Abstract
Lumbar spinal alignment is crucial for spine biomechanics and is linked to various spinal pathologies. However, limited research has explored gender-specific differences using CT scans. The objective was to evaluate and compare lumbar spinal alignment between standing and sitting CT in healthy individuals, focusing on gender differences. 24 young and 25 elderly males (M) and females (F) underwent standing and sitting CT scans to assess lumbar spinal alignment. Parameters measured and compared between genders included lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), pelvic incidence (PI), lordotic angle (LA), foraminal height (FH), and bony boundary area (BBA). Females showed significantly larger changes in SS and PT when transitioning from standing to sitting (p = .044, p = .038). A notable gender difference was also observed in the L4-S LA among the elderly, with females showing a significantly larger decrease in lordotic angle compared to males (− 14.1° vs. − 9.2°, p = .039*). Females consistently exhibited larger FH and BBA values, particularly in lower lumbar segments, which was more prominent in the elderly group (M vs. F: L4/5 BBA 80.1 mm2 [46.3, 97.8] vs. 109.7 mm2 [74.4, 121.3], p = .019 in sitting). These findings underline distinct gender-related variations in lumbar alignment and flexibility, with a focus on noteworthy changes in BBA and FH in females. Gender differences in lumbar spinal alignment were evident, with females displaying greater pelvic and sacral mobility. Considering gender-specific characteristics is crucial for assessing spinal alignment and understanding spinal pathologies. These findings contribute to our understanding of lumbar spinal alignment and have implications for gender-specific spinal conditions and treatments.
Similar content being viewed by others

Introduction
In recent years, the dynamics of spinal alignment have received significant attention in medical research. One aspect that has proven crucial in these studies is the analysis of spinal changes under various loads. Traditionally, image analyses under load have been conducted through standing MRI and loaded CT. However, several factors, such as narrow FOV, long imaging time, and low resolution, have made the use of standing MRI problematic for morphological evaluation1. On the other hand, loaded CT, while able to replicate pseudo standing load in a supine position, lacks physiological accuracy due to the differences from natural standing in terms of gravity direction and muscle activity2.
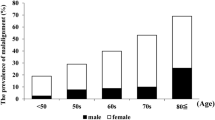
While X-rays or EOS have been extensively used in reporting and evaluations made in positions like standing and sitting, the field lacks evaluations using loaded CT3,4,5,6,7,8,9. Furthermore, while differences in alignment and postural changes according to gender and age have been previously reported, there has been a glaring absence of detailed evaluation using CT4,7,8.
Through CT evaluation, researchers can assess the intervertebral foramina and the facet joints unlike with X-rays. There is also evidence to suggest that lumbar degenerative spondylolisthesis is more common in female, particularly at L4/5 levels, indicating the existence of diseases where the pathology varies between men and female10.
Recognizing these gaps, this study aims to leverage upright CT to evaluate spinal alignment and lumbar components under physiological load during standing and sitting among healthy volunteers. Our goal was to delineate the postural changes between men and female in detail, shedding new light on spinal mobility and its implications in medical diagnostics and treatment plans.
Materials and methods
Study design
This is a cross-sectional study. Images were captured in the standing and relaxed sitting positions using upright CT. The subjects comprised 24 young healthy volunteers (aged 21–40, mean age 30.3 ± 5.7 years, 13 males, 11 females) and 25 elderly individuals (aged 61–79, mean age 65.7 ± 3.8 years, 12 males, 13 females). The criteria for being considered healthy included not having back pain, not smoking, having a body mass index (BMI) between 18.5 and 25 kg/m2, no history of spinal surgery, and not being pregnant or potentially pregnant.
Image acquisition
All subjects were imaged in the standing and relaxed sitting positions using upright CT. For the standing posture, images were taken without leaning on the back rod installed in the upright CT, standing as much as to avoid swaying. For the relaxed sitting position, a plate was set up within the upright CT to allow subjects to sit, with hip and knee joints at 90 degrees, and without using a backrest. Uniformity of posture was managed by an orthopedic doctor and a radiologist present during the imaging process. Before the imaging session, the orthopedic doctor and radiologist demonstrated the required postures to the participants, ensuring they understood exactly how to position their bodies. Both professionals were present to visually inspect and adjust the participants' postures before each imaging session commenced. This direct supervision ensured that the subjects' hip and knee joints were at the correct 90° angle for sitting positions and that their standing posture was as required for the study. The orthopedic doctor and radiologist provided clear, verbal instructions to participants on how to assume the required postures. They also assisted participants in achieving these postures when necessary, making minor adjustments to ensure accuracy. Throughout the imaging process, these specialists performed consistency checks across all participants to ensure that the posture maintained met the study's strict guidelines. Upright CT (prototype TSX-401R, Canon Medical Systems) images were acquired under the same conditions: tube current, 10–350 mA (using noise index 24 for slice thickness 5 mm); rotation speed, 0.5 s; and slice thickness, 0.5 mm. Images were reconstructed using Adaptive Iterative Dose Reduction 3D (Canon Medical Systems, Ohtawara, Japan) to reduce radiation dose11,12.
