Abstract
AI tools intend to transform mental healthcare by providing remote estimates of depression risk using behavioral data collected by sensors embedded in smartphones. While these tools accurately predict elevated depression symptoms in small, homogenous populations, recent studies show that these tools are less accurate in larger, more diverse populations. In this work, we show that accuracy is reduced because sensed-behaviors are unreliable predictors of depression across individuals: sensed-behaviors that predict depression risk are inconsistent across demographic and socioeconomic subgroups. We first identified subgroups where a developed AI tool underperformed by measuring algorithmic bias, where subgroups with depression were incorrectly predicted to be at lower risk than healthier subgroups. We then found inconsistencies between sensed-behaviors predictive of depression across these subgroups. Our findings suggest that researchers developing AI tools predicting mental health from sensed-behaviors should think critically about the generalizability of these tools, and consider tailored solutions for targeted populations.
Similar content being viewed by others
Introduction
Mental healthcare systems are simultaneously facing a shortage of mental health specialty care providers and a large number of patients whose treatment needs remain unmet1,2. This service gap is driving research into AI-driven mental health monitoring tools, where sensed-behavioral data, defined as inferred behavioral data gathered by sensors and software embedded in everyday devices (e.g. smartphones, wearables), are repurposed to remotely monitor depression symptoms3,4,5,6,7. Sensed-behavioral data has also been referred to as personal, behavioral, or passive sensing data in other work7. AI tools that leverage sensed-behavioral data intend to near-continuously identify individuals experiencing elevated depression symptoms in-between clinical encounters and consequently deliver preventive care8. These tools can also be integrated into digital therapeutics to automate precision interventions9. Initial work showed that depression risk could be predicted from sensed-behavioral data at a similar accuracy to general practitioners10 in small populations5,11. More recent work shows that these AI tools predict depression risk at an accuracy only slightly better than a coin flip in larger, more diverse samples4,6,12,13. This prior work has not specifically explored why accuracy is reduced in larger samples, and it is unclear how to improve AI tools for clinical use.
In this work, we hypothesized that accuracy is reduced in larger, more diverse populations because sensed-behaviors are unreliable predictors of depression risk: sensed-behaviors that predict depression are inconsistent across demographic and socioeconomic (SES) subgroups14. We intentionally use the term reliability due to its importance in both a psychometric and AI context. In a psychometric context, reliability refers to the consistency of a tool, typically a symptom assessment, across different contexts (e.g. raters, time)14,15. In AI, reliability is related to generalizability, if an AI tool is consistently accurate in different contexts (e.g. different populations, over time, etc.)12. Given these definitions, researchers in AI fairness have argued that aspects of psychometric reliability are important in an AI context: similar inputs (e.g. sensed-behaviors) to an AI model should yield similar outputs (e.g. estimated depression risk)16.
In this paper, we adapt these ideas to study a specific aspect of reliability important for mental health AI tools deployed in large populations, i.e. if similar sensed-behaviors are consistently related to depression risk across different subgroups of individuals. We hypothesize that if the sensed-behaviors predictive of depression risk are inconsistent across subgroups, AI models that use sensed-behaviors to predict depression risk will be inaccurate because similar sensed-behavioral patterns will indicate different levels of depression risk for different subgroups. For example, imagine that mobility positively correlates with depression risk in subgroup A, and negatively correlates with depression risk in subgroup B. An AI model trained across subgroups using exclusively mobility data, blind to subgroup information as is typically the case in this literature3,4,5,17, will receive unreliable information – high mobility can simultaneously indicate both low and high depression risk – and will make incorrect predictions for one of the subgroups. We note upfront that in this manuscript we do not consider temporal aspects of reliability, though we acknowledge that this is important in discussions of psychometric reliability, specifically if the AI tool is consistently accurate for the same individual, with predictions made under similar conditions18.
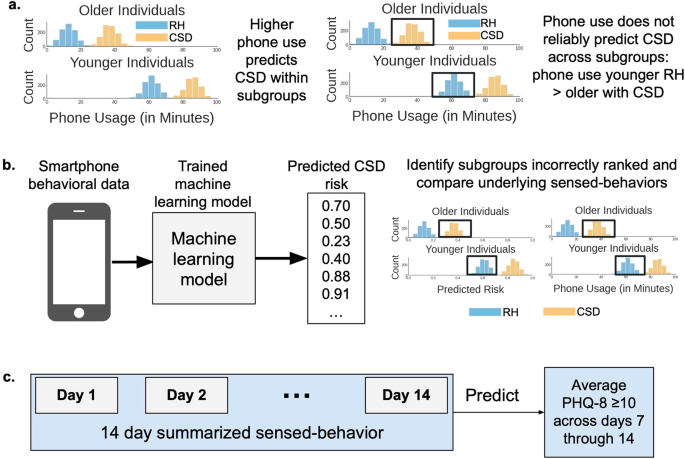
We tested our hypothesis by identifying population subgroups where a depression risk prediction tool underperformed, and then analyzed sensed-behavioral differences across these subgroups. We identified subgroups where the tool underperformed by measuring algorithmic ranking bias (hereafter referred to as “bias”), which measures the degree to which individuals experiencing depression from one subgroup (e.g. older individuals) are incorrectly ranked by the tool to be at lower risk than healthier individuals from other subgroups (e.g. younger individuals)19,20,21,22. Reliability was analyzed by measuring ranking bias because if individuals in large populations have inconsistent relationships between sensed-behaviors and mental health, behaviors that represent high depression risk for one subgroup may represent lower risk for another subgroup. For example, imagine an AI tool predicting that higher phone use increases depression risk. Studies23,24 show that younger individuals have higher phone use than older individuals. Thus, the AI tool may incorrectly rank older individuals with depression to be at lower risk than healthier younger individuals, decreasing model accuracy (Fig. 1a).
a We hypothesized that sensed-behaviors, like phone use, unreliably predict depression in larger populations because behaviors representing high depression risk for some subgroups (e.g. older individuals) may represent lower risk for other subgroups (e.g. younger individuals). RH is relatively healthy and CSD is clinically-significant depression. Histograms show simulated data describing the count of individuals (y-axis) with specific daytime phone usage (x-axis). Colors indicate individuals experiencing CSD (orange) versus RH (light-blue). Plots are split by age subgroups. Black boxes show that increased phone usage is not a reliable predictor of depression because RH younger individuals have higher phone use than CSD older individuals. b The analysis pipeline. Behavioral data from smartphones and mental health outcomes collected during a U.S.-based NIMH-funded study3,25,26,27,28,29 were used to train and validate AI models that predicted depression symptom risk from the behavioral data. We then measured algorithmic ranking bias in the developed tool to identify subgroups where the predicted CSD risk was incorrectly ranked lower than RH subgroups, and compared sensed-behaviors across subgroups where algorithms underperformed. c Similar to prior work3,25, 14 days of sensed-behavioral data were used to predict whether the PHQ-8 value across each weekly reported period indicated clinically-significant depression symptoms (PHQ-8 ≥ 1033).
