Abstract
Background
A lack of fine, spatially-resolute case data for the U.S. has prevented the examination of how COVID-19 infection burden has been distributed across neighborhoods, a key determinant of both risk and resilience. Without more spatially resolute data, efforts to identify and mitigate the long-term fallout from COVID-19 in vulnerable communities will remain difficult to quantify and intervene on.
Methods
We leveraged spatially-referenced data from 21 states collated through the COVID Neighborhood Project to examine the distribution of COVID-19 cases across neighborhoods and states in the U.S. We also linked the COVID-19 case data with data on the neighborhood social environment from the National Neighborhood Data Archive. We then estimated correlations between neighborhood COVID-19 burden and features of the neighborhood social environment.
Results
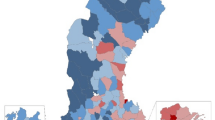
We find that the distribution of COVID-19 at the neighborhood-level varies within and between states. The median case count per neighborhood (coefficient of variation (CV)) in Wisconsin is 3078.52 (0.17) per 10,000 population, indicating a more homogenous distribution of COVID-19 burden, whereas in Vermont the median case count per neighborhood (CV) is 810.98 (0.84) per 10,000 population. We also find that correlations between features of the neighborhood social environment and burden vary in magnitude and direction by state.
Conclusions
Our findings underscore the importance that local contexts may play when addressing the long-term social and economic fallout communities will face from COVID-19.
Plain language summary
A lack of data on the geographic location of COVID-19 cases in the U.S has limited our ability to examine how COVID-19 burden has been distributed across neighborhoods within U.S. states. It may be that certain neighborhoods have borne a disproportionate burden of COVID-19 and are more likely to experience greater long-term social and economic consequences from the pandemic. We used data from 21 states to examine the distribution of COVID-19 cases across neighborhoods and states in the U.S. We find that the distribution of COVID-19 varies widely both within neighborhoods in a state, and between states. We also find that the features of the neighborhood social environment that are correlated with neighborhood COVID-19 burden vary by state. Our findings show that the local neighborhood may play an important role in addressing long-term social and economic consequences from COVID-19.
Similar content being viewed by others
Introduction
In the United States (U.S.), the COVID-19 pandemic has affected nearly every American and nearly every part of American life. However, the burden of COVID-19 has not been equally distributed across the U.S and globally. A recent study by Bollyky et al. provides compelling evidence for the stark differences in the distribution of COVID-19 cases and deaths across states within the U.S., as well as the link between those state-level differences and socioeconomic and demographic state characteristics. The authors reported up to a four-fold difference in age- and comorbidity-standardized COVID-19 death rates across states in the U.S.1 Moreover, infections and deaths were disproportionately clustered in states with lower levels of education, higher levels of poverty, limited access to healthcare, and lower levels of self-reported trust in one another1. This report follows a 2021 study that found that individuals living in U.S. states with high levels of pre-pandemic poverty and a greater proportion of non-Hispanic Black individuals experienced a greater number of COVID-19 hardships including food insufficiency, loss of income, unemployment, and housing instability, and that racialized minorities had a slower recovery from these hardships than their white counterparts2.
While variation in disease risk and post-pandemic socioeconomic repercussions between states has been well documented, a growing number of studies have demonstrated such heterogeneities also exist within states, and specifically between neighborhoods within states3,4,5,6,7,8,9,10,11,12,13,14,15. Understanding local trends is essential for not only quantifying but intervening on the growing social and economic inequities that are a consequence of the uneven burden of COVID-19. Neighborhoods are a source of both risk and resilience to COVID-19 and its long-term sequelae due to their social and economic characteristics (e.g., crowding, housing density, affluence, business types, and political partisanship)16,17,18,19,20,21,22. Since the start of the COVID-19 pandemic, socioeconomically disadvantaged neighborhoods have faced substantially greater population losses, economic hardships, and business closures compared to less disadvantaged neighborhoods, particularly those neighborhoods with a greater share of working-aged adults. For example, in the early months of the pandemic, a multi-state study of COVID-19 prevalence by ZIP code found a higher burden of disease in socioeconomically disadvantaged ZIP codes in Illinois and Maryland3.
Despite initial evidence indicating neighborhood and state contexts play an important role in shaping COVID-19 risk and resilience, two major gaps in both data availability and research have hampered efforts to fully understand neighborhood variation within states in the U.S. First, there has been lack of fine-scale, spatially-resolute COVID-19 case data made available publicly for analysis across the U.S. The national efforts to collate spatially-referenced data have largely focused on the county- or state-level (e.g., Centers for Disease Control and Prevention COVID-19 Data Tracker or the Johns Hopkins University Coronavirus Resource Center, or the Institute for Health Metrics and Evaluation’s (IHME) COVID-19 modelling database)1,23,24,25,26,27. There have been several initiatives that seek to understand neighborhood trends but have focused on select cities only. For example, The Big Cities Health Coalition (BCHC) created a dashboard where the distribution of COVID-19 cases across neighborhoods (i.e., ZIP code tabulation areas) could be examined and linked with relevant social indicators for 35 U.S. cities28. In another example, the City Health Dashboard initiative provided small-scale, spatially-referenced data on a range of health, social, and demographic metrics for over 750 small and large cities in the U.S.29, which at one point included a neighborhood-level COVID-19 risk index30.
Second, while some studies have examined neighborhood variation in COVID-19 burden, they are limited to cities, thereby omitting data from geographic areas beyond the chosen urban settings. For example, studies that have examined finer spatial levels (e.g., ZIP code and/or census tract) have been limited to a single city, region, or state3,4,5,8,9,10,11,12,13,14,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47. Some of these studies have examined a group of cities, regions, or states, including the BCHC initiative noted above but none have employed an expansive effort to look at trends across diverse regions of the U.S.3,10,31,36,38,45 As a result of both the data and research gaps described above, the analyses that have been conducted examining neighborhood-level variation and state differences in neighborhood-level variation have been biased towards cities lending little insight into what is happening among rural populations. Several studies conducted early in the pandemic documented temporal and spatial differences in COVID-19 burden between urban and rural areas48 with rural areas continuing to experience spikes in COVID-19 cases when cases were receding in urban areas49. Further, these trends extend beyond the U.S. setting; studies in both the U.S. and U.K. have documented the unequal toll the pandemic and its aftermath continue to have on rural communities compared to urban communities50,51,52. Taken together, these studies highlight the need for rural communities to be included in both our data and models to understand the predictors of COVID-19 burden and its consequences.
