Abstract
This review delves into the most recent advancements in applying artificial intelligence (AI) within neuro-oncology, specifically emphasizing work on gliomas, a class of brain tumors that represent a significant global health issue. AI has brought transformative innovations to brain tumor management, utilizing imaging, histopathological, and genomic tools for efficient detection, categorization, outcome prediction, and treatment planning. Assessing its influence across all facets of malignant brain tumor management- diagnosis, prognosis, and therapy- AI models outperform human evaluations in terms of accuracy and specificity. Their ability to discern molecular aspects from imaging may reduce reliance on invasive diagnostics and may accelerate the time to molecular diagnoses. The review covers AI techniques, from classical machine learning to deep learning, highlighting current applications and challenges. Promising directions for future research include multimodal data integration, generative AI, large medical language models, precise tumor delineation and characterization, and addressing racial and gender disparities. Adaptive personalized treatment strategies are also emphasized for optimizing clinical outcomes. Ethical, legal, and social implications are discussed, advocating for transparency and fairness in AI integration for neuro-oncology and providing a holistic understanding of its transformative impact on patient care.
Similar content being viewed by others
Introduction
Central nervous system (CNS) tumors, whether primary or secondary, exert a significant impact on global health, accounting for over 250,000 reported cases annually, marking them as a substantial global concern1,2. In 2022, an estimated 26,670 malignant and 66,806 non-malignant CNS tumors were diagnosed in the US population3. Notably, glioblastoma, a fast-growing, aggressive, and malignant type of brain tumor, emerges as a primary contributor to morbidity and mortality among adult brain tumors, exhibiting a disconcerting 6.9% 5-year survival rate and contributing to 10,000 annual deaths in the US4,5. These numbers highlight the current shortcomings in treating brain tumors.
Despite many clinical trials and decades of research, incurable brain tumors with grim prognoses exist, such as the diffuse midline glioma (DMG) seen in children and glioblastoma in adults6. This urgency highlights the need for a personalized treatment approach, which may offer the highest likelihood of cure while minimizing potential toxicity to the patient. However, the development of personalized strategies faces hurdles due to the difficulty of generalizing approaches derived from data originating in a solitary institution or a limited consortium of institutions, and restricted access to advanced technologies and clinical trials, primarily concentrated in specialized centers7. This becomes a critical concern, especially when contemplating the ethical ramifications associated with developing approaches based on data lacking representation across diverse demographics. Alarmingly, individuals with glioblastoma from lower socioeconomic backgrounds are less likely to undergo O6-Methylguanine-DNA-methyltransferase (MGMT) testing8. The absence of MGMT testing may skew predictions and contribute to late-stage diagnoses with larger and more challenging tumors. Moreover, this demographic is less frequently provided with a combination of diverse treatment modalities, leading to lower survival rates9.
For a patient suspected of harboring a brain tumor, the assessment typically initiates with a physical exam and neuroimaging, followed by a biopsy or tumor resection in cases where it is feasible, and subsequent histologic and molecular analyses of extracted tissue conducted through pathology. If deemed necessary, serum or cerebrospinal fluid (CSF) biomarker evaluations may also be performed10. Following these assessments, the clinical team must decide on optimal therapy, considering the standard of care, ongoing clinical trials, patient comorbidities, and risks of toxicity. Treatment response is monitored longitudinally through serial MRIs and, occasionally, other blood or CSF biomarkers11. Decisions regarding brain tumor treatment often involve multidisciplinary meetings between neuro-oncologists, neurosurgeons, neuroradiologists, molecular pathologists, and neuropathologists, underscoring the complexity of these decisions12 (Fig.1).
a AI augments the capabilities of neuro-oncologists/radiation-oncologists by enabling integrated diagnosis, offering deeper insights into the disease, facilitating precise prognosis by predicting outcomes, and assisting in patient stratification to tailor treatment plans to individual needs. b AI supports neuroradiologists by leveraging MRI images for automated detection and tumor segmentation, identifying molecular subtypes of tumors, providing quantitative measurements, and delivering diagnostic assistance to distinguish tumors from necrotic regions, all while ensuring automated quality checks. c AI aids neurosurgeons during surgery, contributing to surgical margin assessment and offering real-time diagnosis information and guidance, enhancing surgical precision and patient outcomes. d AI assists neuropathologists in the analysis of fresh/FFPE samples, providing automated measurement of features, aiding in tumor classification and grading, improving tumor detection, and delivering comprehensive analysis of cellular and tissue structures through histo-molecular classification. e Handling mutation data, single-cell information, methylation patterns, RNA sequencing, and more, AI empowers molecular pathologists by supporting biomarker identification, pathway identification, treatment response prediction, variant identification, and serving as a diagnosis assistant, streamlining the complex molecular analysis process (Created with BioRender.com).
However, these steps in disease management are ridden with challenges, and errors may lead to patient morbidity and mortality13. The challenges include the need for precise disease diagnosis and staging to guide clinical decisions, the continuous monitoring of post-treatment disease progress, which can be complicated by signals from neighboring neural tissue, and the growing significance of identifying genotype patterns14. These genotype patterns have a substantial impact on tumor behavior and clinical outcomes15. Ultimately, the challenges of managing brain tumors arise from various factors, including the complexities of the brain, limited accessibility for accurate imaging and biopsy procedures, inherent heterogeneity of tumor biology, variable progression rates, individual variability in treatment susceptibility, and relative lack of reliable biomarkers predictive of prognosis1,16,17. The sensitivity of neural tissue to standard treatment modalities, including surgery, radiation, and chemotherapy, further complicates their care18.
Artificial intelligence (AI) shows promise as a transformative tool in neuro-oncology, currently addressing challenges across various clinical management stages. In brain tumor management, AI demonstrates its potential across diagnosis, prognosis, and treatment planning by accelerating and enhancing MRI imaging19, detecting abnormalities, optimizing workflows, providing accurate measurements, analyzing extensive medical imaging data, and identifying patterns not easily discernible to human observers20. It has significantly advanced the field by providing detailed image analysis for diagnostics, tumor grading, prognosis determination, and treatment response assessment. It also facilitates surgical and nonsurgical treatment planning21, accelerates drug discovery22, and facilitates recurrence monitoring. AI tools can be incorporated into clinical trials, aiming to improve patient outcomes and may provide the path toward personalized therapy15,23. In clinical neuroimaging, AI plays a crucial role in tasks such as identifying tumor boundaries and types, refining pre-therapeutic planning, and assessing post-therapeutic responses24. The capacity for AI to process extensive datasets offers a transformative approach to precision medicine, potentially addressing commonly encountered pain points at all steps of the patient care experience25,26,27 (Fig. 1). Additionally, it holds promise in ameliorating global healthcare disparities by providing democratized access to diagnostic, prognostic, and therapeutic strategies28,29.
Recently, there has been growing exploration of integrating AI tools into radiological and pathological workflows, suggesting potential advancements in neuro-oncology30,31. In brain tumor analysis, AI serves as a comprehensive framework that encapsulates machine learning (ML) and deep learning (DL) techniques, computer vision (CV), and their integration into Computational Biology. ML algorithms within AI contribute to pattern recognition in imaging and genomic data, while DL, a subset of ML, excels in intricate feature extraction. Computer vision, whether through classical image processing techniques or advanced DL methods, interprets visual data for precise medical image analysis. Computational biology leverages AI, ML, and DL to analyze extensive biological datasets, aiding in understanding the genetic and molecular aspects of brain tumors (Supplementary Table 1). The synergy among these techniques enhances the depth and accuracy of brain tumor characterization, influencing diagnosis, prognosis, and treatment planning.
