Abstract
We developed models for individualized risk prediction of cognitive decline in mild cognitive impairment (MCI) using plasma biomarkers of β-amyloid (Aβ), tau and neurodegeneration. A total of 573 patients with MCI from the Swedish BioFINDER study and the Alzheimer’s Disease Neuroimaging Initiative (ADNI) were included in the study. The primary outcomes were longitudinal cognition and conversion to Alzheimer’s disease (AD) dementia. A model combining tau phosphorylated at threonine 181 (P-tau181) and neurofilament light (NfL), but not Aβ42/Aβ40, had the best prognosis performance of all models (area under the curve = 0.88 for 4-year conversion to AD in BioFINDER, validated in ADNI), was stronger than a basic model of age, sex, education and baseline cognition, and performed similarly to cerebrospinal fluid biomarkers. A publicly available online tool for individualized prognosis in MCI based on our combined plasma biomarker models is introduced. Combination of plasma biomarkers may be of high value to identify individuals with MCI who will progress to AD dementia in clinical trials and in clinical practice.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Plasma and CSF data from ADNI were downloaded from https://ida.loni.usc.edu. Anonymized data from the BioFINDER study will be shared by request from a qualified academic investigator for the sole purpose of replicating procedures and results presented in this Article and as long as the data transfer is in agreement with European Union legislation on general data protection regulation and decisions by the Ethical Review Board of Sweden and Region Skåne, which should be regulated by a material transfer agreement.
Code availability
The code that support the findings of this study is available from the corresponding author upon request. All models were built using publicly available packages and functions in the R programming language.
References
World Alzheimer Report 2019 (Alzheimer’s Disease International, 2019).
Winblad, B. et al. Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol. 15, 455–532 (2016).
Burnham, S. C. et al. The dawn of robust individualised risk models for dementia. Lancet Neurol. 18, 985–987 (2019).
Abbasi, J. Promising results in 18-month analysis of Alzheimer drug candidate. J. Am. Med. Assoc. 320, 965 (2018).
Buchhave, P. et al. Cerebrospinal fluid levels of β-amyloid 1–42, but not of tau, are fully changed already 5 to 10 years before the onset of Alzheimer dementia. Arch. Gen. Psychiatry 69, 98–106 (2012).
Hansson, O. et al. CSF biomarkers of Alzheimer’s disease concord with amyloid-β PET and predict clinical progression: a study of fully automated immunoassays in BioFINDER and ADNI cohorts. Alzheimers Dement. 14, 1470–1481 (2018).
Rabinovici, G. D. et al. Association of amyloid positron emission tomography with subsequent change in clinical management among Medicare beneficiaries with mild cognitive impairment or dementia. J. Am. Med. Assoc. 321, 1286–1294 (2019).
Ossenkoppele, R. et al. Discriminative accuracy of [18F]flortaucipir positron emission tomography for Alzheimer disease vs other neurodegenerative disorders. J. Am. Med. Assoc. 320, 1151–1162 (2018).
Jack, C. R. Jr et al. NIA-AA research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement. 14, 535–562 (2018).
Palmqvist, S. et al. Performance of fully automated plasma assays as screening tests for Alzheimer disease-related β-amyloid status. JAMA Neurol. 76, 1060–1069 (2019).
Janelidze, S. et al. Plasma P-tau181 in Alzheimer’s disease: relationship to other biomarkers, differential diagnosis, neuropathology and longitudinal progression to Alzheimer’s dementia. Nat. Med. 26, 379–386 (2020).
Karikari, T. K. et al. Blood phosphorylated tau 181 as a biomarker for Alzheimer’s disease: a diagnostic performance and prediction modelling study using data from four prospective cohorts. Lancet Neurol. 19, 422–433 (2020).
Thijssen, E. H. et al. Diagnostic value of plasma phosphorylated tau181 in Alzheimer’s disease and frontotemporal lobar degeneration. Nat. Med. 26, 387–397 (2020).