To directly address these gaps, we launched the COVID Neighborhood Project (CONEP) in 2021. CONEP is a repository of locally-referenced (census tract or ZIP code tabulation area (ZCTA)) COVID-19 case data from April 2020 to April 2022 for the U.S. The repository currently includes cumulative case data for 21 states in all five regions of the U.S. (West, Southwest, Midwest, Northeast, and Southeast). Data collation for the remaining states is ongoing. The novelty of this resource has enabled a closer examination of both state- and neighborhood-level variation in COVID-19 burden across a more expansive portion of the U.S., including both urban and rural areas. These local patterns, including in both rural and urban areas across the U.S., are critical to our understanding of which communities will continue to face short-term and long-term health, social and economic consequences from COVID-19, while laying the groundwork for future pandemic preparation.
In this paper, we leverage data from CONEP to illustrate how neighborhood-level COVID-19 infection burden varies between states and examine the neighborhood social characteristics that are correlated with infection burden. We address a critical gap in the literature with the following research questions: (1) How is COVID-19 distributed across neighborhoods (i.e., ZCTAs or census tracts) within states, and is the neighborhood distribution of COVID-19 burden similar between states? (2) Within each state, what features of the neighborhood social environment are correlated with neighborhood COVID-19 burden? We find that the distribution of COVID-19 at the neighborhood-level varies both within and between states. Some states have a more homogenous distribution of COVID-19 compared to other states in which there is a wide variation in COVID-19 burden within the state. We also find that the neighborhood social factors that are correlated with neighborhood COVID-19 burden vary both in magnitude and direction by state.
Methods
The COVID Neighborhood Project
We launched CONEP in 2021 to address the need for fine-scale spatially resolute COVID-19 case data for the entire U.S. We contacted health departments in all 50 U.S. states. Initial contact consisted of calls, emails, and data portal requests asking for fine-scale COVID-19 case data. For some states, census tract or ZIP code data were publicly available. Others required a Freedom of Information Act (FOIA) request. Following request edits, resubmissions, and the eventual approval, we were sent data through a secure email.
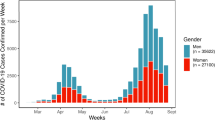
COVID-19 case data and neighborhood data
We used COVID-19 cases at the ZIP-code level for sixteen states, and census tract-level for five states. Data were collected from state health departments throughout the summer and fall for both 2021 and 2022. Data were collected in a cumulative format. State COVID-19 cases were defined as they were by each respective state health department, most commonly as the sum of both laboratory confirmed and probable cases (1–3). Most states did not disaggregate their case data by time period.
We collected both census tract and ZIP code level data. For those states with ZIP code level data, we used a cross-walk to merge ZIP codes into ZIP Code Tabulation Areas (ZCTA)s. ZIP codes are designated by the U.S. Postal Service and used to identify postal delivery routes. Therefore, they do not represent a spatial area. ZCTAs are generated by the U.S. Census Bureau and are generalized representations of ZIP codes. Methods used to create ZCTAs are detailed elsewhere53. Of note, ZIP-code level data were not available in Florida past 23 June 2021.
The study was approved by the Health and Behavioral Sciences Institutional Review Board at the University of Michigan (IRB Approval Number: HUM00202190). Data use agreements were done on a state-by-state basis (see Data and Materials availability statement below). As this study involves only the secondary analysis of de-identified data, informed consent was not required.
Estimates of the neighborhood social and physical context from the National Neighborhood Data Archive (NANDA)
The primary aim of the current investigation was to report state-level patterns in the distribution of COVID-19 burden at the neighborhood level. However, the ultimate goal of CONEP is to examine how features of the social and physical environment have shaped COVID-19 burden throughout the pandemic, providing a roadmap for addressing the long-term consequences certain communities will face. As previous studies of both COVID-19, as well as many other infectious diseases, have consistently demonstrated the importance of neighborhood SES in determining the distribution of infectious disease burden3,24,54,55,56, we focused on two specific measures of neighborhood SES: neighborhood disadvantage and neighborhood affluence. We also employed measures of neighborhood-level rurality, population density, and county-level political partisanship.
We obtained measures of the neighborhood context from NANDA, a publicly available repository of curated measures of social and physical environment context across the US.57.
Neighborhood disadvantage is an analytically derived index and is the mean of four variables collected as part of the American Community Survey (ACS): proportion of female-headed households with children, proportion of households receiving public assistance income or food stamps, proportion of families with income below the federal poverty level, and proportion of the population aged 16 years and older that are unemployed57. Mean scores range from 0-100. Disadvantaged neighborhoods tend to have fewer resources (e.g., healthy food stores, well-maintained parks, good schools, quality medical care)20,58 and are often vulnerable to disinvestment and environmental hazards59. These measurements were based on 2017 ACS data with the exception of New Mexico which was based on the 2020 ACS.
Neighborhood affluence is the mean of three variables from the ACS: percent of household with income greater than $75K per year, percent of the population over the age of 16 employed in professional or managerial occupations, and percent of the population with a Bachelor’s Degree or higher57. Mean scores range from 0-100. Higher values indicate a more affluent neighborhood. Affluent neighborhoods are likely to attract a set of institutions (e.g., food stores, places to exercise, well-maintained buildings, and parks) that foster a set of norms (e.g., an emphasis on exercise and healthy diets) conducive to good health60. Both from a theoretical and analytical standpoint, neighborhood affluence is distinct from neighborhood disadvantage57. Neighborhood affluence is associated with higher levels of social control and leverage over local institutions that can foster social environments that facilitate health16. These measurements were based on 2017 ACS data with the exception of New Mexico which was based on the 2020 ACS.
Neighborhood rurality was defined based on the 2010 rural-urban commuting area (RUCA) codes61. The RUCA was defined at both the census tract and ZCTA level. In the correlation analyses, we used an ordinal RUCA code in which higher values indicate more rural areas. In the univariate analyses, we used a four-level variable classifying neighborhoods according to their RUCA code as metropolitan, micropolitan, small town, or rural. Of note, the 2010 RUCA was not available for New Mexico as they used 2020 geography to define their census tracts and the 2020 RUCA codes are not available yet.
Neighborhood population density is an indicator of the number of persons per square mile in the census tract and/or ZCTA57. We included neighborhood population density to proxy the potential for exposure to the SARS-COV-2 pathogen within a given neighborhood with the hypothesis that those neighborhoods with higher population density would have higher COVID-19 case counts. Given that contact with an infectious pathogen is a necessary cause of infectious disease, we use neighborhood population density as an imperfect proxy of the probability of encountering an infectious case of COVID-1955.
