Abstract
Schizophrenia may represent a trade-off in the evolution of human-specific ontogenetic mechanisms that guide neurodevelopment. Human Accelerated Regions (HARs) are evolutionary markers functioning as neurodevelopmental transcription enhancers that have been associated with brain configuration, neural information processing, and schizophrenia risk. Here, we have investigated the influence of HARs’ polygenic load on neuroanatomical measures through a case-control approach (128 patients with schizophrenia and 115 controls). To this end, we have calculated the global schizophrenia Polygenic Risk Score (Global PRSSZ) and that specific to HARs (HARs PRSSZ). We have also estimated the polygenic burden restricted to the HARs linked to transcriptional regulatory elements active in the foetal brain (FB-HARs PRSSZ) and the adult brain (AB-HARs PRSSZ). We have explored the main effects of the PRSs and the PRSs x diagnosis interactions on brain regional cortical thickness (CT) and surface area (SA). The results indicate that a higher FB-HARs PRSSZ is associated with patients’ lower SA in the lateral orbitofrontal cortex, the superior temporal cortex, the pars triangularis and the paracentral lobule. While noHARs-derived PRSs show an effect on the risk, our neuroanatomical findings suggest that the human-specific transcriptional regulation during the prenatal period underlies SA variability, highlighting the role of these evolutionary markers in the schizophrenia genomic architecture.
Similar content being viewed by others
Introduction
Schizophrenia (SZ) is a complex neuropsychiatric disorder characterised by symptoms that alter perception and behaviour, such as hallucinations, delusions, and affectations of higher-order cognitive functions. These symptoms intimately relate the disorder with traits distinguishing humans as a species, such as abstraction, language, thinking, and some aspects of social cognition, such as Theory of Mind1,2,3. Accordingly, while the foundations of this multifactorial and complex disorder are not entirely understood, multiple pieces of evidence straightforwardly point towards a neurodevelopmental and evolutionary origin.
On the one hand, the polygenic architecture of SZ, with thousands of genetic variants with additive effects accounting up to 80% of its heritability4,5,6,7, converges with pathways related to developmental, neuronal, and synaptic differentiation mechanisms8,9,10. Such pathways are tightly orchestrated and involve gene expression regulatory mechanisms of paramount importance for brain ontogeny11, which, at the same time, are highly influenced by the environmental events occurring during prenatal and early periods. Remarkably, prenatal and obstetric complications are associated with an increased risk for SZ12, and their presence correlates with a higher genomic risk for the disorder13. In parallel, the placenta-associated genomic burden for schizophrenia is linked to reduced brain volumes in neonates and poorer cognitive development during the first two years of life14, while delayed developmental milestones are associated with the disorder and predict psychotic symptoms in childhood and adulthood15,16,17. Also, highly heritable neuroanatomical measures, such as cortical thickness (CT) and cortical surface area (SA), show differences between patients with SZ and healthy controls, even prior to the onset of the psychotic symptoms18,19. All this evidence sustains the prevailing aetiological hypothesis that SZ results from environmental and genetic interactions modulating and deviating neurodevelopmental trajectories during the intrauterine and perinatal periods as well as during childhood and early adolescence20,21 that disrupt the ontogenetic plan guiding brain architecture, brain configuration, and brain functioning.
On the other hand, the common prevalence of the disorder (nearly 1%)22,23,24, and the fact that people affected, particularly males, have a reduced rate of reproduction (fitness) compared with non-affected individuals25,26, raise the question of why the genetic variants that increase the likelihood of suffering from SZ have persisted in the genetic pool. This, together with the close relationship between several clinical aspects of the disorder and human-specific cognitive traits1, has boosted the evolutionary view of the disorder. Accordingly, the evolutionary hypothesis of SZ suggests that the disorder emerged as a costly trade-off in the evolution of the ontogenetic mechanisms guiding human-specific neurodevelopment and sustaining complex cognitive abilities27,28,29,30.
While the evolutionary traces of SZ are challenging to follow, studying human-specific genomic changes through comparative genomics may lead to a better comprehension of human-specific phenotypic traits and increased knowledge of what genetic changes contributed to making us human31,32,33. In this sense, Human Accelerated Regions (HARs) might be helpful. HARs are evolutionary conserved genomic regions that have experienced significant changes after human and chimpanzee divergence34,35,36,37,38,39. This accelerated evolution is suggested to reflect HARs’ role in some human-specific characteristics. Most HARs are intergenic, within introns near protein-coding genes, transcription factors and DNA-binding proteins40,41,42,43,44. All the studies that intended to characterise HARs’ functional role converge in highlighting them as transcription factors binding sites, transcription factors on their own and participants in the neurodevelopmental gene expression machinery43,45,46,47.
Recently, studies inspecting the expression patterns of HARs-associated genes (HARs-genes) show their implication in human-specific cortical expansion, brain functional connectivity and brain’s neural information processing. First, a comparative study exploring the cortical expansion in humans and chimpanzees described that the expression profiles of HARs-genes correlate with the expansion of higher-order cognitive networks, such as the frontoparietal and the default mode networks48. The same study reveals that the genetic variability in HARs-genes expressed in the brain (HARs-brain genes) is associated with the default mode network functional variation in healthy subjects48. Second, the expression patterns of HARs-brain genes have been related to individual variability in functional connectivity and the brain’s information processing49,50. Notably, these studies report that HARs-brain genes show the highest expression in higher-order cognitive networks, such as the frontoparietal and the default mode networks, the ones with the greatest functional heterogeneity across individuals and with predominant synergistic interactions49,50.
The evidence on HARs’ contribution to human-specific brain architectural configuration, functioning and information processing is also accompanied by studies that describe that HARs’ genetic variability influences the risk for SZ. For example, the investigation into the overlap between HARs and whole-genome common genetic variants shows that the SZ polygenic background is enriched in genes associated with these evolutionary regions51. In line, subsequent findings also described that Single Nucleotide Polymorphisms (SNPs) in HARs or in linkage disequilibrium with them are more likely associated with the disorder52. Notwithstanding, to our knowledge, HARs modulation of brain measures in SZ has been scarcely explored, and further studies using brain-based phenotypes to assess their role in the disorder are necessary.
Considering the polygenic nature of both cortical structural configuration and SZ’s susceptibility10,53, the use of measures summarising this complex genetic architecture, such as Polygenic Risk Scores (PRSs), would be helpful to disentangle the genetic roots not only of the disorder but of complex brain traits. The PRS is a quantitative measure of the individual genetic burden for a trait based on data from Genome-Wide Association Studies (GWAS). Although PRS methods do not yet provide clinically feasible information in psychiatric disorders54, schizophrenia PRSs are highly informative for assessing the individual risk for the disorder at the research level and are highly consistent across studies and samples55. PRSs can be calculated on a genome-wide basis, but also within subsets of SNPs defined according to their affiliation to specific biological pathways of interest56. Therefore, based on the evidence of HARs’ role in neurodevelopment, brain configuration and susceptibility for SZ, we aimed to investigate the modulatory effect of HARs’ polygenic load on neuroanatomical measures through a neuroimaging genetics approach in healthy controls and patients with SZ.