Against this backdrop, we developed an AI tool that estimated depression symptom risk using behavioral data collected from individuals’ smartphones, using similar sensed-behaviors and outcome measures from recent work3,4,5,13,25 (Fig. 1b). The data used to develop and analyze the AI tool was collected during a U.S.-based National Institute of Mental Health (NIMH)-funded study3,25,26,27,28,29, one of the largest, most geographically diverse studies of its kind. We then measured bias across attributes including age, sex at birth, race, family income, health insurance, and employment to identify subgroups where the tool underperformed. We studied these specific attributes because of known behavioral differences across demographic and SES subgroups23,24,30,31,32 that could impact the reliability of the developed AI tool. Finally, we interpreted why the tool underperformed by identifying inconsistencies between the AI tool and sensed-behaviors predicting depression across subgroups. A summary of this analysis can be found in Fig. 1.
Results
Data collection
We analyzed data from a U.S.-based, NIMH-funded study conducted from 2019–2021 to identify associations between behavioral data collected from smartphones and depression symptoms3,25,26,27,28,29. Smartphone sensed-behavioral data on GPS location, phone usage (timestamp of screen unlock), and sleep were near-continuously collected from participants across the United States for 16 weeks and the PHQ-8, a self-reported measure of two week depression symptoms33,34 frequently used in mental health research3,5,25,27, was administered multiple times a week every three weeks (on weeks 1, 4, 7, …, known as weekly reporting periods). Sensed-behaviors were summarized over two weeks to align with collected PHQ-8 depression symptoms for prediction (see Table 1). For example, sensed-behaviors collected during weeks 3 and 4 were summarized to predict PHQ-8 responses collected during week 4.
Table 2 summarizes the data used for analysis. 3900 samples were analyzed from 650 individuals, a large cohort and sample size compared to most studies to date analyzing associations between sensed-behaviors and mental health4,5,25,35,36. A sample was a set of sensed-behaviors, summarized over 2 weeks, corresponding to the average PHQ-8 response collected during a single weekly reporting period. 46% of the average self-reported PHQ-8 values were ≥10, indicating clinically-significant depression (CSD)33. The majority of participants were relatively young to middle aged (75% 25 to 54 years old), female (74%), white (82%), middle to high income (61% annual family income ≥$ 40,000), insured (93%) and employed (62%). We focused our results on subgroups with at least 15 participants37. The sensed-behavior distributions across the population for each subgroup can be found in the supplementary materials.
Identifying subgroups where AI models underperform
The PHQ-8 asked participants to self-report depression symptoms experienced over 14 days, and PHQ-8’s were delivered multiple times throughout each weekly reporting period. We trained AI models using 14 days of smartphone sensed-behavioral data to predict if the average PHQ-8 value across each weekly reporting period (days 7 through 14, see Fig. 1c) indicated clinically-significant depression (CSD, PHQ-8 score ≥1033) symptoms. While the PHQ-8 asks participants to self-report 2 week depression symptoms, studies suggest that individual assessments may suffer from recency bias38 or indicate “briefly” elevated depression symptoms39. For this reason, PHQ-8 values were averaged over each weekly reporting period to predict a more stable estimate of self-reported symptoms.
Model performance was assessed by performing 5-fold cross-validation, partitioning on subjects, and predictions across folds were concatenated to calculate model performance. Similar to prior work4,6, within each cross-validation split, models were trained using data collected from 80% of the participants (520 participants), and the trained model was applied to predict CSD in the remaining 20% (130 participants). To analyze performance variability due to specific cross-validation splits, we performed 100 cross-validation trials, shuffling participants into different folds during each trial.
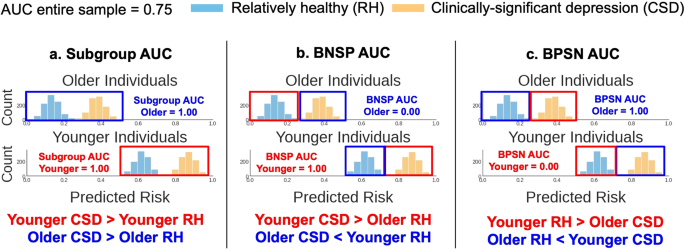
AI models output a predicted risk score from 0–1 of experiencing CSD. We used the predicted risk to calculate common ranking bias metrics20,21,22 (Fig. 2) across the subgroups in Table 2. These metrics were based upon the area under the receiver operating curve (AUC), which measured the probability models correctly predicted that CSD samples were ranked higher (in the predicted risk) than relatively healthy (RH, PHQ-8 < 10) samples. We first calculated the AUC within each subgroup (the “Subgroup AUC”). Note that equal Subgroup AUCs do not guarantee high AUC across an entire sample. For example, Fig. 2a shows simulated data where an algorithm correctly predicted CSD risk within subgroups, but younger individuals, compared to older individuals, have a higher overall predicted risk. Thus, across subgroups, healthy younger individuals may be incorrectly predicted to be at higher risk than older individuals experiencing CSD. Two additional performance metrics assessed such errors. Specifically, the background-negative-subgroup-positive, or BNSP AUC (Fig. 2b) measured the probability that individuals experiencing CSD (the “positive” label) from a subgroup were correctly predicted to have higher risk than RH (the “negative label”) individuals from other subgroups (“the background”), and the background-positive-subgroup-negative, or BPSN AUC (Fig. 2c), measured the probability RH individuals from a subgroup were correctly predicted to have lower risk than background individuals experiencing CSD.
We considered three metrics from prior work to assess algorithmic ranking bias20,21,22. The predicted risk is the probability, output by the AI tool, that individuals were experiencing clinically-significant depression (CSD). Histograms show simulated example predictions from an AI tool, describing the count of individuals (y-axis) who fell into a predicted risk bin (x-axis). Colors indicate individuals experiencing CSD (orange) versus RH (light-blue). Plots are split by age subgroups (younger/older). The AUC is the area under the receiver operating curve. The red and dark-blue boxes, and corresponding text color below each plot, highlight the subgroups compared for each metric. a The high Subgroup AUCs show that the predicted risk for individuals experiencing CSD was greater than the predicted risk for relatively healthy (RH) individuals within both age subgroups. But, this AI tool was biased to predict higher risk for younger individuals, overall, than older individuals. This bias is quantified using the (b) Background-Negative-Subgroup-Positive (BNSP) AUC and (c) Background-Positive-Subgroup-Negative (BPSN) AUC, which respectively show that younger individuals with CSD (“positive samples”) were correctly ranked higher (high BNSP) than RH (“negative samples”) samples from all other subgroups (older individuals, the “background”), but RH younger individuals were incorrectly ranked higher (low BPSN) than background samples with CSD. Older individuals show the complementary result (low BNSP, high BPSN). This bias reduces the model AUC when measured across the entire sample (assuming equal number of older and younger individuals, AUC = 0.75), compared to the AUC in each subgroup (1.00).
