Abstract
Non-human primate studies are unique in translational research, especially in neurosciences where neuroimaging approaches are the preferred methods used for cross-species comparative neurosciences. In this regard, neuroimaging database development and sharing are encouraged to increase the number of subjects available to the community, while limiting the number of animals used in research. Here we present a simultaneous positron emission tomography (PET)/magnetic resonance (MR) dataset of 20 Macaca fascicularis images structured according to the Brain Imaging Data Structure standards. This database contains multiple MR imaging sequences (anatomical, diffusion and perfusion imaging notably), as well as PET perfusion and inflammation imaging using respectively [15O]H2O and [11C]PK11195 radiotracers. We describe the pipeline method to assemble baseline data from various cohorts and qualitatively assess all the data using signal-to-noise and contrast-to-noise ratios as well as the median of intensity and the pseudo-noise-equivalent-count rate (dynamic and at maximum) for PET data. Our study provides a detailed example for quality control integration in preclinical and translational PET/MR studies with the aim of increasing reproducibility. The PREMISE database is stored and available through the PRIME-DE consortium repository.
Similar content being viewed by others
Main
In the framework of open science, sharing imaging databases offers specific benefits in terms of analytical tools development and validation1. According to the FAIR Data Principles, the development of accessible imaging databases will help increase the reproducibility between studies2. In this respect, neuroimaging scientists examine their respective policies and practices3. This is also valid in preclinical research where in vivo imaging of non-human primates (NHPs) holds great potential in comparative biology and biomedical research4,5. NHP neuroimaging databases enable the scaling of findings for cross-species comparative and translational neurosciences and a better understanding of brain regions’ functions in health and disease. Besides, the establishment and sharing of preclinical neuroimaging databases complies with the 3R principles, especially reduction through the use of imaging datasets, and refinement considering that in vivo imaging is non-invasive and favors clinical translation. Therefore, preclinical neuroimaging data sharing associates open science objectives and 3R principles toward better reproducibility and transparency in research6. However, several challenges must be overcome by the NHP neuroscience research community. Historically, single-lab imaging protocols and heavy logistics of research studies have resulted in data acquisition inconsistency and discrepancy of obtained results7. Ultimately, this limitation may compromise appropriate data comparison between research groups. The NHP research community is currently facing a substantial challenge due to the scarcity of animals. The worldwide sanitary crisis caused by severe acute respiratory syndrome coronavirus 2 has severely impacted the already precarious supply chain for these animals, and the drastic price increase for experimental NHP might strongly impact biomedical research8,9.
In recent years, the NHP research community has moved forward to tackle challenges ahead, most notably the limited availability of data. The PRIMatE Data Exchange (PRIMatE-DE) initiative addresses this challenge by aggregating independently acquired NHP in vivo imaging datasets10. Initially intended for magnetic resonance imaging (MRI) data, the community has worked to standardize data collection with minimal acquisition specifications, and data architecture allowing data sharing within the framework of open science10. This collaborative work allowed us to gradually improve our neuroimaging studies to human standards. In this context, the Brain Imaging Data Structure (BIDS) became the gold standard for organizing and sharing neuroimaging datasets1. Nuclear imaging specialists jumped on board and published guidelines to improve the accuracy and sharing of positron emission tomography (PET) data11,12,13. Therefore, while PET neuroimaging databases exist, their counterparts in NHP are either missing or not easily available. Furthermore, considering the development of hybrid PET/magnetic resonance (MR) scanners and their translational potential in NHP neuroimaging studies, there is a growing need for NHP PET/MR hybrid imaging databases.
