Abstract
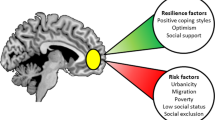
Psychosis research has traditionally focused on vulnerability and the detrimental outcomes of risk exposure. However, there is substantial variability in psychological and functional outcomes for those at risk for psychosis, even among individuals at high risk. Comparatively little work has highlighted the factors associated with resilience and the processes that might avert serious mental illness and promote positive outcomes. In this Review, we first discuss the prevailing risk-based approach to psychosis. We then outline a resilience-based approach by defining multisystemic mental health resilience and considering what constitutes a positive outcome. We examine evidence of biological, psychological, social and environmental protective and promotive factors that might confer resilience in the context of psychosis risk. A greater understanding of the factors and processes implicated in resilience has the potential to inform psychosis intervention and prevention efforts at multiple levels, including individuals, institutions and policy-making.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Laursen, T. M., Nordentoft, M. & Mortensen, P. B. Excess early mortality in schizophrenia. Annu. Rev. Clin. Psychol. 10, 425–448 (2014).
Selten, J. P. et al. Early course of schizophrenia in a representative Dutch incidence cohort. Schizophr. Res. 97, 79–87 (2007).
Levesque, I. S. & Abdel-Baki, A. Homeless youth with first-episode psychosis: a 2-year outcome study. Schizophr. Res. 216, 460–469 (2020).
Melle, I., Friis, S., Hauff, E. & Vaglum, P. Social functioning of patients with schizophrenia in high-income welfare societies. Psychiat. Serv. 51, 223–228 (2000).
Honkonen, T., Saarinen, S. & Salokangas, R. K. Deinstitutionalization and schizophrenia in Finland II: discharged patients and their psychosocial functioning. Schizophr. Bull. 25, 543–551 (1999).
Ran, M. S. et al. Homelessness among patients with schizophrenia in rural China: a 10-year cohort study. Acta Psychiat. Scand. 114, 118–123 (2006).
Gureje, O. & Bamidele, R. Thirteen-year social outcome among Nigerian outpatients with schizophrenia. Soc. Psychiat. Psychiat. Epidemiol. 34, 147–151 (1999).
Folsom, D. P. et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am. J. Psychiat. 162, 370–376 (2005).
Pinikahana, J., Happell, B., Hope, J. & Keks, N. A. Quality of life in schizophrenia: a review of the literature from 1995 to 2000. Int. J. Ment. Health Nurs. 11, 103–111 (2002).
Lieberman, J. A. et al. Science and recovery in schizophrenia. Psychiat. Serv. 59, 487–496 (2008).
Correll, C. U. et al. Comparison of early intervention services vs treatment as usual for early-phase psychosis: a systematic review, meta-analysis, and meta-regression. JAMA Psychiat. 75, 555–565 (2018).
Yung, A. R. et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust. NZ J. Psychiat. 39, 964–971 (2005).
Fusar-Poli, P. et al. Prevention of psychosis: advances in detection, prognosis, and intervention. JAMA Psychiat. 77, 755–765 (2020).
Fusar-Poli, P. et al. Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch. Gen. Psychiat. 69, 220–229 (2012).
Fusar-Poli, P. et al. Real-world long-term outcomes in individuals at clinical risk for psychosis: the case for extending duration of care. eClinicalMedicine 28, 100578 (2020).
Salazar de Pablo, G. et al. Longitudinal outcome of attenuated positive symptoms, negative symptoms, functioning and remission in people at clinical high risk for psychosis: a meta-analysis. eClinicalMedicine 36, 100909 (2021).
Haro, J. M. et al. Cross-national clinical and functional remission rates: worldwide schizophrenia outpatient health outcomes (W-SOHO) study. Br. J. Psychiat. 199, 194–201 (2011). This paper reports rates of clinical and functional remission in over 10,000 outpatients diagnosed with schizophrenia across the world.
Lally, J. et al. Remission and recovery from first-episode psychosis in adults: systematic review and meta-analysis of long-term outcome studies. Br. J. Psychiat. 211, 350–358 (2017).
Rangaswamy, T. Twenty-five years of schizophrenia: the Madras longitudinal study. Indian J. Psychiat. 54, 134–137 (2012).
Jobe, T. H. & Harrow, M. Schizophrenia course, long-term outcome, recovery, and prognosis. Curr. Dir. Psychol. Sci. 19, 220–225 (2010).
Volavka, J. & Vevera, J. Very long-term outcome of schizophrenia. Int. J. Clin. Pract. 72, e13094 (2018).
Masten, A. S., Lucke, C. M., Nelson, K. M. & Stallworthy, I. C. Resilience in development and psychopathology: multisystem perspectives. Annu. Rev. Clin. Psychol. 17, 521–549 (2021). This article describes the history of resilience science in psychology and provides current definitions and an overview of updated resilience models.
Carpenter, W. T. Jr. Schizophrenia: a view of immediate future. Schizophr. Res. 242, 15–16 (2021).
Andreasen, N. C. Understanding the causes of schizophrenia. N. Engl. J. Med. 340, 645–647 (1999).
Bleuler, M. Conception of schizophrenia within the last fifty years and today [abridged]. Proc. R. Soc. Med. 56, 945–952 (1963).
Rosenthal, D. The Genain Quadruplets: A Case Study and Theoretical Analysis of Heredity and Environment in Schizophrenia (Basic Books, 1963).
Hilker, R. et al. Heritability of schizophrenia and schizophrenia spectrum based on the nationwide Danish twin register. Biol. Psychiat. 83, 492–498 (2018).
Rasic, D., Hajek, T., Alda, M. & Uher, R. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta-analysis of family high-risk studies. Schizophr. Bull. 40, 28–38 (2014).
Singh, T. et al. Rare coding variants in ten genes confer substantial risk for schizophrenia. Nature 604, 509–516 (2022).
Trubetskoy, V. et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 604, 502–508 (2022).
Davies, C. et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiat. 7, 399–410 (2020). This is a meta-analysis of 152 studies showing several prenatal and perinatal factors that are associated with the later onset of psychosis.
Radua, J. et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiat. 17, 49–66 (2018). This paper summarizes results of systematic reviews and meta-analyses, and classifies risk and protective factors according to the strength of evidence.
Linszen, M. M., Brouwer, R. M., Heringa, S. M. & Sommer, I. E. Increased risk of psychosis in patients with hearing impairment: review and meta-analyses. Neurosci. Biobehav. Rev. 62, 1–20 (2016).
de Sousa, P., Varese, F., Sellwood, W. & Bentall, R. P. Parental communication and psychosis: a meta-analysis. Schizophr. Bull. 40, 756–768 (2014).
Filatova, S. et al. Early motor developmental milestones and schizophrenia: a systematic review and meta-analysis. Schizophr. Res. 188, 13–20 (2017).
Matheson, S. L., Shepherd, A. M., Laurens, K. R. & Carr, V. J. A systematic meta-review grading the evidence for non-genetic risk factors and putative antecedents of schizophrenia. Schizophr. Res. 133, 133–142 (2011).
Dean, K. & Murray, R. M. Environmental risk factors for psychosis. Dial. Clin. Neurosci. 7, 69–80 (2005).
Loewy, R. L. et al. Childhood trauma and clinical high risk for psychosis. Schizophr. Res. 205, 10–14 (2019).
Varese, F. et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr. Bull. 38, 661–671 (2012).
Beards, S. et al. Life events and psychosis: a review and meta-analysis. Schizophr. Bull. 39, 740–747 (2013).
Lopez, D., Altamirano, O. & Weisman de Mamani, A. The association between perceived racial discrimination and subclinical symptoms of psychosis. J. Ment. Health 31, 14–21 (2022).
Bardol, O. et al. Perceived ethnic discrimination as a risk factor for psychotic symptoms: a systematic review and meta-analysis. Psychol. Med. 50, 1077–1089 (2020).
Post, D. & Veling, W., Investigators, G. Sexual minority status, social adversity and risk for psychotic disorders-results from the GROUP study. Psychol. Med. 51, 770–776 (2021).
Anglin, D. M. et al. From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am. J. Psychiat. 178, 599–610 (2021).
Vassos, E., Pedersen, C. B., Murray, R. M., Collier, D. A. & Lewis, C. M. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr. Bull. 38, 1118–1123 (2012).
Myin-Germeys, I. & van Os, J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin. Psychol. Rev. 27, 409–424 (2007).
Collip, D., Myin-Germeys, I. & Van Os, J. Does the concept of “sensitization” provide a plausible mechanism for the putative link between the environment and schizophrenia? Schizophr. Bull. 34, 220–225 (2008).
Holtzman, C. W. et al. Stress and neurodevelopmental processes in the emergence of psychosis. Neuroscience 249, 172–191 (2013).