The highest performing AI model (a random forest, 100 trees, max depth of 10, balanced class weights, see methods) achieved a median (95% confidence interval, CI) AUC of 0.55 (0.54 to 0.57) across trials. Note that this low AUC was expected: it is comparable to the cross-validation performance of similar depression symptom prediction tools developed in larger, more diverse populations4,6,13, and motivates the objective of this work to study the reliability of these tools in larger populations.
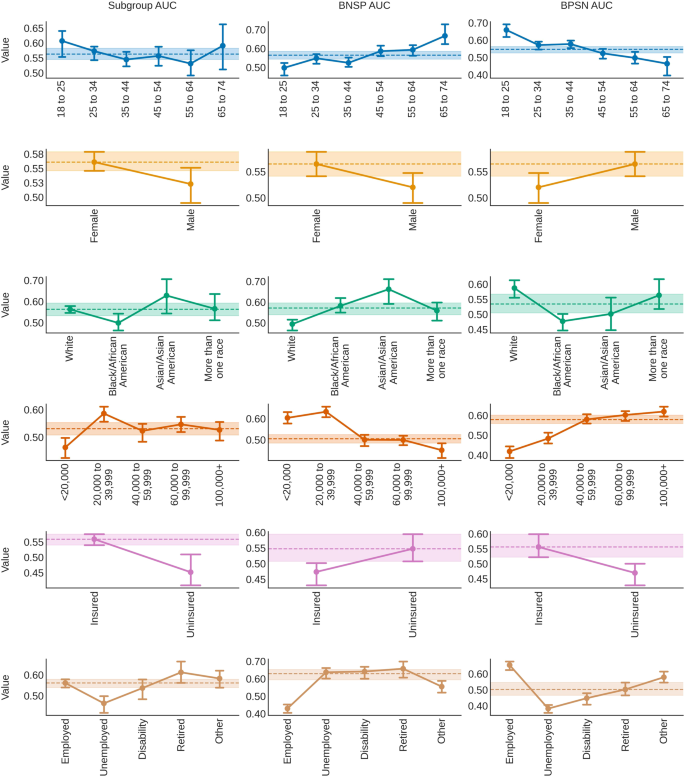
Figure 3 shows the model results by each metric across subgroups. The Subgroup AUC was lower for males (median, 95% CI 0.52, 0.49 to 0.55), Black/African Americans (0.50, 0.46 to 0.54), individuals from low income families (<$ 20,000, 0.46, 0.43 to 0.50), uninsured (0.45, 0.41 to 0.51), and unemployed (0.46, 0.42 to 0.50) individuals, compared to the median subgroup AUC for each attribute (e.g. “Sex at Birth”) across trials. The BNSP AUC increased with age (from 0.50, 0.46 to 0.52 for 18 to 25 year olds, to 0.67, 0.62 to 0.73 for 65 to 74 year olds), but decreased with family income (from 0.60, 0.58 to 0.63 for individuals from <$ 20,000 income families, to 0.45, 0.42 to 0.48 for individuals from $ 100,000+ income families). Individuals who were White (0.49, 0.46 to 0.52), male (0.52, 0.49 to 0.55), insured (0.47, 0.43 to 0.50), employed (0.43, 0.41 to 0.45), or identified with an “Other” type of employment (0.55, 0.52 to 0.59) also had lower BNSP AUC, compared to the median BNSP AUC for each attribute.
Bias was assessed by measuring the area under the receiver operating curve comparing positive (clinically-significant depression, CSD) and negative (relatively healthy, RH) samples within subgroups (Subgroup AUC, left column), subgroup positive samples to negative samples from all other subgroups, called “the background” (background-negative-subgroup-positive, or BNSP AUC, middle column), and subgroup negative samples to background positive samples (background-positive-subgroup-negative, or BPSN AUC, right column)20,22. Point values indicate the median value across trials. Error bars show 95% confidence intervals (2.5 and 97.5 percentiles). Dotted lines and shaded areas show the distribution (median and 95% confidence intervals) of either the median (if >2 subgroups) or highest performing subgroups across trials.
The BPSN AUC findings showed complementary trends: RH older individuals (e.g. 65 to 74, 0.46, 0.40 to 0.50), unemployed (0.38, 0.36 to 0.41), uninsured (0.47, 0.43 to 0.50), Black/African American (0.48, 0.45 to 0.50), females (0.52, 0.49 to 0.55), and individuals coming from lower income families (e.g. <$ 20,000 0.42, 0.39 to 0.44) had a lower BPSN AUC. Results were reasonably consistent across different types of models, within subgroup base rates (% samples with PHQ-8 ≥ 10) were sometimes, but not always, associated with the BNSP/BPSN AUC, and subgroup sample size did not appear to be associated with the Subgroup AUC (see supplementary materials).
Isolating the effects of subgroup membership
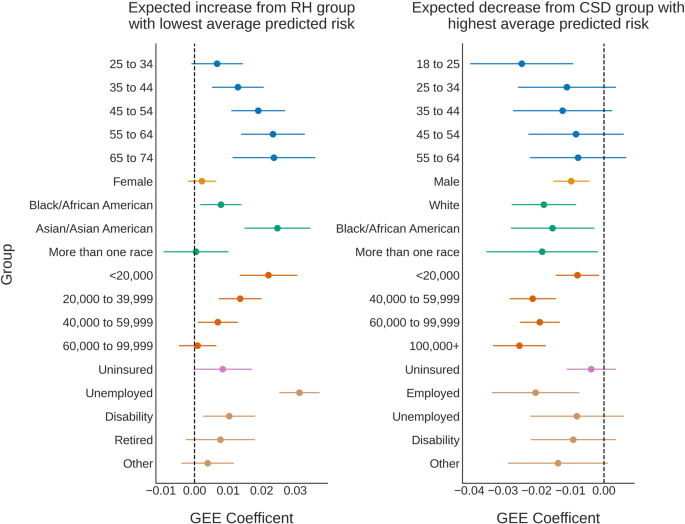
We wished to account for intersectional identities (e.g. female and employed) and isolate the effect of subgroup membership on model underperformance. For an ideal classifier, the predicted risk would be low for RH subgroups, and high for CSD subgroups. In addition, we would expect subgroups with higher base rates (% of samples with PHQ-8 ≥ 10) to have a higher average predicted risk. We thus modeled expected differences from subgroups with either the lowest (for RH) or highest (for CSD) average risk across trials. Generalized estimating equations (GEE, exchangeable correlation structure)40, a type of linear regression, was used to estimate the average effect of subgroup membership on the predicted risk after controlling across all other attributes. GEE was used instead of linear regression to correct for the non-independence of repeated samples across trials40.
