Abstract
The aim of this study was to cross-sectionally investigate the relationships between obesity and spinal posture as well as mobility by comparing the spinal parameters between adults with obesity and normal-weight individuals. The spinal parameters were measured in 71 adults with obesity and 142 normal-weight individuals using a radiation-free back scan, the Idiag M360. Differences in spinal posture and movements between the two groups were determined using a two-way analysis of variance. Adults with obesity had greater thoracic kyphosis [difference between groups (Δ) = 6.1°, 95% CI 3.3°–8.9°, p < 0.0001] and thoracic lateral flexion (Δ = 14.5°, 95% CI 5.1°–23.8°, p = 0.002), as well as smaller thoracic flexion (Δ = 3.5°, 95% CI 0.2°–6.9°, p = 0.03), thoracic extension (Δ = 4.1°, 95% CI 1.1°–7.1°, p = 0.008), lumbar flexion (Δ = 10.4°, 95% CI 7.7°–13.5°, p < 0.0001), lumbar extension (Δ = 4.8°, 95% CI 2.2°–7.4°, p = 0.0003) and lumbar lateral flexion (Δ = 12.8°, 95% CI 9.8°–15.7°, p = < 0.0001) compared to those with normal weight. These findings provide relevant information about the characteristics of the spine in adults with obesity to be taken into careful consideration in the prescription of adapted physical activities within integrated multidisciplinary pathways of metabolic rehabilitation.
Similar content being viewed by others
Introduction
The prevalence of obesity has been increasing across worldwide populations, despite it being preventable1. The obesity rate has tripled since 1975. In 2016, more than one-third of adults were overweight, and around one out of 8 adults were obese. The consequences of obesity cover a wide range of health issues and the associated economic burden in both developed and developing countries1,2,3. A systematic review of the global economic burden of obesity reported that obesity-related costs across different countries range between 0.7% and 2.8% of their health expenditures, whilst medical costs were around 30% greater in people with obesity than in those who were not obese4. Systematic reviews of health and economic consequences of obesity also highlight that an urgent need for improved strategies for better prevention and intervention of obesity as a chronic disease2,3. Various body systems are negatively affected by obesity, leading to an increased risk of pathological conditions, including metabolic, cardiorespiratory, and musculoskeletal diseases1,3. For example, obesity is considered to be one of the five metabolic factors, including high blood pressure, hyperglycemia, central obesity, high triglycerides, and abnormal cholesterol that raise the risk of cardiovascular disease and type 2 diabetes5. The increasing prevalence of obesity worldwide is considered by International Diabetes Federation as one of the main driving factors behind the high prevalence of the metabolic syndrome6. Physical activity, diet and behavioural changes remain the cornerstone of the management of obesity and obesity related conditions7,8 as overweight and obesity are more likely if there is an imbalance between energy intake and expenditure9. Promoting exercise and motion commonly used in the management of obesity is also associated with a reduced risk of common musculoskeletal conditions, including low back pain and knee osteoarthritis8,10,11. However, the influence of obesity on human motion, particularly spinal kinematics/movements, although crucial to daily activities and the management of spinal conditions, has been understudied.
Spinal kinematics/motion appears to be altered by obesity in both adolescents and adults12,13. Spinal kinematics/motion is essential to perform a range of activities of daily living, such as personal hygiene activities (hand washing, washing hair and shaving) and locomotive activities of daily living (walking, ascending and descending stairs)14. Putting on socks and picking up an object off the floor were found to be the activities of daily living requiring the largest lumbar range of motion compared to other activities of daily living14. Alterations of spinal movements are also often linked with musculoskeletal problems, particularly low back pain. To date, both cross sectional and longitudinal studies found that alterations in spinal kinematics are associated with low back pain15,16,17. Abnormal loading in the spine leading to tissue degeneration, potentially causing pain and other symptoms may be caused by alterations in spinal kinematics18. In clinical practice, spinal posture and flexibility/motion are also commonly investigated as part of musculoskeletal examinations, emphasising the importance of preserving spinal kinematics. Additionally, obesity is believed to be a risk factor for developing low back pain, although the mechanism through which obesity influences low back pain remains unclear. A cross-sectional study of nine healthy normal-weight adults and nine obese individuals investigating differences in spinal segment range of motion found that obese adults had smaller lumbopelvic motion compared to age, height and sex matched normal weight individuals13. However, studies examining the influence of obesity on spinal kinematics/motion, particularly spinal postures remain sparse to date. Exploring the effect of obesity on spinal postures as well as kinematics/motion would help to better understand the characteristics of these spinal parameters in obese adults.