We generated different PRSs summarising HARs’ genetic variability, specifically including HARs SNPs related to active regulatory elements in the foetal and adult brain. We explored whether the PRSs modulated CT and SA differently depending on the health/disease condition. Our findings point to a specific effect of HARs linked to foetal brain regulatory elements on patients’ cortical SA, emphasising the importance of human-specific changes in early neurodevelopment and in the structural changes associated with the disorder.
Results
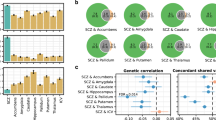
Case-control PRS comparison
Four SZ-based PRSs were estimated: one summarizing the global schizophrenia polygenic burden (Global PRSSZ), another specific to HARs (HARs PRSSZ), as well as two PRSs specific to HARs linked to transcriptional regulatory elements active in the foetal (FB-HARs PRSSZ) and adult brain (AB-HARs PRSSZ). Case-control comparisons revealed differences in the Global PRSSZ: patients presented higher SZ genetic load as compared to HC. The HARs-derived PRSs did not show between-group differences (Table 1). No significant PRS effect was detected on patients’ clinical profiles (age at onset, illness duration, Positive and Negative Syndrome Scale (PANSS) scores, and antipsychotic medication, given as Chlorpromazine (CPZ) equivalents in mg/day) (Supplementary Data 1).
PRS associations with cortical thickness and surface area measures
When examining the extent to which the four PRSs modulated CT and SA measures of each cortical region, we detected that no PRS estimate influenced the CT in HC or patients with SZ. Along the same line, the PRSs x diagnosis interactions on CT did not evidence significant effects (Supplementary Data 2).
In contrast, the linear regression analyses revealed that among patients, the FB-HARs PRSSZ significantly affected the cortical SA in four regions of the right hemisphere: the lateral orbitofrontal cortex (β = −1581.796, Standardised β = −0.234, SE = 440.443, adjusted R2 = 0.491, FDR-pval = 0.008), the superior temporal cortex (β = −1960.151, Standardised β = −0.235, SE = 545.898, adjusted R2 = 0.488, FDR-pval = 0.008), the pars triangularis (β = −1409.886, Standardised β = −0.242, SE = 438.928, adjusted R2 = 0.322, FDR-pval = 0.020) and the paracentral lobule (β = −842.876, Standardised β = −0.233, SE = 282.910, adjusted R2 = 0.264, FDR-pval = 0.031) (Fig. 1). A higher SZ risk load in FB-HARs was associated with lower SA values in these regions. Conversely, no other associations were observed between the other estimated PRSs and SA, neither in HC nor in interaction with diagnosis (Supplementary Data 2). The SA variability in these four regions of interest was not related to the clinical profiles of patients (Supplementary Data 3).
Brain plots include the lateral and medial sagittal views for the right hemisphere. The coloured regions are the ones with significant FB-HARs PRSSZ effect on surface area (SA). Within patients (n = 128), the scatter plots show the FB-HARs PRSSZ, on the X-axis, and the unstandardised SA residuals (estimated regressing out the covariates), on the Y-axis. These plots evidence the negative correlation between the two measures (black solid line and black dashed lines representing the regression line and the 95% confidence intervals, respectively). Each region is numerically labelled as follows: (1) superior temporal cortex; (2) lateral orbitofrontal cortex; (3) pars triangularis; and (4) paracentral lobule.
Inspecting the genomic context of the SNPs in FB-HARs PRSSZ showed that 54.1% were in intergenic regions, 26.5% in introns and 16.6% in intronic non-coding RNA. The SNPs were mapped into 223 genes (Supplementary Data 4). The subsequent functional annotation results highlighted that these genes were enriched in several Gene Ontology (GO) categories (Fig. 2, Supplementary Data 5). The biological processes more significantly enriched were neuron differentiation, neurogenesis, neuron development, and head development. Also, the only cellular component category enriched was cell junction.
Functional annotation results derived from FUMA (https://fuma.ctglab.nl/) in Gene Ontology (GO) categories for biological processes (a), and cellular components (b). In each panel, the GO categories can be seen on the left, followed by the proportion of the overlapping genes, the associated p-value after FDR correction (Enrichment P-value), and the overlapping genes on the right.
Discussion
Through a neuroimaging genetic approach, we have evaluated the SZ’s polygenic burden of human-specific evolutionary markers such as HARs on brain-based phenotypes closely related to the pathophysiology of the disorder. Although studies on HARs are an emerging field, as a recent review by our group highlights57, and the expression profiles of HARs-brain genes have been studied in relation to brain structural changes across different psychiatric disorders48, our study is the first to assess the effect of HARs genetic variability on brain cortical measures in patients with SZ and healthy controls. These analyses provide evidence of the impact of foetal active regulatory HARs on the cortical surface area of different brain regions in patients with SZ. These findings highlight the importance of human-specific genetic changes guiding human brain cortical architecture, particularly those affecting the gene-expression machinery active during prenatal stages.
The comparisons between the different PRSs estimates across diagnostic groups show that individuals with a diagnosis of SZ present higher Global PRSSZ than healthy individuals, and thus, a higher polygenic load for the disorder. This result aligns with the current view on the value of the PRSSZ as a highly informative genetic vulnerability marker for its consistency across numerous studies, not only limited to comparisons between patients and controls58,59, but also through family approaches, which show the intermediate genetic load that healthy relatives of affected patients have60,61.
However, in our sample, the analyses indicate no significant differences across diagnostic groups when using the HARs-related PRSSZ. The lack of association between HARs-derived PRSs and SZ risk in our sample may reflect the broader genotypic background underlying the diagnosis, but it could also result from insufficient power. Therefore, future association studies with larger case-control samples are needed to deepen the direct link between HARs’ polygenic load and the risk of developing SZ. It is challenging to directly compare our findings with previous research because of the absence of HARs-based PRS studies. Some previous SZ association research exploring the variability in candidate HARs points towards a link between these evolutionary regions and the risk for the disorder. For instance, the haplotypic variability at the HAR1A gene, a novel RNA gene with a presumable neurodevelopmental role that harbours the HAR with the highest substitution rate in humans as compared to chimpanzees44, was associated with auditory hallucinations in patients with a schizophrenia-spectrum disorder in a European sample62. Also, several candidate HARs-SNPs, altering transcription factor binding sites and presenting methylation marks of active promoters, repressors, or enhancers in the brain, were associated with the risk for SZ and modulated cognitive performance in a north-Indian population63,64. Convergently, genome-wide-based studies also describe that HARs-genes and HARs-brain genes are associated with SZ at the GWAS level48,51,52,65. Some of these studies, indeed, went beyond common variability and showed that rare variants in HARs-genes were also enriched with the disorder48; suggesting, therefore, that joint analysis of common and rare variants can help disentangling the role of HARs variability on the susceptibility for the disorder and its specific phenotypes.
