Abstract
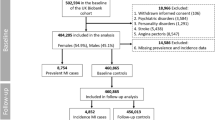
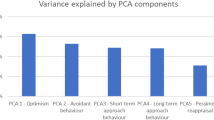
Personality has recently emerged as a critical determinant for multiple health outcomes. However, the evidence is less established for brain health, and the underlying mechanisms remain unclear. Here, utilizing data of 298,259 participants from the UK Biobank, five personality traits, including warmth, diligence, nervousness, sociability and curiosity, were constructed, and their relationships with brain disorders were examined with Cox regression and Mendelian randomization analyses. The results revealed consistent deleterious roles of nervousness, while the protective roles of warmth, diligence, sociability and curiosity in brain disorders were emphasized. Neuroimaging analyses highlighted the associations of personality traits with critical brain regions including the frontal cortex, temporal cortex and thalamus. Exploratory analyses revealed the mediating effects of neutrophil and high-density lipoprotein, indicating the contribution of inflammation and lipid metabolism to the associations between personality and brain health. This study provides a foundation for personality-oriented interventions in brain health, and it is necessary to validate our findings in other populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The main data used in this study were accessed from the publicly available UK Biobank Resource under application number 19542, which cannot be shared with other investigators. The GWAS data of brain disorders were retrieved from the exogenous population which is publicly available (dementia: https://gwas.mrcieu.ac.uk/datasets/finn-b-F5_DEMENTIA/, PD: https://gwas.mrcieu.ac.uk/datasets/ieu-a-812/, stroke: http://megastroke.org/download.html, schizophrenia: https://pgc.unc.edu/for-researchers/download-results/, bipolar affective disorder: https://pgc.unc.edu/for-researchers, and MDD: https://pgc.unc.edu/for-researchers/download-results/).
Code availability
Packages including survival 3.2, TwoSampleMR and lavaan 0.8 in R version 4.0.0 were used to perform Cox proportional hazards regression model, MR study and structural equation model, respectively. PLINK 2.0 was used to perform genome-wide association analysis and PRSice2 was used to calculate the PRS. Freesurfer v6.0 and FSL 6.0 were used to process the imaging data, and MATLAB 2018b was used to perform corresponding linear association analysis. Scripts used to perform the analyses are available at https://github.com/yuzhulineu/UKB_personality.
References
Optimizing Brain Health Across the Life Course: WHO Position Paper (World Health Organization, 2022).
World Mental Health Report: Transforming Mental Health for All (World Health Organization, 2022).
Taquet, M. et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry https://doi.org/10.1016/s2215-0366(22)00260-7 (2022).
Zhang, Y. R. et al. Modifiable risk factors for incident dementia and cognitive impairment: an umbrella review of evidence. J. Affect. Disord. 314, 160–167 (2022).
Ascherio, A. & Schwarzschild, M. A. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol. 15, 1257–1272 (2016).
Boehme, A. K., Esenwa, C. & Elkind, M. S. Stroke risk factors, genetics, and prevention. Circ. Res. 120, 472–495 (2017).
Aschwanden, D., Sutin, A. R., Luchetti, M., Stephan, Y. & Terracciano, A. Personality and dementia risk in England and Australia. GeroPsych 33, 197–208 (2020).
Sieurin, J. et al. Personality traits and the risk for Parkinson disease: a prospective study. Eur. J. Epidemiol. 31, 169–175 (2016).
Lonnqvist, J. E. et al. Premorbid personality factors in schizophrenia and bipolar disorder: results from a large cohort study of male conscripts. J. Abnorm. Psychol. 118, 418–423 (2009).
McAdams, D. P. & Olson, B. D. Personality development: continuity and change over the life course. Annu. Rev. Psychol. 61, 517–542 (2010).
Newton-Howes, G., Clark, L. A. & Chanen, A. Personality disorder across the life course. Lancet 385, 727–734 (2015).
Roberts, B. W. & Yoon, H. J. Personality psychology. Annu. Rev. Psychol. 73, 489–516 (2022).
John, O. & Srivastava, S. in Handbook of Personality: Theory and Research (eds Pervin, L. A. & John, O. P.) 102–138 (Guilford Press, 1999).
