Abstract
The interplay between fatty liver disease (FLD) and metabolic dysfunction has given rise to the concept of metabolic associated fatty liver disease (MAFLD). With vitamin D insufficiency frequently co-occurring with FLD and linked to metabolic abnormalities, this study investigates the potential role of vitamin D in the development of MAFLD. In this cross-sectional analysis, 22,476 participants with baseline metabolic dysfunction and known serum 25-OH-vitamin D3 levels were examined. The fatty liver index (FLI) was utilized to predict FLD, dividing subjects into MAFLD and non-MAFLD groups. Further stratification by vitamin D levels (sufficient vs. insufficient) and gender provided a detailed assessment through binary logistic regression to determine the association of vitamin D status with MAFLD incidence. Vitamin D insufficiency correlated with a higher MAFLD incidence in metabolically impaired individuals. Post-adjustment, the correlation was stronger (men: aOR = 1.32, 95% CI = 1.22–1.43, P < 0.001; women: aOR = 1.53, 95% CI = 1.18–1.98, P = 0.001). Lower serum 25-OH-vitamin D3 levels were found in MAFLD patients across genders (men: P = 0.003; women: P = 0.014), with a higher prevalence of insufficiency in MAFLD cases (men: P = 0.007; women: P = 0.003). The vitamin D-MAFLD link was stable across subgroups and using varying FLI criteria. Our findings indicate a clear association between vitamin D insufficiency and increased MAFLD incidence, underscoring the potential of vitamin D as an anti-lipogenic and anti-fibrotic agent.
Similar content being viewed by others
Introduction
The prevalence of nonalcoholic fatty liver disease (NAFLD) has surged, positioning it as a principal contributor to liver pathology globally and a significant factor in hepatocellular carcinoma within the United States1. Concurrent with the rise in type 2 diabetes mellitus (T2DM), obesity, and metabolic syndrome (MetS), NAFLD's prevalence has also escalated, earning the designation as a hepatic component of MetS. The mortality risk associated with NAFLD is notably amplified by the co-occurrence of metabolic derangements, underlining the critical role of metabolic factors in its pathogenesis2. Given the intricate connection between metabolic dysfunction and the onset of fatty liver diseases, there has been a call for a revised diagnostic paradigm. The existing definition of NAFLD is deemed insufficient as it fails to incorporate a set of "positive" criteria that capture the essential metabolic features3. Consequently, a new term, metabolic associated fatty liver disease (MAFLD), has been proposed by a consortium of international experts, signifying a shift from the traditional NAFLD nomenclature to better reflect the current scientific understanding4.
The portrayal of NAFLD merely as a manifestation of MetS is subject to ongoing debate. Epidemiological findings reveal that MetS does not invariably lead to NAFLD, and the linkage between hepatic steatosis and atherosclerotic cardiovascular disease (ASCVD) persists even after controlling for MetS risk factors5,6,7. This observation alludes to the potential of fatty liver as a distinct marker for ASCVD independent of other metabolic dysfunctions. The role of vitamin D extends beyond its well-established influence on bone metabolism, exerting broad effects on multiple organ systems8. Recently, vitamin D's protective potential against NAFLD development and its progression has attracted significant research interest, fueled by indications that vitamin D may modulate the various phases of NAFLD progression, including its regulatory impact on metabolism, and anti-steatotic, anti-fibrotic, and anti-inflammatory effects8,9. Observations from earlier studies suggest that vitamin D deficiency could play a role in the etiology of NAFLD10,11. However, the correlation between vitamin D status and fatty liver disease in the context of metabolic dysfunction is not well-established. This study aims to delineate the relationship between serum vitamin D levels and the incidence of MAFLD.
Results
Baseline characteristics by gender
Table 1 displays the demographic and clinical baseline characteristics of the participants. The cohort predominantly consisted of men (72.61%), reflecting the occupational demographics of the region. Notable gender disparities were observed in MAFLD incidence (53.27% in men vs. 12.96% in women, P < 0.001) and baseline characteristics. Given alcohol's established association with liver disease and the observed gender differences in alcohol consumption, the analysis was conducted separately for 16,320 men and 6156 women.