In our investigation on the contribution of HARs polygenic background on cortical neuroanatomical measures, we report a modulatory effect of FB-HARs PRSSZ on the SA within patients. These findings suggest that the genetic variability in HARs associated with regulatory elements uniquely active in the foetal brain would specifically influence brain phenotypes in SZ. Results show that as the FB-HARs PRSSZ increases (i.e. as more SZ risk load accumulates in these HARs associated with foetal active regulatory elements), patients present lower cortical SA in the lateral orbitofrontal cortex, the superior temporal cortex, the pars triangularis and the paracentral lobe. First, these findings converge with data highlighting the importance of the foetal period (and the gene expression circumscribed to it) to understand the neurodevelopmental trajectories linked to SZ14. Also, our findings align with the ENIGMA Consortium study reporting widespread smaller surface area in SZ, with the largest effect sizes in the frontal and temporal lobe regions19. In spite of the detected differences in SZ, the reductions in SA were not associated with the patients’ symptoms, the onset of the disorder or its duration. These outcomes are aligned with the findings from van Erp et al., that reported that the regional SA changes in patients were not correlated with PANSS total, positive, and negative symptom scores19. Even so, in previous studies, SA reductions in the right frontal cortex have been correlated with more severe negative symptoms in patients with psychosis, including SZ, schizoaffective disorder, and bipolar disorder type I with psychotic symptoms66. In the same line, other structural and functional alterations in the superior temporal region have been reported in relation to formal thought disorder in patients67,68.
From an evolutionary perspective, if we focus on the regions significantly modulated by the SZ genetic burden in active foetal brain HARs, we can draw attention to the orbitofrontal region and the temporal cortex. These are among the regions suffering the largest expansion in the human cortex in comparison with chimpanzees48. Wei et al.48 described that those areas of the orbital frontal gyrus and the temporal lobe experienced an x4 and x3 expansion, respectively, and evidenced that the transcription profile of 1,711 HARs-genes positively correlated to the pattern of human cortical expansion, meaning that the highest HARs-gene expression occurs in highly expanded areas of the human cortex. Moreover, it has been proposed that the anatomical changes in the human temporal cortex compared to other primates may be involved in higher-level cognitive functions and behaviours especially developed in humans, such as semantic processing, language, and Theory of Mind69. Also, it has been sustained that the orbitofrontal cortex may mediate reward-related behaviours, learning, decision making and expectation70.
A remarkable finding of the present study is the specific HARs’ polygenic association with SA rather than CT variability. This could be interpreted considering that the genetic influences on the two cortical measures and the underlying mechanisms are largely independent and follow distinct developmental trajectories71,72,73, but both are related to neurodevelopmental genetic control53,74,75. As posited by the radial unit hypothesis, cortical SA expansion would be driven by the proliferation of neural progenitor cells, while CT would be determined by the number of their neurogenic divisions76. In this line, a study described that HARs-genes are highly expressed during prenatal development; their expression is upregulated during neurogenesis and enriched in cells from the outer radial glia45. Indeed, radial glia is a major class of neural stem cells in the germinal layer that shows substantial expansion in the primate lineage and, among the neurodevelopmental differences between humans and chimpanzees, there is the proliferative capacity of neural progenitors during cortical development77. Recent data shows that the genetic determinants of SA are predominately related to gene regulatory activity in neural progenitor cells during foetal development, while CT is influenced by regulatory processes that occur after mid-foetal development53. Also, common genetic variants explained a larger part of SA variance (SNP-h2 = 34%, SE = 3%) than CT variance (SNP-h2 = 26%, SE = 2%)53. However, our results could also be influenced by the reduced number of SNPs in our PRS estimates, which could have hampered the capture of the genetic determinants of CT. Likewise, by using HARs, we are focusing on regions highly stable along mammal evolution that have experienced rapid sequence changes in the human lineage since the divergence from our closest relatives. Moreover, while SA has enormously increased during the evolution of primates, cortical thickness has remained relatively constant78. Therefore, other genetic evolutionary markers could be more suitable for inspecting the evolutionary traces of CT.
Relative to the exploratory gene mapping results, it was interesting that the SNPs underlying cortical surface area differences within patients were enriched in biological processes essential for nervous system development. These findings align with previous studies describing that HARs-associated genes mainly participate in biological processes and pathways related to neurodevelopment, neural differentiation and axonogenesis43.
Finally, we should account for some limitations of this study. Regarding our genetic association approach, the samples could be considered small; nonetheless, our study focused on the neuroimaging association approach. According to a recent revision, these analyses have been conducted in a larger sample than the median sample size of neuroimaging association studies to date79; however, it does not exclude the need for new studies in larger samples. In this regard also, we have to point out that our structural images were obtained from two scanners, which could represent a source of bias. Notwithstanding, we did not detect differences in neuroanatomical measures based on the two scanning sites, all the images passed the standardised quality-control protocols recommended by the ENIGMA consortium, which have been previously applied in large-scale multi-centre studies, and the scanner site was accounted as a covariate in the regressions. In terms of the genetic data, we should contemplate that our PRS estimates are pondered using SZ genetic burden, and the use of other GWAS summary statistics, such as the corresponding to the cortical phenotypes, could lead to different effects. The PRS estimation method used in the present study, PRS-C + T, is the most used, and the latest SZ GWAS has been conducted using the same method; however, other PRS calculation methodologies could be helpful80. Speaking of PRS estimations, our results are based on a sample of European ancestry and SZ GWAS statistics were derived from the European cohort. Then, although GWAS studies performed in non-European samples converge in the same SZ’s genes and pathways81, the extrapolation of our findings to other ethnic groups should not be done straightforwardly, and research based on populations of different ethnic origins should be encouraged. We should also consider that upcoming studies would greatly benefit from assessing environmental risk factors occurring along the neurodevelopmental period, which could modulate the genetic background and impact the brain developmental trajectories82,83. Finally, future study designs willing to understand the role of HARs in the neurobiological roots of SZ would benefit from analyses on other brain-based phenotypes such as structural connectivity, white matter microstructure84,85,86, or MRI protocols related to social cognition87.