The regression results can be found in Fig. 4. The RH individuals with the lowest average predicted risk were 18 to 25 years old, male, White, had a family income of $ 100,000 + , were insured, and employed. The predicted risk was expected to be higher than these subgroups (95% CI lower-bound >0) for RH individuals who were older than 34 (e.g. for 65 to 74 year olds, mean, 95% confidence interval 0.02, 0.01 to 0.04), identified as Asian/Asian American (0.02, 0.01 to 0.03), Black/African American (0.01, 0.00 to 0.01), came from <$ 60,000 income families (e.g. for <$ 20,000, 0.02, 0.01 to 0.03), were unemployed (0.03, 0.03 to 0.04), and/or on disability (0.01, 0.00 to 0.02).
For an ideal classifier, the predicted risk would be low for relatively healthy (RH) individuals, and high for individuals with clinically-significant depression (CSD). We thus modeled expected differences from the subgroups with either the lowest (for RH, left) or highest (for CSD, right) average predicted risk across trials. Subgroup effects were calculated using generalized estimating equations (GEE)40, a type of linear model, to analyze the average effect of subgroup membership on the predicted risk, controlling across all attributes. GEE accounted for the non-independence of repeated samples across trials40. Separate regression models were created for each outcome (RH, CSD) to remove the effects of the subgroup base rate. Points represent the GEE coefficient (expected effect), and error bars are 95% confidence intervals around the estimated effect. Dotted vertical lines highlight an expected subgroup effect of 0.
For individuals who were experiencing CSD, models predicted the highest average risk for 65 to 74 year olds, Females, Asian/Asian Americans, individuals who came from families with incomes of $ 20,000 to $ 39,999, were insured, and/or retired. The predicted risk for individuals experiencing CSD was expected to be lower (95% CI upper-bound <0) if individuals were 18 to 25 (–0.02, –0.04 to –0.01), male (–0.01, –0.02 to –0.00), Black/African American (–0.02, –0.03 to –0.00), more than one race (–0.02, –0.03 to –0.00), White (–0.02, –0.03 to –0.01), came from any family with an annual income <$ 20,000 or ≥$ 40,000 (e.g. $100,000+ –0.03, –0.03 to –0.02), and/or were employed (–0.02, –0.03 to –0.01). Predicted risk distributions often overlapped across subgroups with higher or lower risk, though there were general trends across subgroups (e.g. the predicted risk increased with age and unemployment in RH individuals, and risk decreased with income level for both CSD and RH individuals, see Fig. 4 for more details).
Interpreting sensed-behaviors
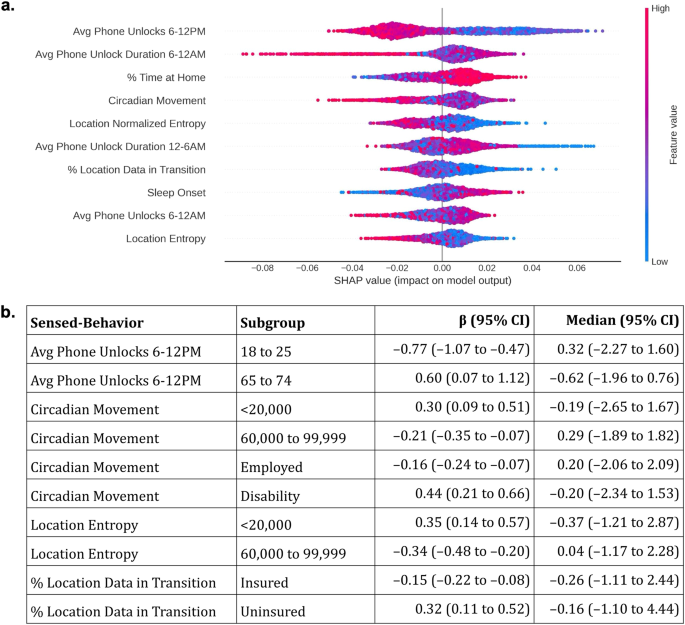
We hypothesized that models underperformed because sensed-behaviors predictive of CSD were inconsistent across subgroups. We thus conducted an analysis to understand differences between how AI tools predicted CSD risk and the different relationships between sensed-behaviors and CSD across subgroups. First, we retrained the AI model on the entire data, and used Shapley additive explanations (SHAP)41 to interpret how the AI tool predicted CSD risk from sensed-behaviors. We then compared SHAP values with coefficients from explanatory logistic regression models estimating how subgroup membership affected the relationship between each sensed-behavior and depression.
We found different relationships between the SHAP values (Fig. 5a) and sensed-behaviors associated with CSD across subgroups (Fig. 5b, comparisons across each attribute and feature can be found in the supplementary materials). For example, the AI tool predicted that higher morning phone usage (6–12PM) was generally associated with lower predicted depression risk. Higher morning phone usage decreased depression risk for 18 to 25 year olds (mean, 95% CI effect on depression, standardized units: –0.77, –1.07 to –0.47), but increased risk for 65 to 74 year olds (0.60, 0.07 to 1.12). Younger individuals, overall, also had higher morning phone use (standardized median, 95% CI 18 to 25 year olds: 0.32, –2.27 to 1.60) compared to older individuals (65 to 74 year olds: –0.62, –1.96 to 0.76).
a Shapley additive explanations (SHAP)41 were used to interpret how the AI tool predicted depression risk using sensed-behaviors. Sensed-behaviors are ordered, descending, on the y-axis by their average impact on the predicted risk (the “SHAP value”, x-axis). Only the top 10 sensed-behaviors with the highest average impact are listed, for space. Colors dictate whether a higher sensed-behavior “feature” value (red) is associated with higher or lower predicted risk. For example, higher average (“Avg”) phone unlocks from 6–12 PM were generally associated with lower predicted risk. Averages and deviations summarize sensed-behaviors over 14 days (see Fig. 1c). b Example coefficients (β, 95% CI, standardized units) from explanatory logistic regression models estimating the associations between sensed-behaviors and depression across subgroups, as well as the median and 95% CI of the sensed-behavior distribution. Full coefficients and statistics can be found in the supplementary materials.