Zetterberg, H. Neurofilament light: a dynamic cross-disease fluid biomarker for neurodegeneration. Neuron 91, 1–3 (2016).
Quiroz, Y. T. et al. Plasma neurofilament light chain in the presenilin 1 E280A autosomal dominant Alzheimer’s disease kindred: a cross-sectional and longitudinal cohort study. Lancet Neurol. 19, 513–521 (2020).
Mielke, M. M. et al. Plasma phospho-tau181 increases with Alzheimer’s disease clinical severity and is associated with tau- and amyloid-positron emission tomography. Alzheimers Dement. 14, 989–997 (2018).
Mattsson, N., Cullen, N. C., Andreasson, U., Zetterberg, H. & Blennow, K. Association between longitudinal plasma neurofilament light and neurodegeneration in patients with Alzheimer disease. JAMA Neurol. 76, 791–799 (2019).
Palmqvist, S. et al. Discriminative accuracy of plasma phospho-tau217 for Alzheimer disease vs other neurodegenerative disorders. J. Am. Med. Assoc. 324, 772–781 (2020).
Van Maurik, I. S. et al. Interpreting biomarker results in individual patients with mild cognitive impairment in the Alzheimer’s Biomarkers In Daily Practice (ABIDE) project. JAMA Neurol. 74, 1481–1491 (2017).
Van Maurik, I. S. et al. Biomarker-based prognosis for people with mild cognitive impairment (ABIDE): a modelling study. Lancet Neurol. 18, 1034–1044 (2019).
Gomersall, T., Smith, S. K., Blewett, C. & Astell, A. ‘It’s definitely not Alzheimer’s’: perceived benefits and drawbacks of a mild cognitive impairment diagnosis. Br. J. Health Psychol. 22, 786–804 (2017).
Ossenkoppele, R. et al. Associations between tau, Aβ, and cortical thickness with cognition in Alzheimer disease. Neurology 92, e601–e612 (2019).
Mattsson-Carlgren, N. et al. Aβ deposition is associated with increases in soluble and phosphorylated tau that precede a positive Tau PET in Alzheimer’s disease. Sci. Adv. 6, eaaz2387 (2020).
Leuzy, A. et al. Diagnostic performance of RO948 F 18 Tau positron emission tomography in the differentiation of Alzheimer disease from other neurodegenerative disorders. JAMA Neurol. 77, 955–965 (2020).
Doecke, J. D. et al. Total Aβ42/Aβ40 ratio in plasma predicts amyloid-PET status, independent of clinical AD diagnosis. Neurology 94, e1580–e1591 (2020).
Mattsson, N., Andreasson, U., Zetterberg, H. & Blennow, K. Alzheimer’s Disease Neuroimaging Initiative Association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol. 74, 557–566 (2017).
Kuhlmann, J. et al. CSF Aβ1–42—an excellent but complicated Alzheimer’s biomarker—a route to standardisation. Clin. Chim. Acta 467, 27–33 (2017).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern. Med. 256, 183–194 (2004).
Petrazzuoli, F. et al. Brief cognitive tests used in primary care cannot accurately differentiate mild cognitive impairment from subjective cognitive decline. J. Alzheimers Dis. 75, 1191–1201 (2020).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34, 939–944 (1984).
Ovod, V. et al. Amyloid β concentrations and stable isotope labeling kinetics of human plasma specific to central nervous system amyloidosis. Alzheimers Dement. 13, 841–849 (2017).
Akaike, H. Likelihood of a model and information criteria. J. Econom. 16, 3–14 (1981).
Burnham K. P. & Anderson D. R. Model Selection and Multimodel Inference (Springer, 2002).