Our findings, together with the increasing knowledge of the functions of HARs and the biological mechanisms in which they are involved, open new investigation venues. Based on the role of HARs as paramount actors in neurodevelopmental transcriptional regulation and their involvement in the genetic burden of neurodevelopmental psychiatric disorders like SZ and autism42,43,47,51,65,88, our study and most of the previous research have been focused on HARs’ common variability. Still, to gain insights into the pathogenic role of these regions, future studies should explore the functional effects of HARs’ rare variability. Also, the prioritisation and interpretation strategies in whole-genome sequencing approaches should consider not only exonic or promoter variants but regulatory regions such as HARs. Furthermore, psychiatric disorders with a strong neurodevelopmental component are intimately related to the emergence of the human condition, sustained by the evolution of human-specific ontogenic mechanisms. Thus, studies on the genetic basis of this disorder should not be separated from this evolutionary component. Future studies would be strengthened by analysing the contribution of evolutionary relevant regions towards the disorders’ genetic background89,90,91.
In conclusion, our study adds evidence on the role of the genetic variability within HARs guiding foetal neurodevelopment and shaping cortical surface area configuration in patients with SZ. The biological plausibility of our findings highlights the importance of HARs in the early developmental gene regulatory machinery and suggests that these regions may contribute to bridging together the neurodevelopmental and evolutionary hypotheses in schizophrenia.
Methods
Sample
The initial sample consisted of a case-control dataset of 378 individuals, of which 284 passed both the genetic and neuroimaging quality control (see details in the corresponding Molecular analyses and MRI data acquisition sections). Patients were recruited from inpatient and outpatient units at various centres from the Germanes Hospitalàries in Barcelona province. Healthy controls (HC) consisted of individuals from the same area, including non-medical staff employed at healthcare facilities, their relatives, and acquaintances, as well as members of the community recruited through online advertisements and independent sources. The patients’ diagnoses were confirmed according to DSM-IV-TR based on an interview with two psychiatrists. Patients’ symptoms were assessed based on the PANSS92,93. All participants were of European ancestry, between 18 and 65 years old, right-handed (based on self-report) and had an estimated intelligence quotient (IQ) (premorbid IQ in patients) higher than 70, as assessed using the Word Accentuation Test94. All participants met the same exclusion criteria, which included suffering from major medical illness, conditions affecting cognitive or brain function, neurological conditions, history of head trauma with loss of consciousness and present or history of drug abuse or dependence. Additionally, for HC, exclusion criteria also included personal or family history of psychiatric service contact or treatment.
A group matching procedure was conducted to minimise the differences across diagnostic groups while maximising the sample size. Therefore, the analyses were conducted in a sample of 115 HC and 128 patients diagnosed with SZ with no age and sex differences between them (Table 2).
All subjects signed a written consent after being fully informed about the procedures and implications of the study, approved by the Germanes Hospitalàries Research Ethics Committee, and performed following its guidelines and in accord with the Declaration of Helsinki. All ethical regulations relevant to human research participants were followed.
Molecular analyses
Genomic DNA was extracted from buccal mucosa through cotton swabs or peripheral blood cells using Realpure Saliva or Blood kits (Durviz, S.L.U., Valencia, Spain).
A genome-wide genotyping was performed using the Infinium Global Screening Array-24 v1.0 (GSA) BeadChip (Illumina, Inc., San Diego, California, U.S) at the Spanish National Cancer Research Centre, in the Human Genotyping lab (CeGen-ISCIII), resulting in the genotyping of 730,059 SNPs. After quality control, a dataset of 447,035 SNPs with the following characteristics was obtained: Hardy-Weinberg equilibrium in patients and healthy controls, SNP call rate higher than 98% and minor allele frequency (MAF) higher than 0.005. Individuals with an SNP missingness higher than 2% were excluded. In addition, through a principal component analysis, those individuals found to be related or not of European ancestry were also excluded. Next, re-phasing and imputation were performed using, respectively, Eagle95 and Minimac496 and the Haplotype Reference Consortium dataset (HRC version r1.1)97 hosted on the Michigan Imputation Server96 (https://imputationserver.sph.umich.edu/). A MAF value of >1% and an imputation quality of R2 > 0.3 were required for the inclusion of the variants into further analyses. Finally, our final SNP dataset included 7,606,397 genetic markers.
Polygenic risk scores estimation
Using SZ GWAS 2022 summary statistics from the European subsample10, we estimated four different PRS using PLINK 1.90 software98 based on the PRS-C + T methodology99, as in several recent GWAS studies10,53,100. This method is defined as the sum of allele counts, weighted by estimated effect sizes obtained from the GWAS, after two filtering steps: LD clumping (based on the European population from phase 3 of the 1000 Genomes Project reference panel) and p-value thresholding.
First, we calculated the whole-genome PRS (Global PRSSZ). The LD filtering was conducted by including the most significant SNP from any pair showing an LD r2 > 0.015 within 1000 kb windows, resulting in a set of informative linkage-disequilibrium independent markers (98,121 SNPs). Subsequently, for the p-value thresholding, we considered a range of thirteen p-value thresholds: p < 5 × 10−8, p < 5 × 10−7, p < 5 × 10−6, p < 5 × 10−5, p < 5 × 10-4, p < 5 × 10−3, p < 0.05, p < 0.1, p < 0.2, p < 0.3, p < 0.4, p < 0.5, p < 1.0. Through logistic regression, we established the best threshold in p < 5 × 10−3 as the better predictor of the diagnosis status based on Nagelkerke’s pseudo-R2 (p = 4.75 × 10−12, R2 = 0.22).
Second, we estimated a PRS accounting for HARs genetic variability (HARs PRSSZ), exclusively including SNPs within the 3070 autosomal HARs sequences compiled by Girskis et al.47 (Supplementary Data 6). Using Bedtools 2.30.0101, we selected the genetic markers in our sample within these HARs sequences. Considering the number of SNPs within the HARs, the PRS estimation was conducted following the same PRS-C + T methodology but adjusting LD clumping parameters. Following PLINK default options, we selected the most significant SNPs within 250 kb windows and with LD r2 > 0.5 and the unique p-value threshold was set at p < 1.0. The final set of variants comprised 2201 SNPs (Supplementary Data 7).