We defined county-level political partisanship with a continuous measure that indicates the mean percent of votes cast for Republican candidates in presidential and senate races from 2012 to 201862. In univariate analyses, we categorized the variable such that a one-unit increase in the political partisanship variable was equivalent to 10% increase in Republican votes. We linked ZCTAs and census tracts to the respective counties in which they resided. For ZCTAs that spanned two counties, we chose the county that had the greatest proportion of the ZCTA. Further, we use a measure of county-level political partisanship to begin to understand the complex role that political ideology has had in shaping COVID-19 testing, vaccination access, and mitigation strategies in the US63,64.
Statistical analyses
We first calculated the cumulative COVID-19 case count per 10,000 population for each state. We then calculated the median case count per 10,000 and coefficient of variation (CV) for ZCTAs or census tracts within states cumulatively for the entire time period for which the state reported data. The CV is calculated by taking the standard deviation and dividing it by the mean in each state.
We estimated the correlation between each neighborhood variable and COVID-19 burden for each state. We then constructed a series of univariate Poisson regression models to estimate the association between each neighborhood factor and the incidence rate ratio (IRR) of COVID-19 cases for neighborhoods within each state. The total population of the neighborhood served as the offset term in the models. We used generalized estimating equations with robust standard errors to account for clustering of census tracts and ZCTAs in counties.
All statistical analyses were carried out in Stata/mp 17.0 and 18.0.
Results
Cumulative case counts are heterogenous between states
Of the spatially-referenced COVID-19 case data from 21 states, 5 states have data at the census-tract level and 16 states have data at the ZIP code level (Table 1). We used a cross-walk to convert the ZIP codes to Zip Code Tabulation Areas (ZCTAs) which is further described in the methods. Case data generally span 2021-2022, although there is state variability in the specific temporal reporting coverage (Table S1). We calculated the cumulative case count (census-tract or ZCTA) per 10,000 population for the entire time period (Table 1). Florida has the lowest cumulative case count of 1108 cases per 10,000 population and Wisconsin the highest with 3142 cases per 10,000 population for the two-year period (Table 1). Multiple states have spatial units with sub-populations that are missing case data (Table S1). See Supplementary Figs. S1–3 for depictions of the distribution of COVID-19 across neighborhoods within states.
Neighborhood-level trends in COVID-19 burden differ by state
We calculated the median case count per 10,000 population and the coefficient of variation (CV) by ZCTA and census tract (Table 1). The median case count per 10,000 population at the neighborhood-level mirrors the trends of the cumulative case count per 10,000. The CV, however, gives an indication of the neighborhood-level variability in mean case counts within each state, and there are notable state-level differences in the CV of the neighborhood-level cases counts. For example, the highest CV’s are observed in Vermont (CV = 0.84) and Maine (0.53), which demonstrates a higher within-state variability in the mean of COVID-19 cases at the neighborhood-level. In contrast, the low CVs for states such as Wisconsin (CV = 0.17) and Delaware (CV = 0.19) suggest a more homogenous spread of COVID-19 cases across neighborhoods within those respective states.
Correlations between neighborhood social factors and neighborhood COVID-19 burden differ within and between states
To address the second research question, whether there are features of the neighborhood social environment that are correlated with COVID-19 burden within a state, we used a series of univariate Poisson regression models to estimate the incidence rate ratio (IRR) of case counts cumulatively per 10,000 population for each neighborhood within each state. We used the recent framework by Noppert, Hegde, and Kubale (2022) to select features of the neighborhood environment that may be particularly relevant for understanding COVID-19 burden, and that may also lend themselves to intervention65. Their framework posits that infectious disease burden is a function of two primary pathways which may operate at both the individual- and neighborhoods-level: exposure, factors that increase the probability of exposure to an infectious pathogen, and susceptibility, factors that increase the likelihood of being infected if exposed. See Fig. 1 for the conceptual diagram used to guide the selection of neighborhood social and physical features.
The framework describes the neighborhood environment as one mechanism through which structural disadvantage operates to affect risk of infectious disease65. The neighborhood environment, as described in this manuscript, is a broad indicator that includes aspects of both the physical and social environment. For the current investigation, we chose to operationalize the neighborhood environment by first selecting two widely used measures of the neighborhood social environment: neighborhood disadvantage and neighborhood affluence. We modeled neighborhood disadvantage and neighborhood affluence as two separate factors given that they capture two distinct concepts of neighborhood socioeconomic status (SES), which is described further in the Methods section below. Briefly, neighborhood SES is essential to understanding the burden of infectious diseases. Low SES neighborhoods tend to have fewer health resources (i.e., hospitals, grocery stores, pharmacies), a higher proportion of their populations employed in lower wage jobs, or jobs classified as essential work with less ability to work from home or take sick leave when needed, and a higher proportion of the population utilizing public transportation14,19,66. All of these factors increase the probability that an individual is more likely to come into contact with an infectious pathogen, with inadequate protections to prevent infection67. Moreover, there is an inherent stress to living in a low SES neighborhood that may itself make an individual more susceptible to an infectious disease68,69. To begin to capture these dynamics, we examined both neighborhood disadvantage, a reflection of material access to resources, and neighborhood affluence, reflection of the power a community has to advocate for resources.
We also examined correlations between case counts and rurality (census tract or ZCTA-level) and political partisanship at the county-level. In the current U.S. context, political partisanship has been shown to be an indicator for the willingness to engage in public health prevention behaviors including vaccination64,70. We examined correlations with a rurality index (rural-urban commuting area code (RUCA)) given that multiple recent studies have demonstrated how rural and urban communities have fared differently throughout the pandemic49,52. Finally, we examined correlations with neighborhood population density as it is conceptualized as a key mechanism that can increase the probability of exposure to an infectious pathogen.
We observe univariate associations between neighborhood affluence and neighborhood COVID-19 burden for many states (Tables 2–6), however, the magnitude and direction of the association differ widely between states. In 52% of states, neighborhood affluence is statistically significantly, negatively correlated with neighborhood COVID-19 burden (Table S2). In these states, neighborhoods in the highest quartile of affluence (Q4; i.e., the most affluent) have significantly lower COVID-19 burden compared to neighborhoods in the lowest quartile of affluence (Q1). For example, in Rhode Island neighborhoods, we observe a 30% lower (b = 0.70, 95% CI: 0.65–0.76) incidence rate of COVID-19 comparing neighborhoods in the highest quartile of affluence (Q4) to neighborhoods in the lowest quartile of affluence (Q1). In New Mexico, neighborhoods in the highest quartile of affluence (Q4) have a 29% lower (b = 0.71, 95% CI: 0.62–0.82) rate of COVID-19 compared to neighborhoods in the lowest quartile (Q1).