In this Article, we developed a multi-modal database of Macaca fascicularis, acquired on a clinical PET/MR scanner, and constructed with MRI, [15O]H2O and [11C]PK11195 PET images. [15O]H2O is a freely diffusible PET tracer used to measure brain perfusion and considered as a reference for non-invasive cerebral blood flow quantification14. [11C]PK11195 is a PET radiotracer specifically targeting the translocator protein 18 kDa (TSPO) and is widely used to investigate brain inflammation in relation to various neurological disorders and notably brain ischemia15,16. The data were formatted to BIDS standards using a self-designed Python script compensating for missing metadata frequently encountered with preclinical and retrospective data. The designed script is available in open access on GitLab. The entire dataset is available upon request from the PRIMatE-DE repository.
Results
The collection of participants’ information enabled a detailed description of the cohort’s age (6 ± 0.65 years) and weight (7.37 ± 1.11 kg). A summary of the age and weight distribution is provided in Table 1. After converting the data to BIDS standards, the sequences’ availability was assessed using an automated counter. The data availability is provided in Fig. 1. This analysis highlighted the presence of a test–retest for two subjects in the dataset and a few missing acquisitions. The lack of data is explained by issues with radiosynthesis, contrasting agents or movement during acquisition for PET, contrast imaging and MRI sequences, respectively. This figure also indicates the study year for each subject, ranging from 2016 to 2019. This parameter is relevant to explain variability in data quality due to software updates on the PET–MRI system.
The quality of the acquisitions in the shared BIDS database is expressed with signal-to-noise ratio (SNR), contrast-to-noise ratio (CNR) and median of intensity. The quality assessment highlighted the consistency of the acquisition quality (averaged and over time) as displayed in Fig. 2.
Quality is expressed in SNR, CNR, median of intensity and maximum of PNECR distributions across subjects and sequences. Anat, anatomical sequences; DWI, diffusion-weighted imaging; FA, flip angle; FLAIR, fluid-attenuated inversion recovery; Perf, perfusion sequences; PET, positron emission tomography; T1map, T1 mapping; T1w, T2w, T2starw, relaxation weighted; TOF, time of flight.
While acquisition quality was highly reproducible, an outlier in T2-weighted and T2*-weighted sequences was identified. This outlier is due to a variation in acquisition parameters during session 2 of subject 4 as shown in Table 2. The dynamic contrast-enhanced (DCE)-perfusion acquisitions also uncovered an outlier due to the movement of subject 15 during acquisition.
Two groups can be discriminated in the diffusion-weighted imaging (DWI) metrics evaluation. This distinction is due to a software update in 2019 after which the sequence’s parameters were strongly modified for this acquisition. As a result of the software update, the median intensity is considerably reduced. A variation in SNR and CNR can also be observed, but with a milder difference between software versions.
A variability in the PET signal intensity can be observed for both tracers. The maximum of pseudo-noise-equivalent count rate (PNECR) metric shows a difference between 2016 acquisitions and later campaigns. These early data show a lower maximum of PNECR with [15O]H2O tracer and a wider variability across subjects with [11C]PK11195 tracer. Figure 3 shows the evolution of PNECR over time for both tracers expressed on a logarithmic scale. This representation highlights the variability in tracer injection time for acquisitions before 2017.
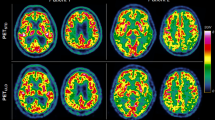
While we uncovered acquisition parameters variations throughout acquisition years, the dataset protocol used did not vary. Figure 4 shows the simultaneous acquisitions of MRI sequences and PET scans.
DCE, dynamic contrast enhanced; DSC, dynamic susceptibility contrast; DWI, diffusion weighted imaging; FA, flip angle; FLAIR, fluid attenuated inversion recovery; MRI, magnetic resonance imaging; PET, positron emission tomography; T1map, T1 mapping; T1w, T2w, T2starw, relaxation weighted; TOF, time of flight.
Discussion
In line with human neuroimaging advances, the NHP scientific community is evolving toward more reproducibility and transparency in biomedical sciences, notably through the means of data sharing. To the best of our knowledge, this NHP imaging database is the first open-source collection including simultaneous dynamic PET-acquisition and MRI sequences. We provide a wide range of NHP MRI acquisitions for download, including structural, diffusion and perfusion imaging.