The scan range included the outer ear canal to the femoral head, including the femur. The total average effective dose of upright CT (standing + sitting CT) in this study was about 8 mSv.
The present study was approved by the Ethics Committee of Keio University School of Medicine. It was conducted in accordance with the Helsinki Declaration and all prescribed protocols. Moreover, an informed consent was obtained from all participants.
Radiographic measurements
All data were analyzed using commercial software (Zed View 14.0.0; LEXI Co., Ltd.). CT images were reconstructed in MPR, and spine-pelvis parameters were measured using the projected data. Lumbar lordosis (LL), sacral slope (SS), pelvic tilt (PT), pelvic incidence (PI), and intervertebral angles were measured13. IVA was defined as the angle in the sagittal plane between the lower endplate of the upper vertebral body and the upper endplate of the lower vertebral body, with forward bending being positive and backward bending negative, in relation to the axis passing through the center of the femoral head. The lordotic angle of the lumbar spine, also referred to as the L1-S to L5-S segment angle, is defined as the angle formed between the superior endplate of the first sacral vertebra (S1) and the inferior endplate of the first to fifth lumbar vertebra (L1-5). In particular, L4-S is a measure of lordosis, present in the lower section of the lumbar spine at the junction where the spine meets the sacrum. It is an important parameter for assessing the biomechanical alignment of the spine and can have implications for posture.
Morphological evaluation of the intervertebral foramen was performed by measuring the foraminal height (FH), and bony boundary area (BBA). These measurements were taken on both sides of the intervertebral foramen in the standing and sitting positions and the average or the average difference for each side was calculated.
FH
FH is defined as the maximum distance between the lower edge of the superior pedicle and the upper edge of the inferior pedicle in the sagittal plane, we pointed out the bottom center and top center of the pedicle and measured the distance (Fig. 1A)14.
Representative image of foraminal height and bone boundary area. (A) Representative Axial View of L4/L5 Foramen. The solid line shows the foraminal height (FH). FH is defined as the maximum distance between the lower edge of the superior pedicle and the upper edge of the inferior pedicle. (B) 3D Reconstruction of L4/L5 Foramen. Dotted circle indicates the bone boundary area (BBA) of the foramen. BBA is defined as the area enclosed by the posterior edge of the vertebral body, the lower edge of the superior pedicle, the anterior edge of the inferior articular process, the anterior edge of the superior articular process, and the upper edge of the inferior pedicle.
BBA
BBA is defined as the area enclosed by the posterior edge of the vertebral body, the lower edge of the superior pedicle, the anterior edge of the inferior articular process, the anterior edge of the superior articular process, and the upper edge of the inferior pedicle. Due to rotation of the vertebral body altering the positions of the anterior and posterior edges when defined in the sagittal plane, we instead assessed the area on the plane formed by the axis of the FH and the axis of the inferior pedicle. We referred to a 3D model created by Zed View and adjusted the area enclosed by the bone to define the BBA (Fig. 1B)15.
Intraclass correlation coefficient values for various spinal parameters and measurements
The intraclass correlation coefficient (ICC) of the intra- and inter-observer reliabilities of measurements obtained from CT images of 10 randomly selected patients were calculated. We classified the ICC values according to the criteria introduced by Aubin et al.; < 0.24, 0.25–0.49, 0.50–0.69, 0.70–0.89, and 0.90–1.0 were considered to be poor, low, fair to moderate, good, good to excellent, respectively. Two board certified orthopedic surgeons independently measured all radiograph parameters. One examiner measured once and the other examiner measured twice a week apart after brief lecture for standardize the measurement. Examiners were blinded to patient clinical information and other measurement.