Men were significantly younger than women (38.77 ± 10.53 years in men vs. 41.49 ± 12.79 years in women, P < 0.001). The prevalence of current smoking was substantially higher in men (45.12% vs. 4.03% in women, P = 0.001). The proportion of heavy drinkers was also significantly higher in men (26.12% vs. 9.45% in women, P < 0.001), as was the engagement in physically active lifestyles (8.46% in men vs. 6.16% in women, P < 0.001). Men had significantly higher rates of hypertension (33.45% vs. 24.35% in women, P < 0.001) and diabetes (9.47% vs. 7.60% in women, P < 0.001). Additionally, men presented with higher levels of total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), body mass index (BMI), waist circumference (WC), fasting plasma glucose (FPG), hemoglobin A1c (HbA1c), and homeostatic model assessment for insulin resistance (HOMA-IR) scores, alongside lower high-density lipoprotein cholesterol (HDL-C) levels. Women had significantly lower serum vitamin D levels (18.23 ± 7.39 ng/mL in men vs. 16.67 ± 9.06 ng/mL in women, P < 0.001), correlating with a higher prevalence of vitamin D insufficiency (65.07% in men vs. 73.05% in women, P < 0.001).
Baseline characteristics based on vitamin D status
Table 2 details the baseline characteristics of participants stratified by vitamin D status. Among the 16,320 men and 6156 women who met the inclusion criteria, 5700 men and 1659 women were categorized into the vitamin D sufficiency group, while 10,620 men and 4497 women comprised the insufficiency group.
In the vitamin D sufficiency group, men were significantly older compared to those in the insufficiency group (41.98 ± 11.33 vs. 37.05 ± 9.64 years; P < 0.001). The proportion of never-smokers was higher in the sufficiency group (25.36% vs. 30.81% in the insufficiency group; P < 0.001). Heavy drinking was more prevalent among sufficient men (30.05% vs. 24.06% in the insufficiency group; P < 0.001), as was engagement in physical activities (10.80% vs. 7.26%; P < 0.001). There were also significantly higher incidences of hypertension (38.21% vs. 30.89% in the insufficiency group; P < 0.001) and diabetes (11.14% vs. 8.58%; P < 0.001). Men in the sufficiency group had higher levels of LDL-C, HDL-C, AST, GGT, FPG, and HbA1c but lower BMI, WC, TG, ALT, and HOMA-IR scores. A higher incidence of MAFLD was observed in the insufficiency group compared to the sufficiency group (54.05% vs. 51.82%; P = 0.007), and viral hepatitis was more prevalent among the sufficient (4.34% vs. 3.19%; P < 0.001).
For women, those in the vitamin D sufficiency group were significantly older than their insufficient counterparts (48.77 ± 13.15 vs. 38.81 ± 11.55 years; P < 0.001) and had a higher proportion of never-smokers (95.11% vs. 90.69%; P < 0.001). Vitamin D insufficient women were more likely to abstain from alcohol (7.19% vs. 3.84%; P = 0.001) and were less physically active (86.85% vs. 84.56%; P = 0.019). Hypertension (35.26% vs. 20.32%; P < 0.001) and diabetes (11.21% vs. 6.27%; P < 0.001) were more frequent in the sufficiency group. Additionally, women with sufficient vitamin D levels had higher TC, HDL-C, LDL-C, AST, ALT, GGT, FPG, HbA1c levels but lower BMI and WC. The MAFLD incidence was greater in the insufficiency group (13.74% vs. 10.85%; P = 0.003). The average serum vitamin D levels were 26.23 ± 5.88 ng/mL for sufficient men and 13.94 ± 3.56 ng/mL for insufficient men; for women, these levels were 28.47 ± 8.47 ng/mL and 12.32 ± 3.96 ng/mL, respectively. Contrary to men, no significant difference in the prevalence of viral hepatitis was observed between the sufficiency and insufficiency groups among women.