The aim of this study was to examine the influence of obesity on spinal postures as well as kinematics/motion and hip kinematics by comparing the parameters in obese adults and in normal weight individuals.
Methods
The present study used a cross-sectional design to examine the relationship between obesity and spinal posture as well as mobility and followed the “Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)” recommendations19.
Participants
Obese and normal-weight individuals according to the World Health Organization guidelines were recruited into the study20. Obesity and normal weight were defined in presence of a body mass index > 35 and BMI < 25, respectively. Participants were excluded if they had past and present musculoskeletal or neurological conditions, such as limb length discrepancy, spinal deformities and surgeries determining physical disabilities, as well as those taking anti-inflammatory medications. Normal-weight individuals were recruited from the general population in the Canton of Zurich, Switzerland. Individuals with obesity who were hospitalized for a three-week multidisciplinary body weight reduction program at the Division of Metabolic Diseases, Istituto Auxologico Italiano, IRCCS, Piancavallo (VB), Italy were recruited in this study. The Ethics Committee of the Istituto Auxologico Italiano (Milan, Italy; research project code: 01C124; acronym: PRORIPONATFIS) and the Ethics Committee of Zurich (BASEC-no. 2018-00979) approved the study. All procedure in this study were in compliance with the Helsinki Declaration of 1975, as revised in 2008. The purpose of the study was explained to the participants and written informed consent was obtained.
Measurements
Posture and mobility of the spine and hip motion were assessed using the Idiag M360 scan tool (Idiag, Fehraltorf, Switzerland)21. Spinal postures were defined from an upright standing position, whilst spinal mobility/range of motion was determined during dynamic tasks, such as flexion, extension and lateral bending. The Idiag M360 is a radiation-free, non-invasive, reliable, skin-surface device, which quantifies the spinal posture and motion through recording angles of each vertebral joint and sacral slope using computer-assisted analysis. The data of these parameters are sampled at a frequency of 150 Hz22,23. During the recording, positions and mobility of each individual segment are estimated. Vertebral distances and angles are measured while two rolling wheels contained in the device follow the vertebral spinous processes. An analogue–digital converter transfers radiographically the parameters, estimated by the rolling wheels, to a personal computer. A validity study evaluating for measurements of spinal curvatures using an X-ray examination showed a very good correlation between measurements made by radiography and spinal mouse22,24. Spinal ranges of motion reported in the literature previously were also comparable with the values determined by the Idiag M36025. Additionally, a previous comparative study exploring the validity and reliability of the device for the measurement of lumbar flexion also reported that segmental and global lumbar ranges of motion determined by radiography and the device were comparable26.
The reliability of the device has previously been examined in both normal weight and obese individuals12,27.
The spinal parameters (spinal and hip mobility) were determined in the longitudinal and coronal planes as participants were instructed to do flexion (bend forward), extension and then bilateral side bending from an upright standing position, as described in the protocol for measuring spinal posture and mobility provided by previous studies12,22,27. Using the educational videos, both assessors who evaluated the spinal posture and mobility in the obese and normal weight participants had been trained by the Idiag staff.
The reliability of the device in obese individuals was examined as part of the previous study, showing that the intrarater intraclass correlation coefficients for the spinal postures ranged from 0.86 to 0.94, and the standard error of measurement values ranged 0.58° to 0.70°12, whilst for spinal mobility the intrarater intraclass correlation coefficients in the coronal and sagittal planes ranged from 0.57 to 0.80 and 0.87 to 0.98, respectively. Measurements of spinal curvature and kinematics/motion using the device in non-obese individuals also showed fair to good reliability25. In this study, the average standard error of measurement was approximately 2°, whilst the interexaminer reliability on lumbar and thoracic movements assessed by two examiners ranged from 0.62 to 0.9325.