Aschwanden, D. et al. Is personality associated with dementia risk? A meta-analytic investigation. Ageing Res. Rev. 67, 101269 (2021).
Santangelo, G. et al. Personality and Parkinson’s disease: a meta-analysis. Parkinsonism Relat. Disord. 49, 67–74 (2018).
DeYoung, C. G. et al. Testing predictions from personality neuroscience. Brain structure and the big five. Psychol. Sci. 21, 820–828 (2010).
Valk, S. L. et al. Personality and local brain structure: their shared genetic basis and reproducibility. NeuroImage 220, 117067 (2020).
Pape, K., Tamouza, R., Leboyer, M. & Zipp, F. Immunoneuropsychiatry—novel perspectives on brain disorders. Nat. Rev. Neurol. 15, 317–328 (2019).
Hussain, G. et al. Lipids as biomarkers of brain disorders. Crit. Rev. Food Sci. Nutr. 60, 351–374 (2020).
Zhang, S., Lachance, B. B., Mattson, M. P. & Jia, X. Glucose metabolic crosstalk and regulation in brain function and diseases. Prog. Neurobiol. 204, 102089 (2021).
Luchetti, M., Barkley, J. M., Stephan, Y., Terracciano, A. & Sutin, A. R. Five-factor model personality traits and inflammatory markers: new data and a meta-analysis. Psychoneuroendocrinology 50, 181–193 (2014).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Malik, R. et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 50, 524–537 (2018).
Simón-Sánchez, J. et al. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat. Genet. 41, 1308–1312 (2009).
Pardiñas, A. F. et al. Common schizophrenia alleles are enriched in mutation-intolerant genes and in regions under strong background selection. Nat. Genet. 50, 381–389 (2018).
Stahl, E. A. et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat. Genet. 51, 793–803 (2019).
Wray, N. R. et al. Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat. Genet. 50, 668–681 (2018).
Terracciano, A., Stephan, Y., Luchetti, M., Albanese, E. & Sutin, A. R. Personality traits and risk of cognitive impairment and dementia. J. Psychiatr. Res. 89, 22–27 (2017).
Duberstein, P. R. et al. Personality and risk for Alzheimer’s disease in adults 72 years of age and older: a 6-year follow-up. Psychol. Aging 26, 351–362 (2011).
Terracciano, A. et al. Neuroticism and risk of Parkinson’s disease: a meta-analysis. Mov. Disord. 36, 1863–1870 (2021).
Bower, J. H. et al. Anxious personality predicts an increased risk of Parkinson’s disease. Mov. Disord. 25, 2105–2113 (2010).
Ishihara-Paul, L. et al. Prospective association between emotional health and clinical evidence of Parkinson’s disease. Eur. J. Neurol. 15, 1148–1154 (2008).
Jokela, M., Pulkki-Råback, L., Elovainio, M. & Kivimäki, M. Personality traits as risk factors for stroke and coronary heart disease mortality: pooled analysis of three cohort studies. J. Behav. Med. 37, 881–889 (2014).
Koorevaar, A. M. et al. Big Five personality and depression diagnosis, severity and age of onset in older adults. J. Affect. Disord. 151, 178–185 (2013).
Xia, J. et al. The relationship between neuroticism, major depressive disorder and comorbid disorders in Chinese women. J. Affect. Disord. 135, 100–105 (2011).
Simonsen, E. & Newton-Howes, G. Personality pathology and schizophrenia. Schizophr. Bull. 44, 1180–1184 (2018).
Gale, C. R. et al. Pleiotropy between neuroticism and physical and mental health: findings from 108 038 men and women in UK Biobank. Transl. Psychiatry 6, e791 (2016).
Zhang, F. et al. Causal influences of neuroticism on mental health and cardiovascular disease. Hum. Genet. 140, 1267–1281 (2021).
Terracciano, A. et al. Reply to: “Is conscientiousness related to the risk of Parkinson’s disease?”. Mov. Disord. 36, 2216 (2021).
Chida, Y. & Steptoe, A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom. Med. 70, 741–756 (2008).
Boehm, J. K. & Kubzansky, L. D. The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol. Bull. 138, 655–691 (2012).
Wickett, R., Muhlert, N. & Niven, K. The influence of personality on interpersonal emotion regulation in the context of psychosocial stress. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph20043073 (2023).