Comparison of characteristics in individuals with and without MAFLD
Characteristics of the study population stratified by the presence of MAFLD are presented in Table 3. Among men, MAFLD was significantly more common in younger individuals, smokers, drinkers, and those less physically active. They exhibited significantly higher BMI, WC, SBP, DBP, FPG, HbA1c, and levels of all lipid profiles except HDL-C, as well as AST, ALT, and GGT. The MAFLD group had a lower mean serum vitamin D level (18.07 ± 7.00 ng/mL) compared to the non-MAFLD group (18.41 ± 7.81 ng/mL, P = 0.003), which coincided with a higher vitamin D insufficiency rate (66.02% vs. 63.99%, P = 0.007). In women, the mean serum vitamin D level was also significantly lower in the MAFLD group (15.93 ± 8.02 ng/mL) than in the non-MAFLD group (16.78 ± 9.21 ng/mL, P = 0.014), and a higher rate of vitamin D insufficiency was observed (77.44% vs. 72.40%, P = 0.003).
Comparison of characteristics according to vitamin D status in MAFLD group
Table 4 compares the characteristics of MAFLD subjects based on vitamin D status. Men with sufficient vitamin D had mean serum levels of 25.85 ± 5.31 ng/mL, while those with insufficiency had levels of 14.07 ± 3.55 ng/mL. The sufficiency group was significantly older and had higher rates of smoking, drinking, physical activity, hypertension, and diabetes. This group also had lower BMI, WC, TC, and TG levels, but higher HDL-C, AST, and GGT levels. Women with sufficient vitamin D levels (27.48 ± 7.67 ng/mL) compared to those with insufficiency (12.57 ± 3.98 ng/mL) were older, more likely to be non-smokers, and had a higher prevalence of hypertension. Unlike men, the sufficiency group in women did not have significant differences in alcohol consumption and physical activity when compared to the insufficiency group, though the smoking rate was significantly lower.
Association between MAFLD and vitamin D status in subjects with metabolic dysfunction
Binary logistic regression was conducted to assess the relationship between vitamin D status and MAFLD incidence, with findings detailed in Table 5. The analysis revealed a significant association between vitamin D insufficiency and MAFLD incidence, with men showing an odds ratio (OR) of 1.09 (95% CI: 1.03–1.17, P = 0.007) and women an OR of 1.31 (95% CI: 1.10–1.56, P = 0.003). After adjusting for potential confounders, the association persisted; in men, the adjusted OR (aOR) ranged from 1.06 (95% CI: 0.99–1.13, P = 0.099) to 1.31 (95% CI: 1.22–1.41, P < 0.001), and in women from 1.28 (95% CI: 1.06–1.54, P = 0.010) to 1.53 (95% CI: 1.20–1.96, P = 0.001) across various models. The strongest associations were noted in the fully adjusted model (Model 4), which included age, sex, time of health checkup, alcohol intake, physical activity, and smoking status (men: aOR = 1.32, 95% CI: 1.22–1.43, P < 0.001; women: aOR = 1.53, 95% CI: 1.18–1.98, P = 0.001). Building on our initial findings, we further refined our analysis to include BMI adjustments. The newly included Model 5, stratified by a BMI threshold of 23, maintains the significant association between vitamin D insufficiency and the incidence of MAFLD. Specifically, this BMI-adjusted model revealed that men with vitamin D insufficiency had an odds ratio (OR) of 1.43 (95% CI: 1.31–1.56, P < 0.001), and women had an OR of 1.34 (95% CI: 1.02–1.76, P = 0.034). These results reaffirm the strength of the association across various BMI categories.
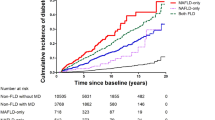
Subgroup analyses stratifying by clinically relevant factors
Subgroup analyses were performed to examine the consistency of the association between vitamin D insufficiency and MAFLD across different clinical contexts, adjusting for all confounders in Model 4 as shown in Fig. 1. In men, vitamin D insufficiency was consistently associated with increased MAFLD incidence, irrespective of hepatitis, diabetes, being overweight/obese, or metabolic dysregulation in normal-weight individuals. Notably, in the context of hepatitis, vitamin D insufficiency significantly raised the incidence of MAFLD (OR = 1.97, 95% CI: 1.26–3.08, P = 0.003). Alcohol consumption also influenced the association, with vitamin D insufficiency correlating with a higher incidence of MAFLD in those who consume alcohol. Conversely, in women, the relationship between vitamin D insufficiency and MAFLD was less pronounced in subgroups with chronic hepatitis, diabetes, or metabolic dysregulation in normal-weight subjects. No association was found in women with or without overweight/obesity. However, vitamin D insufficiency was linked to a higher incidence of MAFLD in alcohol consumers, similar to men, with a pronounced association in heavy drinkers (OR = 4.37, 95% CI: 1.79–10.67, P = 0.001).