In conducting this review, a comprehensive literature search was conducted across several electronic databases. The search was focused on recently published articles, with an emphasis on studies related to AI applications in brain tumor diagnosis, prognosis, and precision treatment. Our search strategy prioritized peer-reviewed articles, systematic reviews, meta-analyses, and landmark studies in the field. This narrative review provides a comprehensive understanding of AI’s pivotal role in managing primary malignant brain tumors, focusing on gliomas. It explores AI applications in brain tumor diagnosis, prognosis, treatment planning, and predictive analytics. Addressing the multifaceted nature of AI in neuro-oncology, we discuss biomarkers, ethical implications, innovative methods, and challenges, including considerations for racial and sex-specific differences within AI applications and efforts to address disparities in current work limitations. What sets our review apart is its explicit focus on integrating AI in radiology, pathology, and genomics for comprehensive brain tumor analysis. Unlike previous papers, our review emphasizes the convergence of AI applications across radiology, pathology, and genomics, providing a holistic approach to brain tumor diagnostics, prognostics, and treatment planning. While many prior reviews have discussed AI in neuro-oncology broadly, they often lack a specific emphasis on the synergistic integration of AI across these critical domains. Concentrating on diagnostic, prognostic, and treatment planning within the imaging domain, our paper not only explores the latest advancements in AI tailored to pathology, radiology, and genomics but also addresses the gaps left by previous reviews in fully comprehending the interconnected roles of these disciplines in brain tumor management. This focused approach contributes a unique perspective, detailing AI’s transformative role in refining imaging-based diagnoses, prognoses, and treatment planning, which were not thoroughly covered by the broader, less-specialized reviews in the field.
Data types and datasets for brain tumor analysis
Brain tumor analysis relies on a range of data types that are effectively utilized by AI algorithms to unveil crucial characteristics. Key data categories encompass imaging data, genomic data, and clinical data. Medical imaging techniques, such as MRI and CT, offer the opportunity to extract intricate visual features about tumor size, location, morphology, and texture. The current standard for brain tumor imaging involves multi-parametric MRI, including sequences like pre- and post-contrast T1-weighted, T2-weighted, fluid-attenuated inversion recovery (FLAIR), diffusion-weighted (DWI), and susceptibility-weighted imaging (SWI) as commonly obtained sequences. High-volume neuro-oncology centers often incorporate additional techniques like MR spectroscopy and perfusion imaging11,32. Beyond standard imaging, radiomics extracts quantitative features, while histopathological data, derived from biopsies or surgical resections, encompasses tumor cell morphology and tissue architecture. Genomic data, derived from DNA and RNA sequencing, transcriptomic analysis, and methylation analysis, aids in classifying subtypes and predicting tumor aggressiveness33. Moreover, prominent molecular biomarkers play a pivotal role in discriminating between brain tumor subtypes1,9,34. These include mutations in IDH for astrocytomas and oligodendrogliomas, TERT promoter mutations for glioblastomas, EGFR amplification for glioblastomas, gain of chromosome 7 and loss of chromosome 10 for glioblastomas, ATRX mutations for astrocytomas, MGMT promoter methylation for glioblastomas, co-deletion of 1p and 19q chromosomes for oligodendrogliomas, and distinct molecular subtypes for medulloblastoma (MBs)9 (See Tables 2 and 3). Lastly, Clinical data, inclusive of patient history, medical records, and treatment responses, contributes to a comprehensive diagnostic profile, with outcomes data serving as a crucial reference for survival prediction models (see Table 1).
In addition to more standardly employed data types, innovative approaches like liquid biopsies have emerged for the early detection of brain tumors35. Circulating tumor DNA (ctDNA) analysis, a non-invasive method, monitors tumor mutations and genetic changes through fragments of tumor DNA in the bloodstream36,37. The integration of these diverse data types and advanced technologies enables a new era of accurate, minimally invasive, and effective approaches for diagnosing and treating brain tumors, overcoming the limitations of conventional diagnostic methods. The integration of multiple data sources through multimodal data fusion enhances analyses accuracy by offering a more comprehensive view of the tumor’s characteristics and behavior38(Fig. 2). A concise overview of each data type, including its description and purpose, is provided in Table 1.
Shown is the structural framework of a multimodal integration method designed to improve brain tumor management. The process involves the assimilation of data from five different sources, each contributing unique information. From MRI scans, radiomic data is generated. This data includes segmented MRI images achieved through AI-driven segmentation techniques, providing information about the tumor’s spatial characteristics. Blood samples yield ctDNA, allowing for the extraction of epigenomic, fragmentomic, and genomic alterations that inform the molecular landscape of the tumor. CFS samples provide cell-free DNA (cfDNA), offering genomic alteration information and contributing to a comprehensive understanding of the tumor’s genetic profile. Formalin-fixed paraffin-embedded (FFPE) tissue samples provide transcriptomic and molecular pathology data, offering information about gene expression and cellular structure. Clinical information such as age, race, gender, and electronic medical records (EMR) data supplement the molecular and imaging data, enriching the patient’s profile. For each of these modalities, feature extraction is performed, generating a set of informative characteristics. Subsequently, predictive models are applied to each dataset to estimate key outcomes related to diagnosis, prognosis, and treatment response. In the late multimodal integration, the predictions from these distinct models are fused to improve performance and precision. By synthesizing information from diverse sources and modalities, the integrated approach enhances the reliability and accuracy of neuro-oncological diagnosis, prognosis, and treatment response prediction (Created with BioRender.com).
In addition to the institutional datasets, numerous public datasets play a crucial role in evaluating AI-based algorithms for brain tumor diagnosis, prognosis, and treatment planning. Tailored to diverse research needs, these datasets cover various aspects of the disease. The Cancer Imaging Archive (TCIA) is notable among general brain tumor datasets, offering a comprehensive repository of medical imaging data, including MRI, CT, and PET scans for various tumor types39. The MICCAI BraTS Challenge provides standardized brain tumor segmentation datasets annually, ideal for assessing algorithms focused on precise tumor delineation40.
For specific tumor types, resources such as the NCI TARGET dataset include dedicated sections for glioblastoma (TCGA-GBM) and lower-grade gliomas (TCGA-LGG)41. Additional platforms such as the open data alliance and the NCI data commons offer open-access datasets across scientific domains, including medical and brain tumor datasets42,43. Selecting the most appropriate dataset depends on factors like tumor type, imaging modality, data type (MRI, CT, PET, etc.), availability of ground truth annotations, and data size, allowing researchers to align their choice with specific research interests for AI-driven investigations into brain tumor diagnosis and treatment planning.
Advancements in AI-enhanced preprocessing for precision brain tumor analysis
In brain tumor analysis, AI has addressed the challenges of navigating brain anatomy and tumor variability and significantly enhanced crucial preprocessing steps for accurate diagnosis, prognosis, and treatment planning. Addressing issues of spatial consistency, AI-powered algorithms, such as those integrated into the BrainNet viewer, correct artifacts and distortions in MRI images44. This correction facilitates more precise tumor localization and segmentation, which is crucial for effective brain tumor analysis.
Moreover, AI streamlines the intricate process of tumor localization with remarkable accuracy, as demonstrated by algorithms evaluated on the BraTS dataset40. Notably, some AI-empowered methods have achieved high accuracy in localizing tumors, thereby enhancing efficiency for radiologists and reducing the potential for human error45,46. Image segmentation via CNNs, which are adept at uncovering complex patterns from data, has emerged as a powerful tool47,48,49,50,51. AI-driven algorithms, including the nnU-Net algorithm52, demonstrate exceptional proficiency in automating the crucial task of segmenting normal tissues in medical images. This segmentation is vital for tumor analysis, assisting radiologists in identifying areas to avoid during radiation therapy or surgery52. In recent developments, the federated learning framework has demonstrated comparable or superior results in the automated segmentation of rare pediatric tumors from MRI images. This approach leverages data from diverse institutions while ensuring the utmost confidentiality of patient information24.