Acknowledgements
Work at the authors’ laboratory at Lund University was supported by the Swedish Research Council, the Wallenberg Center for Molecular Medicine, the Knut and Alice Wallenberg Foundation, Lund University’s Medical Faculty, Region Skåne, the Marianne and Marcus Wallenberg Foundation, the Strategic Research Area MultiPark (Multidisciplinary Research focused on Parkinson’s Disease) at Lund University, the Swedish Alzheimer’s Foundation, the Swedish Brain Foundation, the Swedish Medical Association, the Konung Gustaf V:s och Drottning Victorias Frimurarestiftelse, the Bundy Academy, the Skåne University Hospital Foundation and the Swedish federal government under the ALF agreement. Data collection and sharing for the ADNI part of the study was funded by the ADNI (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). The ADNI is funded by the National Institute on Aging and the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie; Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; Bioclinica; Biogen; Bristol Myers Squibb; CereSpir; Cogstate; Eisai; Elan Pharmaceuticals; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche and its affiliated company Genentech; Fujirebio; GE Healthcare; IXICO; Janssen Alzheimer Immunotherapy Research and Development; Johnson & Johnson Pharmaceutical Research and Development; Lumosity; Lundbeck; Merck & Co.; Meso Scale Diagnostics; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Author information
Authors and Affiliations
Contributions
A.L., N.M.-C. and O.H. conceived of the study. A.L. and N.C.C. performed the statistical analysis. E.S., S.P. and O.H. recruited participants and collected clinical data. H.Z., L.S., J.A.A., J.L.D., K.B., N.K.P., P.P. and S.J. were responsible for the biochemical analyses. N.M.-C. developed an online tool implementing the statistical models. A.L., N.M.-C., L.S., J.A.A., P.P., N.M.C. and O.H. drafted the initial manuscript. All authors contributed to revision and editing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
N.C.C., A.L., S.P., S.J. and N.M.-C. declare no competing interests. P.P., L.S. and J.A.A. are current employees of Araclon Biotech. N.K.P. and J.L.D. are employees and stockholders of Eli Lilly and Company. H.Z. has served on scientific advisory boards for Denali, Roche Diagnostics, Wave, Samumed, Siemens Healthineers, Pinteon Therapeutics and CogRx and has delivered lectures in symposia sponsored by Fujirebio, AlzeCure and Biogen. K.B. has served as a consultant on advisory boards or data monitoring committees for Abcam, Axon, Biogen, JOMDD/Shimadzu, Julius Clinical, Lilly, MagQu, Novartis, Roche Diagnostics and Siemens Healthineers and is a co-founder of Brain Biomarker Solutions in Gothenburg, which is a part of the GU Ventures Incubator Program. O.H. has acquired research support (for the institution) from Roche, Pfizer, GE Healthcare, Biogen, Eli Lilly and AVID Radiopharmaceuticals. In the past 2 years, he has received consultancy/speaker fees (paid to the institution) from Biogen and Roche. E.S. has no competing interests.
Additional information
Peer review information Nature Aging thanks Suzanne Schindler, Charlotte Teunissen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Association between plasma biomarkers in MCI patients in the BioFINDER model selection/prognostic validation cohort.
This figure shows the association between the different possible combinations of ATN plasma biomarkers (left to right: a, plasma P-tau181 vs plasma Aβ42/Aβ40; b, plasma NfL vs plasma P-tau181; and c, plasma Aβ42/Aβ40 vs plasma NfL). Each filled circle represents a single MCI patient from the BioFINDER cohort (n=148); the histograms above the scatterplots show the distribution of concentration values for the plasma biomarker on the x-axis (that is panel A, Aβ42/Aβ40; panel B, P-tau181; panel C, NfL). The blue lines (solid and dashed) indicate the cutoff values for each biomarker.
Extended Data Fig. 2 Association between CSF biomarkers in MCI patients in the BioFINDER model selection/prognostic validation cohort.
This figure shows the association between the different possible combinations of ATN CSF biomarkers (left to right: a, CSF P-tau181 vs CSF Aβ42/Aβ40; b, CSF NfL vs CSF P-tau181; and c, CSF Aβ42/Aβ40 vs CSF NfL). Each filled circle represents a single MCI patient from the BioFINDER cohort (n=148); the histograms above the scatterplots show the distribution of concentration values for the plasma biomarker on the x-axis (that is panel A, Aβ42/Aβ40; panel B, P-tau181; panel C, NfL).