US Department of Health and Human Services. NIMH Strategic Plan for Research (NIH Publication No. 20-MH-8096). National Institute of Mental Health https://www.nimh.nih.gov/sites/default/files/documents/about/strategic-planning-reports/NIMH-Strategic-Plan-for-Research-2021-Update.pdf (2021).
Riechler-Rossler, A. & McGorry, P. D. Early Detection and Intervention in Psychosis: State of the Art and Future Perspectives (Karger, 2016).
Cannon, T. D. et al. An individualized risk calculator for research in prodromal psychosis. Am. J. Psychiat. 173, 980–988 (2016). This paper reports the accuracy of a calculator developed to compute risk for developing a psychotic disorder in individuals formally categorized as clinical high-risk cases.
Studerus, E., Beck, K., Fusar-Poli, P. & Riecher-Rössler, A. Development and validation of a dynamic risk prediction model to forecast psychosis onset in patients at clinical high risk. Schizophr. Bull. 46, 252–260 (2020).
Perkins, D. O., Gu, H., Boteva, K. & Lieberman, J. A. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am. J. Psychiat. 162, 1785–1804 (2005).
Howes, O. D. et al. The clinical significance of duration of untreated psychosis: an umbrella review and random-effects meta-analysis. World Psychiat. 20, 75–95 (2021).
Jonas, K. G. et al. Lead-time bias confounds association between duration of untreated psychosis and illness course in schizophrenia. Am. J. Psychiat. 177, 327–334 (2020).
van Os, J. & Guloksuz, S. A critique of the “ultra-high risk” and “transition” paradigm. World Psychiat. 16, 200–206 (2017).
Rogers, R. The uncritical acceptance of risk assessment in forensic practice. Law Hum. Behav. 24, 595–605 (2000).
Salazar de Pablo, G. et al. Probability of transition to psychosis in individuals at clinical high risk: an updated meta-analysis. JAMA Psychiat. 78, 970–978 (2021).
Addington, J. et al. North American prodrome longitudinal study (NAPLS 2): the prodromal symptoms. J. Nerv. Ment. Dis. 203, 328–335 (2015).
Simon, A. E. et al. Moving beyond transition outcomes: meta-analysis of remission rates in individuals at high clinical risk for psychosis. Psychiat. Res. 209, 266–272 (2013).
Sullivan, S. A. et al. A population-based cohort study examining the incidence and impact of psychotic experiences from childhood to adulthood, and prediction of psychotic disorder. Am. J. Psychiat. 177, 308–317 (2020).
Kaymaz, N. et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol. Med. 42, 2239–2253 (2012). This systematic review and meta-analysis reports the base rate of transition from subthreshold psychotic experiences to psychotic disorder diagnosis in representative and non-help-seeking population-based samples.
Yung, A. R. et al. Validation of “prodromal” criteria to detect individuals at ultra high risk of psychosis: 2 year follow-up. Schizophr. Res. 105, 10–17 (2008).
Haroun, N., Dunn, L., Haroun, A. & Cadenhead, K. S. Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophr. Bull. 32, 166–178 (2006).
Simon, A. E. et al. Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophr. Res. 132, 8–17 (2011).
Nelson, B. et al. Long-term follow-up of a group at ultra high risk (“prodromal”) for psychosis: the PACE 400 study. JAMA Psychiat. 70, 793–802 (2013).
Hartmann, J. A. et al. Declining transition rates to psychotic disorder in “ultra-high risk” clients: investigation of a dilution effect. Schizophr. Res. 170, 130–136 (2016).
Davies, C. et al. Lack of evidence to favor specific preventive interventions in psychosis: a network meta-analysis. World Psychiat. 17, 196–209 (2018).
Pescosolido, B. A., Halpern-Manners, A., Luo, L. & Perry, B. Trends in public stigma of mental illness in the US, 1996–2018. JAMA Netw. Open 4, e2140202 (2021).
Pescosolido, B. A., Medina, T. R., Martin, J. K. & Long, J. S. The “backbone” of stigma: identifying the global core of public prejudice associated with mental illness. Am. J. Public Health 103, 853–860 (2013).
Dubreucq, J., Plasse, J. & Franck, N. Self-stigma in serious mental illness: a systematic review of frequency, correlates, and consequences. Schizophr. Bull. 47, 1261–1287 (2021).
Anglin, D. M., Greenspoon, M. I., Lighty, Q., Corcoran, C. M. & Yang, L. H. Spontaneous labelling and stigma associated with clinical characteristics of peers ‘at-risk’ for psychosis. Early Interv. Psychiat. 8, 247–252 (2014).
Yang, L. H. et al. Public stigma associated with psychosis risk syndrome in a college population: implications for peer intervention. Psychiat. Serv. 64, 284–288 (2013).
Yang, L. H. et al. Stigma related to labels and symptoms in individuals at clinical high-risk for psychosis. Schizophr. Res. 168, 9–15 (2015).
Xu, Z. et al. Pathways between stigma and suicidal ideation among people at risk of psychosis. Schizophr. Res. 172, 184–188 (2016).
Belsky, J., Bakermans-Kranenburg, M. J. & van IJzendoorn, M. H. For better and for worse: differential susceptibility to environmental influences. Curr. Dir. Psychol. Sci. 16, 300–304 (2007).
Albott, C. S., Forbes, M. K. & Anker, J. J. Association of childhood adversity with differential susceptibility of transdiagnostic psychopathology to environmental stress in adulthood. JAMA Netw. Open 1, e185354 (2018).
Ferrarelli, F. & Mathalon, D. The prodromal phase: time to broaden the scope beyond transition to psychosis? Schizophr. Res. 216, 5–6 (2020).
Polari, A. et al. Clinical trajectories in the ultra-high risk for psychosis population. Schizophr. Res. 197, 550–556 (2018).
Ungar, M. Modeling Multisystemic Resilience (Oxford Univ. Press, 2021).
Luthar, S. S., Cicchetti, D. & Becker, B. The construct of resilience: a critical evaluation and guidelines for future work. Child. Dev. 71, 543–562 (2000).
Bronfenbrenner, U. Making Human Beings Human: Bioecological Perspectives on Human Development (Sage Publications, 2005).
Ungar, M. & Theron, L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. Lancet Psychiat. 7, 441–448 (2020). This paper provides an overview of the concept of resilience as the process of multiple systems interacting in ways that promote wellbeing in the context of risk factors.
Baumeister, D., Sedgwick, O., Howes, O. & Peters, E. Auditory verbal hallucinations and continuum models of psychosis: a systematic review of the healthy voice-hearer literature. Clin. Psychol. Rev. 51, 125–141 (2017).
Rose, D. et al. Reported stigma and discrimination by people with a diagnosis of schizophrenia. Epidemiol. Psychiat. Sci. 20, 193–204 (2011).
Marder, S. R. et al. Physical health monitoring of patients with schizophrenia. Am. J. Psychiat. 161, 1334–1349 (2004).
Rutter, M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiat. 57, 316–331 (1987). This is a seminal theory paper on human resilience that provides clear conceptual distinctions between vulnerability and protective factor.
Rutter, M. Transitions and turning points in developmental psychopathology: as applied to the age span between childhood and mid-adulthood. Int. J. Behav. Dev. 19, 603–626 (1996).
Miller-Graff, L. E. The multidimensional taxonomy of individual resilience. Trauma Violence Abuse 23, 660–675 (2020). This is a narrative overview of resilience science, including challenges faced by theoretical models of human resilience, which also proposes a framework for organizing and advancing research in resilience.
Burt, S. A., Klump, K. L., Vazquez, A. Y., Shewark, E. A. & Hyde, L. W. Identifying patterns of youth resilience to neighborhood disadvantage. Res. Hum. Dev. 18, 181–196 (2021). This paper reveals three partly independent domains of resilient outcomes in youth exposed to neighborhood disadvantage, highlighting the heterogeneous nature of positive outcomes.
Cohen, C. I. et al. Focus on geriatric psychiatry: schizophrenia in later life: clinical symptoms and social well-being. Psychiat. Serv. 59, 232–234 (2008).
Antaramian, S. P., Scott Huebner, E., Hills, K. J. & Valois, R. F. A dual-factor model of mental health: toward a more comprehensive understanding of youth functioning. Am. J. Orthopsychiat. 80, 462–472 (2010).
Infurna, F. J. & Luthar, S. S. Parents’ adjustment following the death of their child: resilience is multidimensional and differs across outcomes examined. J. Res. Pers. 68, 38–53 (2017).
Martinez-Torteya, C., Miller-Graff, L. E., Howell, K. H. & Figge, C. Profiles of adaptation among child victims of suspected maltreatment. J. Clin. Child Adolesc. Psychol. 46, 840–847 (2017).