Data processing
The difference between range of motion values in each segment of the spine determined at the standing position and the end of motion ranges in the sagittal and frontal planes was used to estimate each range of motion value for the spinal parameters. The sum of the respective range of motion values in each spinal segment (5 and 12 range of motion values for the lumbar and thoracic spine, respectively) were used to determine the total lumbar and thoracic range of motion of the spine. The sacral inclination at the end of lumbar flexion and extension in the sagittal plane was used to determine hip flexion and extension, respectively.
Statistical analysis
R version 4.2.2 was used to perform descriptive and inferential statistics28. Mean values and standard deviations (SD) for participants’ age, sex, spinal posture and motion, as well as hip motion and lumbar to hip ratio were determined in descriptive statistics. Shapiro–Wilk test was used to assess data normality. Differences in demographic and anthropometric characteristics between the two groups (obese and normal-weight) were determined using the independent samples t-test for normally distributed data, the Wilcoxon’s rank sum test for non-normally distributed parameters and the Pearson’s chi-square test for categorical variables. Multiple regression models adjusting for age and sex were used to explore the association between BMI and spinal movements. Age and sex adjusted two-way analysis of variance (ANOVA) was used to determine statistically significant differences in spinal posture and mobility between the two groups. Pairwise post hoc tests were applied using the software package “emmeans” to compare between groups following the ANOVA tests29. Statistical significance was considered as a p value of less than 0.05.
Results
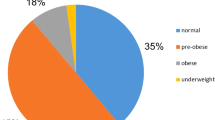
A total of 71 adults with obesity (45 females, 26 males) and 142 normal-weight individuals (91 females, 51 males) participated in the study. Participants’ characteristics are shown in Table 1, and no differences in the mean age, height and sex ratio were not observed between the normal-weight and obese groups (p > 0.05). Segmental posture and motion of the spine in the normal-weight subjects in comparison with individuals with obesity are described in Fig. 1. Differences in segmental postures and movements of proximal thoracic vertabrae were most commonly observed between the two groups. For instance, larger kyphosis and less flexion in proximal thoracic vertabrae were observed in adults with obesity than in normal-weight individuals (Fig. 1).
In the age and sex adjusted regression analysis on BMI and spinal movements of adults with obesity and normal-weight individuals, thoracic flexion (β = − 0.24, 95% confidence interval [CI] − 0.37; − 0.10), lumbar flexion (β = − 0.37, 95% CI − 0.50; − 0.24), lumbar extension (β = − 0.23, 95% CI − 0.34; − 0.13), lumbar lateral flexion (β = − 0.54, 95% CI − 0.66; − 0.42), hip flexion (β = − 0.48, 95% CI − 0.67; − 0.29) and hip extension (β = − 0.28, 95% CI − 0.42; − 0.14) were inversely associated with body mass index except for thoracic lateral flexion (β = 0.76, 95% CI 0.38; 1.14), which was positively associated with body mass index. No statistically significant association was found between thoracic extension and BMI (p > 0.05).
Associations of obesity with spinal posture and mobility as well as hip motion
Statistically significant differences were observed in thoracic kyphosis and spinal as well as hip mobility between the normal-weight and obese groups (Table 2). Individuals with obesity had larger thoracic kyphosis, particularly proximal thoracic kyphosis than the normal-weight subjects, whilst distal thoracic kyphosis was smaller in the obese participants. No statistically significant differences were observed in lumbar lordosis and sacral kyphosis between the two groups. Spinal and hip mobility were smaller in the obese participants than the normal-weight subjects except for the thoracic lateral flexion, which was greater in the individuals with obesity. In the post hot test, the greatest differences observed among spinal mobility were thoracic and lumbar lateral flexion (Table 2). Thoracic lateral flexion was 14.3° greater in obese individuals, whereas lumbar lateral flexion was 13.80 larger in normal-weight subjects. No statistically significant differences were observed between the two groups in lumbar lordosis, sacral kyphosis and lumbar to hip ratio.
Discussion
The purpose of the present study was to investigate the relationship between obesity and spinal posture as well as motion/kinematics in adults, with the key finding being that alterations in spinal posture and mobility as well as hip motion were associated with obesity. Obesity in adults was associated with decreased spinal and hip mobility and increased thoracic kyphosis, particularly proximal kyphosis but decreased distal thoracic kyphosis and lateral flexion. Thoracic kyphosis appears to be substantially influenced by obesity, which may in turn increase mechanical challenges that the thoracic spine must withstand.