In 62% of states, we observe a positive, statistically significant correlation between neighborhood disadvantage and COVID-19 burden wherein higher quartiles of neighborhood disadvantage (i.e., those more disadvantaged) are associated with a higher rate of COVID-19 (Tables 2–6 and S2). For example, in the highest quartile (Q4) of disadvantaged neighborhoods in Vermont, the rate is 2.86 (95% CI: 1.02–7.98) times that of neighborhoods in the lowest quartile of disadvantage (Q1, i.e., those least disadvantaged). In Oregon, neighborhoods in the highest quartile of disadvantage (Q4) have 1.40 (95% CI: 1.29–1.52) times the rate of COVID-19 compared to neighborhoods in the lowest quartile of disadvantage (Q1).
We do not see any consistent patterns among the correlations with population density (Tables 2–6 and S2).
We also examine correlations between political partisanship and COVID-19. For county-level political partisanship, we find that in 38% of states, there is a statistically significant, positive correlation between county-level political partisanship and neighborhood COVID-19 burden (Table S2). That is, neighborhoods in which a greater proportion of the votes were cast for Republican candidates in senate and presidential races from 2012-2018 have a higher burden of COVID-19 at the neighborhood-level. In univariate analyses, we operationalized the partisanship variable such that a one-unit increase in the political partisanship variable is equivalent to a 10% increase in Republican votes (Tables 2–6). For example, in Maine, a 10% increase in Republican votes cast is associated with a 12% increase in the COVID-19 rates in neighborhoods (b = 1.12, 95% CI: 1.08–1.17). In Illinois, a 10% increase in Republican votes cast is associated with a 7% increase in the COVID-19 rate (b = 1.07, 95% CI: 1.05-1.08).
However, for several states (24%) we simultaneously observe a strong, negative correlation between county-level political partisanship and COVID-19 burden (Tables 2–6). In Nevada, for example, a 10% increase in the percentage of votes cast for Republican candidates is associated with a 13% lower rate of COVID-19 (b = 0.87, 95% CI: 0.82–0.91). Similarly, in Florida, a 10% increase in the percentage of votes cast for Republican candidates is associated with a 13% lower rate of COVID-19 (b = 0.87, 95% CI: 0.78–0.97).
Finally, we observe a statistically significant, negative correlation between the RUCA categories and COVID-19 burden for 48% of states (Tables 2–6, Table S2). In Rhode Island, neighborhoods classified as rural have a 59% lower rate of COVID-19 compared to neighborhoods classified as metropolitan (b = 0.41 95% CI: 0.36–0.47). In Arizona, neighborhoods classified as rural have a 45% lower rate of COVID-19 compared to neighborhoods classified as metropolitan (b = 0.55, 95% CI: 0.4–0.74) (Table 2). While there are several states for whom we observe a positive correlation between the RUCA and COVID-19 burden, the correlations are small and not statistically significant.
Discussion
Our results are the first findings from the COVID Neighborhood Project (CONEP), a data effort designed to collate spatially-referenced COVID-19 data at the neighborhood-level across the U.S. The findings from this study are suggestive that the state context may matter for determining the distribution of COVID-19 across neighborhoods. For some states, there is wide variation in the neighborhood COVID-19 burden (i.e., Maine, Vermont, Pennsylvania), a signal that some neighborhoods account for a disproportionate burden of COVID-19 cases compared to other neighborhoods in the same state. In contrast, for other states, the burden of COVID-19 is more homogenously distributed across neighborhoods (i.e., Delaware, Wisconsin, Louisiana). Though the results from the current investigation are preliminary and descriptive in nature, they underscore that local neighborhood patterns and dynamics play an underappreciated role in the distribution and intensity of COVID-19 burden and the long-term sequalae that will be endured. These findings also hint at the complex relationship between state- and local-based policies, neighborhood features, and the myriad ways in which the interaction of these area-based forces may have influenced the COVID-19 burden felt by millions. Indeed, policy makers should be wary in crafting a one-size-fits-all approach for pandemic mitigation and recovery efforts. Our results suggest that among the states included in this analysis, there may be no single, unifying story to describe how COVID-19 has been distributed across neighborhoods within states in the U.S.
Our findings are not only consistent with other investigations conducted in the U.S. but in various global settings as well. For example, in a study of the spatiotemporal dynamics of the spread of COVID-19 in Brazil in 2020, Castro et al, found a diverse array of factors explained how the virus was distributed across various states within Brazil. There were complex interactions between state- and local-level policy, socioeconomic, and political environments that shaped the distribution of COVID-19 both within- and between states71. In a study examining trends in COVID-related intensive care unit admissions in Sweden, Kawalerowicz et al. found that individuals living in neighborhoods that were classified as rural and disadvantaged had a higher risk of ICU admission72. Studies in the United Kingdom (U.K.) have also reported findings that neighborhood deprivation has indeed shaped the distribution of COVID-19 burden but cannot be divorced from individual-level attributes of racial and ethnic identification and socioeconomic conditions73,74. The studies above demonstrate that the complex social and environmental dynamics shaping the COVID-19 pandemic have been observed across multiple country contexts. We resonate with Bollyky et al. in that inequities on the basis of race/ethnicity and socioecomic status and political polarization including politicizing of the pandemic are not unique to the U.S. context1. Collectively, therefore, findings from mutiple countries, including our own, may begin to shed light on how the increasingly complicated socioeconomic, political, and environmental context shapes infectious disease spread.
Historically, there have been numerous studies relating aspects of the social and built neighborhood environment to infectious disease in the U.S.56,75,76,77,78,79. For many of these studies, a traditional paradigm prevails in which more disadvantaged neighborhoods experience a higher burden of disease55,56,76. While our study did not apply a causal framework, our initial findings support the paradigm of an association between disadvantage and higher infectious burden but only for some states. Historically accepted patterns of the relationship between the neighborhood environment and infectious disease burden are challenged in other states; this paradigm is more nuanced and complex than previously imagined. While we are limited by the data we have been able to collect thus far both in geographic scope (i.e., not all 50 states) and other key confounding variables (e.g., neighborhood vaccination rates, access to vaccination sites, access to health facilities, and test positivity rates at the local area level), these broad signals offer a window into the complicated relationship that exists between aspects of the social and built neighborhood environment, state and local policy, and COVID-19 burden. As shown in other studies, there are state-specific behaviors and policies that have shaped the variation in the COVID-19 burden across the U.S.64,80,81,82,83. Our findings lay the groundwork for future work that can build off of our results to more explicitly examine and test how state-specific behaviors interact with local area-level concentrated disadvantage or affluence.
One such example of this interaction is with regards to rural populations. In one of the few studies that focused exclusively on understanding the impacts of COVID-19 on rural populations in the U.S., Mueller et al. found extensive reports of the negative consequences from COVID-19 among rural populations including in unemployment rates, perceptions of the local economy, and impact on their overall lives and mental wellbeing52. They reported a 9.7 percentage point increase in the 2020 unemployment rate in the rural communities included in their sample compared to the year before the pandemic52. This contrasts with a national increase in the unemployment rate of only 7.4 percentage points. With increasing urbanization, rural populations represent a unique, and diverse community in the U.S., one particularly vulnerable to long-term social and economic consequences from COVID-19 and whom have often been overlooked in the pandemic response84,85,86.