Bonanno, G. A. Uses and abuses of the resilience construct: loss, trauma, and health-related adversities. Soc. Sci. Med. 74, 753–756 (2012).
Grych, J., Hamby, S. & Banyard, V. The resilience portfolio model: understanding healthy adaptation in victims of violence. Psychol. Viol. 5, 343–354 (2015).
Mahdiani, H. & Ungar, M. The dark side of resilience. Advers. Resil. Sci. 2, 147–155 (2021).
Andresen, R., Oades, L. & Caputi, P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust. NZ J. Psychiat. 37, 586–594 (2003).
Shinn, A. K. et al. Return to college after a first episode of psychosis. Schizophr. Bull. Open 1, sgaa041 (2020).
Law, H. & Morrison, A. P. Recovery in psychosis: a Delphi study with experts by experience. Schizophr. Bull. 40, 1347–1355 (2014). This article identifies consensus among definitions of recovery in a large sample of service users with a history of psychosis.
Fusar-Poli, P. et al. The lived experience of psychosis: a bottom-up review co-written by experts by experience and academics. World Psychiat. 21, 168–188 (2022).
Jordan, G. et al. Positive changes experienced after a first episode of psychosis: a systematic review. Psychiat. Serv. 69, 84–99 (2018).
Valiente, C., Espinosa, R., Trucharte, A., Nieto, J. & Martínez-Prado, L. The challenge of well-being and quality of life: a meta-analysis of psychological interventions in schizophrenia. Schizophr. Res. 208, 16–24 (2019).
Connell, J., O’Cathain, A. & Brazier, J. Measuring quality of life in mental health: are we asking the right questions? Soc. Sci. Med. 120, 12–20 (2014).
Oliver, D. et al. What causes the onset of psychosis in individuals at clinical high risk? A meta-analysis of risk and protective factors. Schizophr. Bull. 46, 110–120 (2020).
Solmi, M. et al. Risk and protective factors for mental disorders with onset in childhood/adolescence: an umbrella review of published meta-analyses of observational longitudinal studies. Neurosci. Biobehav. Rev. 120, 565–573 (2021).
Sommer, I. E. et al. Healthy individuals with auditory verbal hallucinations; who are they? Psychiatric assessments of a selected sample of 103 subjects. Schizophr. Bull. 36, 633–641 (2010).
Vargas, T. et al. Neuroimaging markers of resiliency in youth at clinical high risk for psychosis: a qualitative review. Biol. Psychiat. Cogn. Neurosci. Neuroimag. 6, 166–177 (2021).
Holz, N. E., Tost, H. & Meyer-Lindenberg, A. Resilience and the brain: a key role for regulatory circuits linked to social stress and support. Mol. Psychiat. 25, 379–396 (2020).
Alvaro, P. K., Roberts, R. M. & Harris, J. K. A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep 36, 1059–1068 (2013).
Buysse, D. J. et al. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 31, 473–480 (2008).
Freeman, D. et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiat. 4, 749–758 (2017). This paper provides evidence that cognitive behavioural therapy for insomnia improves sleep as well as paranoia and hallucinatory experiences in a large sample of university students.
Waters, F., Chiu, V., Atkinson, A. & Blom, J. D. Severe sleep deprivation causes hallucinations and a gradual progression toward psychosis with increasing time awake. Front. Psychiat. 9, 303 (2018).
Haack, M. & Mullington, J. M. Sustained sleep restriction reduces emotional and physical well-being. Pain 119, 56–64 (2005).
Zhai, L., Zhang, H. & Zhang, D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress. Anxiety 32, 664–670 (2015).
Rebar, A. L. et al. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol. Rev. 9, 366–378 (2015).
Rodriguez-Ayllon, M. et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 49, 1383–1410 (2019).
Spence, J. C., McGannon, K. R. & Poon, P. The effect of exercise on global self-esteem: a quantitative review. J. Sport. Exerc. Psychol. 27, 311–334 (2005).
Mammen, G. & Faulkner, G. Physical activity and the prevention of depression: a systematic review of prospective studies. Am. J. Prev. Med. 45, 649–657 (2013).
Teychenne, M., Ball, K. & Salmon, J. Physical activity and likelihood of depression in adults: a review. Prev. Med. 46, 397–411 (2008).
Teychenne, M. et al. Do we need physical activity guidelines for mental health: what does the evidence tell us? Ment. Health Phys. Act. 18, 100315 (2020).
World Health Organization WHO Guidelines on Physical Activity and Sedentary Behavior (2020).
Neill, R. D., Lloyd, K., Best, P. & Tully, M. A. The effects of interventions with physical activity components on adolescent mental health: systematic review and meta-analysis. Ment. Health Phys. Act. 19, 100359 (2020).
Crush, E. et al. Protective factors for psychotic experiences amongst adolescents exposed to multiple forms of victimization. J. Psychiat. Res. 104, 32–38 (2018).
Sormunen, E. et al. Effects of childhood and adolescence physical activity patterns on psychosis risk — a general population cohort study. npj Schizophr. 3, 5 (2017). This population-based cohort study found that higher levels of physical activity in childhood and adolescence were associated with a lower risk of developing a non-affective psychotic disorder.
Koivukangas, J. et al. Physical activity and fitness in adolescents at risk for psychosis within the Northern Finland 1986 Birth Cohort. Schizophr. Res. 116, 152–158 (2010).
Ohi, K. et al. Meta-analysis of physical activity and effects of social function and quality of life on the physical activity in patients with schizophrenia. Eur. Arch. Psychiat. Clin. Neurosci. 269, 517–527 (2019).
Holley, J., Crone, D., Tyson, P. & Lovell, G. The effects of physical activity on psychological well-being for those with schizophrenia: a systematic review. Br. J. Clin. Psychol. 50, 84–105 (2011).
Rosenbaum, S., Tiedemann, A., Sherrington, C., Curtis, J. & Ward, P. B. Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J. Clin. Psychiat. 75, 964–974 (2014).
Mittal, V. A. et al. Exercise treatments for psychosis: a review. Curr. Treat. Options Psychiat. 4, 152–166 (2017).
Firth, J. et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr. Bull. 43, 546–556 (2017).
McMahon, E. M. et al. Risk and protective factors for psychotic experiences in adolescence: a population-based study. Psychol. Med. 51, 1220–1228 (2021).
Perna, G. et al. Heart rate variability: can it serve as a marker of mental health resilience?: Special Section on “Translational and Neuroscience Studies in Affective Disorders” Section Editor, Maria Nobile MD, PhD. J. Affect. Disord. 263, 754–761 (2020).
An, E. et al. Heart rate variability as an index of resilience. Mil. Med. 185, 363–369 (2020).
Williams, D. P. et al. Resting heart rate variability predicts self-reported difficulties in emotion regulation: a focus on different facets of emotion regulation. Front. Psychol. 6, 261 (2015).
Thayer, J. F., Hansen, A. L., Saus-Rose, E. & Johnsen, B. H. Heart rate variability, prefrontal neural function, and cognitive performance: the neurovisceral integration perspective on self-regulation, adaptation, and health. Ann. Behav. Med. 37, 141–153 (2009).
Thayer, J. F. & Lane, R. D. Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci. Biobehav. Rev. 33, 81–88 (2009).
Beauchaine, T. P. Respiratory sinus arrhythmia: a transdiagnostic biomarker of emotion dysregulation and psychopathology. Curr. Opin. Psychol. 3, 43–47 (2015).
Cacciotti-Saija, C., Quintana, D. S., Alvares, G. A., Hickie, I. B. & Guastella, A. J. Reduced heart rate variability in a treatment-seeking early psychosis sample. Psychiat. Res. 269, 293–300 (2018).
Clamor, A., Lincoln, T. M., Thayer, J. F. & Koenig, J. Resting vagal activity in schizophrenia: meta-analysis of heart rate variability as a potential endophenotype. Br. J. Psychiat. 208, 9–16 (2016).
Zhang, T. H. et al. Imbalance model of heart rate variability and pulse wave velocity in psychotic and nonpsychotic disorders. Schizophr. Bull. 48, 154–165 (2022).
Benjamin, B. R. et al. Heart rate variability is associated with disease severity in psychosis spectrum disorders. Prog. Neuropsychopharmacol. Biol. Psychiat. 111, 110108 (2021).
Haigh, S. M., Walford, T. P. & Brosseau, P. Heart rate variability in schizophrenia and autism. Front. Psychiat. 12, 760396 (2021).
Clamor, A., Ludwig, L. & Lincoln, T. M. Heart rate variability as an index of emotion (dys)regulation in psychosis? Int. J. Psychophysiol. 158, 310–317 (2020).
Hamilton, H. K. et al. Social cognition and functional outcome in schizophrenia: the moderating role of cardiac vagal tone. J. Abnorm. Psychol. 123, 764–770 (2014).
