Abstract
The microbiome is a predictor of clinical outcome in patients receiving allogeneic hematopoietic stem cell transplantation (allo-SCT). Microbiota-derived metabolites can modulate these outcomes. How bacteria, fungi and viruses contribute to the production of intestinal metabolites is still unclear. We combined amplicon sequencing, viral metagenomics and targeted metabolomics from stool samples of patients receiving allo-SCT (n = 78) and uncovered a microbiome signature of Lachnospiraceae and Oscillospiraceae and their associated bacteriophages, correlating with the production of immunomodulatory metabolites (IMMs). Moreover, we established the IMM risk index (IMM-RI), which was associated with improved survival and reduced relapse. A high abundance of short-chain fatty acid-biosynthesis pathways, specifically butyric acid via butyryl-coenzyme A (CoA):acetate CoA-transferase (BCoAT, which catalyzes EC 2.8.3.8) was detected in IMM-RI low-risk patients, and virome genome assembly identified two bacteriophages encoding BCoAT as an auxiliary metabolic gene. In conclusion, our study identifies a microbiome signature associated with protective IMMs and provides a rationale for considering metabolite-producing consortia and metabolite formulations as microbiome-based therapies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
Microbial sequencing (bacterial and fungal amplicon data and viral metagenomic sequencing data) that support the findings of this study have been deposited at the European Nucleotide Archive under accession number PRJEB53547 (https://www.ebi.ac.uk/ena/browser/view/PRJEB53547). MS data have been deposited at Zenodo under accession number 6603017 (https://zenodo.org/record/6603017). Both repositories are annotated with clinical metadata. All other data supporting the findings of this study are available from the corresponding author on reasonable request. The stool samples analyzed in this study comprised a unique biosample collection and have been expended for the analyses performed in this study. No additional material is available. Source data are provided with this paper.
Code availability
The scripts and packages used for whole shotgun metagenomic sequencing, viral metagenomic sequencing and MOFA have been deposited at GitHub (https://github.com/guardianre/MOFA-in-allo-SCT.git).
References
Zeiser, R. & Blazar, B. R. Acute graft-versus-host disease — biologic process, prevention, and therapy. N. Engl. J. Med. 377, 2167–2179 (2017).
Holler, E. et al. Metagenomic analysis of the stool microbiome in patients receiving allogeneic stem cell transplantation: loss of diversity is associated with use of systemic antibiotics and more pronounced in gastrointestinal graft-versus-host disease. Biol. Blood Marrow Transpl. 20, 640–645 (2014).
Stoma, I. et al. Compositional flux within the intestinal microbiota and risk for bloodstream infection with gram-negative bacteria. Clin. Infect. Dis. 73, e4627–e4635 (2021).
Golob, J. L. et al. Stool microbiota at neutrophil recovery is predictive for severe acute graft vs host disease after hematopoietic cell transplantation. Clin. Infect. Dis. 65, 1984–1991 (2017).
Malard, F., Gasc, C., Plantamura, E. & Doré, J. High gastrointestinal microbial diversity and clinical outcome in graft-versus-host disease patients. Bone Marrow Transplant. 53, 1493–1497 (2018).
Weber, D. et al. Microbiota disruption induced by early use of broad-spectrum antibiotics is an independent risk factor of outcome after allogeneic stem cell transplantation. Biol. Blood Marrow Transplant. 23, 845–852 (2017).
Peled, J. U. et al. Microbiota as predictor of mortality in allogeneic hematopoietic-cell transplantation. N. Engl. J. Med. 382, 822–834 (2020).
Shono, Y. et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci. Transl. Med. 8, 339ra71 (2016).
Stein-Thoeringer, C. K. et al. Lactose drives Enterococcus expansion to promote graft-versus-host disease. Science 366, 1143–1149 (2019).
Jenq, R. R. et al. Regulation of intestinal inflammation by microbiota following allogeneic bone marrow transplantation. J. Exp. Med. 209, 903–911 (2012).
Mathewson, N. D. et al. Gut microbiome-derived metabolites modulate intestinal epithelial cell damage and mitigate graft-versus-host disease. Nat. Immunol. 17, 505–513 (2016).
Swimm, A. et al. Indoles derived from intestinal microbiota act via type I interferon signaling to limit graft-versus-host disease. Blood 132, 2506–2519 (2018).
Campbell, C. et al. Bacterial metabolism of bile acids promotes generation of peripheral regulatory T cells. Nature 581, 475–479 (2020).
Payen, M. et al. Functional and phylogenetic alterations in gut microbiome are linked to graft-versus-host disease severity. Blood Adv. 4, 1824–1832 (2020).
Michonneau, D. et al. Metabolomics analysis of human acute graft-versus-host disease reveals changes in host and microbiota-derived metabolites. Nat. Commun. 10, 5695 (2019).
Markey, K. A. et al. The microbe-derived short-chain fatty acids butyrate and propionate are associated with protection from chronic GVHD. Blood 136, 130–136 (2020).
Peters, S. G., Pomare, E. W. & Fisher, C. A. Portal and peripheral blood short chain fatty acid concentrations after caecal lactulose instillation at surgery. Gut 33, 1249–1252 (1992).