Figure 5a also shows that specific mobility features, including the circadian movement (regularity in 24 hour movement), location entropy (regularity in travel to unique locations), and the percentage of collected GPS samples in transition (approximated speed >1 km/h) were often associated with lower predicted CSD risk. Circadian movement decreased CSD risk for employed individuals (–0.16, –0.24 to –0.07), but increased CSD risk for individuals who were on disability (0.44, 0.21 to 0.66). Circadian movement and location entropy also decreased depression risk for individuals from middle income ($ 60,000 to $ 99,999) families (circadian movement: –0.21, –0.35 to –0.07; location entropy: –0.34, –0.48 to –0.20), but increased risk for individuals from low income (<$ 20,000) families (circadian movement: 0.30, 0.09 to 0.51; location entropy: 0.35, 0.14 to 0.57). Finally, a higher percentage of GPS samples in transition decreased depression risk for insured individuals (–0.15, –0.22 to –0.08), but increased risk for uninsured individuals (0.32, 0.11 to 0.52).
Discussion
In this study, we hypothesized that sensed-behaviors are unreliable measures of depression in larger populations, reducing the accuracy of AI tools that use sensed-behaviors to predict depression risk. To test this hypothesis, we developed an AI tool that predicted clinically-significant depression (CSD) from sensed-behaviors and measured algorithmic bias to identify specific age, race, sex at birth, and socioeconomic subgroups where the tool underperformed. We then found differences between SHAP values estimating how the AI tool predicted CSD from sensed-behaviors, and explanatory logistic regression models estimating the associations between sensed-behaviors and CSD across subgroups. In this discussion, we show how differences in sensed-behaviors across subgroups may explain the identified bias and AI underperformance in larger, more diverse populations.
Measuring bias showed that models predicted older, female, Black/African American, low income, unemployed, and individuals on disability were at higher risk of experiencing CSD (high BNSP, low BPSN AUC), and younger, male, White, high income, insured, and employed individuals were at lower risk of experiencing CSD (high BPSN, low BNSP AUC), independent of outcomes. Comparing SHAP values to explanatory logistic regression coefficients suggests why AI models incorrectly predicted depression risk. For example, our findings show that younger individuals had higher daytime phone usage than older individuals. Models predicted that higher daytime phone usage was associated with lower CSD risk (Fig. 5a), potentially explaining why younger individuals, overall, had lower predicted risk, and older adults had higher predicted risk (Fig. 3). Differences could be attributed to younger individuals using phones for entertainment and social activities that support well-being, while older individuals may prefer to use their phones for necessary communication or information gathering23.
In another example, the model predicted that mobility, measured through circadian movement, location entropy, and GPS samples in transition, was associated with lower CSD risk (see Fig. 5). Prior work has identified a negative association between these same mobility features and CSD5,25, suggesting that mobility decreases depression risk. While we found the expected negative associations across majority, higher SES ($ 60,000 to $ 99,999 family income, insured, and employed) subgroups, we found the opposite, positive association across less-represented lower SES (<$ 20,000 family income, on disability, uninsured) subgroups, potentially explaining the reduced model performance (lower Subgroup AUC) in these subgroups. There are many possible explanations for the identified differences in behavior. First, underlying reasons to be mobile (e.g. navigating bureaucracy to receive government payments) may increase stress for individuals who are lower income and/or on disability31, increasing depression risk. Second, the analyzed data was collected during the early-to-mid stages of the COVID-19 pandemic, when mobility for low SES essential workers may indicate work travel and increased COVID-19 risk, contributing to stress32 and depression. These findings suggest that sensed-behaviors approximating phone use and mobility used to predict depression in prior work3,4,5,6,25 do not reliably predict depression in larger populations because of subgroup differences.
While existing work developing similar AI tools has strived to achieve generalizability4,42, our findings question this goal. Instead, it may be more practical to improve reliability by developing models for specific, targeted populations43,44. In addition, it may be helpful to train AI models using both sensed-behaviors and demographic information. In prior work and this study, AI models were trained using exclusively sensed-behavioral data3,4,5,17. However, prior work suggests that models may not be more predictive even with added demographic information45. This shows that additional methods are needed to clearly define subgroups, beyond demographics, with more homogenous relationships between sensed-behaviors and depression symptoms.
Another method to improve reliability is to develop personalized models, trained on participants’ data over time6,46. While personalization seems appealing, researchers should ensure that personalized predictions are meaningful. For example, we experimented with personalized models using a procedure suggested from prior work46. The model AUC improved (0.68) compared to the presented results (0.55), but we achieved a higher AUC (>0.80) by developing a naive model re-predicting participants’ first self-reported PHQ-8 value for all future outcomes. Given at least one participant self-report is often needed for personalization, models should show greater accuracy than these naive benchmarks.
Even if accuracy improves, models can still be biased19,37, and it is important to consider the clinical and public health implications of using biased risk scores for depression screening. For example, more frequent exposure to stress47 contributes to higher rates of depression in lower SES populations48, but overestimating depression risk for healthy low SES individuals allocates mental health resources away from other individuals who need care. Similar issues persist for underestimating depression risk. For example, models predicted lower risk for males experiencing depression compared to healthier females (see Fig. 3). Males are less likely to seek treatment for their mental health than females49, and AI tools underestimating male depression risk may further reduce the likelihood that males seek care. Uncovering these biases are important before algorithmic tools are used in clinical settings.
To reduce these harms, researchers can use methods described in this and other work37 to identify subgroups where AI tools underperform by measuring bias. Resources could then be directed to develop new or retrain existing models for these subgroups. Simultaneously, clinical personnel using these tools can be trained to identify algorithmic bias and mitigate its effects50. In addition, depositing de-identified sensed-behavior and mental health outcomes data in research repositories could increase available data to analyze the reliability of AI tools12. Finally, our findings show the importance of developing AI tools using data from populations that have similar behavioral patterns to the populations where these tools will be deployed. More thorough reporting of model training data51, and monitoring AI tools in “silent mode”, in which predictions are made but not used for decision making52, could prevent AI tools developed in dissimilar populations from causing harm.
Finally, it is important to consider how the choice to classify depression symptom severity influenced our results, specifically choosing to predict binarized PHQ-8 values instead of raw PHQ-8 scores. Predicting binarized symptom scores is a fairly common practice in both the depression prediction literature3,4,5,17, as well as in the clinical AI literature, broadly53,54. This practice is motivated by an interest to use AI tools for near-continuous symptom monitoring, in which an action (e.g. follow-up by a care provider) is triggered at a specific elevated symptom threshold. This motivation may be difficult to realize if the field continues to use depression symptom scales as outcomes. As recent work shows, symptom scales do not produce categorical response distributions, with a clear decision boundary distinguishing individuals experiencing versus not experiencing symptoms14. Instead, responses tend to exist along a continuum14. It is also important to consider if subgroup differences affect the interpretation and self-reporting of depression symptom scales. Despite this consideration, prior work provides evidence that the PHQ-8 exhibits measurement invariance across demographic and socioeconomic subgroups55,56. Thus, it may be unlikely that the bias identified in this work was due to subgroup differences in self-reporting symptoms, but our findings could be partially attributed to the mistreatment of depression symptom scales as categorical in nature.