There were multiple strengths to the current study. To the best of our knowledge, we are among one of the first data collation efforts to attempt to collect in-depth, spatially-referenced case data at the neighborhood-level for the entire U.S., and the only to link these spatially-referenced case data at the census tract or ZIP code level with features of the neighborhood built and social environment from the NANDA repository. Our results have implications for both public health practice and policy and for how we understand the health of the U.S. population going forward. They also lay the groundwork for developing effective prevention and mitigation strategies to address continuing inequities in pandemic-related consequences. These data provide the foundation for future studies focused on the impacts of pandemic-related changes to the neighborhood environment and population health trends, and highlight the need to gather robust neighborhood-level disease, long-term sequelae, and environmental metrics for COVID-19 across the U.S. given the heterogeneity we observed by state.
While this study currently advances our understanding of how COVID-19 has differentially impacted neighborhoods across 21 states in the U.S., there are limitations that should be considered when interpreting these results and that may also guide future investigations. Given the emergency nature of the pandemic and the independence of state public health institutions from federal jurisdiction, each state set up surveillance systems differently, including defining different inclusion criteria and methods for counting cases, and in the selection of the types of health facilities surveilled (22-23). For example, if a state only included laboratory-confirmed cases, their case counts were likely an underestimate of the true case counts in a population, however, this was not standardized. Laboratory-confirmed case counts may miss cases identified through at-home testing which increased in the later stages of the pandemic. Further, state case data often differed in geographic and temporal coverage, also in part due to the rise in at home testing beginning from late 2021 onwards and other advances or policy changes, which made more nuanced comparisons by state difficult. While examining trends in the aggregate may mitigate some of the state-to-state differences, comparisons across states should still be made with caution; accounting for the decrease in case count accuracy over time is difficult even for the most robust surveillance teams.
Moreover, we only have data on incident infections. Thus, the case data could reflect repeat infections occurring in the same person. However, we nonetheless can detect neighborhoods that have had the highest COVID-19 burden. Additionally, we do not have information on co-morbid conditions that occurred with COVID-19 infections, which may serve as important underlying drivers of COVID-19 infections and occur more frequently among structurally disadvantaged populations87. Future analyses should incorporate data on the prevalence of key co-morbid conditions into statistical models.
Importantly, as state case counts reflect not only the availability of testing facilities and infrastructure in place to report positive test results but access to such facilities as well, the current results may best be viewed as a proxy indicator of the true underlying trends in COVID-19 case data. In future studies, we plan to collate data on testing sites, test positivity rates, other indicators of the burden of COVID-19 (e.g., wastewater surveillance), and mitigation strategies (e.g., vaccination history) over time to create a more accurate indicator of COVID-19 burden.
Despite the limitations, these findings outline the necessary steps towards a more comprehensive data collation effort and possibly the foundation for a concerted surveillance system across the U.S. Compared to other U.S. spatially-referenced COVID-19 datasets like the Centers for Disease Control and Prevention COVID-19 Data Tracker or the Johns Hopkins University Coronavirus Resource Center, which are both limited to county-level data, harnessing a repository like CONEP will allow researchers and the public to examine more local level trends, while simultaneously accounting for the heterogeneity that exists within counties and across the urban to rural expanse.
As this is the first investigation in a series of studies stemming from CONEP, we will continue to build the CONEP repository to cover all 50 states and build in more contextual data at the state, county, and local levels. Also, it is critical to note that obtaining local-level, finer-scale spatial data is difficult and should involve a deeper discussion of ethics. Calling on public health practitioners, who are often burdened with other real-time tasks, to collect such data may not always allow for the priority it should be given until systems are automated. Still, gathering these data is essential for monitoring health and social well-being in the U.S.
Conclusion
The inequitable distribution of COVID-19 across neighborhoods in the U.S. has consequences both for the current health and economic wellbeing of the American population as well as for the future of population health in the U.S., and specifically population health inequities88,89. Therefore, it is imperative that we interrogate patterns and trends at the local neighborhood-level. Our results represent an initial step to document the complex ways in which the neighborhood social environment may be related to COVID-19 burden and highlight the importance of the local-level for determining patterns of disease risk and resilience. While the traditional paradigm in infectious disease research has long held that poverty increases infectious disease burden, our findings highlight state-level variation, and that a one-size-fits-all approach will not address the unique patterns observed across states in the U.S. By leveraging fine-scale spatially-referenced case data, our findings enhance our understanding of the neighborhood social environment and COVID-19 burden and underscore the continued need for nationwide data for neighborhoods across all states in order to adequately improve the health of populations.
Data availability
All of the individual state-level data are publicly available. We have included information regarding how to obtain the data for each state in the supplement including the necessary links (see Table S3). Efforts are currently underway to work with each individual health department, adhering to their specific data protection procedures, to compile all of the state-level data into a single database that will be publicly available through ICPSR. Further, in the current investigation, we analyzed each state separately and thus downloading each state individually will allow for replicability. For any questions or updates on the process of building a single, national database, please contact the corresponding author. The NANDA data are available through ICPSR and instructions for accessing the NANDA data and the data itself are available at https://www.icpsr.umich.edu/web/ICPSR/series/1920.
Code availability
The code used to generate the results are available at https://doi.org/10.5281/zenodo.1060685690.
References
Bollyky, T. J. et al. Assessing COVID-19 pandemic policies and behaviours and their economic and educational trade-offs across US states from Jan 1, 2020, to July 31, 2022: an observational analysis. Lancet 401, 1341–1360 (2023).
Park, J. Who is hardest hit by a pandemic? Racial disparities in COVID-19 hardship in the US. Int. J. Urban Sci. 25, 149–177 (2021).
Hatef, E., Chang, H.-Y., Kitchen, C., Weiner, J. P. & Kharrazi, H. Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Front. Public Health 8, 571808 (2020).
Boland, M. R. et al. Association of Neighborhood-Level Factors and COVID-19 infection patterns in Philadelphia using spatial regression. AMIA Summits Transl. Sci. Proc. 2021, 545 (2021).
Brown, K. M., Lewis, J. Y. & Davis, S. K. An ecological study of the association between neighborhood racial and economic residential segregation with COVID-19 vulnerability in the United States’ capital city. Ann. Epidemiol. 59, 33–36 (2021).
Bryan, M. S. et al. Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann. Epidemiol. 56, 47–54.e45 (2021).