Boets, E. et al. Systemic availability and metabolism of colonic-derived short-chain fatty acids in healthy subjects: a stable isotope study: short-chain fatty acid systemic availability and metabolism in humans. J. Physiol. 595, 541–555 (2017).
Wang, R. X., Lee, J. S., Campbell, E. L. & Colgan, S. P. Microbiota-derived butyrate dynamically regulates intestinal homeostasis through regulation of actin-associated protein synaptopodin. Proc. Natl Acad. Sci. USA 117, 11648–11657 (2020).
Kieft, K. et al. Ecology of inorganic sulfur auxiliary metabolism in widespread bacteriophages. Nat. Commun. 12, 3503 (2021).
Chen, L. X. et al. Large freshwater phages with the potential to augment aerobic methane oxidation. Nat. Microbiol. 5, 1504–1515 (2020).
Howard-Varona, C. et al. Phage-specific metabolic reprogramming of virocells. ISME J. 14, 881–895 (2020).
Zanella, M. C. et al. Unmasking viral sequences by metagenomic next-generation sequencing in adult human blood samples during steroid-refractory/dependent graft-versus-host disease. Microbiome 9, 28 (2021).
Legoff, J. et al. The eukaryotic gut virome in hematopoietic stem cell transplantation: new clues in enteric graft-versus-host disease. Nat. Med. 23, 1080–1085 (2017).
Velten, B. et al. Identifying temporal and spatial patterns of variation from multimodal data using MEFISTO. Nat. Methods 19, 179–186 (2022).
Ruutu, T. et al. Improved survival with ursodeoxycholic acid prophylaxis in allogeneic stem cell transplantation: long-term follow-up of a randomized study. Biol. Blood Marrow Transplant. 20, 135–138 (2014).
Haring, E. et al. Bile acids regulate intestinal antigen presentation and reduce graft-versus-host disease without impairing the graft-versus-leukemia effect. Haematologica 106, 2131–2146 (2021).
Alwin, A. & Karst, S. M. The influence of microbiota-derived metabolites on viral infections. Curr. Opin. Virol. 49, 151–156 (2021).
Liu, L. et al. Improved production of propionic acid in Propionibacterium jensenii via combinational overexpression of glycerol dehydrogenase and malate dehydrogenase from Klebsiella pneumoniae. Appl. Environ. Microbiol. 81, 2256–2264 (2015).
Molinaro, A. et al. Imidazole propionate is increased in diabetes and associated with dietary patterns and altered microbial ecology. Nat. Commun. 11, 5881 (2020).
Mager, L. F. et al. Microbiome-derived inosine modulates response to checkpoint inhibitor immunotherapy. Science 369, 1481–1489 (2020).
Dubin, K. et al. Intestinal microbiome analyses identify melanoma patients at risk for checkpoint-blockade-induced colitis. Nat. Commun. 7, 10391 (2016).
Pryde, S. E., Duncan, S. H., Hold, G. L., Stewart, C. S. & Flint, H. J. The microbiology of butyrate formation in the human colon. FEMS Microbiol. Lett. 217, 133–139 (2002).
Meedt, E. et al. Prolonged suppression of butyrate producing bacteria is associated with acute gastrointestinal graft-versus-host disease and transplant related mortality after allogeneic stem cell transplantation. Clin. Infect. Dis. 74, 614–621 (2022).
Tisza, M. J. & Buck, C. B. A catalog of tens of thousands of viruses from human metagenomes reveals hidden associations with chronic diseases. Proc. Natl Acad. Sci. USA 118, e2023202118 (2021).
Redder, P., Hausmann, S., Khemici, V., Yasrebi, H. & Linder, P. Bacterial versatility requires DEAD-box RNA helicases. FEMS Microbiol. Rev. 39, 392–412 (2015).
Hatfull, G. F. & Hendrix, R. W. Bacteriophages and their genomes. Curr. Opin. Virol. 1, 298–303 (2011).
Weber, D. et al. Reg3α levels at day of allogeneic stem cell transplantation predict outcome and correlate with early antibiotic use. Blood Adv. 7, 1326–1335 (2023).
Seike, K. et al. Ambient oxygen levels regulate intestinal dysbiosis and GVHD severity after allogeneic stem cell transplantation. Immunity 56, 353–368 (2023).
Tamanai-Shacoori, Z. et al. Roseburia spp.: a marker of health? Future Microbiol. 12, 157–170 (2017).
Ogita, T. et al. Oral administration of Flavonifractor plautii strongly suppresses TH2 immune responses in mice. Front. Immunol. 11, 379 (2020).
Stephen, A. M. & Cummings, J. H. The microbial contribution to human faecal mass. J. Med. Microbiol. 13, 45–56 (1980).
Haak, B. W. et al. Integrative transkingdom analysis of the gut microbiome in antibiotic perturbation and critical illness. mSystems 6, e01148-20 (2021).
Rolling, T. et al. Haematopoietic cell transplantation outcomes are linked to intestinal mycobiota dynamics and an expansion of Candida parapsilosis complex species. Nat. Microbiol. 6, 1505–1515 (2021).
van der Velden, W. J. F. M. et al. Role of the mycobiome in human acute graft-versus-host disease. Biol. Blood Marrow Transplant. 19, 329–332 (2013).
Fujiwara, H. et al. Microbial metabolite sensor GPR43 controls severity of experimental GVHD. Nat. Commun. 9, 3674 (2018).