Bogg, T. & Roberts, B. W. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychol. Bull. 130, 887–919 (2004).
Klein, D. N., Kotov, R. & Bufferd, S. J. Personality and depression: explanatory models and review of the evidence. Annu. Rev. Clin. Psychol. 7, 269–295 (2011).
Bjørnebekk, A. et al. Neuronal correlates of the five factor model (FFM) of human personality: multimodal imaging in a large healthy sample. NeuroImage 65, 194–208 (2013).
Halassa, M. M. & Kastner, S. Thalamic functions in distributed cognitive control. Nat. Neurosci. 20, 1669–1679 (2017).
Szeszko, P. R. et al. Frontotemporal thalamic connectivity in schizophrenia and schizotypal personality disorder. Psychiatry Res. Neuroimaging 322, 111463 (2022).
Lisman, J. et al. Viewpoints: how the hippocampus contributes to memory, navigation and cognition. Nat. Neurosci. 20, 1434–1447 (2017).
Catani, M., Dell’acqua, F. & Thiebaut de Schotten, M. A revised limbic system model for memory, emotion and behaviour. Neurosci. Biobehav. Rev. 37, 1724–1737 (2013).
Zarkali, A. et al. Fiber-specific white matter reductions in Parkinson hallucinations and visual dysfunction. Neurology 94, e1525–e1538 (2020).
White, T. et al. Spatial characteristics of white matter abnormalities in schizophrenia. Schizophr. Bull. 39, 1077–1086 (2013).
Wardlaw, J. M., Smith, C. & Dichgans, M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 12, 483–497 (2013).
Yao, J. et al. The negative affectivity dimension of Type D personality associated with increased risk for acute ischemic stroke and white matter hyperintensity. J. Psychosom. Res. 160, 110973 (2022).
Rost, N. S. et al. White matter hyperintensity burden and susceptibility to cerebral ischemia. Stroke 41, 2807–2811 (2010).
Eisenberger, N. I., Inagaki, T. K., Mashal, N. M. & Irwin, M. R. Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain. Behav. Immun. 24, 558–563 (2010).
Zahodne, L. B., Kraal, A. Z., Zaheed, A., Farris, P. & Sol, K. Longitudinal effects of race, ethnicity, and psychosocial disadvantage on systemic inflammation. SSM Popul. Health 7, 100391 (2019).
Kiecolt-Glaser, J. K., Derry, H. M. & Fagundes, C. P. Inflammation: depression fans the flames and feasts on the heat. Am. J. Psychiatry 172, 1075–1091 (2015).
Irwin, M. R. & Vitiello, M. V. Implications of sleep disturbance and inflammation for Alzheimer’s disease dementia. Lancet Neurol. 18, 296–306 (2019).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
Glass, C. K. & Olefsky, J. M. Inflammation and lipid signaling in the etiology of insulin resistance. Cell Metab. 15, 635–645 (2012).
Camont, L., Chapman, M. J. & Kontush, A. Biological activities of HDL subpopulations and their relevance to cardiovascular disease. Trends Mol. Med. 17, 594–603 (2011).
Kroencke, L., Harari, G. M., Katana, M. & Gosling, S. D. Personality trait predictors and mental well-being correlates of exercise frequency across the academic semester. Soc. Sci. Med. 236, 112400 (2019).
Scheffer, D. D. L. & Latini, A. Exercise-induced immune system response: anti-inflammatory status on peripheral and central organs. Biochim. Biophys. Acta Mol. Basis Dis. 1866, 165823 (2020).
Gregor, M. F. & Hotamisligil, G. S. Inflammatory mechanisms in obesity. Annu. Rev. Immunol. 29, 415–445 (2011).
Sonar, S. A. & Lal, G. Blood–brain barrier and its function during inflammation and autoimmunity. J. Leukoc. Biol. 103, 839–853 (2018).
Huang, X., Hussain, B. & Chang, J. Peripheral inflammation and blood–brain barrier disruption: effects and mechanisms. CNS Neurosci. Ther. 27, 36–47 (2021).
Felger, J. C. Imaging the role of inflammation in mood and anxiety-related disorders. Curr. Neuropharmacol. 16, 533–558 (2018).