Extended Data Fig. 3 Association between plasma biomarkers in MCI patients in the ADNI model selection cohort.
This figure shows the association between the different possible combinations of ATN plasma biomarkers (left to right: a, plasma P-tau181 vs plasma Aβ42/Aβ40; b, plasma NfL vs plasma P-tau181; and c, plasma Aβ42/Aβ40 vs plasma NfL). Each filled circle represents a single MCI patient from the ADNI selection cohort (n=86); the histograms above the scatterplots show the distribution of concentration values for the plasma biomarker on the x-axis (that is panel A, Aβ42/Aβ40; panel B, P-tau181; panel C, NfL). The blue lines (solid and dashed) indicate the cutoff values for each biomarker.
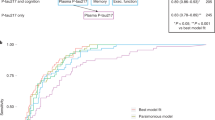
Extended Data Fig. 4 ROC curves for all models in the model selection analysis with four-year conversion to AD dementia as outcome.
This figure shows ROC curves derived from the model selection analysis with four-year conversion to AD dementia as outcome. AUC values were the following in the BioFINDER cohort: Basic Model = 0.70, ATN=0.88, AT=0.86, AN=0.80, TN=0.88, A=0.73, T=0.86, N=0.79. AUC values were the following in the ADNI cohort: Basic Model = 0.74, ATN=0.88, AT=0.86, AN=0.79, TN=0.89, A=0.75, T=0.85, N=0.73. Full data is available in Supplementary Table 2.
Extended Data Fig. 5 Association between plasma biomarkers in MCI patients in the ADNI prognostic validation cohort.
Scatterplot showing plasma NfL versus plasma P-tau181 for the ADNI prognostic validation cohort (n=483). Each filled circle represents a single MCI patient; the histograms above the scatterplots show the distribution of concentration values for plasma P-tau181. The blue lines (solid and dashed) indicate the cutoff values for each biomarker.
Extended Data Fig. 6 Online individualized risk prediction tool.
Screenshots from our webtool predictprogression.com with predictions for a 70-year female with mild cognitive impairment and baseline MMSE 27. The upper panels (A) show predicted MMSE (left) and probability of conversion to AD dementia (right) at 2 and 4 years in a scenario where plasma Aβ42/Aβ40, P-tau181 and NfL are negative. In the lower panels (B), predicted MMSE (left) and probability of conversion to AD dementia (right) are shown at 2 and 4 years in a scenario where plasma Aβ42/Aβ40, P-tau181 and NfL are positive. In both A and B, the dark blue ribbons are 95% confidence interval of the estimates and the light blue ribbon are 90% prediction intervals. The predictions are derived from linear and logistic regression models that were established in the BioFINDER study on non-demented individuals with mild cognitive impairment.
Supplementary information
Supplementary Information
Supplementary notes, figure captions (for Extended Data Figs. 1–6) and Tables 1–16.
Source data
Source Data Fig. 2
Statistics for different ATN models.
Source Data Fig. 3
Statistics for different ATN models.
Rights and permissions
About this article
Cite this article
Cullen, N.C., Leuzy, A., Palmqvist, S. et al. Individualized prognosis of cognitive decline and dementia in mild cognitive impairment based on plasma biomarker combinations. Nat Aging 1, 114–123 (2021). https://doi.org/10.1038/s43587-020-00003-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-020-00003-5
This article is cited by
-
A blood-based biomarker workflow for optimal tau-PET referral in memory clinic settings
Nature Communications (2024)
-
The impact of exercise on blood-based biomarkers of Alzheimer’s disease in cognitively unimpaired older adults
GeroScience (2024)
-
Highly accurate blood test for Alzheimer’s disease is similar or superior to clinical cerebrospinal fluid tests
Nature Medicine (2024)
-
Plasma brain-derived tau is an amyloid-associated neurodegeneration biomarker in Alzheimer’s disease
Nature Communications (2024)
-
Profiling of plasma biomarkers in the context of memory assessment in a tertiary memory clinic
Translational Psychiatry (2023)