Dubouchet, L. et al. Operational tolerance after hematopoietic stem cell transplantation is characterized by distinct transcriptional, phenotypic, and metabolic signatures. Sci. Transl. Med. 14, eabg3083 (2022).
Steed, A. L. et al. The microbial metabolite desaminotyrosine protects from influenza through type I interferon. Science 357, 498–502 (2017).
Pols, T. W. H. et al. Lithocholic acid controls adaptive immune responses by inhibition of TH1 activation through the vitamin D receptor. PLoS ONE 12, e0176715 (2017).
Winkler, E. S. et al. The intestinal microbiome restricts alphavirus infection and dissemination through a bile acid-type I IFN signaling axis. Cell 182, 901–918 (2020).
Fischer, J. C. et al. Type I interferon signaling before hematopoietic stem cell transplantation lowers donor T cell activation via reduced allogenicity of recipient cells. Sci. Rep. 9, 14955 (2019).
Puccetti, M. et al. Enteric formulated indole-3-carboxaldehyde targets the aryl hydrocarbon receptor for protection in a murine model of metabolic syndrome. Int. J. Pharm. 602, 120610 (2021).
Li, W. et al. A bacterial bile acid metabolite modulates Treg activity through the nuclear hormone receptor NR4A1. Cell Host Microbe 29, 1366–1377 (2021).
Stutz, M. R. et al. Immunomodulatory fecal metabolites are associated with mortality in COVID-19 patients with respiratory failure. Nat. Commun. 13, 6615 (2022).
Lee, J. et al. Gut microbiota-derived short-chain fatty acids promote poststroke recovery in aged mice. Circ. Res. 127, 453–465 (2020).
Norona, J. et al. Glucagon-like peptide 2 for intestinal stem cell and Paneth cell repair during graft-versus-host disease in mice and humans. Blood 136, 1442–1455 (2020).
Henden, A. S. et al. Pegylated interferon-2α invokes graft-versus-leukemia effects in patients relapsing after allogeneic stem cell transplantation. Blood Adv. 3, 3013–3019 (2019).
Peled, J. U. et al. Intestinal microbiota and relapse after hematopoietic-cell transplantation. J. Clin. Oncol. 35, 1650–1659 (2017).
Thevaranjan, N. et al. Age-associated microbial dysbiosis promotes intestinal permeability, systemic inflammation, and macrophage dysfunction. Cell Host Microbe 21, 455–466 (2017).
Vital, M., Howe, A. C. & Tiedje, J. M. Revealing the bacterial butyrate synthesis pathways by analyzing (meta)genomic data. mBio 5, e00889 (2014).
Weinbauer, M. & Suttle, C. Lysogeny and prophage induction in coastal and offshore bacterial communities. Aquat. Microb. Ecol. 18, 217–225 (1999).
Romick-Rosendale, L. E. et al. Antibiotic exposure and reduced short chain fatty acid production after hematopoietic stem cell transplant. Biol. Blood Marrow Transplant. 24, 2418–2424 (2018).
Smith, M. et al. Gut microbiome correlates of response and toxicity following anti-CD19 CAR T cell therapy. Nat. Med. 28, 713–723 (2022).
Routy, B. et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 359, 91–97 (2018).
Ma, T. et al. Differences in gut virome related to Barrett esophagus and esophageal adenocarcinoma. Microorganisms 9, 1701 (2021).
Taur, Y. et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood 124, 1174–1182 (2014).
Scrucca, L., Santucci, A. & Aversa, F. Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant. 40, 381–387 (2007).
Gray, R. J. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann. Stat. 16, 1141–1154 (1988).
Scrucca, L., Santucci, A. & Aversa, F. Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant. 45, 1388–1395 (2010).
Stämmler, F. et al. Adjusting microbiome profiles for differences in microbial load by spike-in bacteria. Microbiome 4, 28 (2016).
Usyk, M., Zolnik, C. P., Patel, H., Levi, M. H. & Burk, R. D. Novel ITS1 fungal primers for characterization of the mycobiome. mSphere 2, e00488-17 (2017).
Wahida, A. et al. XIAP restrains TNF-driven intestinal inflammation and dysbiosis by promoting innate immune responses of Paneth and dendritic cells. Sci. Immunol. 6, eabf7235 (2021).
Vollmer, T., Störmer, M., Kleesiek, K. & Dreier, J. Evaluation of novel broad-range real-time PCR assay for rapid detection of human pathogenic fungi in various clinical specimens. J. Clin. Microbiol. 46, 1919–1926 (2008).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet J. 17, 10 (2011).
Callahan, B. J., Sankaran, K., Fukuyama, J. A., McMurdie, P. J. & Holmes, S. P. Bioconductor workflow for microbiome data analysis: from raw reads to community analyses. F1000Res. 5, 1492 (2016).
Murali, A., Bhargava, A. & Wright, E. S. IDTAXA: a novel approach for accurate taxonomic classification of microbiome sequences. Microbiome 6, 140 (2018).
Nilsson, R. H. et al. The UNITE database for molecular identification of fungi: handling dark taxa and parallel taxonomic classifications. Nucleic Acids Res. 47, D259–D264 (2019).
McMurdie, P. J. & Holmes, S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE 8, e61217 (2013).