Third, to assess the effect of HARs SNPs specifically affiliated with active foetal brain (FB) or adult brain (AB) gene regulatory elements, we estimated two additional PRS scores (FB-HARs PRSSZ and AB-HARs PRSSZ) with the same procedure and parameters as for PRS-HARs. We followed the same methodology used in the latest ENIGMA human cerebral cortex GWAS53 to do so. As described by Grasby et al., 202053, we downloaded ChromHMM chromatin states (Core 15-state model) from the Epigenomics Roadmap102. We selected the genomic regions comprising active regulatory elements (active transcription start site (TssA), flanking active transcription start site (TssAflnk), enhancers (Enh) and genic enhancers (EnhG)) for the two available foetal tissues (E081=foetal brain female and E082 = foetal brain male) and the four available cortical adult tissues (E067 = brain angular gyrus, E069 = brain cingulate gyrus, E072 = brain inferior temporal lobe and E073 = brain dorsolateral prefrontal cortex). We combined the foetal (E081 and E082) and adult (E067, E069, E072 and E073) annotations and selected only those regions non-overlapping between them as foetal brain-specific and adult brain-specific. With the selected HARs PRSSZ SNPs, we selected the genetic variants allocated within these foetal and adult brain-specific regions. The final set of variants included in the FB-HARs PRSSZ and AB-HARs PRSSZ estimations were 112 and 81 SNPs, respectively (Supplementary Data 7), and the data on the four estimated PRSs can be found at Supplementary Data 8.
MRI data acquisition
The MRI neuroimaging data were obtained from two scanners: 58% (70 HC, 72 patients) of the sample was scanned in a 1.5 T GE Sigma scanner (General Electrical Medical Systems, Milwaukee, Wisconsin, USA) and the other 42% (45 HC, 56 patients) in a 3 T Philips Ingenia scanner (Philips Medical Systems, Best, The Netherlands) at Hospital Sant Joan de Déu (Barcelona, Spain).
High-resolution structural-T1 MRI data in the 1.5 T scanner was obtained using the following acquisition parameters: matrix size 512 × 512; 180 contiguous axial slices; voxel resolution 0.47 × 0.47 × 1 mm3; echo time (TE) = 3.93 ms, repetition time (TR) = 2000 ms; and flip angle = 15°. At the 3 T scanner, structural T1-weighted sequences were acquired as follows: matrix size 320 × 320 × 250; voxel resolution 0.75 × 0.75 × 0.80 mm3; TE = 3.80 ms, TR = 8.40 ms; and flip angle = 8°. All images were visually inspected to exclude those with artefacts and movement.
Neuroanatomical data
Structural MRI data were processed using the FreeSurfer image analysis suite (http://surfer.nmr.mgh.harvard.edu/). The images obtained from the two different scanners were independently pre-processed. This process included the removal of non-brain tissue, an automated Talairach transformation, tessellation of the grey and white matter boundaries and surface deformation103, after which individual images were normalised to a common stereotaxic space. Several deformation procedures were performed in the data analysis pipeline, including surface inflation and registration to a spherical atlas. This method uses both intensity and continuity information from the entire three-dimensional images in the segmentation and deformation procedures to produce vertex-wise representations of CT and SA. The CT was defined as the measure of the distance between the white matter surface and the pial surface, and cortical SA was calculated as the area of the white matter surface. With FreeSurfer, we automatically performed the segmentation of 34 cortical regions of interest for each hemisphere using the Desikan-Killiany cortical atlas104. Within these defined regions, mean values of CT and SA were quantified for each individual. Additionally, the global mean CT and the total SA were also considered.
All subjects included in the study passed the standardised quality-control protocols from the ENIGMA consortium (https://enigma.ini.usc.edu/protocols/imaging-protocols/) previously applied in large-scale multi-centre studies53,105.
Statistics
Demographic and clinical data were processed and analysed using SPSS (IBM SPSS Statistics, version 29.0, released 2022, IBM Corporation, Armonk, New York, USA).
We compared the SZ polygenic load of patients and controls based on the four different PRS estimations (Global PRSSZ, HARs PRSSZ, FB-HARs PRSSZ and AB-HARs PRSSZ) by means of block-wise logistic regressions with the two diagnostic groups (SPSS). For each PRS, two statistical models with case/control status as outcome were compared, one testing the covariates alone (age, sex and the two first ancestry-specific principal components as a baseline model) and the other testing the covariates plus the corresponding PRS (full model). We report the R2 values as the differences in Nagelkerke’s pseudo-R2 between these two nested models as an indicator of explained variance60,106. To assess whether PRSs modulate patients’ clinical profiles, we tested the effect of the four PRSs estimations on age at onset, illness duration, PANSS scores, and antipsychotic medication dose by means of linear regression models (controlled by sex).
Next, we examined to which extent the four different PRSs modulate CT and SA measures of each cortical region. We applied linear regression models, separately in HC and patients, to test the effect of each of the four PRS (as independent variables) on both neuroanatomical measures (as dependent variables) (R software). To assess whether the diagnostic status modulates the PRS effect, we conducted linear models using the whole sample and tested the PRS x diagnosis interaction. To control for the differences in scanners among individuals plus the potential effects of sex, age, premorbid IQ, and intracranial volume, all these variables were included as covariates in the analyses. In the linear regression within patients with SZ, the antipsychotic dose was also included as a covariate19,107.
According to the findings, to determine if the detected anatomical changes were related to the clinical profiles of patients, we analysed whether the SA changes impacted their age at onset, illness duration, and PANSS scores by means of linear regression models. To do this, we regressed the SA residuals from the four significant cortical regions of interest (obtained after regressing age, sex, intracranial volume, scanner, and antipsychotic medication) on the clinical phenotypes (controlling for age, sex, and antipsychotic medication) (SPSS).
Lastly, the SNPs included in the FB-HARs PRSSZ were furtherly mapped and functionally annotated using FUMA108 with the SNP2GENE and the GENE2FUNC tools. The positional mapping parameters were left as default. The eQTL mapping was conducted in PsychENCODE, ComminMind and BRAINEAC tissues filtering by PsychENCODE and brain open chromatin atlas annotations. The 3D chromatin interaction mapping was built-in PsychENCODE and Hi-C adult and foetal cortex, dorsolateral and hippocampus and neural progenitor cells data, filtered by PsychENCODE and brain open chromatin atlas annotations.
The p-values from each of the before mentioned statistical tests were adjusted using the false discovery rate (FDR) method, precisely the Benjamini-Hochberg procedure, to control for multiple comparisons at level q = 0.05. Accordingly, only those results with a corrected FDR-pval<0.05 are reported as statistically significant.
The significant results on the cortical regions were plotted using the ggseg library in R109 and the regressions with the direction of the results were plotted using SPSS (the numerical source data for graphs is provided in Supplementary Data 9).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The data supporting the findings of this study are available from the corresponding authors upon reasonable request.
Code availability
The custom code used for the analyses of this study is available from the corresponding authors upon reasonable request.
References
Polimeni, J. & Reiss, J. Evolutionary perspectives on Schizophrenia. Can. J. Psychiatry 48, 34–39 (2003).