Mathewson, K. J., Jetha, M. K., Goldberg, J. O. & Schmidt, L. A. Autonomic regulation predicts performance on Wisconsin Card Sorting Test (WCST) in adults with schizophrenia. Biol. Psychol. 91, 389–399 (2012).
Lehrer, P. M. & Gevirtz, R. Heart rate variability biofeedback: how and why does it work? Front. Psychol. 5, 756 (2014).
Goessl, V. C., Curtiss, J. E. & Hofmann, S. G. The effect of heart rate variability biofeedback training on stress and anxiety: a meta-analysis. Psychol. Med. 47, 2578–2586 (2017).
Sandercock, G. R., Bromley, P. D. & Brodie, D. A. Effects of exercise on heart rate variability: inferences from meta-analysis. Med. Sci. Sports Exerc. 37, 433–439 (2005).
Lehrer, P. et al. Heart rate variability biofeedback improves emotional and physical health and performance: a systematic review and meta analysis. Appl. Psychophysiol. Biofeedback 45, 109–129 (2020).
Kirk, U. & Axelsen, J. L. Heart rate variability is enhanced during mindfulness practice: a randomized controlled trial involving a 10-day online-based mindfulness intervention. PLoS One 15, e0243488 (2020).
Grässler, B., Thielmann, B., Böckelmann, I. & Hökelmann, A. Effects of different training interventions on heart rate variability and cardiovascular health and risk factors in young and middle-aged adults: a systematic review. Front. Physiol. 12, 657274 (2021).
McAusland, L. & Addington, J. Biofeedback to treat anxiety in young people at clinical high risk for developing psychosis. Early Interv. Psychiat. 12, 694–701 (2018).
Clamor, A., Koenig, J., Thayer, J. F. & Lincoln, T. M. A randomized-controlled trial of heart rate variability biofeedback for psychotic symptoms. Behav. Res. Ther. 87, 207–215 (2016).
Folkman, S. & Lazarus, R. S. An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 21, 219–239 (1980).
Lazarus, R. S. & Folkman, S. Stress, Appraisal, and Coping (Springer, 1984).
Lin, A. et al. The relationship between coping and subclinical psychotic experiences in adolescents from the general population — a longitudinal study. Psychol. Med. 41, 2535–2546 (2011).
Ered, A., Gibson, L. E., Maxwell, S. D., Cooper, S. & Ellman, L. M. Coping as a mediator of stress and psychotic-like experiences. Eur. Psychiat. 43, 9–13 (2017).
Mian, L., Lattanzi, G. M. & Tognin, S. Coping strategies in individuals at ultra-high risk of psychosis: a systematic review. Early Interv. Psychiat. 12, 525–534 (2018).
Ritsner, M., Gibel, A. & Ratner, Y. Determinants of changes in perceived quality of life in the course of schizophrenia. Qual. Life Res. 15, 515–526 (2006).
Boschi, S. et al. Coping with psychotic symptoms in the early phases of schizophrenia. Am. J. Orthopsychiat. 70, 242–252 (2000).
Cooke, M. et al. Insight, distress and coping styles in schizophrenia. Schizophr. Res. 94, 12–22 (2007).
Rudnick, A. & Martins, J. Coping and schizophrenia: a re-analysis. Arch. Psychiatr. Nurs. 23, 11–15 (2009).
Meyer, B. Coping with severe mental illness: relations of the brief COPE with symptoms, functioning, and well-being. J. Psychopathol. Behav. 23, 265–277 (2001).
Jalbrzikowski, M. et al. Coping styles of individuals at clinical high risk for developing psychosis. Early Interv. Psychiat. 8, 68–76 (2014). This prospective longitudinal study shows that more adaptive coping at baseline is associated with attenuated clinical symptom severity and better social functioning one year later in youth at high risk for psychosis.
Shi, J. et al. The relationship between big five personality traits and psychotic experience in a large non-clinical youth sample: the mediating role of emotion regulation. Front. Psychiat. 9, 648 (2018).
Osborne, K. J., Willroth, E. C., DeVylder, J. E., Mittal, V. A. & Hilimire, M. R. Investigating the association between emotion regulation and distress in adults with psychotic-like experiences. Psychiat. Res. 256, 66–70 (2017).
Sanderson, V. A. et al. Post-secondary students with symptoms of psychosis: a mixed-methods systematic review. Int. J. Ment. Health Nurs. 29, 590–607 (2020).
Shi, J. et al. Protective factors in Chinese university students at clinical high risk for psychosis. Psychiat. Res. 239, 239–244 (2016).
Wartelsteiner, F. et al. Quality of life in stabilized patients with schizophrenia is mainly associated with resilience and self-esteem. Acta Psychiat. Scand. 134, 360–367 (2016).
Harris, K., Haddock, G., Peters, S. & Gooding, P. Psychological resilience to suicidal thoughts and behaviours in people with schizophrenia diagnoses: a systematic literature review. Psychol. Psychother. 93, 777–809 (2020).
Peters, E. et al. Clinical, socio-demographic and psychological characteristics in individuals with persistent psychotic experiences with and without a “need for care”. World Psychiat. 15, 41–52 (2016). The results of this article provide important insights into what might reduce the chance of persistent psychotic experiences leading to poor psychological outcomes.
Krabbendam, L. et al. Neuroticism and low self-esteem as risk factors for psychosis. Soc. Psychiat. Psychiatr. Epidemiol. 37, 1–6 (2002).
Henderson, A. R. & Cock, A. The responses of young people to their experiences of first-episode psychosis: harnessing resilience. Community Ment. Health J. 51, 322–328 (2015).
Ho, W. W., Chiu, M. Y., Lo, W. T. & Yiu, M. G. Recovery components as determinants of the health-related quality of life among patients with schizophrenia: structural equation modelling analysis. Aust. NZ J. Psychiat. 44, 71–84 (2010).
Fisher, H. L. et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr. Bull. 39, 1045–1055 (2013).
Johns, L. C. et al. Auditory verbal hallucinations in persons with and without a need for care. Schizophr. Bull. 40, S255–S264 (2014).
Swyer, A. & Powers, A. R. 3rd Voluntary control of auditory hallucinations: phenomenology to therapeutic implications. npj Schizophr. 6, 19 (2020).
Kuranova, A. et al. Don’t worry, be happy: protective factors to buffer against distress associated with psychotic experiences. Schizophr. Res. 223, 79–86 (2020).
Kentros, M. K., Terkelsen, K., Hull, J., Smith, T. E. & Goodman, M. The relationship between personality and quality of life in persons with schizoaffective disorder and schizophrenia. Qual. Life Res. 6, 118–122 (1997).
Boyette, L. L. et al. Personality compensates for impaired quality of life and social functioning in patients with psychotic disorders who experienced traumatic events. Schizophr. Bull. 40, 1356–1365 (2014).
Ridgewell, C., Blackford, J. U., McHugo, M. & Heckers, S. Personality traits predicting quality of life and overall functioning in schizophrenia. Schizophr. Res. 182, 19–23 (2017).
Corrigan, P. W. & Watson, A. C. Understanding the impact of stigma on people with mental illness. World Psychiat. 1, 16–20 (2002).
Corrigan, P. W. & Rao, D. On the self-stigma of mental illness: stages, disclosure, and strategies for change. Can. J. Psychiat. 57, 464–469 (2012).
Yanos, P. T., Roe, D., Markus, K. & Lysaker, P. H. Pathways between internalized stigma and outcomes related to recovery in schizophrenia spectrum disorders. Psychiat. Serv. 59, 1437–1442 (2008).
Hasson-Ohayon, I. et al. Between self-clarity and recovery in schizophrenia: reducing the self-stigma and finding meaning. Compr. Psychiat. 55, 675–680 (2014).
Sibitz, I., Unger, A., Woppmann, A., Zidek, T. & Amering, M. Stigma resistance in patients with schizophrenia. Schizophr. Bull. 37, 316–323 (2011).
O’Connor, L. K., Yanos, P. T. & Firmin, R. L. Correlates and moderators of stigma resistance among people with severe mental illness. Psychiat. Res. 270, 198–204 (2018).
Firmin, R. L., Luther, L., Lysaker, P. H., Minor, K. S. & Salyers, M. P. Stigma resistance is positively associated with psychiatric and psychosocial outcomes: a meta-analysis. Schizophr. Res. 175, 118–128 (2016).
Rüsch, N. et al. Self-stigma, group identification, perceived legitimacy of discrimination and mental health service use. Br. J. Psychiat. 195, 551–552 (2009).
Yılmaz, E. & Kavak, F. Effects of mindfulness-based psychoeducation on the internalized stigmatization level of patients with schizophrenia. Clin. Nurs. Res. 29, 496–503 (2020).