Statistical analysis
All statistical analyses were performed using R Version 4.2.1. Radiographic measurement data were expressed as median (1st–3rd quartile in parentheses). The level of significance was set at p < 0.05. Differences in posture within the same individual were tested using the Wilcoxon signed-rank test, and differences in posture between ages and sexes were tested using the Mann–Whitney U test.
Results
Reliability assessment of spinal measurements via CT
The intra-observer ICC values for spinal measurements ranged from 0.855 to 0.996, showcasing excellent consistency. Similarly, the inter-observer ICC values exhibited excellent reliability, falling within a range of 0.87–0.98. The parameters FH and BBA also demonstrated good reliability, with intra-observer ICC values of 0.855 and 0.982, and inter-observer ICC values of 0.805 and 0.938, respectively (Supplemental Table 1). These findings highlight the high reproducibility of spinal measurements conducted using CT.
Summary of the patient cohort
Table 1 shows the background of the subjects. The average LL was 42.2°, SS averaged at 31.1°, PT averaged at 14.4°, and the average PI was 43.6°.
Comparisons of the change of regional lumbar spinal parameters by posture between male and female subjects
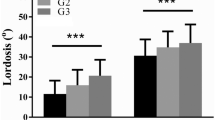
The representative CT images were shown in Figs. 2 and 3. Females had a significantly larger LL than males during standing (46.6° vs. 40.4°, p = 0.03, Table 2). However, when transitioning to sitting, females exhibited a larger reduction rate in LL compared to males, though not statistically significant (− 91.4% vs. − 80.2%, p = 0.052, Table 2). Additionally, while there was a significant decrease in the reduction rate for elderly males, elderly females retained a similar reduction rate in LL compared to young females (− 90.9% vs. − 53.0% for males and − 95.8% vs. − 84.0% for females, p = 0.01, 0.29). (Supplemental Table 2).
Representative cases of the change of spinal alignment by posture in the young subjects. (A) The standing whole spine CT of 32-year-old male. (B) The sitting whole spine CT of 32-year-old male. (C) The standing whole spine CT of 38-year-old female. (D) The sitting whole spine CT of 38-year-old female. A significant spinal alignment change was observed in a female patient when transitioning to a sitting position.
representative cases of the change of spinal alignment by posture in the elderly subjects. (A) The standing whole spine CT of 74-year-old male. (B) The sitting whole spine CT of 74-year-old male. (C) The standing whole spine CT of 72-year-old female. (D) The sitting whole spine CT of 72-year-old female. A significant spinal alignment change was observed in a female patient when transitioning to a sitting position.
For SS, the study found significantly larger delta values in females compared to males among both the overall participant group and the elderly subset. Specifically, the difference was − 23.9° in young males versus − 30.4° in females, and − 10.1° in elderly males versus − 24.8° in elderly females, and − 15.2° in males versus − 26.4° in females for the overall group, with P-values of 0.11, 0.04 and 0.04, respectively. Similarly, for PT, significantly larger delta values were observed in females compared to males in both the overall participant group and the elderly subset. The delta values were 24.4° in young males versus 33.0° in young females, and 12.7° in elderly males versus 25.7° in elderly females 16.2° in males versus 28.7° in females for the overall group, with P-values of 0.09, 0.04 and 0.04, respectively. Lastly, PI was significantly larger in females than in males, with values of 42.3° for males and 47.7° for females, and a P-value of 0.048 (Table 2). Overall, these findings suggest that females exhibited a larger lordosis to match their higher PI and retained this flexibility until their elderly years.
Comparisons of the change of intervertebral disc angle and lordotic angles by posture between male and female subjects
There were no statistically significant changes in intervertebral disc angle between standing and sitting postures for both genders and across different age groups at all lumbar disc levels (Table 3). However, for the L4/5 disc level, there was a trend towards a larger delta in females, though not statistically significant (− 8.2° vs. − 10.4°, p = 0.28, Table 3). Furthermore, when comparing the lordotic angle of the lower lumbar spine (L3-S, L4-S segment), a significantly large delta was observed in elderly females when compared with elderly males (− 11.3° vs. − 21.5°, p = 0.04) (− 9.3° vs. − 14.1°, p = 0.04) (Table 4).
In summary, while there were no significant changes in intervertebral disc angles between standing and sitting postures, a trend towards larger changes in the L4/5 disc level of the females was observed. Additionally, there was a significant gender difference in the lordotic angle of the lower lumbar spine among elderly participants.