The integration of multimodal data enhances detection efficacy by tapping into diverse information sources53. The landscape of DL introduces innovative architectures, with some notable exemplars, including the 3D U-Net46, DeepMedic54, and V-Net55. The 3D U-Net, designed to excel in segmenting 3D images of glioblastoma, and recognized for its straightforward training and consistent effectiveness, achieves remarkable results in brain tumor segmentation. DeepMedic54, known for its robustness in managing noise and artifacts, stands as a strong competitor to the 3D U-Net, trained on glioma images. The V-Net, a nascent innovation designed to accurately segment volumetric medical images, establishes its prowess in segmenting both 2D and 3D MRI images55. Overall, AI’s role in these preprocessing steps empowers radiologists to conduct brain tumor analysis with heightened precision and efficiency.
AI in brain tumor diagnosis
Brain tumor diagnosis involves the identification and characterization of abnormal growths or masses within the brain, utilizing various medical imaging, pathological, and clinical methods to determine the nature, location, and characteristics of the tumor55. Brain tumors vary based on their origin, location, histology, malignancy, and patient age, and categorizing them is crucial for diagnostics, prognosis, and treatment planning55. These tumors consist of diverse subtypes, each characterized by distinct cellular origins and histological features. While pediatric-type low and high-grade gliomas and MB are most common in children, glioblastomas, diffuse gliomas, and meningiomas predominate in adults56. Given their significance, the predominant focus of research has been on glioblastoma and other diffuse glioma in adults and MB, and pediatric type low- and high-grade glioma in children57,58. Accurate identification of the tumor subtype empowers clinicians to customize diagnostic methods, predict disease behavior, and inform targeted therapies59. Unique genetic and histological signatures associated with different tumor types provide information about aggressiveness and treatment responses, guiding the selection of imaging modalities, biomarker assessments, and treatment plans60.
Brain tumors are often identified on CT performed in the emergency room setting, prior to being further characterized via MRI, and are definitively diagnosed via histopathologic examination56. Standard of care in neuropathology now includes molecular and genetic testing for many tumor types, guided by initial histologic findings57. Current diagnosis methods face challenges58,59,60 such as early detection due to tumor concealment61, imaging limitations20, and issues of visualizing small or deep-seated tumors62,63, difficulties in distinguishing tumor types64, invasive procedures with associated risks65, and the heterogeneity of brain tumors66. These approaches are hindered by time-consuming processes, limited accessibility, and interpretation variability among experts, highlighting the need for advanced AI-based methods16,67.
AI can add value at all steps of tumor diagnosis, with the majority of current studies attempting to create predictive models trained using imaging data, pathology data, or both data modes combined68. The integration of AI models in brain tumor diagnosis shows potential, particularly in distinguishing between glioma and solitary brain metastases using quantitative image analysis methods69,70. Neuroimaging provides a unique glimpse into the unaltered tumor in its entirety, while pathologic analyses provide a more in-depth look at the cellular and molecular features of the tumor. ML, as a key element of AI, is contributing to advancements in brain tumor diagnostics by enhancing accuracy, expediting image analysis, enabling early detection, and improving differentiation between tumor types. Recent progress in CV, ML, and DL holds the potential for addressing challenges and improving patient care in brain tumor diagnosis45.
AI-empowered radiology, and histology-based diagnostic methods
Radiology- and histology-based brain tumor diagnosis involves extracting quantitative features from medical images such as MRI scans or H&E WHI to capture tumor morphology, texture, and spatial relationships. Traditional feature extraction approaches such as texture analysis (Gray-level co-occurrence matrix (GLCM), Gray-level run-length matrix (GLRLM), and Haralick71,72), Shape analysis73, Intensity analysis74, Wavelet-based analysis75, are complemented by newer approaches. Then, ML and DL construct predictive models, enabling a personalized, data-driven approach to diagnosis31,76,77. Common techniques comprise CNNs, RNNs, vision transformers, generative adversarial networks (GANs)78, support vector machines, and random forests77 (Supplementary Table 1). Models generated from multiple sequences, such as mpMRI have been shown to be more accurate when compared to single sequence models79 for tumor detection, assessing grades, and guiding treatment planning80.
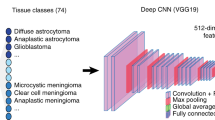
The histology-based diagnosis methods, aligned by the 2021 WHO (World Health Organization) CNS classification book, are central to brain tumor pathology. The histology-based analysis encompasses various molecular techniques leveraging histological data to enhance brain tumor diagnosis. Methylome profiling, a recently influential technique using AI/ML-based classifiers, has become an influential technique for categorizing and diagnosing brain tumors81. While the 2021 WHO classification supports the use of methylome classifiers for various brain tumors either as essential or desirable criteria, there’s ongoing debate over the best method and the limited accessibility of diagnostic tests34. DeepGlioma82, an AI-based diagnostic screening system, offers rapid results (<90 seconds) by streamlining the molecular diagnosis of GMGs using stimulated Raman histology (SRH) images. This innovative system has been developed and validated on a multicenter cohort, highlighting its potential for rapid and accurate brain tumor diagnosis82.
Furthermore, innovative approaches utilizing radiomics on MRI perfusion scans demonstrated the ability to predict IDH mutations, providing valuable information for diagnosis and treatment planning83. Terahertz spectroscopy has been explored as a non-invasive technique for predicting IDH mutations in glioma tissue samples, presenting a promising alternative to existing methods84. Moreover, advanced analysis techniques applied to 18F-FET PET/CT scans have enabled the prediction of both glioma grade and IDH mutation status in untreated patients85. Notably, a deep learning imaging signature (DLIS) has been developed, offering accurate prediction of 1p/19q co-deletion in diffuse lower-grade gliomas through pre-operative MRI scans, presenting a non-invasive alternative with significant diagnostic potential86.
The Integration of immunohistochemistry, methylation profiling, chromosomal microarray, scRNA-seq87, and NGS, with histology-based analysis could further enhance brain tumor diagnosis81,88. While conventional approaches, utilizing imaging, tissue biopsies, and genetic testing, confidently identify many brain tumors by combining histology with specific genetic changes, exceptions exist, such as high-grade astrocytoma with piloid features, introduced in the 2021 WHO classification88,89. This particular condition demands methylome profiling for diagnosis89, but its rarity suggests that methylome classifiers are best suited for specific cases with atypical clinical and pathological presentations. A recent deep learning method named “Sturgeon,” can rapidly and accurately classify CNS tumor types during surgery using sparse methylation array data obtained from nanopore sequencing produced during surgery. It classifies CNS tumors within 40 minutes after starting sequencing, with an accuracy of 72% in real-time surgical settings90. This method allows surgeons to make more informed decisions about the extent of resection, potentially reducing the risk of complications and improving patient outcomes.
AI in brain tumor prognosis
Prognosis in neuro-oncology involves estimating disease progression for an individual, considering treatment planning, disease stage, and site91. Key metrics are overall survival (OS), and progression-free survival (PFS), crucial for assessing prognosis and guiding treatment92. However, conventional methods relying on disease stage and clinical variables face limitations, including interpretational complexities, biases, and the need for extensive datasets. Achieving precision for personalized care in predicting recurrence and survival remains challenging with conventional methods.
In brain tumor care, AI plays a pivotal role in advancing prognostic capabilities. ML and DL techniques are increasingly being harnessed to predict OS, and PFS, leveraging features extracted from pre-treatment imaging data. Noteworthy studies, including radiomic signatures from T1 and FLAIR MRI scans of glioblastoma patients69, and T1, T2, and FLAIR scans from treatment-naïve patients, show significant promise in predicting PFS and OS93,94. The AI models outperform routine clinical variables and demonstrate excellence when combined with clinical attributes in glioblastoma patients95,96. Remarkably, models based on T2-weighted MRI97 and radiomic features from peritumoral edema reveal associations with survival outcomes, site of recurrence, and molecular subtype98, especially in glioma97, and glioblastoma patients99. DL-based models are created to identify tumors and forecast the site of recurrence, sometimes before radiologists can detect it100. These models, using various imaging methods, highlight AI’s exceptional predictive capabilities97,99 (Table 2).