Frith, C. D. & Frith, U. Mechanisms of social cognition. Annu Rev. Psychol. 63, 287–313 (2012).
Weng, Y., Lin, J., Ahorsu, D. K. & Tsang, H. W. H. Neuropathways of theory of mind in schizophrenia: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 137, 1–17 (2022).
Sullivan, P. F., Kendler, K. S. & Neale, M. C. Schizophrenia as a complex trait. Arch. Gen. Psychiatry 60, 1187–1192 (2003).
Purcell, S. M. et al. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460, 748–752 (2009).
Hilker, R. et al. Heritability of Schizophrenia and Schizophrenia spectrum based on the nationwide Danish twin register. Biol. Psychiatry 83, 492–498 (2018).
Legge, S. E. et al. Genetic architecture of schizophrenia: a review of major advancements. Psychol. Med. 51, 2168–2177 (2021).
Gulsuner, S. et al. Spatial and temporal mapping of de novo mutations in schizophrenia to a fetal prefrontal cortical network. Cell 154, 518–529 (2013).
O’dushlaine, C. et al. Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat. Neurosci. 18, 199–209 (2015).
Trubetskoy, V. et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 604, 502–508 (2022).
Davidson, E. H. The Regulatory Genome. Gene Regulatory Networks in Development and Evolution. Academic Press, https://doi.org/10.1016/B978-012088563-3.50019- (2006).
Rapoport, J. L., Addington, A. M., Frangou, S. & Psych, M. R. C. The neurodevelopmental model of schizophrenia: update 2005. Mol. Psychiatry 10, 434–449 (2005).
Ursini, G. et al. Convergence of placenta biology and genetic risk for schizophrenia article. Nat. Med. 24, 792–801 (2018).
Ursini, G. et al. Placental genomic risk scores and early neurodevelopmental outcomes. Proc. Natl Acad. Sci. USA 118, e2019789118 (2021).
Cannon, M. et al. Evidence for early-childhood, pan-developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort. Arch. Gen. Psychiatry 59, 449–456 (2002).
Niemi, L. T., Suvisaari, J. M., Tuulio-Henriksson, A. & Lönnqvist, J. K. Childhood developmental abnormalities in schizophrenia: evidence from high-risk studies. Schizophr. Res. 60, 239–258 (2003).
Sørensen, H. J. et al. Early developmental milestones and risk of schizophrenia: a 45-year follow-up of the Copenhagen Perinatal Cohort. Schizophr. Res. 118, 41–47 (2010).
Jauhar, S., Johnstone, M. & McKenna, P. J. Schizophrenia. Lancet 399, 473–486 (2022).
van Erp, T. G. M. et al. Cortical brain abnormalities in 4474 individuals with Schizophrenia and 5098 control subjects via the enhancing neuro imaging genetics through meta analysis (ENIGMA) consortium. Biol. Psychiatry 84, 644–654 (2018).
Birnbaum, R. & Weinberger, D. R. Genetic insights into the neurodevelopmental origins of schizophrenia. Nat. Rev. Neurosci. 18, 727–740 (2017).
Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Primers 1, 15067 (2015).
Perälä, J. et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch. Gen. Psychiatry 64, 19–28 (2007).
McGrath, J., Saha, S., Chant, D. & Welham, J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol. Rev. 30, 67–76 (2008).
Charlson, F. J. et al. Global epidemiology and burden of schizophrenia: findings from the global burden of disease study 2016. Schizophr. Bull. 44, 1195–1203 (2018).
Haukka, J., Suvisaari, J. & Lönnqvist, J. Fertility of patients with schizophrenia, their siblings, and the general population: a cohort study from 1950 to 1959 in Finland. Am. J. Psychiatry 160, 460–463 (2003).
McGrath, J. J. et al. The fertility and fecundity of patients with psychoses. Acta Psychiatr. Scand. 99, 441–446 (1999).
Crow, T. J. Schizophrenia as the price that Homo sapiens pays for language: a resolution of the central paradox in the origin of the species. Schizophr. Res. 31, 118–129 (2000).
Burns, J. K. Psychosis: a costly by-product of social brain evolution in Homo sapiens. Prog Neuropsychopharmacol Biol Psychiatry. 30, 797–814 (2006).
Burns, J. K. An evolutionary theory of schizophrenia: cortical connectivity, metarepresentation, and the social brain. Behav. Brain Sci. 27, 831–855 (2004).
Wynn, T. & Coolidge, F. L. The implications of the working memory model for the evolution of modern cognition. Int. J. Evol. Biol. 2011, 1–12 (2011).
O’Bleness, M., Searles, V. B., Varki, A., Gagneux, P. & Sikela, J. M. Evolution of genetic and genomic features unique to the human lineage. Nat. Rev. Genet. 13, 853–866 (2012).
Pollen, A. A., Kilik, U., Lowe, C. B. & Camp, J. G. Human-specific genetics: new tools to explore the molecular and cellular basis of human evolution. Nat. Rev. Genet. 1–25. https://doi.org/10.1038/s41576-022-00568-4 (2023).
Schmidt, E. R. E. & Polleux, F. Genetic mechanisms underlying the evolution of connectivity in the human cortex. Front. Neural Circuits 15, 1–16 (2022).
Prabhakar, S., Noonan, J. P., Pääbo, S. & Rubin, E. M. Accelerated evolution of conserved noncoding sequences in humans. Science 314, 786 (2006).
Bird, C. P. et al. Fast-evolving noncoding sequences in the human genome. Genome Biol. 8, 1–12 (2007).
Bush, E. C. & Lahn, B. T. A genome-wide screen for noncoding elements important in primate evolution. BMC Evol. Biol. 8, 1–10 (2008).
Lindblad-Toh, K. et al. A high-resolution map of human evolutionary constraint using 29 mammals. Nature 478, 476–482 (2011).
Gittelman, R. M. et al. Comprehensive identification and analysis of human accelerated regulatory DNA. Genome Res. 25, 1245–1255 (2015).
Pollard, K. S. et al. Forces shaping the fastest evolving regions in the human genome. PLoS Genet. 2, 1599–1611 (2006).
Capra, J. A., Erwin, G. D., Mckinsey, G., Rubenstein, J. L. R. & Pollard, K. S. Many human accelerated regions are developmental enhancers. Philos. Trans. R Soc. Lond. B Biol. Sci. 368, 20130025 (2013).
Hubisz, M. J. & Pollard, K. S. Exploring the genesis and functions of Human Accelerated Regions sheds light on their role in human evolution. Curr. Opin. Genet Dev. 29, 15–21 (2014).
Won, H., Huang, J., Opland, C. K., Hartl, C. L. & Geschwind, D. H. Human evolved regulatory elements modulate genes involved in cortical expansion and neurodevelopmental disease susceptibility. Nat. Commun. 10, 2396 (2019).