Comparisons of the change of FH by posture between male and female subjects
At the upper disc levels, there were no significant differences in FH between males and females during standing and sitting (Table 5). At the L4/5 disc level, large delta for FH was observed in females when compared with males being statistically significant in elderly females and a trend observed in overall females (p = 0.28, 0.04).
In summary, there was no significant difference in the change of FH between standing and sitting postures for both genders and all age groups in lumbar disc levels, except for the L4/5 level where a significant increase was observed in elderly females.
Comparisons of the change of BBA by posture between male and female subjects (Figs. 4 and 5)
Representative Cases of the Change of Foramen by Posture in the Young Subjects. (A) The L4/5 foramen of 32-year-old male during standing. (B) The L4/5 foramen of 32-year-old male during sitting. (C) The L4/5 foramen of 38-year-old female during standing, (D) The L4/5 foramen of 38-year-old female during sitting. A significant change of BBA was observed in a female patient when transitioning to a sitting position.
Representative cases of the change of foramen by posture in the elderly subjects. (A) The L4/5 foramen of 74-year-old male during standing. (B) The L4/5 foramen of 74-year-old male during sitting. (C) The L4/5 foramen of 72-year-old female during standing. (D) The L4/5 foramen of 72-year-old female during sitting. A significant change of FH was observed in a female patient when transitioning to a sitting position.
Similar to the findings in FH, at the upper disc levels, there were no significant differences in BBA between males and females during standing and sitting (Table 6). However, at the lower disc levels (L3/4, L4/5), females exhibited significantly larger BBA compared to males in both standing and sitting positions. Furthermore, the delta values were consistently larger in young females, with statistical significance observed in L4/5 (p = 0.01) and a trend observed in L3/4 in whole females (p = 0.08). Although the difference in the delta value between elderly males and females did not reach statistical significance, there was a trend towards a larger change in all lumbar foramen of BBA for females. These results indicate a consistent trend of larger BBA in females at the lower lumbar segments and that female tend to retain lumbar foraminal changes even in elderly age.
Discussion
This study meticulously evaluated and compared lumbar alignment obtained from CT scans in standing and sitting positions among a group of 24 healthy young individuals and 25 elderly individuals, with both groups equally distributed between genders.
In the study, significant differences between male and female were found in LL, PI, and L3/4 BBA in standing positions, and in PT, PI, L3/4/5 BBA in sitting positions, and SS, PT, L4/5BBA when comparing the change from standing to sitting position. Among the elderly subjects, significant differences were observed in SS, PT, and L4/5 FH in changes in posture.
Gender differences in lumbar alignment
A study by Zhou. reported the following values for standing and sitting positions in both genders (male vs. female; standing: LL: 51.1° vs. 52.0°, PT: 13.6° vs. 14.6°, sitting: LL: 26.8° vs. 21.3°, PT: 28.3° vs. 32.4°).7 Our study found smaller LL and PT values in both positions. This discrepancy could be attributed to the fact that our study reconstructed the sagittal plane from CT scans and involved a mixed cohort of young and elderly participants, whereas Zhou S's study focused on middle-aged and above. Moreover, the standing posture without any support may have caused subjects to be more bent forward in the standing CT, leading to different results. Hey et al. described a 50% decrease in LL and a 100% increase in PT when changing from a standing to a sitting position8. Another report by Hey et al. noted that in healthy young adults, the spinal alignment changes to a C-shape in a relaxed sitting position, with an 80% decrease in LL from the erect sitting position4. Our current study showed a decrease in LL of approximately 77% in male and 80% in female when moving from a standing to a relaxed sitting position.
Considering the changes in LL, SS, and PT due to postural changes, our results suggested that the decrease in LL and SS, and increase in PT due to the relaxed sitting position, result from the flexion of the hip joint and the tilt of the pelvis, reducing lumbar lordosis. The position of the hip joint and pelvis is fixed by the chair and foot angle, so the posterior bending of the lumbar spine that is compensated more than in the usual forward bending position is reflected.
Assessment of intervertebral foramen area
The assessment of intervertebral foraminal area is a crucial aspect of understanding lumbar spinal biomechanics. This study assessed the intervertebral foramen area by measuring FH and BBA. Previous reports have indicated that the intervertebral foramen area and height both decreases with age15. In our study, we obtained similar results, demonstrating a decrease in FH and BBA with age (p < 0.01).