Increased thoracic kyphosis was associated with obesity, but no significant associations were found between obesity and lumbar lordosis as well as sacral kyphosis. Although the excess of fat mass is generally believed to add strain to the spine, studies specifically examining the association of obesity with spinal postures in adults are lacking but alterations in spinal postures have been explored in relation to obesity in children and adolescents12,30. For instance, a cohort study of 1621 adolescents with and without idiopathic scoliosis examining retrospectively the association of BMI with thoracic kyphosis showed that the relationship between increased BMI and increased thoracic kyphosis in both adolescents with and without spinal deformity30. Our previous study examining the influence of obesity on spinal posture in children and adolescents also found the association of obesity with increased thoracic kyphosis12, suggesting that obesity may play an important role in the characteristics of spinal postures in both children and adults, regardless of age. Additionally, these findings also imply that the influence of obesity determined in children and adolescents on thoracic kyphosis may be preserved in adulthood. Obesity was not associated with lumbar and sacral postures in the current study, which was consistent with the findings from previous cross-sectional studies exploring the impact of BMI and obesity on spino-pelvic parameters, including lumbar lordosis and sacral slope, measured on lateral X-ray31,32. A previous cross-sectional study of female participants (30 normal-weight, 30 overweight and 29 obese) examining the impact of age, BMI and the bone mineral density on lumbar and pelvic postures demonstrated no differences in the vertebral and spinopelvic angle measures between the three different BMI groups31. Another cross-sectional study of individuals who were assigned into the three different BMI groups (51 normal weight individuals, 93 overweight, and 56 obese) exploring the association between obesity and the spino-pelvic characteristics revealed that no significant differences were observed in lumbar lordosis as well as sacral slope across the three different BMI groups32. These results suggest that obesity appears to affect thoracic kyphosis more than lumbar and sacral postures, regardless of age. Both cross-sectional and longitudinal studies have shown that hyperkyphotic posture is associated with reduced physical function, such as reduced gait speed as well as impaired functional mobility and physical performance33,34,35,36,37. These results imply that the combination of obesity and increased risk of hyperkyphotic posture could potentially further worsen physical performance and mobility. However, future longitudinal studies are needed to deepen the understanding of potential impacts of obesity on physical performance and mobility. In addition, alterations in thoracic kyphosis appears to increase with aging as a systematic review examining the posture and motion of the thoracic spine reported that thoracic kyphosis deepens by approximately 3 degrees per decade38. In the present study, thoracic alignment of participants in both the obese and normal-weight groups also was hyperkyphotic as the mean angle of the thoracic kyphosis was more than 40°39. A change in thoracic kyphosis is also observed in the transition from sitting to standing position40,41. For instance, a prospective study reported that a decrease of 8.5° in thoracic kyphosis in the transition between sitting and standing positions due to the change in the sagittal balance and the center of gravity from standing to sitting40. A recent review study also summarized that the thoracic kyphosis, lumbar lordosis and sacral slope decreased from standing to sitting by up to approximately 50% as sitting leads to straighten the spine41. These findings would help to better understand spinal posture and kinematics/motion in relation to obesity and provide further insights into mechanical challenges associated with obesity such as excessive accumulation of body fat in the trunk, increasing the mechanical load of the thoracic spine. However, future studies exploring the effect of obesity on alterations in spinal posture longitudinally could be important to better understand the role of obesity in spinal posture and its deformity.