Martinez, A. P. pairwiseAdonis: pairwise multilevel comparison using adonis. R package version 0.4 (2020).
Yarza, P. et al. The All-Species Living Tree project: a 16S rRNA-based phylogenetic tree of all sequenced type strains. Syst. Appl. Microbiol. 31, 241–250 (2008).
Mallick, H. et al. Multivariable association discovery in population-scale meta-omics studies. PLoS Comput. Biol. 17, e1009442 (2021).
Blanco-Miguez, A. et al. Extending and improving metagenomic taxonomic profiling with uncharacterized species with MetaPhlAn 4. Nat. Biotechnol. 41, 1633–1644 (2023); https://doi.org/10.1038/s41587-023-01688-w
Beghini, F. et al. Integrating taxonomic, functional, and strain-level profiling of diverse microbial communities with bioBakery 3. eLife 10, e65088 (2021).
Kanehisa, M. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 28, 27–30 (2000).
Ru, J., Khan Mirzaei, M., Xue, J., Peng, X. & Deng, L. ViroProfiler: a containerized bioinformatics pipeline for viral metagenomic data analysis. Gut Microbes 15, 2192522 (2023).
Nurk, S., Meleshko, D., Korobeynikov, A. & Pevzner, P. A. metaSPAdes: a new versatile metagenomic assembler. Genome Res. 27, 824–834 (2017).
Guo, J. et al. VirSorter2: a multi-classifier, expert-guided approach to detect diverse DNA and RNA viruses. Microbiome 9, 37 (2021).
von Meijenfeldt, F. A. B., Arkhipova, K., Cambuy, D. D., Coutinho, F. H. & Dutilh, B. E. Robust taxonomic classification of uncharted microbial sequences and bins with CAT and BAT. Genome Biol. 20, 217 (2019).
Ren, J. et al. Identifying viruses from metagenomic data using deep learning. Quant. Biol. 8, 64–77 (2020).
Johansen, J. et al. Genome binning of viral entities from bulk metagenomics data. Nat. Commun. 13, 965 (2022).
Bin Jang, H. et al. Taxonomic assignment of uncultivated prokaryotic virus genomes is enabled by gene-sharing networks. Nat. Biotechnol. 37, 632–639 (2019).
Steinegger, M. & Söding, J. MMseqs2 enables sensitive protein sequence searching for the analysis of massive data sets. Nat. Biotechnol. 35, 1026–1028 (2017).
Price, M. N., Dehal, P. S. & Arkin, A. P. FastTree 2 — approximately maximum-likelihood trees for large alignments. PLoS ONE 5, e9490 (2010).
Terzian, P. et al. PHROG: families of prokaryotic virus proteins clustered using remote homology. NAR Genom. Bioinform. 3, lqab067 (2021).
Weiss, A. S. et al. In vitro interaction network of a synthetic gut bacterial community. ISME J. 16, 1095–1109 (2022).
Pang, Z. et al. MetaboAnalyst 5.0: narrowing the gap between raw spectra and functional insights. Nucleic Acids Res. 49, W388–W396 (2021).
Reiter, S. et al. Development of a highly sensitive ultra-high-performance liquid chromatography coupled to electrospray ionization tandem mass spectrometry quantitation method for fecal bile acids and application on Crohn’s disease studies. J. Agric. Food Chem. 69, 5238–5251 (2021).
Argelaguet, R. et al. Multi‐Omics Factor Analysis—a framework for unsupervised integration of multi‐omics data sets. Mol. Syst. Biol. 14, e8124 (2018).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B Methodol. 57, 289–300 (1995).
Acknowledgements
This study was supported by the Deutsche Forschungsgemeinschaft (Projektnummer 360372040—SFB 1335 (to S.H., H.P., K.S. and F.B.), Projektnummer 395357507—SFB 1371 (to L.D., H.P., J. Ruland, E.T.O., J.C.F., K.-P.J., M.Q., K.S., S.J., D.H.B. and E.H.), Projektnummer 324392634—TRR 221 (to H.P., W.H., D.Wolff, M.E., D.Weber, A.G. and E.H.), Projektnummer 464797012—SPP 2330 (to L.D.), DE 2360/6-1 (to L.D.), BA 2851/6-1 (to F.B.), DE 2360/1-1 (Emmy Noether Program, to L.D.)), German Cancer Aid (70114547 to H.P.), the Wilhelm Sander Foundation (2021.040.1 to H.P.), the Bavarian Cancer Research Center (BZKF to H.P. and F.B.), the European Hematology Association (to H.P.), the Else Kröner-Fresenius-Stiftung (funding line, Else-Kröner Forschungskolleg to E.T.O. and E.M.), the Bavarian State Ministry of Science and Art (to H.P.), the DKMS Foundation for Giving Life (to H.P.), the German José Carreras Leukemia Foundation (grant DJCLS 01 GvHD/2016 to E.H.), the European Research Commission (project BCM-UPS, grant no. 682473 to F.B. and EU ERC StG—GA no. 803077 to L.D.), the Deutsches Konsortium für Translationale Krebsforschung (fellowship to E.T.O.) and the Deutsche Gesellschaft für Innere Medizin (fellowship to E.T.O.). H.P. is supported by the EMBO Young Investigator Program. We thank the REG allo-SCT team, especially H. Bremm, M. Caioni, T. Schifferstein and Y. Schumann for their help in collecting and cryopreserving stool samples and S. Gleich for data management. We express gratitude to the MUC allo-SCT team, especially K. Braitsch, K. Koch, L. Oßwald, K. Nickel and the entire D2a nursing staff for their excellency in sample acquisition. We acknowledge A. Conrad and W. Johannes (K.