This work had limitations. First, we analyzed data from a single study, though the studied cohort was larger in size, geographic representation, and timespan compared to prior work. In addition, the study cohort was majority White, employed, and female, though we did not find that sample size was associated with classification accuracy. Only inter-individual variability was considered, not intra-individual variability, and thus these findings do not extend to longitudinal monitoring contexts, where changes in sensed-behaviors may indicate changes in depression risk. In addition, data was only analyzed from participants who provided complete outcomes data (participants who reported at least one PHQ-8 value during each of the 6 weekly reporting periods). Data was exclusively collected from individuals who owned Android devices, and only specific data types (GPS and phone usage) were analyzed. Only smartphone sensed-behaviors were analyzed, and data collected from other devices (e.g. wearables) and platforms (e.g. social media) were not analyzed. Finally, data collection took place from 2019–2021, when COVID-19 restrictions varied across the United States, which may influence our findings. Future work can examine if these results replicate over larger, more diverse cohorts, in both demographic and socioeconomic attributes, as well as the data collection devices and platforms. In addition, future work can explore if sensed-behaviors are reliable predictors of depression in longitudinal monitoring contexts, though recent work suggests that sensed-behaviors have low predictive power, even when used for longitudinal monitoring25.
In conclusion, we present one method to assess the reliability of AI tools that use sensed-behaviors to predict depression risk. Specifically we measured ranking bias in a developed AI tool to identify subgroups where the tool underperformed, and then we interpreted why models underperformed by comparing the AI tool to sensed-behaviors predictive of depression across subgroups. Researchers and practitioners developing AI-driven mental health monitoring tools using behavioral data should think critically about whether these tools are likely to generalize, and consider developing tailored solutions that are well-validated in specific, targeted populations.
Methods
Cohort
In this work, we performed a secondary analysis of data collected during a U.S.-based National Institute of Mental Health (NIMH) funded study. The motivation for this study was to identify smartphone sensed-behavioral patterns predictive of depression symptoms3,25,26,27,28,29. Participants were recruited from across the United States using social media, online advertisements, and an internally maintained registry of individuals interested in participating in digital mental health research. Participants were also recruited through Focus Pointe Global, a national research panel. Focus Pointe Global merged with the Schlesinger Group during data collection.
Eligible participants lived in the United States, could read/write English, and owned an Android smartphone and data plan. In addition, eligible participants with at least moderate depression symptom severity based upon the Patient Health Questionnaire-8 (PHQ-8) ≥ 10 were intentionally oversampled to create a sample with elevated depression symptoms. Individuals were excluded from the study if they self-reported a diagnosis of bipolar disorder, any psychotic disorder, shared a smartphone with another individual, or were unwilling to share data. Eligible participants were asked to provide electronic informed consent after receiving a complete description of the study. Eligible participants had the option to not provide consent, and could withdraw from the study at any point.
Consented participants downloaded a study smartphone application57 and completed a baseline assessment to self-report demographic and lifestyle information. The study application passively collected GPS location, sampled every 5 min, and smartphone interactions (screen unlock and time of unlock) for 16 weeks. Individuals completed depression symptom assessments every 3 weeks within the smartphone application (the PHQ-833,34). Data collection took place from 2019–2021, and all study procedures were approved by the Northwestern University Institutional Review Board (study #STU00205316).
Sensed-behavioral features
We calculated sensed-behavioral features from the collected smartphone data to predict depression risk. Following established methods from prior work3,5,25, we calculated GPS mobility features including the location variance (variability in GPS), number of unique locations, location entropy (variability in unique locations), normalized location entropy (entropy normalized by number of unique locations), duration of time spent at home, percentage of collected samples in-transition (participant moving at >1 km/h), and circadian movement (24 hour regularity in movement)5. We also calculated phone usage features from the screen unlock data42, including the duration of phone use and the number of screen unlocks each day and within four 6 hour periods (12–6 AM, 6–12 PM, 12–6 PM, 6–12 AM). Finally, we used a standard algorithm42,58 to approximate daily sleep onset and duration from screen unlock data.
Depression symptom classification
The PHQ-8 asks participants to self-report depression symptoms that occurred during the past 2 weeks. Symptoms are reported from 0 (not experiencing the symptom) to 3 (frequently experiencing the symptom). Scores are summed and thresholded to classify severity, where summed scores of 10 or greater indicate a higher likelihood of experiencing a clinically-significant depression33. We thus followed prior work5,25 to calculate sensed-behavioral features in the 2 week period up to and including each weekly PHQ-8 reporting period. Behavioral features were input into machine learning models to predict clinically-significant symptoms (PHQ-8 ≥ 10).
Data preprocessing
Screen unlock and sleep features were summarized to align with the PHQ-842. The average and standard deviation of each daily and 6 hour epoch feature were calculated across the 2 week prediction period, and the number of days with daily phone use and within each 6 hour epoch were summed. GPS features were directly calculated over the 2 weeks. As recommended by Saeb et al.5, skewed features were log-transformed. Missing data was filled using multivariate imputation59 and then standardized (mean = 0, standard deviation = 1) based upon each training dataset prior to being input into predictive models.
AI model training and validation
We trained machine learning models commonly used to predict mental health status from smartphone behavioral data including regularized (L2-norm) logistic regression (LR)3,5, support vector machines (SVM)4,60, and tree-based ensemble models including random forest (RF) and gradient boosting trees (GBT)3,42. We varied the strength of the LR and SVM regularization parameter (0.01, 0.1, 1.0), used a radial basis function SVM kernel, varied class balancing weights in the RF and SVM (unbalanced/balanced), varied the number of ensemble tree estimators (10, 100), depth (3, 10, or until pure), and the GBT learning rate (0.01, 0.1, 1.0) and loss (deviance and exponential). Non-logistic prediction models were calibrated using Platt scaling to approximately match the predicted risk to the proportion of individuals experiencing clinically-significant symptoms at each risk level61. Logistic regression models, as shown in prior work61, output calibrated probabilities. Models were implemented using the scikit-learn Python library62.