The spinal and hip movements measured in the sagittal and frontal planes were smaller in the obese adults than in the normal-weight individuals, except for thoracic lateral flexion, which was larger in the obese participants. Spinal and hip movements were also inversely associated with BMI, except for thoracic lateral flexion, which was positively associated with BMI. Reduced spinal mobility in adults with obesity could mainly be explained by their dimensions potentially restricting the available range of motion at the hip and the spine. For example, a previous retrospective of 84 patients stratified into normal, overweight and obese groups found that individuals with obesity demonstrated more posterior spinopelvic tilt from standing to sitting to compensate for soft-tissue tension around the hip joint limiting hip flexion42. However, more research is needed to better understand whether there are other mechanisms/factors associated with obesity contributing to restrict spinal mobility other than the body dimensions or physical features of obesity. Spinal mobility is crucial for performing daily activities and reduced spinal movements are often linked with musculoskeletal problem, particularly low back pain, suggesting the importance of preserving spinal mobility14,17,43. For example, a systematic review of prospective studies exploring the association of reduced spinal mobility with low back pain demonstrated that restricted lumbar mobility in the coronal plane was associated with the risk of low back pain17. Previous studies exploring differences in the characteristics of the spine between obese and normal-weight people also revealed that individuals with obesity had smaller spinal mobility30,44. Additionally, a systematic review of in vivo studies investigating thoracic posture and motion in adults with and without idiopathic scoliosis highlighted decreased thoracic range of motion in obese individuals30, which was consistent with the findings from the present study. However, in the present study, thoracic lateral flexion was greater in adults with obesity whereas lumbar lateral flexion was smaller in these participants compared to the normal-weight adults. Obesity appears to have an influence on decreased lumbar lateral flexion, which in turn may require increased thoracic lateral flexion. Our previous study conducted in obese and normal-weight children and adolescents showed that both thoracic and lumbar lateral flexion movements were smaller in the obese participants12, suggesting that smaller spinal lateral movements needed for daily activities may be compensated by increased thoracic lateral flexion. Nevertheless, future longitudinal studies following adolescents until their adult age may be important to better understand how obesity impacts on the characteristics of the spine from childhood to adulthood.
Obesity was associated with reduced hip mobility as well, but no associations were found with lumbar to hip ratio. Hip mobility is also important for our daily activities that allows individuals to move around in the environment. Hip range of motion is crucially important to conduct activities of daily living and functional activities requiring a large range of motion such as squatting, kneeling, as well as cross-legged sitting43. For example, a previous cross-sectional study of generating three-dimensional kinematics at the hip, knee and ankle joints of 30 healthy participants when performing high range of motion activities, namely (squatting heels down, squatting heels up, kneeling dorsi-flexed, kneeling plantar-flexed and sitting cross-legged) reported that squatting with heels up required the largest hip flexion, reaching up to 95 degrees, whereas kneeling plantar-flexed required the smallest hip flexion, reaching up to 62 degrees among the five activities of daily living43. Therefore, obesity could potentially hinder adults with obesity more in performing functional activities, such as squatting compared to those with normal weight.
Restrictions in hip mobility are also associated with musculoskeletal conditions, particularly hip conditions. For example, a systematic review of prospective and case control studies determined the association of reduced total hip range of motion, particularly hip rotation with the risk of developing groin pain in athletes45. A previous study of 30 female participants with non-specific low back pain exploring the effect of stretching exercises targeting the hip flexors for a period of 8 weeks revealed that disability, pain, and passive range of motion improved more in participants who received the exercises than those who did not this intervention46. The findings of this study suggest that hip flexibility, particularly hip extension may be crucial to be taken into account in the management of non-specific low back pain. In addition to reduced hip flexibility in people with obesity, the combination of hyperkyphotic posture and reduced spinal mobility could potentially further contribute to increase the risk of low back pain. Although hip mobility was smaller in adults with obesity, lumbar to hip ratio was not different between adults with obesity and normal weight controls. Decreased range of motions observed in both the hip and lumbar mobility could explain this as the proportion of these two variables defines the lumbar to hip ratio. Our previous study conducted in children and adolescents also demonstrated that obesity was associated with reduced hip mobility but not with lumbar to hip ratio, implying that the influence of obesity on hip mobility may also be preserved in adulthood12. However, a need for future studies to investigate whether longitudinal associations between obesity and hip mobility exist to further understand the role of obesity in hip mobility.
We acknowledge that the present study has several limitations. The present study employed the cross-sectional design, which precludes any causal interpretations of the observed relationships between obesity and spinal posture as well as motion/kinematics. In the present study, spinal mobility was measured in the sagittal and frontal planes, thus hampering to generalise the influence of obesity on the spinal movements measured to spinal mobility in the transverse plane. The accuracy of the Idiag M360 as a skin surface device for the measurement of spinal posture and mobility could potentially be affected by skin movement artefact, particularly in the obese participants due to a greater percentage of soft tissue. However, the study was strengthened by providing detailed information about the characteristics of the spine such as global as well as segmental posture and motion of the spine in adults with obesity and normal weight controls. In addition, the relatively broad study population (obese and controls) was evaluated in the two research centers by well-trained staff in standardized experimental conditions.