Doan, R. N. et al. Mutations in Human Accelerated Regions disrupt cognition and social behavior. Cell 167, 341–354.e12 (2016).
Pollard, K. S. et al. An RNA gene expressed during cortical development evolved rapidly in humans. Nature 443, 167–172 (2006).
Won, H., Huang, J., Opland, C. K., Hartl, C. L. & Geschwind, D. H. Human evolved regulatory elements modulate genes involved in cortical expansion and neurodevelopmental disease susceptibility. Nat. Commun. 10, 1–11 (2019).
Uebbing, S. et al. Massively parallel discovery of human-specific substitutions that alter enhancer activity. Proc. Natl Acad. Sci. USA 118, 1–11 (2021).
Girskis, K. M. et al. Rewiring of human neurodevelopmental gene regulatory programs by human accelerated regions. Neuron 109, 3239–3251.e7 (2021).
Wei, Y. et al. Genetic mapping and evolutionary analysis of human-expanded cognitive networks. Nat. Commun. 10, 1–11 (2019).
Li, L. et al. Gene expression associated with individual variability in intrinsic functional connectivity. Neuroimage 245, 118743 (2021).
Luppi, A. I. et al. A synergistic core for human brain evolution and cognition. Nat. Neurosci. 25, 771–782 (2022).
Xu, K., Schadt, E. E., Pollard, K. S., Roussos, P. & Dudley, J. T. Genomic and network patterns of schizophrenia genetic variation in human evolutionary accelerated regions. Mol. Biol. Evol. 32, 1148–1160 (2015).
Srinivasan, S. et al. Probing the association between early evolutionary markers and schizophrenia. PLoS One 12, 1–15 (2017).
Grasby, K. L. et al. The genetic architecture of the human cerebral cortex. Science 367, eaay6690 (2020).
Murray, G. K. et al. Could polygenic risk scores be useful in psychiatry? A review. JAMA Psychiatry 78, 210–219 (2021).
Raben, T. G., Lello, L., Widen, E. & Hsu, S. D. H. From Genotype to Phenotype: Polygenic Prediction of Complex Human Traits. Methods. Mol. Biol. 2467, 421–446 (2022).
Pergola, G., Penzel, N., Sportelli, L. & Bertolino, A. Lessons learned from parsing genetic risk for schizophrenia into biological pathways. Biol. Psychiatry 94, 121–130 (2023).
Guardiola-Ripoll, M. & Fatjó-Vilas, M. A systematic review of the human accelerated regions in Schizophrenia and related disorders: where the evolutionary and neurodevelopmental hypotheses converge. Int. J. Mol. Sci. 24, 3597 (2023).
Vassos, E. et al. An examination of polygenic score risk prediction in individuals with first-episode psychosis. Biol. Psychiatry 81, 470–477 (2017).
Calafato, M. S. et al. Use of schizophrenia and bipolar disorder polygenic risk scores to identify psychotic disorders. Br. J. Psychiatry 213, 535–541 (2018).
Smigielski, L. et al. Polygenic risk scores across the extended psychosis spectrum. Transl. Psychiatry 11, 1–11 (2021).
van Os, J. et al. Replicated evidence that endophenotypic expression of schizophrenia polygenic risk is greater in healthy siblings of patients compared to controls, suggesting gene-environment interaction. The EUGEI study. Psychol. Med. 50, 1884–1897 (2020).
Tolosa, A. et al. Rapid evolving RNA gene HAR1A and schizophrenia. Schizophr. Res. 99, 370–372 (2008).
Bhattacharyya, U., Bhatia, T., Deshpande, S. N. & Thelma, B. K. Genetic variations in evolutionary accelerated regions disrupt cognition in schizophrenia. Psychiatry Res. 314, 114586 (2022).
Bhattacharyya, U. et al. Probing the association between early evolutionary markers and schizophrenia. Schizophr. Bull. 109, 1–15 (2021).
Cheung, J. P., Tubbs, J. D. & Sham, P. C. Extended gene set analysis of human neuro-psychiatric traits shows enrichment in brain-expressed human accelerated regions across development. Schizophr. Res. 246, 148–155 (2022).
Padmanabhan, J. L. et al. Correlations between brain structure and symptom dimensions of psychosis in schizophrenia, schizoaffective, and psychotic bipolar i disorders. Schizophr. Bull. 41, 154–162 (2015).
Cavelti, M., Kircher, T., Nagels, A., Strik, W. & Homan, P. Is formal thought disorder in schizophrenia related to structural and functional aberrations in the language network? A systematic review of neuroimaging findings. Schizophr. Res. 199, 2–16 (2018).
Sun, J., Maller, J. J., Guo, L. & Fitzgerald, P. B. Superior temporal gyrus volume change in schizophrenia: a review on Region of Interest volumetric studies. Brain Res. Rev. 61, 14–32 (2009).
Braunsdorf, M. et al. Does the temporal cortex make us human? A review of structural and functional diversity of the primate temporal lobe. Neurosci. Biobehav. Rev. 131, 400–410 (2021).
Kringelbach, M. L. The human orbitofrontal cortex: linking reward to hedonic experience. Nat. Rev. Neurosci. 6, 691–702 (2005).
Jha, S. C. et al. Genetic influences on neonatal cortical thickness and surface area. Hum. Brain Mapp. 39, 4998–5013 (2018).
Wierenga, L. M., Langen, M., Oranje, B. & Durston, S. Unique developmental trajectories of cortical thickness and surface area. Neuroimage 87, 120–126 (2014).
Lyall, A. E. et al. Dynamic development of regional cortical thickness and surface area in early childhood. Cereb. Cortex 25, 2204–2212 (2015).
Strike, L. T. et al. Genetic complexity of cortical structure: differences in genetic and environmental factors influencing cortical surface area and thickness. Cereb. Cortex 29, 952–962 (2019).
Panizzon, M. S. et al. Distinct genetic influences on cortical surface area and cortical thickness. Cereb. Cortex 19, 2728–2735 (2009).
Rakic, P. Specification of cerebral cortical areas. Science 241, 170–176 (1988).
Mora-Bermúdez, F. et al. Differences and similarities between human and chimpanzee neural progenitors during cerebral cortex development. Elife 5, 1–24 (2016).
Eickhoff, S. et al. High-resolution MRI reflects myeloarchitecture and cytoarchitecture of human cerebral cortex. Hum. Brain Mapp. 24, 206–215 (2005).
Marek, S. et al. Reproducible brain-wide association studies require thousands of individuals. Nature 603, 654–660 (2022).
Ni, G. et al. A comparison of ten polygenic score methods for psychiatric disorders applied across multiple cohorts. Biol. Psychiatry 90, 611–620 (2021).