Sensitivity analysis
A sensitivity analysis was conducted to evaluate the robustness of the association between vitamin D insufficiency and MAFLD. This study initially defined fatty liver based on a Fatty Liver Index (FLI) of 60 or higher, excluding individuals with an FLI between 30 to < 60. The sensitivity analysis utilized an alternative FLI threshold of ≥ 30 for a fatty liver diagnosis, as commonly adopted in Korean studies12,13. After classifying fatty liver with this lower cut-off and adjusting for all confounders outlined in Model 4 (details provided in Supplementary Table 1), the association of vitamin D insufficiency with MAFLD remained significant. In men, the adjusted odds ratio (aOR) was 1.25 (95% CI: 1.17–1.34, P < 0.001), and in women, it was 1.39 (95% CI: 1.18–1.64, P < 0.001), confirming that vitamin D insufficiency is a significant predictor of MAFLD regardless of the FLI threshold used.
Discussion
In our population-based study, we explored the relationship between serum vitamin D levels and MAFLD incidence. The findings indicate that vitamin D insufficiency is associated with increased likelihood of MAFLD in individuals with metabolic dysfunction. Our data suggest that metabolic dysfunction may predispose subjects to MAFLD when accompanied by insufficient vitamin D levels. This study also found that subjects with MAFLD had notably lower mean serum vitamin D levels than those without the disease, leading to a significantly higher prevalence of vitamin D insufficiency in both men and women with MAFLD.
Vitamin D, primarily synthesized in the liver, acts as an important secosteroid hormone with pleiotropic effects14. Beyond its role in calcium and bone homeostasis, vitamin D is implicated in the regulation of cell proliferation and differentiation15, with relevance to the pathogenesis of chronic liver disease16. Evidence increasingly suggests a link, potentially causative, between vitamin D deficiency and NAFLD17,18,19. Consequently, vitamin D's anti-lipogenic, antifibrotic, and anti-inflammatory properties have been highlighted20. However, the debate persists over the significance of vitamin D status in NAFLD progression. Targher et al.'s study, the first to examine this relationship through biopsy-proven NAFLD, found lower vitamin D levels in NAFLD subjects compared to controls and an association between vitamin D status and NAFLD severity, with NASH patients exhibiting lower levels than those with isolated fatty liver21. Pacifico et al. conducted a systematic review of 45 studies, finding an inverse relationship between vitamin D status and NAFLD in over half the studies21. These findings align with our observations, which also demonstrated common vitamin D insufficiency in MAFLD subjects. Contrarily, Jaruvongvanich et al.'s meta-analysis did not find a significant correlation between serum vitamin D levels and NAFLD severity as indicated by NAFLD activity scores (NAS) and fibrosis stages22.
MetS is often viewed as a pivotal factor in NAFLD development. Several studies have correlated low serum vitamin D levels with MetS features23,24. Animal research further suggests that deficiency in hepatic vitamin D receptors, which regulate intra-hepatic lipid accumulation, or vitamin D insufficiency itself, impairs insulin secretion from pancreatic beta cells, highlighting vitamin D's beneficial role in diabetes and insulin resistance25. While the full NAFLD pathogenesis remains elusive, insulin resistance is considered a core mechanism in hepatic steatosis. The MAFLD acronym emphasizes metabolic factors in patients with hepatic steatosis. There is evidence suggesting that vitamin D insufficiency is directly associated with insulin resistance, especially in overweight and obese individuals, increasing MAFLD risk26. Current evidence supports vitamin D's potential role in MAFLD prevention by ameliorating aspects of MetS.
