company cohort data-sharing restrictions, individual data cannot be publicly posted. However, data are available from the corresponding authors upon request and with permission of KDDI Corporation. Data requests should be sent to the corresponding authors and will be responded to within 21 days.
References
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M. & Nelson, C. B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 52, 1048–1060 (1995).
Koenen, K. C. et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol. Med. 47, 2260–2274 (2017).
Benjet, C. et al. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol. Med. 46, 327–343 (2016).
Smith, F. B. The Russian influenza in the United Kingdom, 1889–1894. Soc. Hist. Med. 8, 55–73 (1995).
Zortea, T. C. et al. The impact of infectious disease-related public health emergencies on suicide, suicidal behavior, and suicidal thoughts. Crisis 42, 474–484 (2021).
Cheung, Y. T., Chau, P. H. & Yip, P. S. F. A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 23, 1231–1238 (2008).
Chan, S. M. S., Chiu, F. K. H., Lam, C. W. L., Leung, P. Y. V. & Conwell, Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 21, 113–118 (2006).
Ohto, H., Maeda, M., Yabe, H., Yasumura, S. & Bromet, E. E. Suicide rates in the aftermath of the 2011 earthquake in Japan. Lancet 385, 1727 (2015).
McGinty, E. E., Presskreischer, R., Han, H. & Barry, C. L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 324, 93–94 (2020).
John, A., Pirkis, J., Gunnell, D., Appleby, L. & Morrissey, J. Trends in suicide during the COVID-19 pandemic. BMJ 371, m4352 (2020).
Wasserman, D., Iosue, M., Wuestefeld, A. & Carli, V. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry 19, 294–306 (2020).
McIntyre, R. S. & Lee, Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry 19, 250–251 (2020).
Ketphan, O., Juthamanee, S., Racal, S. J. & Bunpitaksakun, D. The mental health care model to support the community during the COVID-19 pandemic in Thailand. Belitung Nurs. J. 6, 152–156 (2020).
Tanaka, T. & Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 5, 229–238 (2021).
Pirkis, J. et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 8, 579–588 (2021).
Orellana, J. D. Y. & de Souza, M. L. P. Excess suicides in Brazil: inequalities according to age groups and regions during the COVID-19 pandemic. Int. J. Soc. Psychiatry 68, 997–1009 (2022).
Bray, M. J. C. et al. Racial differences in statewide suicide mortality trends in Maryland during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Psychiatry 78, 444–447 (2021).
Zheng, X.-Y. et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open 11, e045317 (2021).
Osváth, P. et al. Changes in suicide mortality of Hungary during the first year of the COVID-19 pandemic. Orv. Hetil. 162, 1631–1636 (2021).
Kõlves, K., Kõlves, K. E. & De Leo, D. Natural disasters and suicidal behaviours: a systematic literature review. J. Affect. Disord. 146, 1–14 (2013).
Kessler, R. C. et al. Trends in mental illness and suicidality after Hurricane Katrina. Mol. Psychiatry 13, 374–384 (2008).
Barraclough, B., Bunch, J., Nelson, B. & Sainsbury, P. A hundred cases of suicide: clinical aspects. Br. J. Psychiatry 125, 355–373 (1974).
Robins, E., Murphy, G. E., Wilkinson, R. H. Jr, Gassner, S. & Kayes, J. Some clinical considerations in the prevention of suicide based on a study of 134 successful suicides. Am. J. Public Health Nations Health 49, 888–899 (1959).
Rich, C. L. & Runeson, B. S. Mental illness and youth suicide. Am. J. Psychiatry 152, 1239–1240 (1995).
Isometsä, E. et al. Mental disorders in young and middle aged men who commit suicide. BMJ 310, 1366–1367 (1995).
Cavanagh, J. T. O., Carson, A. J., Sharpe, M. & Lawrie, S. M. Psychological autopsy studies of suicide: a systematic review. Psychol. Med. 33, 395–405 (2003).
Mann, J. J., Waternaux, C., Haas, G. L. & Malone, K. M. Toward a clinical model of suicidal behavior in psychiatric patients. Am. J. Psychiatry 156, 181–189 (1999).
Blair-West, G. W., Cantor, C. H., Mellsop, G. W. & Eyeson-Annan, M. L. Lifetime suicide risk in major depression: sex and age determinants. J. Affect. Disord. 55, 171–178 (1999).
Fox, V. et al. Suicide risk in people with post-traumatic stress disorder: a cohort study of 3.1 million people in Sweden. J. Affect. Disord. 15, 609–616 (2020).
Allgulander, C. Suicide and mortality patterns in anxiety neurosis and depressive neurosis. Arch. Gen. Psychiatry 51, 708–712 (1994).
Louzon, S. A., Bossarte, R., McCarthy, J. F. & Katz, I. R. Does suicidal ideation as measured by the PHQ-9 predict suicide among VA patients? Psychiatr. Serv. 67, 517–522 (2016).