BIDS standards were originally designed to guide best practices for the storage and sharing of fMRI datasets1. PET imaging modalities came afterwards as extensions to the original BIDS specifications12. In this context, Drs. Gitte Knudsen and Robert Innis initiated a collaborative working program to address specific PET imaging challenges through the definition of standards for organizing and sharing11. We followed the current recommendations regarding the description of data acquisition and reconstruction methods as well as the molecular description of the radiotracers.
The purpose of the present brain NHP database is to provide the molecular imaging community with a full dataset with detailed quality descriptions. We included quality control measures of PET images using the median intensity metric. Although the methods we propose here are derived from MRI applications, we believe that they can be used to quantify the variability of the different PET data acquisitions. This variability is due to the injected radioactivity, subject’s weight and physiological constants’ variations. While corrections can be applied to normalize weight and dose variations using standardized uptake value quantification, variability of physiological constants can be compensated using reference region ratios (standardized uptake value ratios). We provided uncorrected data enabling future users to apply their own normalization and modeling methods. We assessed the variability of our PET data using the PNECRmax, which showed a high reproducibility for [15O]H2O tracer given the highly standardized injected dose; however, the data show a variability in the timing of injection for the scans acquired in 2016. The variability in PNECRmax is slightly higher for [11C]PK11195 radiotracer, due to a larger range of injected dose. However, [15O]H2O data displayed more noise compared with [11C]PK11195 data due to the shorter frame duration and the extremely short half-life of [15O]. We analyzed the dynamic evolution of PNECR, which was stable over time and between animals, except for early frames corresponding to the bolus entry into the brain. As expected the counting rate is almost ten times higher for the [11C]PK11195 than for the [15O]H2O.
We are aware of the quality limitations of the MRI data in comparison with the standards in NHP imaging17. These drawbacks are largely due to the specifics of our research protocol dedicated to translational stroke research. Therefore, baseline acquisitions (before stroke induction) were acquired in the same conditions as further occlusion–reperfusion acquisitions18,19, which precludes the use of a stereotaxic frame for a repeatable animal position in the scanner. Moreover, due to the specificity of our model, acquisitions had to be shortened to fit experimental conditions in stroke phases. While we observed variability in our data quality that might alter the automation of pipelines, the diversity of our database can represent a source of interest for a wide range of applications from noise reduction to anatomical studies. Furthermore, simultaneous acquisitions enable modality comparison; for instance our database provides perfusion imaging with MRI (dynamic susceptibility contrast, DSC) and PET ([15O]H2O) for potential cross-comparative studies of the resulting parameters.
When formatting a retrospective and/or preclinical database to BIDS standards, we frequently encounter missing data and missing Digital Imaging and Communications in Medicine (DICOM) tags. These inconsistencies are difficult to identify and compensate. Therefore, we found a need for a self-designed tool to format data following BIDS guidelines. Additionally, this tool enables the selection of specific setting/experimental phase to include in the converted database. We think this functionality could encourage scientists to share parts of their data while holding the remaining settings until results are published. The tool also supports a variety of raw data folder organization, as we know it varies between structures and institutes. A common issue faced in data formatting and sharing is the time and resources these initiatives require. This issue highlights the need for data scientists dedicated to these tasks in research teams. We are hoping that the provided tool will facilitate such initiatives that are urgently needed to address challenges raised by the use of NHP in biomedical research.
To conclude, we generated an original and diverse NHP hybrid PET/MR database available for the community through PRIME-DE platform and hope that the present work, describing the quality of the published data and metadata, will encourage the neuroimaging community to use it.