Multiple PHQ-8 surveys were administered each weekly reporting period (e.g. week 1, 4, 7, etc.). Survey scores in each reporting week were averaged to remove overlap between sensor and outcomes data. Data was analyzed from study participants who self-reported at least one PHQ-8 during each reporting week, resulting in 6 predictions per participant. Data from all other participants were removed (288 participants removed, 31% of 938 total, leaving 650 participants for analysis) to focus this analysis towards algorithmic bias due to subgroup differences rather than bias due to missing outcomes data.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
Sensed-behavioral data cannot be made publicly available due to potentially identifying information (e.g. GPS location) that may compromise participant privacy. De-identified self-reported data (the PHQ-8) will be made available through the NIMH Data Archive.
Code availability
A repository for all code used for analysis can be found at the following link: https://github.com/dadler6/reliability_depression_ml.
Reference
Cai, A. et al. Trends In mental health care delivery by psychiatrists and nurse practitioners in medicare, 2011–19. Health Aff. (Millwood) 41, 1222–1230 (2022).
Mohr, D. C. et al. Banbury forum consensus statement on the path forward for digital mental health treatment. Psychiatr. Serv. 6, 677–683 (2021).
Liu, T. et al. The relationship between text message sentiment and self-reported depression. J. Affect. Disord. 302, 7–14 (2022).
Xu, X. et al. GLOBEM: Cross-dataset generalization of longitudinal human behavior modeling. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 6, 190:1–190:34 (2023).
Saeb, S. et al. Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study. J. Med. Internet Res. 17, e175 (2015).
Meegahapola, L. et al. Generalization and personalization of mobile sensing-based mood inference models: an analysis of college students in eight countries. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 6, 176:1–176:32 (2023).
Mohr, D. C., Shilton, K. & Hotopf, M. Digital phenotyping, behavioral sensing, or personal sensing: names and transparency in the digital age. Npj Digit. Med. 3, 1–2 (2020).
Lee, E. E. et al. Artificial intelligence for mental health care: clinical applications, barriers, facilitators and artificial isdom. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 6, 856–864(2021).
Frank, E. et al. Personalized digital intervention for depression based on social rhythm principles adds significantly to outpatient treatment. Front. Digit. Health 4, 870522 (2022).
Mitchell, A. J., Vaze, A. & Rao, S. Clinical diagnosis of depression in primary care: a meta-analysis. The Lancet. 374, 609–619 (2009).
Wang, R. et al. Tracking depression dynamics in college students using mobile phone and wearable sensing. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2, 43:1–43:26 (2018).
Adler, D. A. et al. A call for open data to develop mental health digital biomarkers. BJPsych. Open 8, e58 (2022).
Müller, S. R. et al. Depression predictions from GPS-based mobility do not generalize well to large demographically heterogeneous samples. Sci. Rep. 11, 14007 (2021).
Fried, E. I., Flake, J. K. & Robinaugh, D. J. Revisiting the theoretical and methodological foundations of depression measurement. Nat. Rev. Psychol. 1, 358–368 (2022).
Beck, A. T. Reliability of psychiatric diagnoses: 1 a critique of systematic studies. Am. J. Psychiatry 119, 210–216 (1962).
Jacobs, A. Z. & Wallach, H. Measurement and fairness. In Proc. 2021 ACM Conference on Fairness, Accountability, and Transparency 375–385 (ACM, 2021).
Jacobson, N. C., Weingarden, H. & Wilhelm, S. Digital biomarkers of mood disorders and symptom change. Npj Digit. Med. 2, 1–3 (2019).
Boateng, G. O., Neilands, T. B., Frongillo, E. A., Melgar-Quiñonez, H. R. & Young, S. L. Best practices for developing and validating scales for health, social and behavioral research: a primer. Front. Public Health 6, 149 (2018).
Obermeyer, Z., Powers, B., Vogeli, C. & Mullainathan, S. Dissecting racial bias in an algorithm used to manage the health of populations. Science 366, 447–453 (2019).
Borkan, D., Dixon, L., Sorensen, J., Thain, N. & Vasserman, L. Nuanced Metrics for Measuring Unintended Bias with Real Data for Text Classification. In Companion Proceedings of The 2019 World Wide Web Conference 491–500 (ACM, 2019).
Kallus, N. & Zhou, A. The Fairness of Risk Scores Beyond Classification: Bipartite Ranking and the XAUC Metric. In Advances in Neural Information Processing Systems vol. 32 (Curran Associates, Inc., 2019).
Vogel, R., Bellet, A. & Clémençon, S. Learning fair scoring functions: bipartite ranking under ROC-based fairness constraints. In Proc. The 24th International Conference on Artificial Intelligence and Statistics 784–792 (PMLR, 2021).
Andone, I. et al. How age and gender affect smartphone usage. In Proc. 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct 9–12 (ACM, 2016).
Horwood, S., Anglim, J. & Mallawaarachchi, S. R. Problematic smartphone use in a large nationally representative sample: Age, reporting biases, and technology concerns. Comput. Hum. Behav. 122, 106848 (2021).
Meyerhoff, J. et al. Evaluation of changes in depression, anxiety, and social anxiety using smartphone sensor features: longitudinal cohort study. J. Med. Internet Res. 23, e22844 (2021).
Mohr, D. C. LifeSense: Transforming Behavioral Assessment of Depression Using Personal Sensing Technology. https://reporter.nih.gov/search/N6YCr94ZvkOVUNu1i5HNaQ/project-details/9982127 (2017).
Stamatis, C. A. et al. Prospective associations of text-message-based sentiment with symptoms of depression, generalized anxiety, and social anxiety. Depress. Anxiety 39, 794–804 (2022).
Meyerhoff, J. et al. Analyzing text message linguistic features: do people with depression communicate differently with their close and non-close contacts. Behav. Res. Ther. 166, 104342 (2023).
Stamatis, C. A. et al. The association of language style matching in text messages with mood and anxiety symptoms. Procedia Comput. Sci. 206, 151–161 (2022).
Greissl, S. et al. Is unemployment associated with inefficient sleep habits a cohort study using objective sleep measurements. J. Sleep Res. 31, e13516 (2022).
Iezzoni, L. I., McCarthy, E. P., Davis, R. B. & Siebens, H. Mobility difficulties are not only a problem of old age. J. Gen. Intern. Med. 16, 235–243 (2001).
Levy, B. L., Vachuska, K., Subramanian, S. V. & Sampson, R. J. Neighborhood socioeconomic inequality based on everyday mobility predicts COVID-19 infection in San Francisco, Seattle and Wisconsin. Sci. Adv. 8, eabl3825 (2022).
Kroenke, K. et al. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 114, 163–173 (2009).
Wu, Y. et al. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol. Med. 50, 1368–1380 (2020).
Opoku Asare, K. et al. Predicting depression from smartphone behavioral markers using machine learning methods, hyperparameter optimization and feature importance analysis: exploratory study. JMIR. MHealth UHealth. 9, e26540 (2021).