Mittal, V., Brown, W. A. & Shorter, E. Are patients with depression at heightened risk of suicide as they begin to recover? Psychiatr. Serv. 60, 384–386 (2009).
American Psychiatric Association. Practice guideline for the assessment and treatment of patients with suicidal behaviors. Am. J. Psychiatry 160, 1–60 (2003).
Kraepelin, E. Clinical Psychiatry: A Text-book for Students and Physicians (Macmillan, 1915).
Melhem, N. M. et al. Severity and variability of depression symptoms predicting suicide attempt in high-risk individuals. JAMA Psychiatry 76, 603–613 (2019).
Garlow, S. J. et al. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress. Anxiety 25, 482–488 (2008).
Sher, L. Preventing suicide. QJM 97, 677–680 (2004).
Shalev, A. Y. et al. Prevention of posttraumatic stress disorder by early treatment: results from the Jerusalem Trauma Outreach And Prevention study. Arch. Gen. Psychiatry 69, 166–176 (2012).
Sagar, R., Chawla, N. & Sen, M. S. Is it correct to estimate mental disorder through online surveys during COVID-19 pandemic? Psychiatry Res. 291, 113251 (2020).
Di Crosta, A. et al. Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID-19 emergency. Front. Psychol. 11, 567367 (2020).
Ren, Y. et al. Public mental health under the long-term influence of COVID-19 in China: geographical and temporal distribution. J. Affect. Disord. 277, 893–900 (2020).
Yoshioka, E., Hanley, S. J. B., Sato, Y. & Saijo, Y. Impact of the COVID-19 pandemic on suicide rates in Japan through December 2021: an interrupted time series analysis. Lancet Reg. Health West. Pac. 24, 100480 (2022).
Oka, T. et al. Prevalence and risk factors of internet gaming disorder and problematic internet use before and during the COVID-19 pandemic: a large online survey of Japanese adults. J. Psychiatr. Res. 142, 218–225 (2021).
Oka, T. et al. Multiple time measurements of multidimensional psychiatric states from immediately before the COVID-19 pandemic to one year later: a longitudinal online survey of the Japanese population. Transl. Psychiatry 11, 573 (2021).
Chiba, T. et al. PTSD symptoms related to COVID-19 as a high risk factor for suicide—key to prevention. Preprint at medRxiv https://doi.org/10.1101/2020.12.15.20246819 (2020).
Wang, C. et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 87, 40–48 (2020).
Davico, C. et al. Psychological impact of the COVID-19 pandemic on adults and their children in Italy. Front. Psychiatry 12, 572997 (2021).
Weiss, D. S. in Cross-Cultural Assessment of Psychological Trauma and PTSD (eds Wilson, J. P. & Tang, C. S.-K.) 219–238 (Springer, 2007).
Radloff, L. S. The CES-D Scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401 (1977).
Spielberger, C. D. State-Trait Anxiety Inventory for Adults (STAI-AD) (PsycTESTS, 1983); https://doi.org/10.1037/t06496-000
Raftery, A. E. Bayesian model selection in social research. Sociol. Methodol. 25, 111–163 (1995).
Acknowledgements
This research was supported by a KDDI collaborative research contract (T.C., K.I., M.M., T.O., F.N., R.Y., T. Kubo, M.K. and A.C.). This work was also supported by the Innovative Science and Technology Initiative for Security grant number JPJ004596, ATLA (M.M., R.Y., M.K. and A.C.), the Ikegaya Brain-AI Hybrid ERATO grant (JPMJER1801) from the Japan Science and Technology Agency (T.O., T. Kubo, M.K. and A.C.) and AMED under grant number JP20dm0307008 (M.M., T.O., R.Y. and A.C.). We thank M. Nagata for data collection and organization. Beyond employment, the funder had no direct role in the study design, data collection and analysis, decision to publish or preparation of the article.
Author information
Authors and Affiliations
Contributions
T.C., K.I. and A.C. contributed to study conception and design. T.C., N.K., T.O., Y.M., T.H. and M.H. contributed to data acquisition. T.C., M.M., T.O., F.N., R.Y., T. Kubo and A.C. conducted statistical analyses. T.C., K.I., T.O., H.T., T. Kanazawa, S.B., T. Kubo, A.H., M.K. and A.C. contributed to interpretation of data. T.C., K.I. and M.M. drafted the first version of the article. T.C., M.M., T.O., N.K. and A.C. had full access to the data. All authors revised and approved the final version of the article. T.C. and A.C. take responsibility for the integrity of the work.
Corresponding authors
Ethics declarations
Competing interests
N.K., Y.M., T.H. and M.H. are employees of KDDI Research. The other authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Stuart Leske, Jennifer Stevens and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–5 and Tables 1 and 2.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chiba, T., Ide, K., Murakami, M. et al. Event-related PTSD symptoms as a high-risk factor for suicide: longitudinal observational study. Nat. Mental Health 1, 1013–1022 (2023). https://doi.org/10.1038/s44220-023-00157-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00157-2