Obesity was associated with changes in spinal posture, and spinal as well as hip motion/kinematics in adults. Obesity was associated with increased thoracic kyphosis but decreased spinal and hip mobility, except for thoracic lateral flexion. Increased thoracic kyphosis observed in those with obesity may be a biomechanical adaptation to maintain center of gravity in the anterior–posterior direction. Reduced lumbar lateral movements found in the adults with obesity may be compensated by increased thoracic lateral flexion to perform for daily activities. Lumbar lordosis and sacral kyphosis or the lumbar to hip ratio appear to be not affected by obesity. These results provide relevant important information about the characteristics of the spine in adults with obesity to be taken into careful consideration in the prescription of adapted physical activities within integrated multidisciplinary pathways of metabolic rehabilitation, as well as unique insights into mechanical challenges associated with obesity such as excessive accumulation of body fat in the trunk, increasing the mechanical load of the spine. These findings also highlight the significance of considering obesity in the musculoskeletal assessment of spinal curvatures and approaches designed to promote spinal and hip flexibility in adults with obesity.
Data availability
The data presented in this study are available from the corresponding author upon reasonable request.
References
World Health Organization. Obesity and Overweight, https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (2021).
Tremmel, M., Gerdtham, U. G., Nilsson, P. M. & Saha, S. Economic burden of obesity: A systematic literature review. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph14040435 (2017).
Powell-Wiley, T. M. et al. Obesity and cardiovascular disease: A scientific statement from the american heart association. Circulation 143, e984–e1010. https://doi.org/10.1161/cir.0000000000000973 (2021).
Withrow, D. & Alter, D. A. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes. Rev. Off. J. Int. Assoc. Study Obes. 12, 131–141. https://doi.org/10.1111/j.1467-789X.2009.00712.x (2011).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; National heart, lung, and blood institute; american heart association; World heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120, 1640–1645. https://doi.org/10.1161/circulationaha.109.192644 (2009).
Alberti, K. G. M. M., Zimmet, P. & Shaw, J. Metabolic syndrome—A new world-wide definition. A consensus statement from the international diabetes federation. Diabet. Med. 23, 469–480. https://doi.org/10.1111/j.1464-5491.2006.01858.x (2006).
Fock, K. M. & Khoo, J. Diet and exercise in management of obesity and overweight. J. Gastroenterol. Hepatol. 28(Suppl 4), 59–63. https://doi.org/10.1111/jgh.12407 (2013).
Dantas, L. O., Salvini, T. F. & McAlindon, T. E. Knee osteoarthritis: Key treatments and implications for physical therapy. Braz. J. Phys. Ther. 25, 135–146. https://doi.org/10.1016/j.bjpt.2020.08.004 (2021).
Wiklund, P. The role of physical activity and exercise in obesity and weight management: Time for critical appraisal. J. Sport Health Sci. 5, 151–154. https://doi.org/10.1016/j.jshs.2016.04.001 (2016).
Hayden, J. A., Ellis, J., Ogilvie, R., Malmivaara, A. & van Tulder, M. W. Exercise therapy for chronic low back pain. Cochrane Database Syst. Rev. 9, 009790. https://doi.org/10.1002/14651858.CD009790.pub2 (2021).
Alzahrani, H., Shirley, D., Cheng, S. W. M., Mackey, M. & Stamatakis, E. Physical activity and chronic back conditions: A population-based pooled study of 60,134 adults. J. Sport Health Sci. 8, 386–393. https://doi.org/10.1016/j.jshs.2019.01.003 (2019).
Bayartai, M. E. et al. Differences in spinal posture and mobility between children/adolescents with obesity and age-matched normal-weight individuals. Sci. Rep. https://doi.org/10.1038/s41598-022-19823-z (2022).
Ghasemi, M. & Arjmand, N. Spinal segment ranges of motion, movement coordination, and three-dimensional kinematics during occupational activities in normal-weight and obese individuals. J. Biomech. 123, 110539. https://doi.org/10.1016/j.jbiomech.2021.110539 (2021).