Consideration of axis and 3D morphology
The prior studies lack descriptions regarding the axis for intervertebral foramen measurements5,16. We addressed this limitation by aligning the axis towards the lower vertebral arch root and adjusting the measured area according to 3D constructed bone. This approach improved measurement accuracy and minimized inter-observer error.
Comparison of male and female
Previous literature lacks studies comparing the intervertebral foramen between males and females. In our study, we observed significant gender differences in sitting posture and delta BBA at L4/5, suggesting gender-specific compensatory changes in this intervertebral space. Notably, with aging, significant gender differences emerged in the angle of lordosis in the lower lumbar spine (L4 to S1), as well as delta FH. These findings imply a potential for instability in the vertical direction of vertebrae.
Gender-specific changes and degenerative lumbar spondylolisthesis
Our research indicated that differences in SS and PT between females and males contribute to increased stress on the lower part of the lumbar spine, notably at the L4/L5 level. This stress is pronounced due to the anatomical and biomechanical changes that occur at this segment. With the process of aging, the intervertebral foramen may diminish in size but also exhibit a shift toward the upper part of the spinal column17. These changes correlate with a greater incidence of degenerative lumbar spondylolisthesis in females, with the L4/L5 segment being particularly susceptible. The study further suggests that with age, alterations of trunk muscle strength and postural instability may exacerbate this condition, leading to a forward slippage of the vertebrae, especially at the cranial aspect of the spinal segment.
In conclusion, our study highlights gender differences and age-related changes in the intervertebral foramen area. The findings provide insights into gender-specific compensatory changes and their potential association with degenerative lumbar spondylolisthesis, particularly in female.
Limitations
In this cross-sectional study, we sought to evaluate the lumbar spine components in standing and relaxed sitting positions using upright CT, with a sample comprising 24 young (aged 21–40, mean age 30.3 ± 5.7 years, 13 males, 11 females) and 25 elderly individuals (aged 61–79, mean age 65.7 ± 3.8 years, 12 males, 13 females). The selection criteria ensured a healthy cohort by excluding individuals with back pain, smokers, those outside a normal BMI range, individuals with a history of spinal surgery, non-Japanese, and those pregnant or possibly pregnant.
Despite rigorous methods, our study encounters several limitations. Firstly, the upright CT scanner's constraints on trunk motion may have affected the results, as it might not capture the full range of spinal movements. Secondly, while consistent seated postures without back support were maintained, there remains a possibility of individual variations in the "relaxed" position. Thirdly, the use of agency-recruited volunteers could introduce a selection bias, potentially affecting the representativeness of the sample. Lastly, the absence of middle-aged participants creates a gap in the data, possibly limiting the wider applicability of our findings to all age groups. Fourthly, the number of subjects might not be sufficient to determine significant differences with high statistical power, a factor that could influence the strength of our findings. Lastly, the absence of middle-aged participants creates a gap in the data, possibly limiting the wider applicability of our findings to all age groups.”
Nevertheless, this research, as a pioneering study using standing CT to detail lumbar spine components in a healthy population across genders, provides important contributions. The observed gender-based differences could enhance our understanding of conditions like degenerative spondylolisthesis.
Conclusion
This study offers a comprehensive analysis of the detailed lumbar components in healthy individuals using standing CT, while making a comparison between genders. The findings indicate significant gender differences in the changes of pelvic tilt and sacral slope during the transition from standing to sitting, with females exhibiting a greater range of change in these parameters. This difference is particularly amplified in a sitting posture, suggesting a potential for increased stress on the lower lumbar spine. Moreover, the study highlights the changes in the area of the vertebral foramen with aging. Notably, these changes show significant gender differences, suggesting different patterns of spinal degeneration between male and female.
One key observation is the possible impact of these changes at the L4/5 level, which may explain the higher incidence of lumbar degenerative spondylolisthesis in female. As the first study of its kind, it sheds light on the physiological differences in the lumbar spine between genders and contributes to a better understanding of spinal pathologies such as degenerative spondylolisthesis.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Botchu, R., Bharath, A., Davies, A. M., Butt, S. & James, S. L. Current concept in upright spinal MRI. Eur Spine J. 27, 987–993 (2018).
Kimura, T. et al. Evaluation of first-ray mobility in patients with hallux valgus using weight-bearing CT and a 3-D analysis system: A comparison with normal feet. J. Bone Joint Surg. Am. 99-A(3), 247–55 (2017).