-P.J. laboratory) for help with biobanking and A. Wahida for logistical support as well as the MUC ColoBAC team: R. Schmid, M. Middelhoff, J. Horstmann and L. Fricke. We thank the tissue bank of MRI and TUM (MTBIO) for excellent technical support. We acknowledge R.R. Jenq for critical review of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: E.T.O., L.D., E.H., H.P. Methodology: J.Ru, A.H., J.X., M.G., K.K., S.J., D.H.B., K.S., M.Q. Formal analysis: E.T.O., E.M., A.H., J.X., P.Heinrich. Investigation: E.T.O., E.M., S. Ghimire, T.E., S. Göldel, A.S. Resources: C.S., D.Weber, D.Wolff, M.E., D.H.B., W.H., P.Herhaus, M.V., F.B., M.Q., K.-P.J. Data curation: E.T.O., E.M., M.T. Writing (original draft): E.T.O., E.M. Writing (review and editing): E.T.O., E.M., P.Heinrich, O.M., J.X., F.B., S. Göttert, S.L., J.C.F., S.H., M.R.M.v.d.B., L.D., E.H., H.P. Visualization: E.T.O., E.M., A.H., J.X., J.R., T.E., S. Göldel, A.S., P.Heinrich. Supervision: E.T.O., D.H.B., A.G., L.D., E.H. and H.P. Project administration: E.T.O., E.M. Contributions are specified according to CRediT (Contributor Roles Taxonomy). All authors read, revised and approved the final draft.
Corresponding authors
Ethics declarations
Competing interests
E.T.O.: honoraria (BeiGene), travel (BeiGene). M.R.M.v.d.B.: research support and stock options from Seres Therapeutics and stock options from Notch Therapeutics and Pluto Therapeutics; he has received royalties from Wolters Kluwer; he has consulted, received honorarium from or participated in advisory boards for Seres Therapeutics, Vor Biopharma, Rheos Medicines, Frazier Healthcare Partners, Nektar Therapeutics, Notch Therapeutics, Ceramedix, LyGenesis, Pluto Therapeutics, GlaxoSmithKline, Da Volterra, Thymofox, Garuda, Novartis (spouse), Synthekine (spouse), BeiGene (spouse), Kite (spouse); he has IP licensing with Seres Therapeutics and Juno Therapeutics; and he holds a fiduciary role on the foundation board of DKMS (a nonprofit organization). E.H.: scientific advisory board (MaaT Pharma, PharmaBiome (Novartis–Medac)), honoraria and research funding (Neovii, Novartis and Medac). H.P.: honoraria (Novartis, Gilead–Kite, AbbVie, Pfizer, MSD, Bristol Myers Squibb (BMS), Servier, Janssen-Cilag), travel (Janssen-Cilag, Novartis, AbbVie, Novartis, Jazz, Gilead–Kite, AMGEN), research (BMS). C.S.: honoraria (Lilly, Tillotts, Juvisé), research (Luvos). S.H. has been a consultant for BMS, Novartis, Merck, AbbVie and Roche; has received research funding from BMS and Novartis; and is an employee of and holds equity interest in Roche–Genentech. M.V.: honoraria from Novartis, Medac, AbbVie and Jazz Pharmaceuticals as well as travel grants from Medac, Gilead and Jazz Pharmaceuticals. A.S.: honoraria (BeiGene), travel (BeiGene). W.H.: honoraria (Amgen, Novartis), travel (Amgen, Janssen-Cilag). The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Stewart J. Anderson and Gerard Socie for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
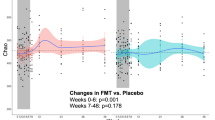
Extended Data Fig. 1 Longitudinal dynamics of bacterial, fungal and viral community compositions in patients receiving allo-SCT.
a) Quantification of the bacterial and fungal load by 16S and 28S rDNA copy numbers per gram of stool at time-points relative to all-SCT (Day 0). Solid lines represent the smoothed conditional means for the entire cohort (black), Munich (MUC, orange) or Regensburg (REG, red) calculated by locally weighted regression using the locally estimated scatterplot smoothing (LOESS) method. The gray shading indicates the 95% confidence interval for entire cohort. Each individual patient stool sample is plotted as a gray dot superimposed on the graph. The number of samples is indicated. b) Beta diversity analysis illustrating changes in bacteriome, fungome and virome by time-points relative to allo-SCT (Day 0). For bacteriome and fungome, beta diversity was calculated by weighted UniFrac. For virome, beta diversity was calculated by Bray-Curtis dissimilarity. Distances were projected in Principal coordinate analysis (PCoA). Bacteriome: Comparisons between Day +7 (p = 0.001), Day + 14 (p = 0.001), Day +21 (p = 0.001), Day +28 (p = 0.001) vs baseline (Day −7) are significant (pairwise Adonis test adjusted for multiple comparisons). Virome: Comparisons between Day +7 (p = 0.013) and Day +28 (p = 0.001) vs baseline are significant (PERMANOVA test). The number of samples is indicated. c) Beta diversity analysis illustrating changes in bacteriome, fungome and virome according to study center (MUC or REG) and whether patients received antifungal therapy (’No Antifungals’ or ‘Antifungals’). For bacteriome and virome, beta diversity was calculated by weighted UniFrac. For virome, beta diversity was calculated by Bray-Curtis dissimilarity. Distances were projected in Principal coordinate analysis (PCoA). The number of samples is indicated.