Consolazio, D. et al. Assessing the impact of individual characteristics and neighborhood socioeconomic status during the COVID-19 pandemic in the provinces of Milan and Lodi. Int. J. Health Serv. 51, 311–324 (2021).
Gu, A., Shafeeq, H., Chen, T. & Gadhoke, P. Factors Associated with COVID-19 Infection, Hospitalization and Death in New York City Neighborhoods. Innov. Pharm. 12, 3 (2021).
Lamb, M. R., Kandula, S. & Shaman, J. Differential COVID‐19 case positivity in New York City neighborhoods: socioeconomic factors and mobility. Influenza Other Respir. Viruses 15, 209–217 (2021).
Levy, B. L., Vachuska, K., Subramanian, S. & Sampson, R. J. Neighborhood socioeconomic inequality based on everyday mobility predicts COVID-19 infection in San Francisco, Seattle, and Wisconsin. Sci. Adv. 8, eabl3825 (2022).
Oluyomi, A. O., Gunter, S. M., Leining, L. M., Murray, K. O. & Amos, C. COVID-19 community incidence and associated neighborhood-level characteristics in Houston, Texas, USA. Int. J. Environ. Res. Public Health 18, 1495 (2021).
Samuels-Kalow, M. E. et al. Neighborhood disadvantage measures and COVID-19 cases in Boston, 2020. Public Health Rep. 136, 368–374 (2021).
Tung, E. L., Peek, M. E., Rivas, M. A., Yang, J. P. & Volerman, A. Association Of Neighborhood Disadvantage With Racial Disparities In COVID-19 Positivity In Chicago: Study examines the association of neighborhood disadvantage with racial disparities in COVID-19 positivity in Chicago. Health Aff. 40, 1784–1791 (2021).
Whittle, R. S. & Diaz-Artiles, A. An ecological study of socioeconomic predictors in detection of COVID-19 cases across neighborhoods in New York City. BMC Med. 18, 1–17 (2020).
Wrigley-Field, E., Garcia, S., Leider, J. P. & Van Riper, D. COVID-19 mortality at the neighborhood level: racial and ethnic inequalities deepened in minnesota in 2020: study examines COVID-19 racial and ethnic inequalities in Minnesota communities. Health Aff. 40, 1644–1653 (2021).
Browning, C. R. & Cagney, K. A. Moving beyond poverty: neighborhood structure, social processes, and health. J. Health Soc. Behav. 44, 552–571 (2003).
Cagney, K. A. Neighborhood age structure and its implications for health. J. Urban Health 83, 827–834 (2006).
Clarke, P. & Nieuwenhuijsen, E. R. Environments for healthy ageing: a critical review. Maturitas 64, 14–19 (2009).
Diez Roux, A. V. & Mair, C. Neighborhoods and health. Ann N Y Acad Sci 1186, 125–145 (2010).
Ross, C. E. & Mirowsky, J. Neighborhood disadvantage, disorder, and health. J. Health Soc. Behav. 42, 258–276 (2001).
Yen, I. H. & Kaplan, G. A. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am. J. Epidemiol. 149, 898–907 (1999).
Yen, I. H., Michael, Y. L. & Perdue, L. Neighborhood environment in studies of health of older adults: a systematic review. Am. J. Prev. Med. 37, 455–463 (2009).
Yang, T.-C., Emily Choi, S.-W. & Sun, F. COVID-19 cases in US counties: roles of racial/ethnic density and residential segregation. Ethn. Health 26, 11–21 (2021).
Sung, B. A spatial analysis of the effect of neighborhood contexts on cumulative number of confirmed cases of COVID-19 in US Counties through October 20 2020. Prev. Med. 147, 106457 (2021).
Andrews, M. R. et al. Spatial clustering of county-level COVID-19 rates in the US. Int. J. Environ. Res. Public Health 18, 12170 (2021).
Saffary, T. et al. Analysis of COVID-19 cases’ spatial dependence in US counties reveals health inequalities. Front. Public Health 8, 579190 (2020).
Thorpe, L. E. & Gourevitch, M. N. Vol. 112. p. 889-892 (American Public Health Association, 2022).
Bilal, U. et al. Tracking COVID-19 inequities across Jurisdictions represented in the Big cities health Coalition (Bchc): The COVID-19 health inequities in Bchc cities dashboard. Am. J. Public Health 112, 904–912 (2022).
Department of Population Health (NYU Langone Health, 2021).
Spoer, B. R. et al. Validation of a neighborhood-level COVID Local Risk Index in 47 large US cities. Health Place 76, 102814 (2022).
Benitez, J., Courtemanche, C. & Yelowitz, A. Racial and ethnic disparities in COVID-19: evidence from six large cities. J. Econ. Race Policy 3, 243–261 (2020).
Zhang, X., Smith, N., Spear, E. & Stroustrup, A. Neighborhood characteristics associated with COVID-19 burden—the modifying effect of age. J. Expo. Sci. Environ. Epidemiol. 31, 525–537 (2021).
Baidal, J. W. et al. Social determinants of health and COVID-19 among patients in New York City. Res. Sq. rs.3.rs-70959 (2020). https://doi.org/10.21203/rs.3.rs-70959/v1.
Kashem, S. B., Baker, D. M., González, S. R. & Lee, C. A. Exploring the nexus between social vulnerability, built environment, and the prevalence of COVID-19: A case study of Chicago. Sustain. Cities Soc. 75, 103261 (2021).
Chan, P. Y., Greene, S. K., woo Lim, S., Fine, A. & Thompson, C. N. Persistent disparities in SARS-CoV-2 test percent positivity by neighborhood in New York City, March 1–July 25, 2020. Ann. Epidemiol. 63, 46–51 (2021).
Bilal, U., Tabb, L. P., Barber, S. & Diez Roux, A. V. Spatial inequities in COVID-19 testing, positivity, confirmed cases, and mortality in 3 US cities: an ecological study. Ann. Intern. Med. 174, 936–944 (2021).
Carrión, D. et al. Neighborhood-level disparities and subway utilization during the COVID-19 pandemic in New York City. Nat. Commun. 12, 1–10 (2021).
Maroko, A. R., Nash, D. & Pavilonis, B. T. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J. Urban Health 97, 461–470 (2020).
Kim, B. et al. COVID-19 testing, case, and death rates and spatial socio-demographics in New York City: an ecological analysis as of June 2020. Health Place 68, 102539 (2021).
Zhang, Y. et al. Socioeconomic variation in characteristics, outcomes, and healthcare utilization of COVID-19 patients in New York City. PLoS ONE 16, e0255171 (2021).