Methods
Animal cohort description
This dataset, which includes 20 mature male cynomolgus macaques (M. fascicularis), was generated using baseline images from the primate stroke model described by Debatisse et al. and Becker et al. in 2021 and 2023, respectively16,18. The experimental protocol was approved by the Animal Welfare Body of Cynbiose and the Ethics Committees of VetAgro-Sup and CELYNE CEEA n°42 and was carried out in accordance with the European Directive 2010/63/UE and ARRIVE guidelines (Animal Research: Reporting in Vivo Experiments)20,21.
The subjects underwent combined PET–MRI acquisitions following anesthesia induced by intramuscular injection of ketamine (4 mg/kg; KetamineVR 1000, Virbac) and midazolam (1.3 mg/kg; MidazolamVR 5 mg/ml, Mylan). Sevoflurane (1%, variable depending on the animal’s anesthetic depth; SevoFloVR, Abbott Laboratories) maintained anesthesia during acquisition. Animals were intubated and monitored through heart and respiratory rate, end-tidal CO2, systolic, diastolic and mean arterial pressure, oxygen saturation and body temperature.
PET–MRI acquisitions
PET–MRI sequences were acquired on a fully integrated hybrid Biograph mMR PET-MRI 3T Siemens scanner (Siemens Healthcare). Imaging acquisitions were conducted between 2016 and 2019 with software versions ‘syngo MR B20P’ and ‘syngo MR E11’.
MRI sequences are previously described in Results with corresponding parameters according to years of acquisition (Table 2).
Images from PET radiotracers [15O]H2O (255 ± 15 MBq) and [11C]PK11195 (140.1 ± 21.4 MBq) were acquired for 6 min and 70 min, respectively, after bolus injections. While molar activity could be measured for [11C]PK11195 (48.0 ± 24.5 GBq/μmol) providing information on injected mass (3.50 ± 1.7 nmol), the half-life of [15O]H2O did not permit such precise radioactivity measurements. The data were reconstructed on a 256 × 256 × 127 matrix (voxel size 0.7 × 0.7 × 2.0 mm3), 26 cm axial field of view using a point-spread function and ordinary poisson ordered subset expectation maximization (OP-OSEM) iterative reconstruction method including normalization as well as correction for attenuation, scatter, random counts and dead time. Before the PET–MRI session, a computed tomography scan (Siemens Biograph mCT64, Siemens Healthcare) was obtained for each animal and used for PET attenuation correction. [11C]PK11195 dynamic PET data were reconstructed in 28 frames: 6 × 10 s, 6 × 20 s, 6 × 120s and 8 × 300s. [15O]H2O dynamic PET were reconstructed in 26 frames: 8 × 4 s, 4 × 6 s, 6 × 10 s and 8 × 20s. Lastly, a post-reconstruction 3D Gaussian filter of 4 mm was applied.
Data processing
The data processing pipeline consisted in formatting datasets to BIDS1. Existing formatting tools such as dcm2bids22 have limited support for missing DICOM tags frequently encountered in preclinical and retrospective datasets. Therefore, an automated Python script compatible with MRI and PET acquisitions was developed. Raw images are loaded in DICOM format and converted to NIfTI format with associated metadata in JSON format in accordance with BIDS guidelines. An overview of the Python script tasks is provided in Supplementary Fig. 1. The script’s ambition is to provide flexibility in data organization and selection when formatting raw data for sharing purposes. Because raw-data folder organization varies between structures, additional parameters are provided enabling the definition of the raw folder structure. For instance, single-session and multiple-session studies are supported by the pipeline. It is also possible to select which acquisitions and sessions to format to BIDS. This option may be useful in multi-phase studies in which data exploration of key phases delays data sharing of baseline acquisitions. Additionally to the data conversion, the script provides templates for mandatory BIDS files such as dataset description and participants list.