Mittal, D., Sullivan, G., Chekuri, L., Allee, E. & Corrigan, P. W. Empirical studies of self-stigma reduction strategies: a critical review of the literature. Psychiat. Serv. 63, 974–981 (2012).
Koenig, H. G. Research on religion, spirituality, and mental health: a review. Can. J. Psychiat. 54, 283–291 (2009).
Migdal, L. & MacDonald, D. A. Clarifying the relation between spirituality and well-being. J. Nerv. Ment. Dis. 201, 274–280 (2013).
Pargament, K. I. & Mahoney, A. In Oxford Handbook of Positive Psychology (eds Lopez, S. J. & Snyder, C. R.) 611–619 (Oxford Univ. Press, 2009).
Murray-Swank, A. et al. Correlates of religious service attendance and contact with religious leaders among persons with co-occurring serious mental illness and type 2 diabetes. Nerv. Ment. Disord. 195, 382–388 (2007).
Severaid, K. B., Osborne, K. J. & Mittal, V. A. Implications of religious and spiritual practices for youth at clinical high risk for psychosis. Schizophr. Res. 208, 481–482 (2019).
Daalman, K. et al. The same or different? A phenomenological comparison of auditory verbal hallucinations in healthy and psychotic individuals. J. Clin. Psychiat. 72, 320–325 (2011).
Moseley, P., Powell, A., Woods, A., Fernyhough, C. & Alderson-Day, B. Voice-hearing across the continuum: a phenomenology of spiritual voices. Schizophr. Bull. 48, 1066–1074 (2022).
Roxburgh, E. C. & Roe, C. A. Reframing voices and visions using a spiritual model. An interpretative phenomenological analysis of anomalous experiences in mediumship. Ment. Health Relig. Cult. 17, 641–653 (2014).
Siddle, R., Haddock, G., Tarrier, N. & Faragher, E. B. Religious delusions in patients admitted to hospital with schizophrenia. Soc. Psychiat. Psychiat. Epidemiol. 37, 130–138 (2002).
Gearing, R. E. et al. Association of religion with delusions and hallucinations in the context of schizophrenia: implications for engagement and adherence. Schizophr. Res. 126, 150–163 (2011).
Sariah, A. E., Outwater, A. H. & Malima, K. I. Risk and protective factors for relapse among individuals with schizophrenia: a qualitative study in Dar es Salaam, Tanzania. BMC Psychiat. 14, 240 (2014).
Gooding, P. A., Littlewood, D., Owen, R., Johnson, J. & Tarrier, N. Psychological resilience in people experiencing schizophrenia and suicidal thoughts and behaviours. J. Ment. Health 28, 597–603 (2019).
Harris, K., Gooding, P., Haddock, G. & Peters, S. Factors that contribute to psychological resilience to suicidal thoughts and behaviours in people with schizophrenia diagnoses: qualitative study. BJPsych. Open 5, e79 (2019).
Pargament, K. I. The Psychology of Religion and Coping: Theory, Research, and Practice (Guilford Press, 1997).
Koenig, H. G. et al. Religious coping and depression among elderly, hospitalized medically ill men. Am. J. Psychiat. 149, 1693–1700 (1992).
Ferraro, K. F. & Koch, J. R. Religion and health among Black and white adults: examining social support and consolation. J. Sci. Study Relig. 33, 362–375 (1994).
Nguyen, A. W. Religion and mental health in racial and ethnic minority populations: a review of the literature. Innov. Aging 4, igaa035 (2020). This review of research on religiosity in Black and Latino communities living in the USA highlights racial and ethnic differences in the relationship between religion and mental health outcomes.
Heriot-Maitland, C., Knight, M. & Peters, E. A qualitative comparison of psychotic-like phenomena in clinical and non-clinical populations. Br. J. Clin. Psychol. 51, 37–53 (2012).
Powers, A. R. 3rd, Kelley, M. S. & Corlett, P. R. Varieties of voice-hearing: psychics and the psychosis continuum. Schizophr. Bull. 43, 84–98 (2017).
Lal, S. et al. Well-being and engagement in valued activities: experiences of young people with psychosis. Occup. Ther. J. Res. 33, 190–197 (2013).
Lal, S., Ungar, M., Malla, A., Leggo, C. & Suto, M. Impact of mental health services on resilience in youth with first episode psychosis: a qualitative study. Adm. Policy Ment. Health 44, 92–102 (2017).
Johnson, S., Sathyaseelan, M., Charles, H., Jeyaseelan, V. & Jacob, K. S. Insight, psychopathology, explanatory models and outcome of schizophrenia in India: a prospective 5-year cohort study. BMC Psychiat. 12, 159 (2012).
Riggio, R. E. In The Sourcebook of Nonverbal Measures: Going Beyond Words (ed. Manusov, V.) 25–33 (Lawrence Erlbaum, 2005).
Lecomte, T. et al. Predicting and preventing symptom onset and relapse in schizophrenia — a metareview of current empirical evidence. J. Abnorm. Psychol. 128, 840–854 (2019).
Rossi, R. et al. Personal and contextual components of resilience mediate risky family environment’s effect on psychotic-like experiences. Early Interv. Psychiat. 15, 1677–1685 (2021).
Pan, P. M. et al. Childhood trauma and adolescent psychotic experiences in a community-based cohort: the potential role of positive attributes as a protective factor. Schizophr. Res. 205, 23–29 (2019).
Lam, M. et al. Longitudinal cognitive changes in young individuals at ultrahigh risk for psychosis. JAMA Psychiat. 75, 929–939 (2018).
Fusar-Poli, P. et al. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch. Gen. Psychiat. 69, 562–571 (2012).
De Herdt, A. et al. Neurocognition in clinical high risk young adults who did or did not convert to a first schizophrenic psychosis: a meta-analysis. Schizophr. Res. 149, 48–55 (2013).
Hall, M. H., Holton, K. M., Öngür, D., Montrose, D. & Keshavan, M. S. Longitudinal trajectory of early functional recovery in patients with first episode psychosis. Schizophr. Res. 209, 234–244 (2019).
Crush, E., Arseneault, L., Jaffee, S. R., Danese, A. & Fisher, H. L. Protective factors for psychotic symptoms among poly-victimized children. Schizophr. Bull. 44, 691–700 (2018). This prospective longitudinal study shows that factors such as cognitive abilities, home environment qualities, and neighbourhood cohesion protect children with exposure to multiple victimization experiences from later psychotic symptoms.
Allen, J., Balfour, R., Bell, R. & Marmot, M. Social determinants of mental health. Int. Rev. Psychiat. 26, 392–407 (2014).
Crush, E., Arseneault, L. & Fisher, H. L. Girls get by with a little help from their friends: gender differences in protective effects of social support for psychotic phenomena amongst poly-victimised adolescents. Soc. Psychiat. Psychiatr. Epidemiol. 53, 1413–1417 (2018).
Crush, E., Arseneault, L., Danese, A., Jaffee, S. R. & Fisher, H. L. Using discordant twin methods to investigate an environmentally mediated pathway between social support and the reduced likelihood of adolescent psychotic experiences. Psychol. Med. 50, 1898–1905 (2020).
Riches, S. et al. Protective factors for early psychotic phenomena among children of mothers with psychosis. Front. Psychiat. 9, 750 (2018).
Pruessner, M., Iyer, S. N., Faridi, K., Joober, R. & Malla, A. K. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr. Res. 129, 29–35 (2011).
Norman, R. M. et al. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr. Res. 80, 227–234 (2005).
Lim, M. H., Gleeson, J. F., Jackson, H. J. & Fernandez, K. C. Social relationships and quality of life moderate distress associated with delusional ideation. Soc. Psychiat. Psychiat. Epidemiol. 49, 97–107 (2014). This paper highlights the importance of both receiving and giving social support in buffering against distress associated with persistent psychotic experiences.
Angell, B. & Test, M. A. The relationship of clinical factors and environmental opportunities to social functioning in young adults with schizophrenia. Schizophr. Bull. 28, 259–271 (2002).
Norman, R. M., Windell, D., Manchanda, R., Harricharan, R. & Northcott, S. Social support and functional outcomes in an early intervention program. Schizophr. Res. 140, 37–40 (2012).
Robustelli, B. L., Newberry, R. E., Whisman, M. A. & Mittal, V. A. Social relationships in young adults at ultra high risk for psychosis. Psychiat. Res. 247, 345–351 (2017).
Gan, G. et al. Neural correlates of affective benefit from real-life social contact and implications for psychiatric resilience. JAMA Psychiat. 78, 790–792 (2021).
Bjornestad, J. et al. “With a little help from my friends” social predictors of clinical recovery in first-episode psychosis. Psychiat. Res. 255, 209–214 (2017).
O’Keeffe, D. et al. The iHOPE-20 study: relationships between and prospective predictors of remission, clinical recovery, personal recovery and resilience 20 years on from a first episode psychosis. Aust. NZ J. Psychiat. 53, 1080–1092 (2019).