Furthermore, Intra-tumoral heterogeneity and cell-state plasticity have been identified as key drivers for the therapeutic resistance of glioblastoma30. Spatial transcriptional profiles and prognosis from histology images were predicted using this DL framework, shedding light on the potential of AI in unraveling complex aspects of tumor behavior30. Additionally, the identification of IDH mutations has been leveraged to guide prognosis, while the definition of glioblastoma has been refined through the analysis of TERT promoter, EGFR amplification, gain of chromosome 7, and loss of chromosome 10. Additionally, H3F3A has emerged as a key marker for aggressive pediatric tumors101.
AI in brain tumor therapeutic management
In addition to adding value to both diagnostic and prognostic capabilities, AI has been used for improving brain tumor treatment planning and treatment response assessment102. It transforms therapeutic approaches and enhances precision by aiding in the identification and characterization of brain tumors. It guides clinicians in determining the most suitable treatment strategies for individual patients. This multifaceted process involves diverse techniques, including imaging, clinical assessments, biopsies, and molecular analyses, for precise determination of tumor presence, type, location, and extent.
AI-based methods excel in predicting therapy responses, enabling improved treatment planning across various cancers103. Novel approaches, such as predicting responses to gamma knife radiosurgery for metastatic brain tumors using radiomic features104 from contrast-enhanced T1 and FLASH scan and utilizing predictive models based on pre-treatment ADC maps for forecasting responses to radiation therapy, showcase AI’s efficacy104. Integrated models, combining radiomics with clinical attributes, effectively assess radiotherapy responses for patients with brain metastasis from primary breast and lung cancer across multicenter patient cohorts105. Spatial heterogeneity analysis of peritumoral edema (ED) in glioblastoma aids in identifying high-risk habitats within ED, leading to enhanced treatment planning106. While identifying the crucial marker MGMT for temozolomide (TMZ) resistance in glioblastoma patients presents challenges, AI-based radiomic methods emerge as predictors of both MGMT status and TMZ response, providing valuable insights for informed treatment decisions101,107 (Table 3).
Integrative multimodal and multiscale analysis
In multimodal and multiscale approaches, the hope is for a more comprehensive understanding of brain tumors through the integration of genomics, pathomics, and radiomics data. Genomics, especially through techniques like NGS, takes a prominent role in unraveling the genetic landscape of brain tumors, providing information into their genomic alterations88. Molecular subtyping and biomarkers identified play a critical role in personalized precision medicine, impacting early detection, prognosis, and treatment response prediction. This integrative approach, when combined with clinical data, advances our comprehension and lays the groundwork for tailored treatments targeting specific genetic alterations.
Complementing this genomic foundation, multimodal imaging techniques such as MRI, CT, and PET contribute a rich layer to the integrative tapestry, albeit with challenges of cost and time108. When fused with clinical expertize and other diagnostic data, multimodal imaging significantly enhances diagnostic accuracy. The integration of genomics and radiomics, facilitated by AI, emerges as a revolutionary force in understanding and treating brain tumors.
Furthermore, AI’s advancements extend beyond unimodal predictions, ushering in an era of multimodal prognostic and treatment approaches. These multiscale, multimodal approaches extract features from diverse data sources, including radiomic images and multimodal imaging, resulting in a more comprehensive and accurate understanding of the disease trajectory100 (Fig. 2).
Challenges and limitations of AI in brain tumor diagnosis, prognosis, and treatment
Despite the successful integration of AI models in different steps of brain tumor management, challenges persist. These challenges include restricted access to high-quality data, concerns regarding the interpretability and explainability of DL models, and the need for generalizability across diverse populations and tumor types109. The reproducibility of radiomic-based features across different institutes faces challenges due to variations in image acquisition parameters, including machines, models, and contrast amounts110. Particularly, achieving reproducibility is more complex in MR radiomics compared to CT radiomics111. To standardize radiomics, the introduction of the radiomic quality score (RQS) has been pivotal112. However, despite the importance of validation of the AI method in neuro-oncology using external dataset, only 29.4% of original studies included external validation113.
Additionally, in brain tumors management, it becomes evident that racial disparities introduce intricate dynamics shaped by race, socioeconomic variables, and geographical influences114. This complexity extends to various aspects, including recommendations for brain tumor surgery115, emphasizing the importance of addressing such disparities in AI-based methods throughout the spectrum of brain tumor management to advance cancer care. Moreover, disparities in brain tumor rates and outcomes, particularly in glioblastoma, manifest differently between males and females116. This underscores the necessity for AI-based approaches to factor in sex-related influences across incidence, survival, tumor biology, genetics, treatment response, and prognosis. The key advantages of these models lie in offering enhanced predictions for personalized treatment and the potential for early detection by accounting for gender-specific characteristics.
Ethical, legal, and social implications of AI in brain tumor management
The integration of AI in brain tumor diagnosis, prognosis, and treatment raises critical ethical, legal, and social considerations117. Key ethical concerns include ensuring patient privacy through robust data privacy measures, obtaining informed consent, addressing algorithmic fairness, and promoting transparency in AI algorithms and accountability to build and maintain patient trust28. Innovations like federated learning aim to tackle the privacy challenge in AI by enabling collaborative model training among multiple parties without the need to share raw data24. Ethical imperatives extend to addressing biases and ensuring equitable access. Legal considerations, encompassing liability for AI-generated errors, medical malpractice standards, and regulatory compliance, underscore the need for robust legal frameworks. Collaborative efforts involving policymakers, regulatory bodies, and legal experts are crucial to clarify responsibilities, protect patient safety, and foster responsible AI development. Social implications, such as impacts on patient-doctor relationships, patient empowerment, and healthcare disparities, require careful consideration. AI has the potential to empower patients by providing personalized information and enabling shared decision-making117,118. However, the equitable access and affordability of AI-driven healthcare need to be addressed to avoid exacerbating existing disparities117,118.
Discussion
This review highlights the transformative impact of AI in brain tumor management, signifying a paradigm shift in healthcare that addresses longstanding challenges. AI’s proficiency in ML and DL techniques, specifically in image segmentation, spatial consistency, and prediction, enhances precision in identifying and characterizing brain tumors. This precision contributes to improved diagnostics, prognosis, and personalized treatment planning. The seamless integration of diverse data types, from medical imaging to genomics, along with clinical history, enables a holistic understanding of tumor characteristics, shaping prognosis and personalized treatment plans. AI’s potential to empower clinicians with real-time monitoring, enhanced treatment planning, and optimization is emphasized, promising improved patient outcomes.
The prognostic capabilities of AI-based models surpass routine clinical variables, providing superior predictive accuracy and refining survival predictions30. The integration of AI in predicting treatment response, survival time, and site of recurrence is a significant advancement, enabling precise, personalized therapies tailored to individual tumor characteristics and patient-specific data. AI-driven diagnosis not only facilitates real-time monitoring but also improves treatment planning and optimization. This section highlights AI’s potential to deliver more precise, personalized, and effective interventions, contributing to enhanced patient outcomes. Clinical decision support systems, empowered by AI, not only provide evidence-based treatment recommendations but also contribute to ongoing research by generating novel insights and biomarkers.
Ethical considerations in the integration of AI in brain tumor diagnosis, prognosis, and treatment are acknowledged, covering data privacy, algorithmic fairness, legal liability, and social implications. Robust legal frameworks and collaborative efforts such as federated learning are deemed necessary to address these challenges for responsible AI development and societal acceptance in healthcare. Despite challenges such as data collection costs and interpretational complexities, AI integration holds substantial promise, offering prospects for precise and personalized patient care in the future. However, workforce changes and training may be necessary to effectively integrate AI technologies into healthcare settings. The ethical and societal acceptance of AI in healthcare depends on transparent communication, addressing privacy concerns, and promoting fair and inclusive practices.
Overall, AI extends its influence into treatment planning, revolutionizing therapeutic strategies and significantly contributing to improved patient outcomes. The integration of AI into the treatment landscape holds promise for personalized and effective interventions in neuro-oncology.