Converting pixel data to NIfTI image
DICOM volume loading and conversion to NIfTI format is performed using the pydicom and nibabel Python packages23,24. These packages were integrated in a Python class handling multi-dimensional volumes from lists of DICOM files enabling the building of pixel data arrays and managing data orientation to improve NIfTI encoding. Limitations remain for oblique orientations, frequently encountered in large animal models; special care should be provided when handling NIfTI conversions, and manual corrections might be necessary. Therefore, the orientation of the pixel data was manually validated using the ITK-snap software25. The provided data were acquired on a clinical PET–MRI system without a stereotaxic frame; therefore, a unique subject position was established close to a patient position. All images are shared in raw space; no registration to standard atlas space was applied. The oblique encoding of MRI sequences led to potential errors in conversions. The closest orientation was right–superior–anterior for the majority of subjects. Other subjects were oriented oblique closest to right–anterior–inferior. To provide uniform data, the identified right–anterior–inferior subject’s data were manually oriented to right–superior–anterior. To match PRIME-DE orientation homogeneity criteria, the full dataset was then oriented to right–posterior–inferior. Additionally, DWI and diffusion tensor imaging require bval and bvec files to qualify the sequences. These files are obtained with the dicom2nifti Python package26.
Generating the metadata file
To collect the necessary metadata for each acquisition sequence, compensate missing tags and integrate subject-specific radioactivity parameters, three configuration files are necessary.
Sequence overview
The sequence overview configuration file provides a list of sequences to integrate in the BIDS formatting. It provides details on tags necessary for each sequence and replacement values if the tag is missing in the DICOM metadata. In this configuration file, the naming format for the sequence in the BIDS database is also defined along with instructions on where to find and store the corresponding data. Supplementary Table 1 provides a description of each column required in the sequence overview configuration file along with examples.
PET doses
The PET-specific configuration file enables the definition of each subject’s injected radioactivity parameters. The file sets values for BIDS-guideline required PET tags SpecificRadioactivity (that is, molar activity, the current term recommended by the guidelines27), InjectedRadioactivity and InjectedMass. This file is required only for PET data formatting. Configuration file description and examples are provided in Supplementary Table 2.
DICOM to BIDS tag converter
This configuration file provides the DICOM tag name for each required BIDS tag compensating for variable naming conventions between the two formats. If no DICOM tag equivalent exists for a given BIDS requirement, the sequence overview or PET-doses replacement option is triggered. Description and examples of the configuration file are given in Supplementary Table 3.
Data quality assessment
To provide an indication of the quality of the database formatted to BIDS standards, we analyzed the distribution of three relevant metrics: SNR and CNR for MRI acquisitions, and median intensity for PET and MRI acquisitions. The metrics were measured on voxels with tissue signal (volume of interest, VOI) following Otsu thresholding on the volume with the highest intensity28. Voxels below the given threshold were considered background for noise measurement. The metrics were calculated using the following formulas:
Categorical violin plots were plotted for each metric. These plots show the distribution of the metric values across subjects. Strip plots were superimposed on the violin plots to provide additional information on time distributions. In these plots, each category corresponds to an MRI sequence or PET tracer, and the points represent the metric values for each acquisition within that sequence. For dynamic MRI sequences and PET acquisitions, we averaged the metrics across time points or frames and plotted the resulting values. For multi-echo sequences, we averaged the median of intensity across echo times and plotted the resulting values. In terms of noise evaluation, only the first echo was plotted as the SNR is maximal at this echo time. Additionally, we provided a specific PET metric based on counting statistics before reconstruction, enabling the calculation of the PNECR (PNECR = (P − D)2/P, with P total prompts and D total randoms)29. The maximum of PNECR was represented following the representation methods of the previously described metrics. The dynamic evolution of PNECR over time was represented on a logarithmic scale to uncover variations in tracer injection times. Lastly, a sample of the data was manually inspected to ensure that the results were accurate and to identify any issues that might have been missed. Based on these evaluations, we were able to provide an indication of the overall quality of the database for potential future users of the dataset, including the detection of potential outliers and the assessment of the homogeneity and consistency of the data.