Myin-Germeys, I., Nicolson, N. A. & Delespaul, P. A. The context of delusional experiences in the daily life of patients with schizophrenia. Psychol. Med. 31, 489–498 (2001). This study uses experience sampling methodology and shows that the mere presence of family or acquantainces decreases the probability of the experience of delusional thoughts in individuals with schizophrenia.
Malmberg, A., Lewis, G., David, A. & Allebeck, P. Premorbid adjustment and personality in people with schizophrenia. Br. J. Psychiat. 172, 308–313 (1998).
Deegan, P. E. The importance of personal medicine: a qualitative study of resilience in people with psychiatric disabilities. Scand. J. Public Health Suppl. 66, 29–35 (2005).
March, D. et al. Psychosis and place. Epidemiol. Rev. 30, 84–100 (2008).
Veling, W. et al. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. Am. J. Psychiat. 165, 66–73 (2008). This prospective study shows that the incidence of psychotic disorders was increased among immigrants living in neighbourhoods where their ethnic group was a small proportion of the neighbourhood population.
Bosqui, T. J., Hoy, K. & Shannon, C. A systematic review and meta-analysis of the ethnic density effect in psychotic disorders. Soc. Psychiat. Psychiat. Epidemiol. 49, 519–529 (2014).
Li, D., Ramos, M. R., Bennett, M. R., Massey, D. S. & Hewstone, M. Does ethnic diversity affect well-being and allostatic load among people across neighbourhoods in England? Health Place 68, 102518 (2021).
van der Meer, T. & Tolsma, J. Ethnic diversity and its effects on social cohesion. Annu. Rev. Sociol. 40, 459–478 (2014).
Ramos, M. R., Bennett, M. R., Massey, D. S. & Hewstone, M. Humans adapt to social diversity over time. Proc. Natl Acad. Sci. USA 116, 12244–12249 (2019).
Becares, L., Nazroo, J. & Stafford, M. The buffering effects of ethnic density on experienced racism and health. Health Place 15, 670–678 (2009).
Maxwell, J. Social dimensions of economic growth. In Eric John Hanson Memorial Lecture Series Vol. 8 (University of Alberta, 1996).
Ansari, S. Social capital and collective efficacy: resource and operating tools of community social control. J. Theor. Phil. Criminol. 5, 75–94 (2013).
Schneider, J., Arthur, A., Doody, G., Simpson, J. & Jones, P. Individual social capital and psychosis: secondary analysis of AESOP data for Nottingham. Ment. Health Rev. 14, 4–12 (2009).
Kirkbride, J. B. et al. Neighbourhood-level effects on psychoses: re-examining the role of context. Psychol. Med. 37, 1413–1425 (2007).
Lofors, J. & Sundquist, K. Low-linking social capital as a predictor of mental disorders: a cohort study of 4.5 million Swedes. Soc. Sci. Med. 64, 21–34 (2007).
Rotenberg, M., Anderson, K. K. & McKenzie, K. Social capital and psychosis: a scoping review. Soc. Psychiat. Psychiat. Epidemiol. 55, 659–671 (2020).
Selten, J. P., van der Ven, E., Rutten, B. P. & Cantor-Graae, E. The social defeat hypothesis of schizophrenia: an update. Schizophr. Bull. 39, 1180–1186 (2013).
Gevonden, M. et al. Increased release of dopamine in the striata of young adults with hearing impairment and its relevance for the social defeat hypothesis of schizophrenia. JAMA Psychiat. 71, 1364–1372 (2014).
Bratman, G. N. et al. Nature and mental health: an ecosystem service perspective. Sci. Adv. 5, eaax0903 (2019).
Buxton, R. T., Pearson, A. L., Allou, C., Fristrup, K. & Wittemyer, G. A synthesis of health benefits of natural sounds and their distribution in national parks. Proc. Natl Acad. Sci. USA 118, e2013097118 (2021).
Engemann, K. et al. Childhood exposure to green space — a novel risk-decreasing mechanism for schizophrenia? Schizophr. Res. 199, 142–148 (2018).
Engemann, K. et al. Natural surroundings in childhood are associated with lower schizophrenia rates. Schizophr. Res. 216, 488–495 (2020). This large population-cohort study shows that childhood exposure to natural environments was associated with a reduced chance of being diagnosed with schizophrenia later in life.
Engemann, K. et al. Association between childhood green space, genetic liability, and the incidence of schizophrenia. Schizophr. Bull. 46, 1629–1637 (2020).
Fett, A. J., Lemmers-Jansen, I. L. J. & Krabbendam, L. Psychosis and urbanicity: a review of the recent literature from epidemiology to neurourbanism. Curr. Opin. Psychiat. 32, 232–241 (2019).
Henson, P., Pearson, J. F., Keshavan, M. & Torous, J. Impact of dynamic greenspace exposure on symptomatology in individuals with schizophrenia. PLoS One 15, e0238498 (2020).
Kaplan, S. The restorative benefits of nature: toward an integrative framework. J. Environ. Psychol. 15, 169–182 (1995).
Kellert, S. R. & Wilson, E. O. The Biophilia Hypothesis (Island Press/Shearwater Books, 1993).
Söderström, O. et al. Unpacking ‘the city’: an experience-based approach to the role of urban living in psychosis. Health Place 42, 104–110 (2016).
Shin, W. S., Yeoun, P. S., Yoo, R. W. & Shin, C. S. Forest experience and psychological health benefits: the state of the art and future prospect in Korea. Environ. Health Prev. Med. 15, 38–47 (2010).
Rosa, C. D., Larson, L. R., Collado, S. & Profice, C. C. Forest therapy can prevent and treat depression: evidence from meta-analyses. Urban For. Urban Green. 57, 126943 (2021).
Zabini, F. et al. Comparative study of the restorative effects of forest and urban videos during COVID-19 lockdown: intrinsic and benchmark values. Int. J. Environ. Res. Public Health 17, 8011 (2020).
Brancato, G., Van Hedger, K., Berman, M. G. & Van Hedger, S. C. Simulated nature walks improve psychological well-being along a natural to urban continuum. J. Environ. Psychol. 81, 101779 (2022).
Bielinis, E., Jaroszewska, A., Łukowski, A. & Takayama, N. The effects of a forest therapy programme on mental hospital patients with affective and psychotic disorders. Int. J. Environ. Res. Public Health 17, 118 (2019).
Moore, T. H. M. et al. The effects of changes to the built environment on the mental health and well-being of adults: SYSTEMATIC review. Health Place 53, 237–257 (2018).
Roe, J. et al. The urban built environment, walking and mental health outcomes among older adults: a pilot study. Front. Public Health 8, 575946 (2020).
Renalds, A., Smith, T. H. & Hale, P. J. A systematic review of built environment and health. Fam. Commun. Health 33, 68–78 (2010).
Rautio, N., Filatova, S., Lehtiniemi, H. & Miettunen, J. Living environment and its relationship to depressive mood: a systematic review. Int. J. Soc. Psychiat. 64, 92–103 (2018).
Vancampfort, D. et al. Associations between physical activity and the built environment in patients with schizophrenia: a multi-centre study. Gen. Hosp. Psychiat. 35, 653–658 (2013).
Vancampfort, D. et al. Associations of the built environment with physical activity and sedentary time in Ugandan outpatients with mental health problems. J. Phys. Act. Health 16, 243–250 (2019).
Vancampfort, D. et al. Associations between perceived neighbourhood environmental attributes and self-reported sitting time in patients with schizophrenia: a pilot study. Psychiat. Res. 215, 33–38 (2014).
Chaiyachati, K. H., Hom, J. K., Hubbard, R. A., Wong, C. & Grande, D. Evaluating the association between the built environment and primary care access for new Medicaid enrollees in an urban environment using Walk and Transit scores. Prev. Med. Rep. 9, 24–28 (2018).
Song, J. et al. Built environment and schizophrenia re-hospitalization risk in China: a cohort study. Environ. Res. 227, 115816 (2023).
Ungar, M. The differential impact of social services on young people’s resilience. Child Abuse Negl. 78, 4–12 (2018).
Engemann, K. et al. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proc. Natl Acad. Sci. USA 116, 5188–5193 (2019).
Heller, A. S. et al. Association between real-world experiential diversity and positive affect relates to hippocampal–striatal functional connectivity. Nat. Neurosci. 23, 800–804 (2020).
Werker, J. F. & Hensch, T. K. Critical periods in speech perception: new directions. Annu. Rev. Psychol. 66, 173–196 (2015).
Frankenhuis, W. E. & Walasek, N. Modeling the evolution of sensitive periods. Dev. Cogn. Neurosci. 41, 100715 (2020).