Bible, J. E., Biswas, D., Miller, C. P., Whang, P. G. & Grauer, J. N. Normal functional range of motion of the lumbar spine during 15 activities of daily living. J. Spinal Disord. Tech. 23, 106–112. https://doi.org/10.1097/BSD.0b013e3181981823 (2010).
Scholtes, S. A., Gombatto, S. P. & Van Dillen, L. R. Differences in lumbopelvic motion between people with and people without low back pain during two lower limb movement tests. Clin. Biomech. (Bristol, Avon) 24, 7–12. https://doi.org/10.1016/j.clinbiomech.2008.09.008 (2009).
Zhou, J., Ning, X. & Fathallah, F. Differences in lumbopelvic rhythm between trunk flexion and extension. Clin. Biomech. (Bristol, Avon) 32, 274–279. https://doi.org/10.1016/j.clinbiomech.2015.10.012 (2016).
Sadler, S. G., Spink, M. J., Ho, A., De Jonge, X. J. & Chuter, V. H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 18, 179–179. https://doi.org/10.1186/s12891-017-1534-0 (2017).
Iorio, J. A., Jakoi, A. M. & Singla, A. Biomechanics of degenerative spinal disorders. Asian Spine J. 10, 377–384. https://doi.org/10.4184/asj.2016.10.2.377 (2016).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 61, 344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008 (2008).
World Health Organization. Obesity, https://www.who.int/tools/growth-reference-data-for-5to19-years/indicators/bmi-for-age (2023).
Idiag. Idiag M360, https://www.idiag.ch/en/idiag-m360-en/ (2021).
Livanelioglu, A., Kaya, F., Nabiyev, V., Demirkiran, G. & Fırat, T. The validity and reliability of “Spinal Mouse” assessment of spinal curvatures in the frontal plane in pediatric adolescent idiopathic thoraco-lumbar curves. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 25, 476–482. https://doi.org/10.1007/s00586-015-3945-7 (2016).
Mannion, A. F., Knecht, K., Balaban, G., Dvorak, J. & Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. 13, 122–136. https://doi.org/10.1007/s00586-003-0618-8 (2004).
Nouh, M. R. Imaging of the spine: Where do we stand?. World J. Radiol. 11, 55–61. https://doi.org/10.4329/wjr.v11.i4.55 (2019).
Mannion, A. F., Knecht, K., Balaban, G., Dvorak, J. & Grob, D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: Reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 13, 122–136. https://doi.org/10.1007/s00586-003-0618-8 (2004).
Guermazi, M. et al. Validity and reliability of Spinal Mouse to assess lumbar flexion. Ann. Readapt. Med. Phys. 49, 172–177. https://doi.org/10.1016/j.annrmp.2006.03.001 (2006).
Kellis, E., Adamou, G., Tzilios, G. & Emmanouilidou, M. Reliability of spinal range of motion in healthy boys using a skin-surface device. J. Manip. Physiol. Ther. 31, 570–576. https://doi.org/10.1016/j.jmpt.2008.09.001 (2008).
R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2019).
Lenth R. Emmeans: Estimated Marginal Means, aka Least-Squares Means. R package version 1.6.3. (2021).
Valdovino, A. G. et al. Obesity is associated with increased thoracic kyphosis in adolescent idiopathic scoliosis patients and nonscoliotic adolescents. Spine Deform. 7, 865–869. https://doi.org/10.1016/j.jspd.2019.03.010 (2019).
Canbek, U. et al. The effect of age, BMI, and bone mineral density on the various lumbar vertebral measurements in females. Surg Radiol. Anat. 43, 101–108. https://doi.org/10.1007/s00276-020-02560-1 (2021).
Romero-Vargas, S. et al. The impact of body mass index and central obesity on the spino-pelvic parameters: A correlation study. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 22, 878–882. https://doi.org/10.1007/s00586-012-2560-0 (2013).
Katzman, W. B., Vittinghoff, E. & Kado, D. M. Age-related hyperkyphosis, independent of spinal osteoporosis, is associated with impaired mobility in older community-dwelling women. Osteoporos. Int. 22, 85–90. https://doi.org/10.1007/s00198-010-1265-7 (2011).