Dahlen, A. D., Miguet, M., Schioth, H. B. & Rukh, G. The influence of personality on the risk of myocardial infarction in UK Biobank cohort. Sci. Rep. 12, 6706 (2022).
Ruijter, M. J. T., Dahlen, A. D., Rukh, G. & Schioth, H. B. Association of diligence and sociability with stroke: a UK Biobank study on personality proxies. Front. Biosci. 27, 231 (2022).
Fry, A., Littlejohns, T., Sudlow, C., Doherty, N. & Allen, N. OP41 The representativeness of the UK Biobank cohort on a range of sociodemographic, physical, lifestyle and health-related characteristics. J. Epidemiol. Community Health 70, A26–A26 (2016).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Markon, K. E., Krueger, R. F. & Watson, D. Delineating the structure of normal and abnormal personality: an integrative hierarchical approach. J. Pers. Soc. Psychol. 88, 139–157 (2005).
Samuel, D. B. & Widiger, T. A. A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: a facet level analysis. Clin. Psychol. Rev. 28, 1326–1342 (2008).
Forgy, E. W. Cluster analysis of multivariate data: efficiency vs interpretability of classifications. Biometrics 21, 768–769 (1965).
Hartigan, J. A. & Wong, M. A. Algorithm AS 136: a K-means clustering algorithm. Appl. Stat. 28, 100–108 (1979).
Miller, K. L. et al. Multimodal population brain imaging in the UK Biobank prospective epidemiological study. Nat. Neurosci. 19, 1523–1536 (2016).
Brain imaging documentation. UK Biobank https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/brain_mri.pdf.
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Fischl, B. et al. Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 33, 341–355 (2002).
Griffanti, L. et al. BIANCA (Brain Intensity AbNormality Classification Algorithm): a new tool for automated segmentation of white matter hyperintensities. NeuroImage 141, 191–205 (2016).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScience 4, https://doi.org/10.1186/s13742-015-0047-8 (2015).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8, 1826 (2017).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Bulik-Sullivan, B. K. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Choi, S. W. & O’Reilly, P. F. PRSice-2: Polygenic Risk Score software for biobank-scale data. Gigascience https://doi.org/10.1093/gigascience/giz082 (2019).
Bowden, J. et al. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat. Med. 36, 1783–1802 (2017).
Bowden, J., Davey Smith, G., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40, 304–314 (2016).
Hartwig, F. P., Davey Smith, G. & Bowden, J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int. J. Epidemiol. 46, 1985–1998 (2017).
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525 (2015).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 7, e34408 (2018).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Modeling 6, 1–55 (1999).
Acknowledgements
This study was supported by grants from the STI2030-Major Projects (2022ZD0211600), National Natural Science Foundation of China (82071201, 82071997), Shanghai Municipal Science and Technology Major Project (2018SHZDZX01), Research Start-up Fund of Huashan Hospital (2022QD002), Excellence 2025 Talent Cultivation Program at Fudan University (3030277001), Shanghai Talent Development Funding for The Project (2019074), Shanghai Rising-Star Program (21QA1408700), 111 Project (B18015), ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute, the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, and Shanghai Center for Brain Science and Brain-Inspired Technology, Fudan University. We want to thank all the participants and researchers from the cohorts, including UKB, FinnGen, IPDGC, MEGASTROKE, PGC and CLOZUK.
Author information
Authors and Affiliations
Contributions
All authors had full access to the data in the study and accepted responsibility to submit them for publication. J.-T.Y. designed the study. Y.-R.Z. and Y.-T.D. conducted the primary analyses and drafted the manuscript. Y.-Z.L., R.-Q.Z., Y.-J.G., B.-S.W., W.Z. and K.K. contributed to imaging, SEM and genetic data analyses. J.-T.Y., W.C., J.-F.F., B.J.S., J.S. and A.D.S. critically revised the manuscript, and all authors approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks M. Hughes, A. Ibanez and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Tables 1–9.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, YR., Deng, YT., Li, YZ. et al. Personality traits and brain health: a large prospective cohort study. Nat. Mental Health 1, 722–735 (2023). https://doi.org/10.1038/s44220-023-00119-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00119-8