A vision for the future: a spectrum of approaches
The integration of AI in brain tumor diagnosis, treatment, and prognosis has seen significant progress, yet there are still gaps and promising future directions to explore. Multimodal data integration108, real-time monitoring, diagnosis, and adaptive treatment strategies hold the potential to enhance diagnostic accuracy and treatment outcomes90. AI can play a critical role in long-term prognostication and survivorship care planning, aiding in treatment decision-making. Bridging the gap between clinical practice and research through data-sharing networks can accelerate AI model development and validation. Transparency and interpretability of AI models are essential for gaining trust and acceptance in clinical settings119,120. Ethical considerations and human-centered design principles must be prioritized to ensure responsible and patient-centric AI integration. By addressing these aspects, AI has the potential to revolutionize brain tumor care and improve patient outcomes120.
Envisioning the future of brain tumor analysis, DL stands at the forefront, but various techniques beckon exploration based on specific applications and data availability. Improved imaging methods, such as functional magnetic resonance imaging (fMRI)121 and diffusion tensor imaging (DTI)122, provide more precise tumor characterization, despite challenges like sensitivity to noise, head motion, magnetic field distortions, and computational expenses123,124. Computational advancements, notably CNNs and Transformer-based models, enhance accuracy in the detection and classification of brain tumors125,126,127. Multimodal data fusion108, encompassing MRI, CT, and PET scans38, along with transfer learning using pre-trained models from vast image datasets, addresses the challenge of limited labeled medical data77 (Supplementary Table 1).
Graph-based methods leverage intricate brain region relationships128, with graph neural networks (GNNs) and graph-based convolutional networks (GCNs) illuminating the path of modeling brain connectivity and uncovering tumor-associated anomalies129. Radiomics and feature engineering extract an array of quantitative features from medical images, with ML algorithms illuminating patterns and correlations. Explainable AI (XAI), a pivotal facet, ensures algorithm transparency and interpretability, a cornerstone in medical applications130,131. Recent endeavors have gravitated toward devising AI models with explicable outputs, fostering clinicians’ comprehension of decision-making processes, and thus nurturing trust in automated brain tumor detection and classification. Data augmentation and synthesis techniques, encompassing image rotation, scaling, flipping, and the ingenuity of GANs, fortify the training dataset’s robustness78,127. Additionally, AutoML and hyperparameter optimization tools streamline the optimization of architecture and hyperparameters in brain tumor detection algorithms, culminating in more efficient and precise models.
Collaborative platforms and datasets, such as federated learning24,132 burgeoning repositories of meticulously annotated brain tumor data, expedite algorithmic training, evaluation, and innovation while catalyzing benchmarking efforts. The realm of real-time detection, propelled by advances in hardware such as graphics processing units (GPUs) and field-programmable gate arrays (FPGAs), unlocks the potential for real-time processing of medical images90,133. Such real-time algorithms hold the promise of streamlining clinical workflows and elevating patient care. The recent utilization of Large Language Models (LLMs) in neurological research demonstrates a remarkable capacity to analyze diverse data sources, offering significant contributions to early diagnosis, patient support, and clinical assistance. Noteworthy challenges, including concerns related to data privacy and biases, highlight the imperative for collaborative endeavors to ensure the responsible development of LLMs in neurology134 (Supplementary Table 1).
Conclusions
We explored the transformative applications of AI, including CV, ML, and DL, in managing brain tumors. AI shows significant promise in diagnosis, prognosis, and treatment planning by effectively detecting and classifying brain tumors from medical images. Through radiomic, pathomic, and genomic analyses, AI contributes to precise tumor characterization. In treatment, AI plays a crucial role in planning, optimization, and response prediction, supporting personalized recommendations and real-time monitoring. The integration of AI-driven approaches aligns with precision medicine and patient-centered care. However, the adoption of AI in brain tumor management requires careful consideration of ethical, legal, and social implications, addressing concerns related to data privacy and healthcare disparities.
Future directions include bridging research gaps, exploring LLM models, multimodal data integration, and advancing real-time monitoring. AI models trained on diverse datasets hold promise for predicting treatment responses and improving patient outcomes. Ongoing development and fine-tuning are essential for uncovering the full potential and challenges in the clinical management of brain tumors, positioning AI as a valuable tool in research and practice.
References
Brain tumors - classifications, symptoms, diagnosis and treatments. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Brain-Tumors.
Fan, Y. et al. Burden and trends of brain and central nervous system cancer from 1990 to 2019 at the global, regional, and country levels. Arch. Public Health 80, 209 (2022).
Ostrom, Q. T. et al. CBTRUs statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015-2019. Neuro. Oncol. 24, V1–V95 (2022).
About Glioblastoma. https://braintumor.org/events/glioblastoma-awareness-day/about-glioblastoma/. National Brain Tumor Society.
Fekete, B. et al. What predicts survival in glioblastoma? A population-based study of changes in clinical management and outcome. Front. Surg. 10, 1249366 (2023).
Al Sharie, S., Abu Laban, D. & Al-Hussaini, M. Decoding diffuse midline gliomas: a comprehensive review of pathogenesis, diagnosis and treatment. Cancers (Basel). 15, 4869 (2023).
Acuña-Villaorduña, A., Baranda, J. C., Boehmer, J., Fashoyin-Aje, L. & Gore, S. D. Equitable access to clinical trials: how do we achieve it? Am. Soc. Clin. Oncol. Educ. B. https://doi.org/10.1200/edbk_389838 (2023).
Lamba, N. et al. Socioeconomic disparities associated with MGMT promoter methylation testing for patients with glioblastoma. JAMA Oncol. 6, 1972–1974 (2020).
Porter, A. B., Wen, P. Y. & Polley, M.-Y. C. Molecular profiling in neuro-oncology: where we are, where we’re heading, and how we ensure everyone can come along. Am. Soc. Clin. Oncol. Educ. B. https://doi.org/10.1200/edbk_389322 (2023).
Xiao, F. et al. Cerebrospinal fluid biomarkers for brain tumor detection: clinical roles and current progress. Am. J. Transl. Res. 12, 1379–1396 (2020).
Villanueva-Meyer, J. E., Mabray, M. C. & Cha, S. Current clinical brain tumor imaging. Neurosurgery 81, 397–415 (2017).
Weinberg, B. et al. Nimg-23. Brain tumor reporting and data system (bt-rads) and quantitative tools to guide its implementation. Neuro. Oncol. 21, vi166 (2019).
Atanasov, A. G. et al. First, do no harm (gone wrong): total-scale analysis of medical errors scientific literature. Front. Public Heal. 8, 558913 (2020).
Aldape, K. et al. Challenges to curing primary brain tumours. Nat. Rev. Clin. Oncol. 16, 509 (2019).
Bi, W. L. et al. Artificial intelligence in cancer imaging: clinical challenges and applications. CA. Cancer J. Clin. 69, 127–157 (2019).
Dong, X. et al. 911 Anti-VEGF therapy improves EGFR-vIII-CAR-T cell delivery and efficacy in syngeneic glioblastoma models in mice. J. Immunother. Cancer 11, e005583 (2022).
Becker, A. P., Sells, B. E., Jaharul Haque, S. & Chakravarti, A. Tumor heterogeneity in glioblastomas: from light microscopy to molecular pathology. Cancers (Basel). 13, 1–25 (2021).
Stone, J. B. & DeAngelis, L. M. Cancer-treatment-induced neurotoxicity-focus on newer treatments. Nat. Rev. Clin. Oncol. 13, 92–105 (2016).
Monsour, R., Dutta, M., Mohamed, A. Z., Borkowski, A. & Viswanadhan, N.A. Neuroimaging in the era of artificial intelligence: current applications. Fed. Pract. 39, S14–S20 (2022).