Katzman, W. B., Vittinghoff, E., Ensrud, K., Black, D. M. & Kado, D. M. Increasing kyphosis predicts worsening mobility in older community-dwelling women: A prospective cohort study. J. Am. Geriatr. Soc. 59, 96–100. https://doi.org/10.1111/j.1532-5415.2010.03214.x (2011).
Eum, R. et al. Is kyphosis related to mobility, balance, and disability?. Am. J. Phys. Med. Rehabil. 92, 980–989. https://doi.org/10.1097/PHM.0b013e31829233ee (2013).
Antonelli-Incalzi, R. et al. Relationship between the occiput-wall distance and physical performance in the elderly: A cross sectional study. Aging Clin. Exp. Res. 19, 207–212. https://doi.org/10.1007/bf03324691 (2007).
Gladin, A. et al. Secondary analysis of change in physical function after exercise intervention in older adults with hyperkyphosis and low physical function. BMC Geriatr. 21, 133. https://doi.org/10.1186/s12877-021-02062-8 (2021).
Pan, F., Firouzabadi, A., Reitmaier, S., Zander, T. & Schmidt, H. The shape and mobility of the thoracic spine in asymptomatic adults - A systematic review of in vivo studies. J. Biomech. 78, 21–35. https://doi.org/10.1016/j.jbiomech.2018.07.041 (2018).
Katzman, W. B., Wanek, L., Shepherd, J. A. & Sellmeyer, D. E. Age-related hyperkyphosis: Its causes, consequences, and management. J. Orthop. Sports Phys. Ther. 40, 352–360. https://doi.org/10.2519/jospt.2010.3099 (2010).
Hey, H. W. D. et al. How the spine differs in standing and in sitting—Important considerations for correction of spinal deformity. Spine J. 17, 799–806. https://doi.org/10.1016/j.spinee.2016.03.056 (2017).
Tsagkaris, C. et al. The sitting vs standing spine. North American Spine Soc. J. (NASSJ) 9, 100108. https://doi.org/10.1016/j.xnsj.2022.100108 (2022).
Buckland, A. J. et al. Obesity alters spinopelvic alignment changes from standing to relaxed sitting: The influence of the soft-tissue envelope. Arthroplasty Today 6, 590-595.e591. https://doi.org/10.1016/j.artd.2020.02.011 (2020).
Hemmerich, A., Brown, H., Smith, S., Marthandam, S. S. & Wyss, U. P. Hip, knee, and ankle kinematics of high range of motion activities of daily living. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 24, 770–781. https://doi.org/10.1002/jor.20114 (2006).
Gilleard, W. & Smith, T. Effect of obesity on posture and hip joint moments during a standing task, and trunk forward flexion motion. Int. J. Obes. 2005(31), 267–271. https://doi.org/10.1038/sj.ijo.0803430 (2007).
Tak, I. et al. Is lower hip range of motion a risk factor for groin pain in athletes? A systematic review with clinical applications. Br. J. Sports Med. 51, 1611–1621. https://doi.org/10.1136/bjsports-2016-096619 (2017).
Hatefi, M., Babakhani, F. & Ashrafizadeh, M. The effect of static stretching exercises on hip range of motion, pain, and disability in patients with non-specific low back pain. J. Exp. Orthop. 8, 55. https://doi.org/10.1186/s40634-021-00371-w (2021).
Acknowledgements
The authors acknowledge Dario Morelli and Donato Grieco, MVM, Lainate, Italy for their technical support and advice.
Funding
This work was supported by the Italian Ministry of Health – ricerca corrente.
Author information
Authors and Affiliations
Contributions
Conceptualization: A.S., H.L.; Data acquisition: R.D.M., G.T., L.A.; Formal analysis: M.E.B.; Funding acquisition: A.S.; Investigation: R.D.M., G.T., L.A.; Supervision, A.S., H.L.; Writing original draft: M.E.B..; Writing, review and editing: A.S., H.L, M.E.B. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bayartai, ME., Luomajoki, H., Tringali, G. et al. Differences in spinal posture and mobility between adults with obesity and normal weight individuals. Sci Rep 13, 13409 (2023). https://doi.org/10.1038/s41598-023-40470-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40470-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.