Execution protocol
Detailed protocol steps to execute the formatting script are provided on protocol.io30.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The dataset supporting the results of this article is available in the PRIME-DE repository, with identifier ‘pending identifier’ and licensed under Data Usage Agreement (https://fcon_1000.projects.nitrc.org/indi/PRIME/carmen-lyon.html).
Code availability
The code is hosted in a Public GitLab repository under the name cermep-bids-retro (https://gitlab.in2p3.fr/cermep/cermep-bids-retro). It is fully implemented in the Python programming language and is operating system independent. The Python environment requirements are provided in the environment.yml file. The code is licensed under MIT.
References
Gorgolewski, K. J. et al. The brain imaging data structure, a format for organizing and describing outputs of neuroimaging experiments. Sci. Data 3, 160044 (2016).
Wilkinson, M. D. et al. The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data 3, 160018 (2016).
Poldrack, R. A. et al. Scanning the horizon: towards transparent and reproducible neuroimaging research. Nat. Rev. Neurosci. 18, 115–126 (2017).
Friedrich, P. et al. Imaging evolution of the primate brain: the next frontier? NeuroImage 228, 117685 (2021).
Phillips, K. A. et al. Why primate models matter. Am. J. Primatol. 76, 801–827 (2014).
Aske, K. C. & Waugh, C. A. Expanding the 3R principles. EMBO Rep. 18, 1490–1492 (2017).
Milham, M. et al. Accelerating the evolution of nonhuman primate neuroimaging. Neuron 105, 600–603 (2020).
Subbaraman, N. The US is boosting funding for research monkeys in the wake of COVID. Nature 595, 633–634 (2021).
O’Grady, C. Airline’s decision to end monkey transports will worsen shortage in research. Science https://doi.org/10.1126/science.add8083 (2022).
Milham, M. P. et al. An open resource for non-human primate imaging. Neuron 100, 61–74.e2 (2018).
Knudsen, G. M. et al. Guidelines for the content and format of PET brain data in publications and archives: a consensus paper. J. Cereb. Blood Flow Metab. 40, 1576–1585 (2020).
Norgaard, M. et al. PET-BIDS, an extension to the brain imaging data structure for positron emission tomography. Sci. Data 9, 65 (2022).
Mérida, I. et al. CERMEP-IDB-MRXFDG: a database of 37 normal adult human brain [18F]FDG PET, T1 and FLAIR MRI, and CT images available for research. EJNMMI Res. 11, 91 (2021).
Wintermark, M. et al. Comparative overview of brain perfusion imaging techniques. Stroke 36, e83–e99 (2005).
Chauveau, F., Becker, G. & Boutin, H. Have (R)-[11C]PK11195 challengers fulfilled the promise? A scoping review of clinical TSPO PET studies. Eur. J. Nucl. Med. Mol. Imaging 49, 201–220 (2021).
Becker, G. et al. Spatio-temporal characterization of brain inflammation in a non-human primate stroke model mimicking endovascular thrombectomy. Neurotherapeutics 20, 789–802 (2023).
Autio, J. A. et al. Minimal specifications for non-human primate MRI: challenges in standardizing and harmonizing data collection. NeuroImage 236, 118082 (2021).
Debatisse, J. et al. A non-human primate model of stroke reproducing endovascular thrombectomy and allowing long-term imaging and neurological read-outs. J. Cereb. Blood Flow Metab. 41, 745–760 (2021).
Debatisse, J. et al. PET-MRI nanoparticles imaging of blood–brain barrier damage and modulation after stroke reperfusion. Brain Commun. 2, fcaa193 (2020).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 8, e1000412 (2010).
Percie du Sert, N. et al. The ARRIVE guidelines 2.0: updated guidelines for reporting animal research. PLoS Biol. 18, e3000410 (2020).