Extended Data Fig. 2 Longitudinal dynamics of SCFAs, BCFAs, IIMs, PBAs and SBAs in patients receiving in allo-SCT.
a) Heatmap of normalized Panel 1 metabolite levels in stool samples of allo-SCT patients averaged by time-points relative to allo-SCT. Normalized concentrations are indicated in the adjacent color legend. Clustering based on metabolite expression patterns using the Ward algorithm. Distance measure is Euclidian. The number of samples is indicated. b) Heatmap of normalized Panel 2 metabolite levels in stool samples of allo-SCT patients averaged by time-points relative to allo-SCT. Normalized concentrations are indicated in the adjacent color legend. Clustering based on metabolite expression patterns using the Ward algorithm. Distance measure is Euclidian. The number of samples is indicated. c) Principal component analysis (PCA) of Panel 1 metabolite profiles by time-points relative to allo-SCT. Comparisons at Day 0 (p = 0.004), Day +7 (p = 0.001), Day +14 (p = 0.001), Day +21 (p = 0.001) and Day +28 (p = 0.001) vs Day -7 are significant (pairwise Adonis test of Euclidean distances adjusted for multiple comparisons). d) PCA of Panel 2 metabolite profiles by time-points relative to allo-SCT. Comparisons at Day +7 (p = 0.001), Day +14 (p = 0.001), Day +21 (p = 0.001) and Day +28 (p = 0.001) vs Day −7 are significant (pairwise Adonis test of Euclidean distances adjusted for multiple comparisons).
Extended Data Fig. 3 MOFA (multi-omics factor analysis) and MEFISTO (a method for the functional integration of spatial omics data) in allo-SCT patients.
a) Correlation between MOFA-identified Factors and normalized intestinal metabolite concentrations. Associations between Factor values and metabolites were analyzed via Pearson’s correlation. The correlation coefficient is indicated in the adjacent color legend. The p-values associated with the correlations were corrected for multiple testing with the FDR approach. b) Top 15 Features in bacteriome, virome and metabolites in Factor 4 in descending order according to Feature weight. Larger weights indicate a higher correlation with that Factor, while the positive or negative sign indicates the directionality of that variation, that is, ‘+’ indicates a positive association, ‘−’ a negative association. c) Bar plot of time scale parameters assigned to Factors 1 through 10 identified by MEFISTO. MEFISTO assigns a time scale value between 0 and 1 to each Factor, which reflects the degree to which that Factor is dependent on time. A value of 0 implies no time-dependency, a value of 1 strong time-dependency. Of note, results pertaining to the identified Factors, their weight/covariance structure, variance explained across omics entities and Factor values obtained by MEFISTO modelling were almost identical and thus comparable to the output of our original MOFA model. d) Heatmap of normalized abundance of viral contigs assigned to eukaryotic and prokaryotic viruses at time-points relative to allo-SCT. The number of samples is indicated.
Extended Data Fig. 4 Correlation between top 15 bacterial and metabolite as well as bacterial and viral high-weight Features in Factors 1, 3 and 4.
a) Heatmaps of pairwise Pearson’s correlations of top Features across different omics modalities. The Feature values of the top 15 high-weight Features of a given omics modality were correlated with that of another omics modality. (Left) bacterial taxa at genus level and metabolites, (right) bacterial taxa at genus level and bacteriophages at species level. The correlation coefficient is indicated in the adjacent color legend. The p-values associated with Pearson correlation have been corrected for multiple testing by applying the FDR approach to each set of correlations of two omics modalities of a given Factor. b) As in a) for Factor 3. c) As in a) for Factor 4.
Extended Data Fig. 5 Co-abundance of MOFA-identified bacterial and viral Features is associated with high-level IMM expression, which declines progressively after allo-SCT.
a) Correlation scatter plots of high-weight Features within Factor 4, comparing normalized abundance of bacterial taxa at genus level (x-axis) with that of bacteriophages at species level (y-axis) together with the metabolite propionic acid. Dots represent samples from individual patients at different time points (91 samples from 45 patients), all of which had both 16S and viral metagenomic sequencing data. Dots are colored by intestinal levels of propionic acid, or in grey if no propionic acid data was available. Normalized concentrations of metabolites are indicated in the adjacent heatmap. Associations between bacterial genera and viral species were analyzed via Pearson correlation and linear regression. The R- and p-values are indicated in each plot. The regression line is drawn in blue and the 95 % confidence interval of the regression line is shaded in grey. b) As in a) for Features in Factor 3 and the metabolite isovaleric acid. c) As in a) for Features in Factor 3 and the metabolite DAT. d) As in a) for Features in Factor 3 and the metabolite ICA. e) Levels of intestinal microbiota-derived metabolites at time-points relative to allo-SCT (Day 0) in µmol per gram of dried stool measured by targeted mass spectrometry. Number of patients per time-point is indicated in Fig. 4d. Significance by two-sided Kruskal-Wallis test corrected for multiple testing via Dunn’s test of all time-points against baseline (Day -7). In the box plots, the box ranges from the 25th to 75th percentiles. The line in the middle of the box is plotted at the median. The whiskers are drawn down to the 10th and up to the 90th percentile. Points below and above the whiskers are drawn as individual points. Points indicate individual patient stool samples sampled at the specified time-points. SBA…secondary bile acids; UDCA…ursodeoxycholic acid; TUDCA…tauroursodeoxycholic acid.