Philip, A. K., Samuel, B. A., Bhatia, S., Khalifa, S. A. M. & El-Seedi, H. R. Artificial intelligence and precision medicine: a new frontier for the treatment of brain tumors. Life. 13, 24 (2023).
Dundar, T. T. et al. Machine learning-based surgical planning for neurosurgery: artificial intelligent approaches to the cranium. Front. Surg. 9, 863633 (2022).
Mock, M., Edavettal, S., Langmead, C. & Russell, A. AI can help to speed up drug discovery — but only if we give it the right data. Nature 621, 467–470 (2023).
Qureshi, R. et al. AI in drug discovery and its clinical relevance. Heliyon 9, e17575 (2023).
Pati, S. et al. Federated learning enables big data for rare cancer boundary detection. Nat. Commun. 13, 7346 (2022).
Schork, N. J. Artificial intelligence and personalized medicine. Cancer Treat. Res. 178, 265 (2019).
Uddin, M., Wang, Y. & Woodbury-Smith, M. Artificial intelligence for precision medicine in neurodevelopmental disorders. npj Digit. Med. 2, 1–10 (2019).
Hashimoto, D. A., Rosman, G., Rus, D. & Meireles, O. R. Artificial intelligence in surgery: promises and perils. Ann. Surg. 268, 70–76 (2018).
Chen, R. J. et al. Algorithmic fairness in artificial intelligence for medicine and healthcare. Nat. Biomed. Eng. 7, 719–742 (2023).
Thomasian, N. M., Eickhoff, C. & Adashi, E. Y. Advancing health equity with artificial intelligence. J. Public Health Policy 42, 602–611 (2021).
Zheng, Y., Carrillo-Perez, F., Pizurica, M., Heiland, D. H. & Gevaert, O. Spatial cellular architecture predicts prognosis in glioblastoma. Nat. Commun. 14, 4122 (2023).
Wu, J. et al. Radiological tumour classification across imaging modality and histology. Nat. Mach. Intell. 3, 787–798 (2021).
García-Figueiras, R. et al. Proton magnetic resonance spectroscopy in oncology: the fingerprints of cancer? Diagn. Interv. Radiol. 22, 75–89 (2016).
Phillips, H. S. et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 9, 157–173 (2006).
Louis, D. N. et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro. Oncol. 23, 1231–1251 (2021).
Alix-Panabières, C. & Pantel, K. Liquid biopsy: from discovery to clinical application. Cancer Discov. 11, 858–873 (2021).
Yang, H. et al. Cerebrospinal fluid-derived circulating tumor DNA is more comprehensive than plasma in NSCLC patients with leptomeningeal metastases regardless of extracranial evolution. Heliyon 8, e12374 (2022).
Lehner, K. R., Jiang, K., Rincon-Torroella, J., Perera, R. & Bettegowda, C. Cerebrospinal fluid biomarkers in pediatric brain tumors: a systematic review. Neoplasia 35, 100852 (2023).
Liu, H. et al. M3AE: multimodal representation learning for brain tumor segmentation with missing modalities. Proc. AAAI Conf. Artif. Intell. 37, 1657–1665 (2023).
Clark, K. et al. The cancer imaging archive (TCIA): maintaining and operating a public information repository. J. Digit. Imaging 26, 1045–1057 (2013).
Menze, B. H. et al. The multimodal brain tumor image segmentation benchmark (BRATS). IEEE Trans. Med. Imaging 34, 1993–2024 (2015).
Therapeutically applicable research to generate effective treatments (TARGET) - NCI. https://www.cancer.gov/ccg/research/genome-sequencing/target.
Welcome to the cancer imaging archive - the cancer imaging archive (TCIA). https://www.cancerimagingarchive.net/.
Xia, M., Wang, J. & He, Y. BrainNet viewer: a network visualization tool for human brain connectomics. PLoS One 8, e68910 (2013).
Sun, L., Zhang, S., Chen, H. & Luo, L. Brain tumor segmentation and survival prediction using multimodal MRI scans with deep learning. Front. Neurosci. 13, 810 (2019).
Feng, X., Tustison, N. J., Patel, S. H. & Meyer, C. H. Brain tumor segmentation using an ensemble of 3D U-nets and overall survival prediction using radiomic features. Front. Comput. Neurosci. 14, 25 (2020).
ZainEldin, H. et al. Brain tumor detection and classification using deep learning and sine-cosine fitness grey wolf optimization. Bioengineering 10, 1–19 (2023).
Latif, G., Iskandar, D. N. F. A., Alghazo, J. & Butt, M. M. Brain MR image classification for glioma tumor detection using deep convolutional neural network features. Curr. Med. imaging 17, 56–63 (2021).
Saeedi, S., Rezayi, S., Keshavarz, H. & R. Niakan Kalhori, S. MRI-based brain tumor detection using convolutional deep learning methods and chosen machine learning techniques. BMC Med. Inform. Decis. Mak. 23, 16 (2023).
Bhandari, A., Koppen, J. & Agzarian, M. Convolutional neural networks for brain tumour segmentation. Insights Imaging 11, 77 (2020).
Chen, S., Ding, C. & Liu, M. Dual-force convolutional neural networks for accurate brain tumor segmentation. Pattern Recognit. 88, 90–100 (2019).
Isensee, F., Jaeger, P. F., Kohl, S. A. A., Petersen, J. & Maier-Hein, K. H. nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat. Methods 18, 203–211 (2021).
Steyaert, S. et al. Multimodal deep learning to predict prognosis in adult and pediatric brain tumors. Commun. Med. 3, 44 (2023).
Kamnitsas, K. et al. Efficient multi-scale 3D CNN with fully connected CRF for accurate brain lesion segmentation. Med. Image Anal. 36, 61–78 (2017).
Milletari, F., Navab, N. & Ahmadi, S. A. V-Net: fully convolutional neural networks for volumetric medical image segmentation. In: 2016 Fourth International Conference on 3D Vision (3DV), Stanford, CA, USA, 565–571 (2016).
https://www.cancer.org/cancer/types/brain-spinal-cord-tumors-adults/detection-diagnosis-staging/how-diagnosed.html Tests for Brain and Spinal Cord Tumors in Adults.
Nasrallah, M. P. et al. Molecular neuropathology in practice: clinical profiling and integrative analysis of molecular alterations in glioblastoma. Acad. Pathol. 6, 2374289519848353 (2019).
Afridi, M., Jain, A., Aboian, M. & Payabvash, S. Brain tumor imaging: applications of artificial intelligence. Semin. Ultrasound Ct. MR 43, 153–169 (2022).
Ellingson, B. M., Wen, P. Y., Van Den Bent, M. J. & Cloughesy, T. F. Pros and cons of current brain tumor imaging. Neuro. Oncol. 16, vii2 (2014).
Ghandour, F. et al. Presenting psychiatric and neurological symptoms and signs of brain tumors before diagnosis: a systematic review. Brain Sci. 11, 1–20 (2021).
Grant, R. et al. Interventions to reduce the time to diagnosis of brain tumours. Cochrane Database Syst. Rev. 9, CD013564 (2020).
Iijima, K. et al. Microrecording and image-guided stereotactic biopsy of deep-seated brain tumors. J. Neurosurg. 123, 978–988 (2015).
Luo, Q., Li, Y., Luo, L. & Diao, W. Comparisons of the accuracy of radiation diagnostic modalities in brain tumor: a nonrandomized, nonexperimental, cross-sectional trial. Med. 97, e11256 (2018).
Histed, S. N. et al. Review of functional/ anatomic imaging in oncology. Nucl. Med. Commun. 33, 349 (2012).
Riche, M. et al. Complications after frame-based stereotactic brain biopsy: a systematic review. Neurosurg. Rev. 44, 301–307 (2021).
Keane, L., Cheray, M., Blomgren, K. & Joseph, B. Multifaceted microglia - key players in primary brain tumour heterogeneity. Nat. Rev. Neurol. 17, 243–259 (2021).