Gee, D. G. When do sensitive periods emerge later in development? Trends Cogn. Sci. 26, 97–98 (2022).
Walasek, N., Frankenhuis, W. E. & Panchanathan, K. An evolutionary model of sensitive periods when the reliability of cues varies across ontogeny. Behav. Ecol. 33, 101–114 (2022).
Theron, L. C. & Liebenberg, L. Understanding cultural contexts and their relationship to resilience processes. In Youth Resilience and Culture. Cross Cultural Advancements in Positive Psychology (eds Theron, L., Liebenberg, L. & Ungar, M.) Vol. 11, 23–36 (Springer, 2015).
Ungar, M. A constructionist discourse on resilience: multiple contexts, multiple realities among at-risk children and youth. Youth Soc. 35, 341–365 (2004).
Lin, K. M. & Kleinman, A. M. Psychopathology and clinical course of schizophrenia: a cross-cultural perspective. Schizophr. Bull. 14, 555–567 (1988).
Luhrmann, T. M. Social defeat and the culture of chronicity: or, why schizophrenia does so well over there and so badly here. Cult. Med. Psychiat. 31, 135–172 (2007).
Craig, T. J., Siegel, C., Hopper, K., Lin, S. & Sartorius, N. Outcome in schizophrenia and related disorders compared between developing and developed countries. A recursive partitioning re-analysis of the WHO DOSMD data. Br. J. Psychiat. 170, 229–233 (1997).
Harrison, G. et al. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br. J. Psychiat. 178, 506–517 (2001).
Hopper, K. In Schizophrenia, Culture and Subjectivity (eds Jenkins, J. H. & R. J. Barrett, J. H.) 62–86 (Cambridge Univ. Press, 2004).
Hopper, K. Rethinking social recovery in schizophrenia: what a capabilities approach might offer. Soc. Sci. Med. 65, 868–879 (2007).
Thara, R. & Anuradha Cognitive functioning in schizophrenia: its relevance to rehabilitation. Indian J. Med. Res. 126, 414–416 (2007).
Thara, R. & Eaton, W. W. Outcome of schizophrenia: the Madras longitudinal study. Aust. NZ J. Psychiat. 30, 516–522 (1996).
Kane, J. M. et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am. J. Psychiat. 173, 362–372 (2016).
Bennett, D. & Rosenheck, R. Socioeconomic status and the effectiveness of treatment for first-episode psychosis. Health Serv. Res. 56, 409–417 (2021). This follow-up analysis from a large treatment study shows that the initially promising effects of a coordinated specialty care intervention for early psychosis that adopts a strengths- and resilience-based approach were limited to those at the top 25% of the socioeconomic distribution.
Fusar-Poli, P. et al. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiat. 20, 200–221 (2021).
DeTore, N. R. et al. Efficacy of a transdiagnostic, prevention-focused program for at-risk young adults: a waitlist-controlled trial. Psychol. Med. https://doi.org/10.1017/S0033291722000046 (2022).
Burke, A. S. et al. Rationale, methods, feasibility, and preliminary outcomes of a transdiagnostic prevention program for at-risk college students. Front. Psychiat. 10, 1030 (2019).
Shah, J. L., Jones, N., van Os, J., McGorry, P. D. & Guloksuz, S. Early intervention service systems for youth mental health: integrating pluripotentiality, clinical staging, and transdiagnostic lessons from early psychosis. Lancet Psychiat. 9, 413–422 (2022).
Hartmann, J. A. et al. Pluripotential risk and clinical staging: theoretical considerations and preliminary data from a transdiagnostic risk identification approach. Front. Psychiat. 11, 553578 (2020).
Bonanno, G. A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 59, 20–28 (2004).
Erlenmeyer-Kimling, L. & Cornblatt, B. The New York High-Risk Project: a followup report. Schizophr. Bull. 13, 451–461 (1987).
Mednick, S. A., Parnas, J. & Schulsinger, F. The Copenhagen High-Risk Project, 1962–86. Schizophr. Bull. 13, 485–495 (1987).
Addington, J. et al. North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr. Bull. 33, 665–672 (2007).
Addington, J. et al. North American Prodrome Longitudinal Study (NAPLS 2): overview and recruitment. Schizophr. Res. 142, 77–82 (2012).
Liu, R. T. A developmentally informed perspective on the relation between stress and psychopathology: when the problem with stress is that there is not enough. J. Abnorm. Psychol. 124, 80–92 (2015).
Minor, K. S. et al. Personalizing interventions using real-world interactions: improving symptoms and social functioning in schizophrenia with tailored metacognitive therapy. J. Consult. Clin. Psychol. 90, 18–28 (2022).
Raugh, I. M. et al. Geolocation as a digital phenotyping measure of negative symptoms and functional outcome. Schizophr. Bull. 46, 1596–1607 (2020).
Fulford, D. et al. Smartphone sensing of social interactions in people with and without schizophrenia. J. Psychiat. Res. 137, 613–620 (2021).
Rapado-Castro, M., McGorry, P. D., Yung, A., Calvo, A. & Nelson, B. Sources of clinical distress in young people at ultra high risk of psychosis. Schizophr. Res. 165, 15–21 (2015).
Masten, A. S. Ordinary magic. Resilience processes in development. Am. Psychol. 56, 227–238 (2001).
Charlson, F. J. et al. Global epidemiology and burden of schizophrenia: findings from the Global Burden of Disease Study 2016. Schizophr. Bull. 44, 1195–1203 (2018).
Kraepelin, E. Dementia Praecox and Paraphrenia (Chicago Medical, 1919).
Rapoport, J. L., Giedd, J. N. & Gogtay, N. Neurodevelopmental model of schizophrenia: update 2012. Mol. Psychiat. 17, 1228–1238 (2012).
Jacobs, G. D., Pace-Schott, E. F., Stickgold, R. & Otto, M. W. Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison. Arch. Intern. Med. 164, 1888–1896 (2004).
Ritterband, L. M. et al. Efficacy of an internet-based behavioral intervention for adults with insomnia. Arch. Gen. Psychiat. 66, 692–698 (2009).
Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J. & Hall, M. H. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep. Med. Rev. 22, 23–36 (2015).
Hale, L., Troxel, W. & Buysse, D. J. Sleep health: an opportunity for public health to address health equity. Annu. Rev. Public Health 41, 81–99 (2020).
Morgan, A. J., Parker, A. G., Alvarez-Jimenez, M. & Jorm, A. F. Exercise and mental health: an exercise and sports science Australia commissioned review. J. Exerc. Physiol. Online 16, 64–73 (2013).
Firth, J., Cotter, J., Elliott, R., French, P. & Yung, A. R. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol. Med. 45, 1343–1361 (2015).
Damme, K. S. F. et al. Exercise intervention in individuals at clinical high risk for psychosis: benefits to fitness, symptoms, hippocampal volumes, and functional connectivity. Schizophr. Bull. 48, 1394–1405 (2022).
Pizzoli, S. F. M. et al. A meta-analysis on heart rate variability biofeedback and depressive symptoms. Sci. Rep. 11, 6650 (2021).
Schlier, B., Ludwig, L., Wiesjahn, M., Jung, E. & Lincoln, T. M. Fostering coping as a mechanism of symptom change in cognitive behavioural therapy for psychosis. Schizophr. Res. 215, 416–423 (2020).
Wykes, T., Steel, C., Everitt, B. & Tarrier, N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr. Bull. 34, 523–537 (2008).
Fusar-Poli, P. et al. Preventive treatments for psychosis: umbrella review (just the evidence). Front. Psychiat. 10, 764 (2019).
Meyer, P. S., Gottlieb, J. D., Penn, D., Mueser, K. & Gingerich, S. Individual resiliency training: an early intervention approach to enhance well-being in people with first-episode psychosis. Psychiat. Ann. 45, 554–560 (2015).
Niveau, N., New, B. & Beaudoin, M. Self-esteem interventions in adults — a systematic review and meta-analysis. J. Res. Pers. 94, 104131 (2021).
Arzy, S., Thut, G., Mohr, C., Michel, C. M. & Blanke, O. Neural basis of embodiment: distinct contributions of temporoparietal junction and extrastriate body area. J. Neurosci. 26, 8074–8081 (2006).
Tsang, H. W. et al. Therapeutic intervention for internalized stigma of severe mental illness: a systematic review and meta-analysis. Schizophr. Res. 173, 45–53 (2016).
Pargament, K. I. & Lomax, J. W. Understanding and addressing religion among people with mental illness. World Psychiat. 12, 26–32 (2013).
Weisman de Mamani, A., Tuchman, N. & Duarte, E. A. Incorporating religion/spirituality into treatment for serious mental illness. Cogn. Behav. Pract. 17, 348–357 (2010).