Extended Data Fig. 6 Intestinal bacterial but not fungal nor viral diversity predicts outcome after allo-SCT.
a) 2-year OS after Day 21 stratified according to higher and lower fungal (left) and viral (right) alpha diversity. The mean alpha diversity of patient samples at Days +7–21 was calculated and patients were stratified into higher (blue curve) and lower (red curve) diversity groups, defined as above or below the center-specific median Inverse Simpson’s diversity index. For fungome, there were 12 deaths among 32 patients in the lower-diversity group (estimated mean survival time 521 (95% CI 428-614) days) and 10 deaths among 30 patients in the higher-diversity group (estimated mean survival time 597 (95% CI 522-672) days). For virome, there were 4 deaths among 16 patients in the lower-diversity group (estimated mean survival time 587 (95% CI 479-696) days) and 4 deaths among 15 patients in the higher-diversity group (estimated mean survival time 576 (95% CI 450-701) days). Analysis via Kaplan–Meier estimator, significance according to the log-rank test. b) 2-year cumulative incidence of relapse and transplantation-related mortality (TRM) in a competing risks analysis stratified according to higher and lower bacterial (top), fungal (middle) and viral (bottom) alpha diversity, calculated as in a). For bacteriome, there were 12 cases of TRM and 6 relapses among 35 patients in the lower-diversity group and one case of TRM and 8 relapses among 33 patients in the higher-diversity group. For fungome, there were 7 cases of TRM and 6 relapses among 32 patients in the lower-diversity group and 5 cases of TRM and 7 relapses among 30 patients in the lower-diversity. For virome, there was one case of TRM and 3 relapses among 16 patients in the lower-diversity group and 3 cases of TRM and 2 relapses among 15 patients in the higher-diversity. Significance according to Gray’s test. c) 2-year cumulative incidence of GvHD and its competing risk Death in a competing risks analysis stratified by alpha diversity as in a). For bacteriome, there were 12 cases of GvHD and 6 deaths among 35 patients in the lower-diversity group and 1 case of GvHD and 8 deaths among 33 patients in the higher-diversity group. For fungome, there were 7 cases of GvHD and 6 deaths among 32 patients in the lower-diversity group and 5 cases of GvHD and 7 deaths among 30 patients in the lower-diversity group. For virome, there was one case of GvHD and 3 deaths among 16 patients in the lower-diversity group and 3 cases of GvHD and 2 deaths among 15 patients in the higher-diversity group. Statistics as in b).
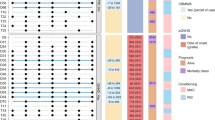
Extended Data Fig. 7 Characterization of differentially abundant microbial pathways and the species which encode them in IMM-RI low- vs high-risk patients via whole shotgun metagenomic sequencing.
a) Species-level association with MetaCyc pathways differentially abundant between IMM-RI low and high-risk patients (as shown in Fig. 6). The relative abundance and species-level identity of taxa encoding the indicated MetaCyc pathways are shown. b) Box plot of relative abundance of indicated MetaCyc pathways in IMM-RI low- vs high-risk patients. In the box plots, the box ranges from the 25th to 75th percentiles. The line in the middle of the box is plotted at the mean. The whiskers are drawn down to the minimum and up to the maximum. Samples outside the 1.5-fold IQR were regarded as outliers. Patient samples are plotted as a point superimposed on the graph (high IMM-RI: n = 10 patients; low IMM-RI: n = 7 patients). Significance by 1-sided Wilcoxon Rank Sum Test corrected for multiple comparisons via the Benjamini & Hochberg correction for multiple testing. c) Box plot of relative abundance of acetic acid and propionic acid superclasses in IMM-RI low- vs high-risk patients. Plots, numbers and statistics as in b).
Extended Data Fig. 8 BCoAT-coding VC-1 and VC-2 bacteriophages are associated with MOFA Factors 1 and 3 and the IMM-RI.
a) Gene alignment plot of VC-2. The identity overlap (in percent) is indicated in the adjacent color legend. The BCoAT AMG is highlighted in red. b) Gene alignment plot of VC-1 as in a). c) Box plots of Factor values for Factors 1 and 3 (averaged across time-points Days +7–21) according to whether VC-1 was detected by viral metagenomic sequencing (‘Yes’) or not (‘No‘). The center line corresponds to the median, the box ranges from the 25th to the 75th percentile. Whisker length corresponds to the largest/lowest data point that does not exceed the 75th/25th percentile +/− 1.5-fold IQR. Blue: detected (n = 16 patients); red: not detected (n = 13 patients). Significance by two-tailed Mann-Whitney-U-test corrected for multiple testing via FDR. d) As in c) for VC-2. Blue: detected (n = 13 patients); red: not detected (n = 16 patients). e) Detection of the BCoAT-coding VC-1 in patient samples stratified according to IMM-RI. Bar plots show percentage, exact values are provided. The numbers of samples screened vs those in which VC-1 was detected is indicated below. f) As in e) for VC-2.