Gulsuner, S. et al. Genetics of schizophrenia in the South African Xhosa. Science (1979) 367, 569–573 (2020).
Stilo, S. A. & Murray, R. M. Non-genetic factors in Schizophrenia. Curr. Psychiatry Rep. 21, 100 (2019).
Schmitt, A., Falkai, P. & Papiol, S. Neurodevelopmental disturbances in schizophrenia: evidence from genetic and environmental factors. J. Neural Transm. 12, 1–11 (2022).
Canales-Rodríguez, E. J. et al. Age- and gender-related differences in brain tissue microstructure revealed by multi-component T2 relaxometry. Neurobiol. Aging 106, 68–79 (2021).
van den Heuvel, M. P. et al. Evolutionary modifications in human brain connectivity associated with schizophrenia. Brain 142, 3991–4002 (2019).
Canales-Rodríguez, E. J. et al. Structural abnormalities in bipolar euthymia: a multicontrast molecular diffusion imaging study. Biol. Psychiatry 76, 239–248 (2014).
Fujiwara, H., Yassin, W. & Murai, T. Neuroimaging studies of social cognition in schizophrenia. Psychiatry Clin. Neurosci. 69, 259–267 (2015).
Srinivasan, S. et al. Probing the association between early evolutionary markers and schizophrenia. PLoS One 12, e0169227 (2017).
Pardiñas, A. F. et al. Common schizophrenia alleles are enriched in mutation-intolerant genes and in regions under strong background selection. Nat. Genet. 50, 381–389 (2018).
Srinivasan, S. et al. Genetic markers of human evolution are enriched in Schizophrenia. Biol. Psychiatry 80, 284–292 (2016).
Liu, C., Everall, I., Pantelis, C. & Bousman, C. Interrogating the evolutionary paradox of schizophrenia: a novel framework and evidence supporting recent negative selection of schizophrenia risk alleles. Front. Genet. 10, 1–7 (2019).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276 (1987).
Peralta, V. & Cuesta, M. J. Validación de la escala de síntomas positivos y negativos (PANSS) en una muestra de esquizofrénicos españoles. Actas Luso Españolas de. Neurol.ía Psiquiátrica 22, 171–177 (1994).
Gomar, J. J. et al. Validation of the Word Accentuation Test (TAP) as a means of estimating premorbid IQ in Spanish speakers. Schizophr. Res. 128, 175–176 (2011).
Durbin, R. Efficient haplotype matching and storage using the positional Burrows-Wheeler transform (PBWT). Bioinformatics 30, 1266–1272 (2014).
Das, S. et al. Next-generation genotype imputation service and methods. Nat. Genet. 48, 1284–1287 (2016).
McCarthy, S. et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat. Genet. 48, 1279–1283 (2016).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 1–16 (2015).
Privé, F., Vilhjálmsson, B. J., Aschard, H. & Blum, M. G. B. Making the most of clumping and thresholding for polygenic scores. Am. J. Hum. Genet. 105, 1213–1221 (2019).
Mullins, N. et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat. Genet. 53, 817–829 (2021).
Quinlan, A. R. & Hall, I. M. BEDTools: a flexible suite of utilities for comparing genomic features. Bioinformatics 26, 841–842 (2010).
Roadmap Epigenomics Consortium et al. Integrative analysis of 111 reference human epigenomes. Nature 518, 317–329 (2015).
Fischl, B. et al. Automatically parcellating the human. Cereb. Cortex. Cereb. Cortex 14, 11–22 (2004).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31, 968–980 (2006).
Hibar, D. P. et al. Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Mol. Psychiatry 23, 932–942 (2018).
Smith, T. J. & Mckenna, C. M. A Comparison of Logistic Regression Pseudo R 2 Indices. Multiple Linear Regression Viewpoints. 39, 17–26 (2013).
Scherk, H. & Falkai, P. Effects of antipsychotics on brain structure. Curr. Opin. Psychiatry 19, 145–150 (2006).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8, 1–10 (2017).
Mowinckel, A. M. & Vidal-Piñeiro, D. Visualization of brain statistics with R packages ggseg and ggseg3d. Adv. Methods Pr. Psychol. Sci. 3, 466–483 (2020).
Acknowledgements
This study received project funding from the Brain & Behavior Research Foundation (NARSAD Young Investigator Award) to MF-V (grant ID 26206). Researchers were supported by: (i) Instituto de Salud Carlos III (ISCIII) through the contracts FI19/0352 to MG-R, CD22/00106 to MAG-L, and CP20/00072 to MF-V (co-funded by European Regional Development Fund (ERDF)/European Social Fund “Investing in your future”); (ii) la “Caixa” Foundation through the Junior Leader Fellowship contract LCF/BQ/PR22/11920017 to PF-C; (iii) the Swiss National Science Ambizione grant PZ00P2_185814 to EJC-R; (iv) Júlia Gil Pineda Research Fellowship to ER-C. We thank the Comissionat per a Universitats i Recerca del DIUE of the Generalitat de Catalunya (Agència de Gestio d’Ajuts Universitaris i de Recerca (AGAUR, 2021SGR01475). CeGen PRB3 is supported by grant PT17/0019 of the PE I + D + i 2013–2016, funded by ISCIII and ERDF.
Author information
Authors and Affiliations
Contributions
M.G.-R. and M.F.-V. conceived the study. M.G.-R. conducted the DNA extraction and sample normalisation for genotyping. E.J.C.-R., M.A.G.-L. and P.F.-C. pre-processed and segmented the MRI images. E.P.-C., P.F.-C., J.S., J.T., L.T. and E.R.-C. conducted the recruitment and/or the clinical evaluation. E.J.C.-R., R.S. and E.P.-C. designed the MRI protocols. M.G.-R., C.A. and A.A. performed the data curation. M.G.-R. conducted the formal statistical analyses and graphical representations with the help of C.A.-P., A.A., and M.L.-G. S.P. and M.F.-V. guided and reviewed the methodology. M.G.-R. and M.F.-V. interpreted the results. M.G.-R. and M.F.-V. wrote the first and subsequent drafts of the paper. M.F.-V. supervised the study activity planning and execution. M.F.-V. and E.P.-C. participated in the funding acquisition. All the authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks Noriyoshi Usui, Ruben Gur and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Karli Montague-Cardoso and Christina Karlsson Rosenthal. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guardiola-Ripoll, M., Almodóvar-Payá, C., Arias-Magnasco, A. et al. Human-specific evolutionary markers linked to foetal neurodevelopment modulate brain surface area in schizophrenia. Commun Biol 6, 1040 (2023). https://doi.org/10.1038/s42003-023-05356-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-023-05356-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.