Yet, the extent to which vitamin D mitigates fatty liver development through MetS improvement alone is under scrutiny. With the evolution of NAFLD understanding from the "two-hit" to the "multiple-hits" hypothesis, FLD is seen as the result of several concurrent processes27. Vitamin D impacts these pathways non-classically, including hormonal, immune, and cellular differentiation mechanisms28,29,30. Our study delves into vitamin D's relationship with fatty liver in individuals with preexisting metabolic dysfunction. The observed benefits of vitamin D could stem from improvements in insulin resistance, elevation of adipokines like adiponectin, and reduction of hepatic inflammation. MAFLD in obesity is determined by changes in AT due to excessive caloric intake and weight gain31. Clinical trials and experiments indicate vitamin D treatment mitigates oxidative stress and local pro-inflammatory cytokine concentrations, such as tumor necrosis factor-ɑ (TNF-ɑ) and monocyte chemoattractant protein-1 (MCP-1)32,33. Vitamin D's systemic and tissue-specific anti-inflammatory properties are well documented34. In MAFLD rat models, active vitamin D treatment reduced liver inflammation and oxidative stress by inhibiting the p53-p21 pathway and associated cell senescence. Human studies have shown inverse correlations between VDR expression and the severity of steatosis and lobular inflammation30. Conversely, vitamin D insufficiency may exacerbate hepatic inflammation.
Another significant clinical observation is the more pronounced association between vitamin D insufficiency and MAFLD as vitamin D levels increase, suggesting a concentration-dependent preventive effect of vitamin D against MAFLD development. However, this inference warrants caution. Our findings also suggest that women with vitamin D insufficiency have higher odds for MAFLD incidence compared to men, supporting Bennouar's report of NAFLD association with vitamin D insufficiency in women irrespective of weight or metabolic profile34. Gender-specific differences in FLD development could be due to variations in circulating sex hormones and binding globulins35. Thus, the interplay of low vitamin D levels with high estradiol and low SHBG may contribute to the higher incidence of MAFLD in women. Additionally, gender differences emerged in the subgroup analyses, with consistent associations between vitamin D insufficiency and MAFLD in men across most subgroups, but not in women. Specifically, no link was found in women with hepatitis, diabetes, metabolic dysregulation, or those abstaining from alcohol. However, among heavy-drinking women, vitamin D had a more significant impact on MAFLD incidence than in men. Further research is needed to clarify these observations.
The conclusions of our study must be approached with circumspection due to several methodological limitations. Firstly, the cross-sectional design does not allow for definitive inferences regarding causality and may be prone to reverse causation between vitamin D insufficiency and MAFLD. Secondly, our study's reliance on the FLI as the sole predictor for hepatic steatosis was a pragmatic decision influenced by the large scale of our cohort and the standardized procedures of the health examinations undertaken. The FLI is an established indirect method for estimating liver fat content within large population groups. However, we recognize it is not a direct imaging method such as ultrasound, Fibroscan, or advanced techniques like magnetic resonance imaging derived proton density fat fraction (MRI-PDFF), which may offer more specificity. Although these diagnostic tools were not utilized, potentially affecting the precision of our fatty liver disease prevalence estimates, the FLI remains a vital tool for epidemiological insights, particularly in settings where direct imaging is impractical. Despite its limitations in detailing the complexities and differentiating the stages of NAFLD and NASH, the FLI is widely accepted for its non-invasive assessment capabilities.
Thirdly, while our study provides valuable insights into the relationship between vitamin D levels and the incidence of MAFLD, we must acknowledge that dietary patterns, which were not captured in our dataset, represent a potential confounding factor. Total calorie intake and diet composition are known to influence both vitamin D status and hepatic outcomes. The absence of this data limits our ability to fully account for dietary influences and necessitates cautious interpretation of the associations reported herein. Future investigations would benefit from incorporating detailed dietary assessments to delineate the independent effects of vitamin D from those of dietary habits on MAFLD outcomes. This approach would undoubtedly contribute to a more comprehensive understanding of the multifactorial nature of MAFLD and its potential nutritional determinants. The modest associations reported here between vitamin D insufficiency and MAFLD suggest that the role of vitamin D might be more complex and potentially moderated by a variety of factors, including but not limited to, nutritional intake, lifestyle, and genetic variability. This complexity is further compounded by the absence of direct imaging techniques in our study, a limitation which we have sought to address through careful interpretation and the consideration of additional confounders. Fourthly, being a single-center study, there's a possibility that the baseline characteristics of our subjects, who were selected based on routine health examinations, may not be representative of the broader population. This limits the extent to which our findings can be generalized. Lastly, the threshold we set for vitamin D insufficiency, at less than 20 ng/mL, could be contentious given the ongoing clinical debate and lack of a standardized definition for optimal vitamin D levels.