Sano, H. et al. The difference of sagittal lumbo-pelvic alignment in standing and sitting position; analysis differences and aging. J. Tokyo Med. Univ. 81(1), 49–54 (2023).
Hey, H. W. et al. Differences in erect sitting and natural siting spinal alignment-insights into a new paradigm and implications in deformity correction. Spinal J. 17, 183–189 (2017).
Endo, K. et al. Sagittal lumbar and pelvic alignment in the standing and sitting positions. J. Orthop. Sci. 17, 682–686 (2012).
Lazennec, J. Y., Brusson, A. & Rousseau, M. A. Lumbar-pelvic-femoral balance on sittiing and standing lateral radiographs. Orthop. Traumatol. Surg. Res. 99(1), S87–S102 (2013).
Zhou, S. et al. Sagittal spinal and pelvic alignment in middle aged and older men and women in the natural and erect sitting positions: a prospective study in a Chinese population. Med. Sci. Monit. https://doi.org/10.12659/MSM.919441 (2020).
Hey, H. W. D. et al. How the spine differs in standing and in sitting-important considerations for correction of spinal deformity. Spine J. 17, 799–806 (2017).
Zhou, S. et al. The standing and sitting sagittal spinopelvic alignment of Chinese young and elderly population: Does age influence the differences between the two positions?. Euro. Spine J. 29, 405–412 (2020).
Jacobsen, S., Sonne-Holm, S., Rovsing, H., Monrad, H. & Gebuhr, P. Degenerative lumbar spondylolisthesis: An epidemiological perspective: The Copenhagen osteoarthritis study. Spine. 32, 120–125 (2007).
Jinzaki, M. et al. Development of upright computed tomography with area detector for whole-body scans: Phantom study, efficacy on workflow, effect of gravity on human body, and potential clinical impact. Invest. Radiol. 55, 73–83 (2020).
Yamada, Y. et al. Dose reduction in chest CT: Comparison of the adaptive iterative dose reduction 3D, adaptive iterative dose reduction, and filtered back projection reconstruction techniques. Eur. J. RADIOL. 81, 4185–4195 (2012).
O’Brien, M. F., Kuklo, T. R., Blanke, K. M. & Lenke, L. G. Radiographic measurement manual (Spine Deformity Study Group. Medtronic Sofamor Danek USA Inc., MN, 2008).
Zhu, K. et al. Morphological changes of contralateral intervertebral foramen induced by cage insertion orientation after unilateral transforaminal lumbar interbody fusion. J. Orthop. Surg. Res. 14, 79 (2019).
Yan, S. et al. Three-dimensional morphological characteristics of lower lumbar intervertebral foramen with age. BioMed. Res. Int. 2018, 8157061 (2018).
Liu, M. et al. Dimensional changes of lumbar intervertebral foramen in direct anterior approach-specific hyperextension supine position. Orthop. Surg. 12(4), 1173–1181 (2020).
Hasegewa, K., Kitahara, K., Hara, T., Takano, K. & Shimoda, H. Biomechanical evaluation of segmental instability in degenerative lumbar spondylolisthesis. Eur Spine J. 18(4), 465–470 (2009).
Funding
Funding was provided by Japan Society for the Promotion of Science (Grant No. JP23K07214, JP21H03799, JP20K08056) and Takeda Science Foundation.
Author information
Authors and Affiliations
Contributions
Ryo Mizukoshi, Mitsuru Yagi, and Takeo Nagura contributed to the study conception and design. Data collection was performed by Ryo Mizukoshi and Mitsuru Yagi. Ryo Mizukoshi, Mitsuru Yagi, Yoshitake Yamada, Yoishi Yokoyama, and Minoru Yamada contributed to the data analyses. The first draft of the manuscript was written by Mitsuru Yagi. Kota Watanabe, Masaya Nakamura, and Masahiro Jinzaki revised it critically for important intellectual content and all authors commented on the manuscript. All authors read and approved the final manuscript. Masahiro Jinzaki and Mitsuru Yagi are both corresponding author of this study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mizukoshi, R., Yagi, M., Yamada, Y. et al. Gender differences in spinal mobility during postural changes: a detailed analysis using upright CT. Sci Rep 14, 9154 (2024). https://doi.org/10.1038/s41598-024-59840-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-59840-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.