Corponi, F. et al. Automated mood disorder symptoms monitoring from multivariate time-series sensory data: getting the full picture beyond a single number. medRXiv https://doi.org/10.1101/2023.03.25.23287744 (2023).
Seyyed-Kalantari, L., Zhang, H., McDermott, M. B. A., Chen, I. Y. & Ghassemi, M. Underdiagnosis bias of artificial intelligence algorithms applied to chest radiographs in under-served patient populations. Nat. Med. 27, 2176–2182 (2021).
Aguilera, A., Schueller, S. & Leykin, Y. Daily mood ratings via text message as a proxy for clinic based depression assessment. J. Affect. Disord. 175, 471–474 (2015).
Horwitz, A. G., Zhao, Z. & Sen, S. Peak-end bias in retrospective recall of depressive symptoms on the PHQ-9. Psychol. Assess. 35, 378–381 (2023).
Ballinger, G. A. Using generalized estimating equations for longitudinal data analysis. Organ. Res. Methods 7, 127–150 (2004).
Lundberg, S. M. & Lee, S.-I. A unified approach to interpreting model predictions. arXiv https://doi.org/10.48550/arXiv.1705.07874 (2017).
Adler, D. A., Wang, F., Mohr, D. C. & Choudhury, T. Machine learning for passive mental health symptom prediction: Generalization across different longitudinal mobile sensing studies. PLoS One 17, e0266516 (2022).
Sperrin, M., Riley, R. D., Collins, G. S. & Martin, G. P. Targeted validation: validating clinical prediction models in their intended population and setting. Diagn. Progn. Res. 6, 24 (2022).
Mitchell, M. et al. Model cards for model reporting. arXiv https://doi.org/10.48550/arXiv.1810.03993 (2019).
Pratap, A. et al. The accuracy of passive phone sensors in predicting daily mood. Depress. Anxiety 36, 72–81 (2019).
Wang, R. et al. CrossCheck: toward passive sensing and detection of mental health changes in people with schizophrenia. In Proc. 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing 886–897 (ACM, 2016).
Williams, D. R., Mohammed, S. A., Leavell, J. & Collins, C. Race, socioeconomic status and health: complexities, ongoing challenges and research opportunities. Ann. N. Y. Acad. Sci. 1186, 69–101 (2010).
Everson, S. A., Maty, S. C., Lynch, J. W. & Kaplan, G. A. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity and diabetes. J. Psychosom. Res. 53, 891–895 (2002).
Chatmon, B. N. Males and mental health stigma. Am. J. Mens Health 14, 1557988320949322 (2020).
Rajkomar, A., Hardt, M., Howell, M. D., Corrado, G. & Chin, M. H. Ensuring fairness in machine learning to advance health equity. Ann. Intern. Med. 169, 866–872 (2018).
Gebru, T. et al. Datasheets for datasets. arXiv https://doi.org/10.48550/arXiv.1803.09010 (2020).
Wiens, J. et al. Do no harm: a roadmap for responsible machine learning for health care. Nat. Med. 25, 1337–1340 (2019).
Wong, A. et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern. Med. https://doi.org/10.1001/jamainternmed.2021.2626 (2021).
Adams, R. et al. Prospective, multi-site study of patient outcomes after implementation of the TREWS machine learning-based early warning system for sepsis. Nat. Med. 7,1455–1460 (2022).
Galenkamp, H., Stronks, K., Snijder, M. B. & Derks, E. M. Measurement invariance testing of the PHQ-9 in a multi-ethnic population in Europe: the HELIUS study. BMC Psychiatry. 17, 349 (2017).
Villarreal-Zegarra, D., Copez-Lonzoy, A., Bernabé-Ortiz, A., Melendez-Torres, G. J. & Bazo-Alvarez, J. C. Valid group comparisons can be made with the patient health questionnaire (PHQ-9): a measurement invariance study across groups by demographic characteristics. PLoS One 14, e0221717 (2019).
Audacious Software. Passive Data Kit. https://passivedatakit.org/ (2018).
Abdullah, S., Matthews, M., Murnane, E. L., Gay, G. & Choudhury, T. Towards circadian computing: ‘early to bed and early to rise’ makes some of us unhealthy and sleep deprived. In Proc. 2014 ACM International Joint Conference on Pervasive and Ubiquitous Computing 673–684 (ACM, 2014).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67 (2011).
Tseng, V. W.-S. et al. Using behavioral rhythms and multi-task learning to predict fine-grained symptoms of schizophrenia. Sci. Rep. 10, 15100 (2020).
Niculescu-Mizil, A. & Caruana, R. Predicting Good Probabilities With Supervised Learning. https://www.cs.cornell.edu/~alexn/papers/calibration.icml05.crc.rev3.pdf (2005).
Pedregosa, F. et al. Scikit-learn: Machine Learning in Python. https://www.jmlr.org/papers/v12/pedregosa11a.html (2018).
Acknowledgements
D.A. is supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-2139899, and a Digital Life Initiative Doctoral Fellowship. Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. Data collection was supported by NIMH Grant No. R01MH111610 to D.C.M. J.M. is supported by K08MH128640. C.A.S. is supported by T32MH115882. Computing costs were funded by a Microsoft Azure Cloud Computing Grant through the Cornell Center for Data Science for Enterprise and Society, awarded to T.C. T.C. and F.W. were also supported by a multi-investigator seed grant awarded from the Cornell Academic Integration program.
Author information
Authors and Affiliations
Contributions
D.A. conducted the analysis and wrote the draft manuscript. T.C., F.W., J.M., C.A.S. and D.C.M. provided supervisory support throughout the analysis. D.C.M. and J.M. were involved in data collection. All authors participated in drafting and revising the manuscript.
Corresponding author
Ethics declarations
Competing interests
D.A. and T.C. have submitted patent applications related to this work. T.C. is a co-founder and equity holder of HealthRhythms, Inc. and has received grants from Click Therapeutics related to digital therapeutics. D.C.M has accepted honoraria and consulting fees from Boehringer-Ingelheim, Otsuka Pharmaceuticals, Optum Behavioral Health, Centerstone Research Institute, and the One Mind Foundation, royalties from Oxford Press, and has an ownership interest in Adaptive Health, Inc. J.M. has accepted consulting fees from Boehringer Ingelheim. G.J.A. holds equity in HealthRhythms, Inc. and Lyra Health, Inc., and has accepted consulting fees and honoraria from BetterUp and Quantum Health.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adler, D.A., Stamatis, C.A., Meyerhoff, J. et al. Measuring algorithmic bias to analyze the reliability of AI tools that predict depression risk using smartphone sensed-behavioral data. npj Mental Health Res 3, 17 (2024). https://doi.org/10.1038/s44184-024-00057-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44184-024-00057-y