Martucci, M. et al. Magnetic resonance imaging of primary adult brain tumors: state of the art and future perspectives. Biomedicines 11, 364 (2023).
Zhang, B., Shi, H. & Wang, H. Machine learning and AI in cancer prognosis, prediction, and treatment selection: a critical approach. J. Multidiscip. Healthc. 16, 1779–1791 (2023).
Bauer, A. H., Erly, W., Moser, F. G., Maya, M. & Nael, K. Differentiation of solitary brain metastasis from glioblastoma multiforme: a predictive multiparametric approach using combined MR diffusion and perfusion. Neuroradiology 57, 697–703 (2015).
Voicu, I. P. et al. Differentiating solitary brain metastases from high-grade gliomas with MR: comparing qualitative versus quantitative diagnostic strategies. Radiol. Med. 127, 891–898 (2022).
Kunimatsu, A. et al. Texture analysis in brain tumor MR imaging. Magn. Reson. Med. Sci. 21, 95–109 (2022).
Soni, X. N., Priya, S. & Bathla, X. G. Texture analysis in cerebral gliomas: a review of the literature. AJNR Am. J. Neuroradiol. 40, 928 (2019).
Bharath, K., Kurtek, S., Rao, A. & Baladandayuthapani, V. Radiologic image-based statistical shape analysis of brain tumours. J. R. Stat. Soc. Ser. C. Appl. Stat. 67, 1357–1378 (2018).
Rajan, P. G. & Sundar, C. Brain tumor detection and segmentation by intensity adjustment. J. Med. Syst. 43, 282 (2019).
Kader et al. Brain tumor detection and classification on MR images by a deep wavelet auto-encoder model. Diagnostics 11, 1589 (2021).
Nie, D. et al. Multi-channel 3D deep feature learning for survival time prediction of brain tumor patients using multi-modal neuroimages. Sci. Rep. 9, 1–14 (2019).
Srinivas, C. et al. Deep transfer learning approaches in performance analysis of brain tumor classification using MRI images. J. Healthc. Eng. 2022, 3264367 (2022).
Ali, H. et al. The role of generative adversarial networks in brain MRI: a scoping review. Insights Imaging 13, 98 (2022).
Guo, W. et al. Multiparametric MRI-based radiomics model for predicting H3 K27M mutant status in diffuse midline glioma: a comparative study across different sequences and machine learning techniques. Front. Oncol. 12, 796583 (2022).
Kihira, S. et al. Multiparametric MRI texture analysis in prediction of glioma biomarker status: added value of MR diffusion. Neuro-Oncol. Adv. 3, vdab051 (2021).
Schepke, E. et al. DNA methylation profiling improves routine diagnosis of paediatric central nervous system tumours: a prospective population-based study. Neuropathol. Appl. Neurobiol. 48, e12838 (2022).
Hollon, T. et al. Artificial-intelligence-based molecular classification of diffuse gliomas using rapid, label-free optical imaging. Nat. Med. 29, 828–832 (2023).
Kim, M. et al. Diffusion- and perfusion-weighted MRI radiomics model may predict isocitrate dehydrogenase (IDH) mutation and tumor aggressiveness in diffuse lower grade glioma. Eur. Radiol. 30, 2142–2151 (2020).
Sun, Z. et al. Prediction of IDH mutation status of glioma based on terahertz spectral data. Spectrochim. Acta A Mol. Biomol. Spectrosc. 295, 122629 (2023).
Hajri, R., Nicod-Lalonde, M., Hottinger, A. F., Prior, J. O. & Dunet, V. Prediction of glioma grade and IDH status using 18F-FET PET/CT dynamic and multiparametric texture analysis. Diagnostics 13, 2604 (2023).
Yan, J. et al. Predicting 1p/19q co-deletion status from magnetic resonance imaging using deep learning in adult-type diffuse lower-grade gliomas: a discovery and validation study. Lab. Investig. 102, 154–159 (2022).
Murdaugh, R. L. & Anastas, J. N. Applying single cell multi-omic analyses to understand treatment resistance in pediatric high grade glioma. Front. Pharmacol. 14, 1002296 (2023).
Kool, M. et al. Integrated genomics identifies five medulloblastoma subtypes with distinct genetic profiles, pathway signatures and clinicopathological features. PLoS One 3, e3088 (2008).
Bender, K. et al. High-grade astrocytoma with piloid features (HGAP): the Charité experience with a new central nervous system tumor entity. J. Neurooncol. 153, 109–120 (2021).
Vermeulen, C. et al. Ultra-fast deep-learned CNS tumour classification during surgery. Neuro. Oncol. 622, 842–849 (2023).
Rees, J. H. Diagnosis and treatment in neuro-oncology: an oncological perspective. Br. J. Radiol. 84, S82–S89 (2011).
Mariotto, A. B. et al. Cancer survival: an overview of measures, uses, and interpretation. J. Natl Cancer Inst. Monogr. 2014, 145–186 (2014).
Kickingereder, P. et al. Radiomic profiling of glioblastoma: identifying an imaging predictor of patient survival with improved performance over established clinical and radiologic risk models. Radiology 280, 880–889 (2016).
Prasanna, P., Patel, J., Partovi, S., Madabhushi, A. & Tiwari, P. Radiomic features from the peritumoral brain parenchyma on treatment-naïve multi-parametric MR imaging predict long versus short-term survival in glioblastoma multiforme: preliminary findings. Eur. Radiol. 27, 4198–4199 (2017).
Kickingereder, P. et al. Radiomic subtyping improves disease stratification beyond key molecular, clinical, and standard imaging characteristics in patients with glioblastoma. Neuro. Oncol. 20, 848–857 (2018).
Kim, J. Y. et al. Radiomics in peritumoral non-enhancing regions: fractional anisotropy and cerebral blood volume improve prediction of local progression and overall survival in patients with glioblastoma. Neuroradiology 61, 1261–1272 (2019).
Li, G. et al. An MRI radiomics approach to predict survival and tumour-infiltrating macrophages in gliomas. Brain 145, 1151–1161 (2022).
Iyer, S. et al. Novel MRI deformation-heterogeneity radiomic features are associated with molecular subgroups and overall survival in pediatric medulloblastoma: preliminary findings from a multi-institutional study. Front. Oncol. 12, 915143 (2022).
Long, H. et al. MRI radiomic features of peritumoral edema may predict the recurrence sites of glioblastoma multiforme. Front. Oncol. 12, 1042498 (2023).
Zhou, T. et al. Prediction of brain tumor recurrence location based on multi-modal fusion and nonlinear correlation learning. Comput. Med. Imaging Graph. 106, 102218 (2023).
Śledzińska, P., Bebyn, M. G., Furtak, J., Kowalewski, J. & Lewandowska, M. A. Prognostic and predictive biomarkers in gliomas. Int. J. Mol. Sci. 22, 10373 (2021).
Wang, C., Zhu, X., Hong, J. C. & Zheng, D. Artificial intelligence in radiotherapy treatment planning: present and future. Technol. Cancer Res. Treat. 18, https://doi.org/10.1177/1533033819873922 (2019).
Creasy, J. M. et al. Quantitative imaging features of pretreatment CT predict volumetric response to chemotherapy in patients with colorectal liver metastases. Eur. Radiol. 29, 458–467 (2019).
Kawahara, D., Tang, X., Lee, C. K., Nagata, Y. & Watanabe, Y. Predicting the local response of metastatic brain tumor to gamma knife radiosurgery by radiomics with a machine learning method. Front. Oncol. 10, 569461 (2021).
Wang, Y. et al. The radiomic-clinical model using the SHAP method for assessing the treatment response of whole-brain radiotherapy: a multicentric study. Eur. Radiol. 32, 8737–8747 (2022).
Yang, Y. et al. Spatial heterogeneity of edema region uncovers survival-relevant habitat of Glioblastoma. Eur. J. Radiol. 154, 110423 (2022).