Moreland, A., Alpert, N., Eugene, A., Flores, R. & Taioli, E. A neighborhood analysis of time trends in COVID-19 infection in NYC. J. Commun. Health 47, 143–149 (2022).
Van Holm, E. J., Wyczalkowski, C. K. & Dantzler, P. A. Neighborhood conditions and the initial outbreak of COVID-19: the case of Louisiana. J. Public Health 43, 219–224 (2021).
Cromer, S. J. et al. Geospatial analysis of individual and community-level socioeconomic factors impacting SARS-CoV-2 prevalence and outcomes. MedRxiv https://doi.org/10.1101/2020.09.30.20201830 (2020).
Kiaghadi, A., Rifai, H. S. & Liaw, W. Assessing COVID-19 risk, vulnerability and infection prevalence in communities. PLoS ONE 15, e0241166 (2020).
Oates, G. R. et al. The association between neighborhood social vulnerability and COVID-19 testing, positivity, and incidence in Alabama and Louisiana. J. Community Health 46, 1115–1123 (2021).
Stephen, A. H. et al. The association between household and neighborhood characteristics and COVID-19 related ICU admissions. SSM-Popul. Health 19, 101133 (2022).
Ogedegbe, G. et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Netw. Open 3, e2026881 (2020).
Paul, R., Arif, A., Pokhrel, K. & Ghosh, S. The association of social determinants of health with COVID‐19 mortality in rural and urban counties. J. Rural Health 37, 278–286 (2021).
Cuadros, D. F., Branscum, A. J., Mukandavire, Z., Miller, F. D. & MacKinnon, N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 59, 16–20 (2021).
Rose, D. C. et al. The impact of COVID-19 on farmers’ mental health: a case study of the UK. J. Agromed. 28, 346–364 (2023).
Rifat, S. A. A. & Liu, W. One year into the pandemic: the impacts of social vulnerability on COVID-19 outcomes and urban–rural differences in the conterminous United States. Int. J. Environ. Health Res. 32, 2601–2619 (2022).
Mueller, J. T. et al. Impacts of the COVID-19 pandemic on rural America. Proc. Natl Acad. Sci. USA 118, 2019378118 (2021).
U.S. Census Bureau ZIP Code Tabulation Areas (ZCTAs) <https://www.census.gov/programs-surveys/geography/guidance/geo-areas/zctas.html#:~:text=ZIP%20Code%20Tabulation%20Areas%20(ZCTAs)%20are%20generalized%20areal%20representations%20of,station%20associated%20with%20mailing%20addresses.> (2022).
Oren, E., Narita, M., Nolan, C. & Mayer, J. Neighborhood socioeconomic position and tuberculosis transmission: a retrospective cohort study. BMC Infect. Dis. 14, 227 (2014).
Acevedo-Garcia, D. Residential segregation and the epidemiology of infectious diseases. Soc. Sci. Med. 51, 1143–1161 (2000).
Acevedo-Garcia, D. Zip code-level risk factors for tuberculosis: neighborhood environment and residential segregation in New Jersey, 1985-1992. Am. J. Public Health 91, 734 (2001).
Clarke, P., Noppert, G., Melendez, R., Chenoweth, M. & Gypin, L. National Neighborhood Data Archive (NANDA): Socioeconomic Status and Demographic Characteristics of Census Tracts and ZIP Code Tabulation Areas, United States, 2000-2020. Inter-university Consortium for Political and Social Research [distributor], 2023-04-17. https://doi.org/10.3886/ICPPSR38528.v3.
Ross, C. E., Mirowsky, J. & Pribesh, S. Powerlessness and the amplification of threat: neighborhood disadvantage, disorder, and mistrust. Am. Soc. Rev. 66, 568–591 (2001).
Mohai, P., Lantz, P. M., Morenoff, J., House, J. S. & Mero, R. P. Racial and socioeconomic disparities in residential proximity to polluting industrial facilities: evidence from the Americans’ Changing Lives Study. Am. J. Public Health 99, S649–S656 (2009).
Clarke, P. et al. Cumulative exposure to neighborhood context: consequences for health transitions over the adult life course. Res. Aging 36, 115–142 (2014).
U.S. Department of Agriculture Rural-Urban Commuting Area (RUCA) Codes 2010 https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/documentation/ (2023).
Chenoweth, M., Li, M., Gomez-Lopez, I. N. & Kollman, K. National Neighborhood Data Archive (NANDA): Voter Registration, Turnout, and Partisanship by County, United States, 2004-2018. Inter-university Consortium for Political and Social Research [distributor], 2022-08-31. https://doi.org/10.3886/ICPRS38506.v1.
Chen, H.-F. & Karim, S. A. Relationship between political partisanship and COVID-19 deaths: future implications for public health. J. Public Health 44, 716–723 (2022).
Grossman, G., Kim, S., Rexer, J. M. & Thirumurthy, H. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc. Natl Acad. Sci. USA 117, 24144–24153 (2020).
Noppert, G. A., Hegde, S. T. & Kubale, J. T. Exposure, susceptibility, and recovery: a framework for examining the intersection of the social and physical environment and infectious disease risk. Am. J. Epidemiol. 192, 475–482 (2023).
Lynch, E. E. et al. The legacy of structural racism: associations between historic redlining, current mortgage lending, and health. SSM-Popul. Health 14, 100793 (2021).
McClure, E. S., Vasudevan, P., Bailey, Z., Patel, S. & Robinson, W. R. Racial capitalism within public health—how occupational settings drive COVID-19 disparities. Am. J. Epidemiol. 189, 1244–1253 (2020).
Attar, B. K., Guerra, N. G. & Tolan, P. H. Neighborhood disadvantage, stressful life events and adjustments in urban elementary-school children. J. Clin. Child Psychol. 23, 391–400 (1994).
Cohen, S. et al. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychol. 27, 268 (2008).
Gadarian, S. K., Goodman, S. W. & Pepinsky, T. B. Partisanship, health behavior, and policy attitudes in the early stages of the COVID-19 pandemic. PLoS ONE 16, e0249596 (2021).
Castro, M. C. et al. Spatiotemporal pattern of COVID-19 spread in Brazil. Science 372, 821–826 (2021).
Kawalerowicz, J., Cederström, A., Andersson, E. & Malmberg, B. COVID-19 in The Neighbourhood: The Socio-Spatial Selectivity of Severe COVID-19 Cases in Sweden, March 2020-June 2021 (2022).
Lo, C.-H. et al. Race, ethnicity, community-level socioeconomic factors, and risk of COVID-19 in the United States and the United Kingdom. EClinicalMedicine 38, 101029 (2021).
Harris, R. Exploring the neighbourhood-level correlates of Covid-19 deaths in London using a difference across spatial boundaries method. Health Place 66, 102446 (2020).