Bedetti, C. et al. UNFmontreal/Dcm2Bids: 2.1.8. Zenodo https://doi.org/10.5281/zenodo.6658099 (2022)
Mason, D. et al. pydicom/pydicom: pydicom 2.3.1. Zenodo https://doi.org/10.5281/zenodo.7319790 (2022)
Brett, M. et al. nipy/nibabel:. Zenodo https://doi.org/10.5281/zenodo.6658382 (2022).
Yushkevich, P. A., Gao, Y. & Gerig, G. ITK-SNAP: an interactive tool for semi-automatic segmentation of multi-modality biomedical images. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2016, 3342–3345 (2016).
icometrix/dicom2nifti. GitHub https://github.com/icometrix/dicom2nifti (2022).
Luurtsema, G. et al. EANM guideline for harmonisation on molar activity or specific activity of radiopharmaceuticals: impact on safety and imaging quality. EJNMMI Radiopharm. Chem. 6, 34 (2021).
Otsu, N. A threshold selection method from Gray-level histograms. IEEE Trans. Syst. Man Cybern. 9, 62–66 (1979).
Watson, C. C. et al. Evaluation of clinical PET count rate performance. IEEE Trans. Nucl. Sci. 50, 1379–1385 (2003).
cermep-bids-retro V.1. protocols.io https://www.protocols.io/view/cermep-bids-retro-261ge319dl47/v1 (2023).
Acknowledgements
This work was supported by ANR CYCLOPS and CMRO2 (ANR-15-CE17-0020 and ANR-21-CE17-0028), the RHU MARVELOUS (ANR-16-RHUS-0009) of Lyon University, under the Investissements d’Avenir program of the French National Research Agency (ANR). The PET–MRI acquisitions were carried out thanks to the Equipex LILI funding (LILI—Lyon Integrated Life Imaging: hybrid MR-PET ANR-11-EQPX-0026). The PhD salary of L.C. (Cifre, OLEA Medical) is co-funded by the French Ministry of Higher Education and Research (ANRT). G.B. is supported by Labex PRIMES (ANR-11-LABX-0063). The authors would like to express their sincere gratitude to Cynbiose SAS scientific leadership, J. Confais and H. Contamin for their invaluable scientific advices. We acknowledge the IRIS team, the RHU MARVELOUS and its Scientific Advisory Board for their fruitful discussions.
Author information
Authors and Affiliations
Contributions
L.C. conducted the data curation, formal analysis and methodology, provided code resources, software, validation and visualization and wrote the original draft, reviews and editions. J.D. and O.W. conducted the investigation and project administration, and provided resources, formal analysis and reviews. T.B. supervised the software development and draft redaction. M.W. acquired funding and provided supervision, project administration, reviews and editions. N.C. and I.M. conducted the data acquisition and provided resources, methodology, formal analysis, validation, reviews and edition. J.R. provided reviews and editions. J.-B.L., S.L. and C.L. conducted the investigation, and provided methodology, project administration and resources. T.-H.C., O.F.E. and N.N. acquired funding and conducted the investigation and project administration. L.M. acquired funding and conducted the investigation and project administration, and supervised writing—review and editing. E.C.-S. conceptualized the project, acquired funding and conducted the investigation and project administration, and supervised writing—review and editing. G.B. conceptualized the project, supervised the methodology, wrote the original draft, reviews and editions.
Corresponding authors
Ethics declarations
Competing interests
L.C. is employee of Olea Medical. O.W. is employee of Cynbiose SAS. The other authors declare no competing interests.
Peer review
Peer review information
Lab Animal thanks Doris Doudet and the other, anonymous, reviewer(s) for their contribution to the peer review of this work
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Fig. 1 and Tables 1–3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chalet, L., Debatisse, J., Wateau, O. et al. The PREMISE database of 20 Macaca fascicularis PET/MRI brain images available for research. Lab Anim 53, 13–17 (2024). https://doi.org/10.1038/s41684-023-01289-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41684-023-01289-9