Do, D. T., Yang, M. R., Lam, L. H. T., Le, N. Q. K. & Wu, Y. W. Improving MGMT methylation status prediction of glioblastoma through optimizing radiomics features using genetic algorithm-based machine learning approach. Sci. Rep. 12, 13412 (2022).
Boehm, K. M. & Khosravi, P. Harnessing multimodal data integration to advance precision oncology. 22, 114–126 (2022).
Cè, M. et al. Artificial intelligence in brain tumor imaging: a step toward personalized medicine. Curr. Oncol. 30, 2673–2701 (2023).
Midya, A., Chakraborty, J., Gönen, M., Do, R. K. G. & Simpson, A. L. Influence of CT acquisition and reconstruction parameters on radiomic feature reproducibility. J. Med. Imaging 5, 011020 (2018).
Zwanenburg, A. Radiomics in nuclear medicine: robustness, reproducibility, standardization, and how to avoid data analysis traps and replication crisis. Eur. J. Nucl. Med. Mol. Imaging 46, 2638–2655 (2019).
Lambin, P. et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 14, 749–762 (2017).
Park, J. E. et al. A systematic review reporting quality of radiomics research in neuro-oncology: toward clinical utility and quality improvement using high-dimensional imaging features. BMC Cancer 20, 29 (2020).
Ambe, S. et al. Racial disparities in malignant primary brain tumor survival in Texas from 1995 to 2013. Cureus 12, e11710 (2020)
Butterfield, J. T. et al. Racial disparities in recommendations for surgical resection of primary brain tumours: a registry-based cohort analysis. Lancet 400, 2063–2073 (2022).
Carrano, A., Juarez, J. J., Incontri, D., Ibarra, A. & Cazares, H. G. Sex-specific differences in glioblastoma. Cells 10, 1783 (2021).
Shreve, J. T., Khanani, S. A. & Haddad, T. C. Artificial intelligence in oncology: current capabilities, future opportunities, and ethical considerations. Am. Soc. Clin. Oncol. Educ. B. 42, 1–10 (2022)
Naik, N. et al. Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front. Surg. 9, 862322 (2022).
Amann, J., Blasimme, A., Vayena, E., Frey, D. & Madai, V. I. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med. Inform. Decis. Mak. 20, 310 (2020).
Holzinger, A., Langs, G., Denk, H., Zatloukal, K. & Müller, H. Causability and explainability of artificial intelligence in medicine. Wiley Interdiscip. Rev. Data Min. Knowl. Discov. 9, e1312 (2019).
DeYoe, E. A., Bandettini, P., Neitz, J., Miller, D. & Winans, P. Functional magnetic resonance imaging (FMRI) of the human brain. J. Neurosci. Methods 54, 171–187 (1994).
Assaf, Y. & Pasternak, O. Diffusion tensor imaging (DTI)-based white matter mapping in brain research: a review. J. Mol. Neurosci. 34, 51–61 (2008).
Singh, N. M. et al. Data consistent deep rigid MRI motion correction. https://arxiv.org/abs/2301.10365 (2023).
Chen, Z. et al. Deep learning for image enhancement and correction in magnetic resonance imaging—state-of-the-art and challenges. J. Digit. Imaging 36, 204 (2023).
Han, K. et al. A survey on vision transformer. IEEE Trans. Pattern Anal. Mach. Intell. 45, 87–110 (2022).
Asiri, A. A. et al. Exploring the power of deep learning: fine-tuned vision transformer for accurate and efficient brain tumor detection in MRI scans. Diagnostics 13, 2094 (2023).
Huang, L. et al. A transformer-based generative adversarial network for brain tumor segmentation. Front. Neurosci. 16, 1054948 (2022).
Saueressig, C., Berkley, A., Kang, E., Munbodh, R. & Singh, R. Exploring graph-based neural networks for automatic brain tumor segmentation. Lect. Notes Comput. Sci. 12611, 18–37 (2021).
Ravinder, M. et al. Enhanced brain tumor classification using graph convolutional neural network architecture. Sci. Rep. 13, 1–22 (2023).
Zeineldin, R. A. et al. Explainability of deep neural networks for MRI analysis of brain tumors. Int. J. Comput. Assist. Radiol. Surg. 17, 1673–1683 (2022).
Esmaeili, M., Vettukattil, R., Banitalebi, H., Krogh, N. R. & Geitung, J. T. Explainable artificial intelligence for human-machine interaction in brain tumor localization. J. Pers. Med. 11, 1213 (2021).
Ogier du Terrail, J. et al. Federated learning for predicting histological response to neoadjuvant chemotherapy in triple-negative breast cancer. Nat. Med. 29, 135–146 (2023).
Nasrallah, M. P. et al. Machine learning for cryosection pathology predicts the 2021 WHO classification of glioma. Med 4, 526-540.e4 (2023).
Romano, M. F., Shih, L. C., Paschalidis, I. C., Au, R. & Kolachalama, V. B. Large language models in neurology research and future practice. Neurology 101, 1058–1067 (2023).
Acknowledgements
Research reported in this publication was supported by Emory Radiology-Pathology-Informatics Seed Grant Award Project 00128909, and Project 00131546 (M.A), the National Cancer Institute under award numbers R01CA249992-01A1, R01CA202752-01A1, R01CA208236-01A1, R01CA216579-01A1, R01CA220581-01A1, R01CA257612-01A1, 1U01CA239055-01, 1U01CA248226-01, 1U54CA254566-01, National Heart, Lung and Blood Institute 1R01HL15127701A1, R01HL15807101A1, National Institute of Biomedical Imaging and Bioengineering 1R43EB028736-01, National Center for Research Resources under award number 1 C06 RR12463-01, VA Merit Review Award IBX004121A (A.M) from the United States Department of Veterans Affairs Biomedical Laboratory Research and Development Service the Office of the Assistant Secretary of Defense for Health Affairs, through the Breast Cancer Research Program (W81XWH-19-1-0668), the Prostate Cancer Research Program (W81XWH-15-1-0558, W81XWH-20-1-0851), the Lung Cancer Research Program (W81XWH-18-1-0440, W81XWH-20-1-0595), the Peer-Reviewed Cancer Research Program (W81XWH-18-1-0404, W81XWH-21-1-0345, W81XWH-21-1-0160), the Mayo Clinic Breast Cancer SPORE grant P50 CA116201 from the NIH, the Kidney Precision Medicine Project (KPMP) Glue Grant, and sponsored research agreements from Bristol Myers-Squibb, Boehringer-Ingelheim, Eli-Lilly and AstraZeneca. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the U.S. Department of Veterans Affairs, the Department of Defense, or the United States Government.
Author information
Authors and Affiliations
Contributions
M.A. and A.M. were responsible for the concept proposal and study design. M.A. conceptualized the study, attained funding, provided supervision, prepared the initial draft, and reviewed and revised the final manuscript. S.K. wrote the manuscript with feedback and contributions from all other authors. K.R., Ab.M. and K.B.P. contributed to the data analysis and writing of the manuscript. All authors have revised, read, and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Dr. Abedalthagafi is part of the Editorial Board of this journal. Dr. Madabhushi is an equity holder in Picture Health, Elucid Bioimaging, and Inspirata Inc. Currently, he serves on the advisory board of Picture Health, Aiforia Inc., and SimBioSys. He also currently consults for SimBioSys. He also has sponsored research agreements with AstraZeneca, Boehringer-Ingelheim, Eli-Lilly, and Bristol Myers-Squibb. His technology has been licensed to Picture Health and Elucid Bioimaging. He is also involved in 3 different R01 grants with Inspirata Inc. He also serves as a member of the Frederick National Laboratory Advisory Committee. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Khalighi, S., Reddy, K., Midya, A. et al. Artificial intelligence in neuro-oncology: advances and challenges in brain tumor diagnosis, prognosis, and precision treatment. npj Precis. Onc. 8, 80 (2024). https://doi.org/10.1038/s41698-024-00575-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-024-00575-0