Lantos, P. M. et al. Neighborhood disadvantage is associated with high cytomegalovirus seroprevalence in pregnancy. J. Racial Ethn. Health Disparities 5, 782–786 (2018).
Noppert, G. A. et al. Individual-and neighborhood-level contextual factors are associated with Mycobacterium tuberculosis transmission: genotypic clustering of cases in Michigan, 2004–2012. Ann. Epidemiol. 27, 371–376.e375 (2017).
Grantz, K. H. et al. Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918. Proc. Natl Acad. Sci. USA 113, 13839–13844 (2016).
Chowell, G., Bettencourt, L. M., Johnson, N., Alonso, W. J. & Viboud, C. The 1918–1919 influenza pandemic in England and Wales: spatial patterns in transmissibility and mortality impact. Proc. R. Soc. B: Biol. Sci. 275, 501–509 (2008).
Dalziel, B. D. et al. Urbanization and humidity shape the intensity of influenza epidemics in US cities. Science 362, 75–79 (2018).
Wilson, F. A. & Stimpson, J. P. US policies increase vulnerability of immigrant communities to the COVID-19 pandemic. Ann. Glob. Health 86, 57 (2020).
Lyu, W. & Wehby, G. L. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates In The US: study examines impact on COVID-19 growth rates associated with state government mandates requiring face mask use in public. Health Aff. 39, 1419–1425 (2020).
Cowger, T. L. et al. Lifting universal masking in schools—Covid-19 incidence among students and staff. N. Engl. J. Med. 387, 1935–1946 (2022).
Feyman, Y., Bor, J., Raifman, J. & Griffith, K. N. Effectiveness of COVID-19 shelter-in-place orders varied by state. PLoS ONE 15, e0245008 (2020).
Lichter, D. T. Immigration and the new racial diversity in rural America. Rural Sociol. 77, 3–35 (2012).
Lichter, D. T. & Brown, D. L. Rural America in an urban society: changing spatial and social boundaries. Annu. Rev. Sociol. 37, 565–592 (2011).
Lichter, D. T., Parisi, D. & Taquino, M. C. Toward a new macro-segregation? Decomposing segregation within and between metropolitan cities and suburbs. Am. Sociol. Rev. 80, 843–873 (2015).
Tai, D. B. G., Shah, A., Doubeni, C. A., Sia, I. G. & Wieland, M. L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin. Infect. Dis. 72, 703–706 (2021).
Arias, E., Tejada-Vera, B., Kochanek, K. D. & Ahmad, F. B. Provisional Life Expectancy Estimates For 2021 (2022).
Noppert, G. A., Duchowny, K. A. & Clarke, P. J. Declining US life expectancy since COVID-19--structural inequities foreshadow future fallout. Vol. 378 (British Medical Journal Publishing Group, 2022).
Noppert, G.A., & Melendez R. gracenoppert/CONEP- v1.0 https://doi.org/10.5281/zenodo.10606856 (2024).
Acknowledgements
This study was partially funded by the U.S. National Institutes of Health, National Institute on Aging Network on Life Course Dynamics and Disparities in the 21st Century R24 AG045061 (PI Noppert). Funding support was also provided by the National Institutes of Health, National Institute of Nursing Research, and National Institute of Minority Health and Health Disparities U01 NR020556 (MPI Noppert and Clarke). KAD received support for this work from the National Institutes of Health, National Institute on Aging R00 AG066846 and JTK received support for this work from the National Institutes of Health, National Institute on Aging U24 AG076462. The authors are deeply grateful to the health departments who shared their data with us. Additionally, this work has been done as part of the Social Environmental and Equity in Infectious Disease Lab—an interdisciplinary collaborative between the University of Michigan and Johns Hopkins University. COVID-19 Data Health Department Acknowledgements. Data for Arizona were obtained through public download from the Arizona Department of Health Services (ADHS). ADHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Delaware were obtained through public download from the Delaware Department of Health and Social Services (DHSS). DHSS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Florida were obtained through public download from the Florida Department of Health (FDOH). FDOH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Illinois were obtained through public download from the Illinois Department of Public Health (IDPH). IDPH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Indiana were obtained through public download from the Indiana Department of Health (IDOH). IDOH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Louisiana were obtained through public download from the Louisiana Department of Health (LDH). LDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Maine were obtained through public download from the Maine Department of Health and Human Services (Maine DHHS). Maine DHHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Maryland were obtained through public download from the Maryland Department of Health (MDH). MDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Minnesota were obtained through a data practices request to the Minnesota Department of Health (MDH). MDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Nevada were obtained through a public records request to the Nevada Department of Health and Human Services (Nevada DHHS) and the assistance of Kavita Batra. Nevada DHHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for New Mexico were obtained through a public records request from the New Mexico Department of Health (NMDOH). NMDOH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for New York were obtained through public download from the New York State Department of Health (NYSDOH). NYSDOH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for North Carolina were obtained through public download from the North Carolina Department of Health and Human Services (NCDHHS). NCDHHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Ohio were obtained through public download from the Ohio Department of Health (ODH). ODH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Oklahoma were obtained through public download from the Oklahoma State Department of Health (OSDH). OSDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Oregon were obtained through public download from the Oregon Department of Human Services (ODHS). ODHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Pennsylvania were obtained through public download from the Pennsylvania Department of Health (PDH). PDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Rhode Island were obtained through a request to the Center for Health Data and Analytics, COVID-19 Quant Team, Rhode Island Department of Health (RIDOH). RIDOH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Vermont were obtained through a public records request to the Vermont Department of Health (VDH), and the assistance of Lucy Lincoln. VDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Virginia were obtained through public download from the Virginia Department of Health (VDH). VDH is not responsible for the author’s analysis, opinions, and conclusions contained in this document. Data for Wisconsin were obtained through public download from the Wisconsin Department of Health Services (Wisconsin DHS). Wisconsin DHS is not responsible for the author’s analysis, opinions, and conclusions contained in this document.
Author information
Authors and Affiliations
Contributions
G.N., P.C. and S.H. conceptualized and designed the study, and led the efforts to interpret the results. A.H. led the efforts to obtain the state-level data. R.M. carried out the statistical analysis. G.N., P.C., A.H. and S.H. wrote the manuscript with input from all authors. J.K. and K.D. provided critical input and feedback on the manuscript and assisted with editing. All authors provided critical feedback on the manuscript and helped shape the research, analysis, and manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Blake Byron Walker and Alina Schnake-Mahl for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Noppert, G.A., Clarke, P., Hoover, A. et al. State variation in neighborhood COVID-19 burden across the United States. Commun Med 4, 36 (2024). https://doi.org/10.1038/s43856-024-00459-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-024-00459-1