Granholm, E. L., McQuaid, J. R. & Holden, J. L. Cognitive-Behavioral Social Skills Training For Schizophrenia: A Practical Treatment Guide (Guilford Publications, 2016).
Horan, W. P. et al. Social cognitive skills training in schizophrenia: an initial efficacy study of stabilized outpatients. Schizophr. Res. 107, 47–54 (2009).
Roberts, D. L. et al. A randomized, controlled trial of social cognition and interaction training (SCIT) for outpatients with schizophrenia spectrum disorders. Br. J. Clin. Psychol. 53, 281–298 (2014).
Nahum, M. et al. Online social cognition training in schizophrenia: a double-blind, randomized, controlled multi-site clinical trial. Schizophr. Bull. 47, 108–117 (2021).
Vita, A. et al. Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiat. 78, 848–858 (2021).
Wykes, T., Huddy, V., Cellard, C., McGurk, S. R. & Czobor, P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am. J. Psychiat. 168, 472–485 (2011).
Glenthoj, L. B., Hjorthoj, C., Kristensen, T. D., Davidson, C. A. & Nordentoft, M. The effect of cognitive remediation in individuals at ultra-high risk for psychosis: a systematic review. npj Schizophr. 3, 20 (2017).
Hogan, B. E., Linden, W. & Najarian, B. Social support interventions: do they work? Clin. Psychol. Rev. 22, 383–442 (2002).
White, S. et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiat. 20, 534 (2020).
Liu, C. H., Keshavan, M. S., Tronick, E. & Seidman, L. J. Perinatal risks and childhood premorbid indicators of later psychosis: next steps for early psychosocial interventions. Schizophr. Bull. 41, 801–816 (2015).
Bauer, A. et al. Mobilising social support to improve mental health for children and adolescents: a systematic review using principles of realist synthesis. PLoS One 16, e0251750 (2021).
Webber, M. & Fendt-Newlin, M. A review of social participation interventions for people with mental health problems. Soc. Psychiat. Psychiat. Epidemiol. 52, 369–380 (2017).
Semenza, J. C. & March, T. L. An urban community-based intervention to advance social interactions. Environ. Behav. 41, 22–42 (2009).
Cohen, D. A., Inagami, S. & Finch, B. The built environment and collective efficacy. Health Place 14, 198–208 (2008).
Hunter, R. F. et al. Environmental, health, wellbeing, social and equity effects of urban green space interventions: a meta-narrative evidence synthesis. Environ. Int. 130, 104923 (2019).
South, E. C., Hohl, B. C., Kondo, M. C., MacDonald, J. M. & Branas, C. C. Effect of greening vacant land on mental health of community-dwelling adults: a cluster randomized trial. JAMA Netw. Open 1, e180298 (2018).
Urban green space and health: intervention impacts and effectiveness. WHO https://www.who.int/europe/publications/m/item/urban-green-space-interventions-and-health--a-review-of-impacts-and-effectiveness.-full-report (2017).
Dauwan, M., Begemann, M. J., Heringa, S. M. & Sommer, I. E. Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophr. Bull. 42, 588–599 (2016).
Tao, F. B. et al. Physical activity might not be the protective factor for health risk behaviours and psychopathological symptoms in adolescents. J. Paediatr. Child Health 43, 762–767 (2007).
Chekroud, S. R. et al. Association between physical exercise and mental health in 1.2 million individuals in the USA between 2011 and 2015: a cross-sectional study. Lancet Psychiat. 5, 739–746 (2018).
Firth, J., Schuch, F. & Mittal, V. A. Using exercise to protect physical and mental health in youth at risk for psychosis. Res. Psychother. 23, 433 (2020).
Dawkins, M. P., Williams, M. M. & Guilbault, M. Participation in school sports: risk or protective factor for drug use among Black and white students. J. Negro Educ. 75, 25–33 (2006).
Quinton, D., Rutter, M. & Liddle, C. Institutional rearing, parenting difficulties and marital support. Psychol. Med. 14, 107–124 (1984).
Crawford, J. R. & Henry, J. D. The positive and negative affect schedule (PANAS): construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 43, 245–265 (2004).
Freeman, D. et al. Comparison of a theoretically driven cognitive therapy (the Feeling Safe programme) with befriending for the treatment of persistent persecutory delusions: a parallel, single-blind, randomised controlled trial. Lancet Psychiat. 8, 696–707 (2021).
Bell, V., Halligan, P. W. & Ellis, H. D. Explaining delusions: a cognitive perspective. Trends Cogn. Sci. 10, 219–226 (2006).
Mehl, S., Werner, D. & Lincoln, T. M. Does cognitive behavior therapy for psychosis (CBTp) show a sustainable effect on delusions? A meta-analysis. Front. Psychol. 6, 1450 (2015).
Fried, E. I., Koenders, M. A. & Blom, J. D. Bleuler revisited: on persecutory delusions and their resistance to therapy. Lancet Psychiat. 8, 644–646 (2021).
Ritunnano, R., Broome, M. & Stanghellini, G. Charting new phenomenological paths for empirical research on delusions: embracing complexity, finding meaning. JAMA Psychiat. 78, 1063–1064 (2021).
Feyaerts, J., Henriksen, M. G., Vanheule, S., Myin-Germeys, I. & Sass, L. A. Delusions beyond beliefs: a critical overview of diagnostic, aetiological, and therapeutic schizophrenia research from a clinical-phenomenological perspective. Lancet Psychiat. 8, 237–249 (2021).
Ritunnano, R., Humpston, C. & Broome, M. R. Finding order within the disorder: a case study exploring the meaningfulness of delusions. BJPsych. Bull. 46, 109–115 (2021).
Bilu, Y., Witztum, E. & van der Hart, O. Paradise regained: “miraculous healing” in an Israeli psychiatric clinic. Cult. Med. Psychiat. 14, 105–127 (1990).
Appelbaum, P. S., Robbins, P. C. & Roth, L. H. Dimensional approach to delusions: comparison across types and diagnoses. Am. J. Psychiat. 156, 1938–1943 (1999).
Coid, J. W. et al. The relationship between delusions and violence: findings from the East London first episode psychosis study. JAMA Psychiat. 70, 465–471 (2013).
Roberts, G. Delusional belief systems and meaning in life: a preferred reality? Br. J. Psychiat. Suppl. 14, 19–28 (1991).
Rutunnano, R. & Bortolotti, L. Do delusions have and give meaning? Phenom. Cogn. Sci. 21, 949–968 (2021).
Chennaoui, M., Arnal, P. J., Sauvet, F. & Léger, D. Sleep and exercise: a reciprocal issue? Sleep. Med. Rev. 20, 59–72 (2015).
Minkel, J. et al. Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychol. 33, 1430–1434 (2014).
Hamilton, J. L. & Alloy, L. B. Atypical reactivity of heart rate variability to stress and depression across development: systematic review of the literature and directions for future research. Clin. Psychol. Rev. 50, 67–79 (2016).
Joao, K., Jesus, S. N., Carmo, C. & Pinto, P. The impact of sleep quality on the mental health of a non-clinical population. Sleep. Med. 46, 69–73 (2018).
Sallis, J. F. et al. Built environment, physical activity, and obesity: findings from the international physical activity and environment network (IPEN) adult study. Annu. Rev. Public Health 41, 119–139 (2020).
Marshall, S. L., Parker, P. D., Ciarrochi, J. & Heaven, P. C. L. Is self-esteem a cause or consequence of social support? A 4-year longitudinal study. Child Dev. 85, 1275–1291 (2014).
Ludyga, S., Gerber, M., Puhse, U., Looser, V. N. & Kamijo, K. Systematic review and meta-analysis investigating moderators of long-term effects of exercise on cognition in healthy individuals. Nat. Hum. Behav. 4, 603–612 (2020).
Soundy, A. et al. The transcending benefits of physical activity for individuals with schizophrenia: a systematic review and meta-ethnography. Psychiat. Res. 220, 11–19 (2014).
Astell-Burt, T., Feng, X., Mavoa, S., Badland, H. M. & Giles-Corti, B. Do low-income neighbourhoods have the least green space? A cross-sectional study of Australia’s most populous cities. BMC Public Health 14, 292 (2014).
Acknowledgements
The authors would like to thank J. Bao and J. Fattal for their help with the literature search.
Author information
Authors and Affiliations
Contributions
K.N.T., A.McC., K.S.M., C.S.H. and S.P. wrote the article. All authors researched data for the article, contributed substantially to discussion of the content, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Psychology thanks Thomas Kwapil and Angus Macbeth for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thakkar, K.N., McCleery, A., Minor, K.S. et al. Moving from risk to resilience in psychosis research. Nat Rev Psychol 2, 537–555 (2023). https://doi.org/10.1038/s44159-023-00205-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44159-023-00205-9
This article is cited by
-
Considering resilience
Nature Reviews Psychology (2023)