Extended Data Fig. 9 Onset of acute GI-GvHD shifts intestinal bacterial and viral communities and impacts IMM expression profiles.
a) Quantification of the bacterial and fungal load by 16S and 28S rDNA copy numbers per gram of stool stratified by patients diagnosed with GI-GvHD (GI-GvHD, red) vs control allo-SCT patients (No GI-GvHD, blue). The box ranges from the 25th to 75th percentiles. The line in the middle of the box is plotted at the median. The whiskers are drawn down to the minimum and maximum. Samples outside the 1.5-fold IQR were regarded as outliers. Significance by two-tailed Wilcoxon rank sum test adjusted for multiple comparisons via the Benjamini & Hochberg procedure. Each individual patient is plotted as a point superimposed on the graph. Number of patients: for 16S & 28S n = 22 vs n = 37, corresponding to ‘No GI-GvHD‘ vs ‘GvHD‘, respectively. b) Intestinal fungal alpha diversity (Richness, Inverse Simpson’s diversity index) stratified by patients diagnosed with GI-GvHD (GI-GvHD) vs control allo-SCT patients (No GI-GvHD). Plots, numbers and statistics as in a). c) Beta diversity analysis illustrating changes in bacteriome, fungome and virome in patients with GI-GvHD vs control allo-SCT patients. For bacteriome and fungome, beta diversity was calculated by weighted UniFrac. For virome, beta diversity was calculated by Bray-Curtis dissimilarity. Distances were projected in PCoA. Bacteriome: Comparison between patients with GI-GvHD vs No GI-GvHD is significant (p = 0.026 by one-side pairwise Adonis test). Virome: Comparison between patients with GI-GvHD vs No GI-GvHD is significant (p = 0.03 by PERMANOVA test). d) Levels of indicated microbiota-derived metabolites stratified by patients diagnosed with GI-GvHD vs control allo-SCT patients. Significance by two-tailed Mann-Whitney test. In the scatter-dot plots, the box is plotted at the mean. Error bars indicate standard deviation. Each individual patient is plotted as a point superimposed on the graph. The number of patients per group are indicated in the legend.
Extended Data Fig. 10 Impact of antibiotics on bacterial abundance, bacterial and viral community composition and IMM expression profiles.
a) Quantification of the bacterial and fungal load by 16S and 28S rDNA copy numbers per gram of stool stratified by antibiotic exposure: No Antibiotics (‘No ABX’, blue) (blue) vs Antibiotics (‘ABX’, red). Once a patient was treated with antibiotics, the current and all subsequent samples were classified as ‘ABX’. The box ranges from the 25th to 75th percentiles. The line in the middle of the box is plotted at the median. The whiskers are drawn down to the minimum and maximum. Samples outside the 1.5-fold IQR were regarded as outliers. Significance by two-tailed Wilcoxon rank sum test adjusted for multiple comparisons via the Benjamini & Hochberg procedure. Each individual patient is plotted as a point superimposed on the graph. Number of patients: for 16S n = 59 vs n = 70, for 28S n = 56 vs n = 70, corresponding to ‘No ABX’ vs ‘ABX’, respectively. b) Intestinal fungal alpha diversity (Richness, Inverse Simpson’s diversity index) in paired patient samples according to antibiotic status as in a). Plots, numbers and statistics as in a). c) Beta diversity analysis illustrating the impact of antibiotics on the intestinal bacterial, fungal and viral communities. Each point represents individual patient samples annotated with metadata regarding concomitant antibiotic therapy. For bacteriome and virome, beta diversity was calculated by weighted UniFrac. For virome, beta diversity was calculated by Bray-Curtis dissimilarity. Distances were projected in PCoA. Bacteriome: Comparison between patients with ‘No ABX’ vs ‘ABX’ is significant (p = 0.001 by one-side pairwise Adonis test). Virome: Comparison between patients with ‘No ABX’ vs ‘ABX’ is significant (p = 0.003 by PERMANOVA test). d) Levels of indicated microbiota-derived metabolites in paired patient samples before and after exposure to ABX. Significance by two-tailed Wilcoxon matched-pairs signed rank test. In the scatter-dot plots, the box is plotted at the mean. Error bars indicate standard deviation. Each individual patient is plotted as a point superimposed on the graph. The number of patients per group are indicated in the legend.
Supplementary information
Supplementary Information
Supplementary Fig. 1 and Note 1
Supplementary Tables
Supplementary Tables 1–9.
Source data
Source Data Figs. 2 and 7 and Extended Data Figs. 1, 4 and 7
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thiele Orberg, E., Meedt, E., Hiergeist, A. et al. Bacteria and bacteriophage consortia are associated with protective intestinal metabolites in patients receiving stem cell transplantation. Nat Cancer 5, 187–208 (2024). https://doi.org/10.1038/s43018-023-00669-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-023-00669-x