Conclusion
Our comprehensive study has identified a significant relationship between vitamin D insufficiency and the incidence of MAFLD in individuals exhibiting metabolic dysfunction. Despite the inherent limitations of a cross-sectional and single-center design, these preliminary findings are noteworthy, suggesting an association that merits deeper investigation. Future studies, ideally featuring a more varied and longitudinal participant group, are essential to corroborate our findings and to determine the role of vitamin D more definitively in MAFLD pathogenesis.
Methods
Study design and population
Our research included men and women aged 19 years and above who attended the Health Promotion Center at Samsung Changwon Hospital, Korea, for routine health examinations from January 2013 to July 2022, totaling 221,161 participants. For those with multiple health check-ups within this timeframe, the initial visit was designated as the baseline date. From this population, we excluded 148,793 individuals due to incomplete serum vitamin D measurements or missing FLI data, leaving 72,368 individuals suitable for fatty liver and vitamin D status assessment. A further exclusion of 37,910 subjects who did not fulfill the criteria for any of three metabolic conditions—diabetes mellitus, overweight/obesity, or metabolic dysregulation in normal weight—was performed to focus on subjects with metabolic dysfunction. Additionally, 35 individuals with a history of hepatic malignancy were also excluded from the study. To further refine our cohort, we excluded 11,982 subjects with an FLI between 30 to < 60, where the presence of fatty liver was ambiguous. Consequently, our final analytical cohort consisted of 22,476 participants who had evidence of metabolic dysfunction at baseline and available serum vitamin D status. Within this cohort, subjects with an FLI < 30 were categorized into the non-MAFLD group, while those with an FLI ≥ 60 were placed in the MAFLD group. Each group was then subdivided based on vitamin D levels into sufficiency and insufficiency subgroups for detailed analysis, as depicted in Fig. 2. The Institutional Review Board of Samsung Changwon Hospital (SCMC 2022-10-003) granted ethical approval for this study, which was conducted in line with the Declaration of Helsinki's guidelines. Given the study's retrospective nature, involving the analysis of pre-existing administrative and clinical data, the Institutional Review Board waived the requirement for informed consent from participants.
Variables and measurements
For the anthropometric and physiological measurements, an InBody 770 body composition analyzer (Inbody Inc., Seoul, Korea) was employed, recording height, body weight, and WC. BMI was determined using the formula: weight in kilograms divided by the square of height in meters. Blood pressure was measured after a five-minute seated rest using an automated oscillometric sphygmomanometer, noting both systolic (SBP) and diastolic blood pressure (DBP). The self-reported health behavior questionnaire provided data on alcohol consumption, smoking habits, and physical activity. Alcohol consumption was categorized into never, moderate (less than 30 g/day for men and less than 20 g/day for women), or heavy (30 g/day or more for men and 20 g/day or more for women). Smoking status was classified as never, former, or current. Physical activity was divided into three tiers based on the International Physical Activity Questionnaires (IPAQ): inactive, moderately active, and health-enhancing physical activity (HEPA) active, with specific criteria for each category based on vigorous activity durations, moderate-intensity activities, walking, and MET-minutes per week36.
Laboratory measurements were conducted on blood samples collected after a minimum eight-hour overnight fast. The analysis included FPG, TC, LDL-C, TG, HDL-C, AST, ALT, and GGT. Vitamin D status was evaluated using a serum 25-OH-vitamin D3 Total Assay (Cobas e 602, Roche Diagnostics). HbA1c levels were measured by an HLC-723 G11 analyzer (Tosho, Inc). Additionally, serum insulin was assayed with commercial kits on an electrochemiluminescence device (Cobas e 602, Roche Diagnostics). Insulin resistance was calculated using the HOMA formula: HOMA-IR = fasting insulin (µIU/mL) * fasting glucose (mmol/L)/22.537.
Diagnostic criteria and definition of groups
Metabolic dysfunction within the study cohort was determined by the presence of one or more of the following criteria: (1) overweight or obesity, defined as a BMI of 23 kg/m2 or greater, following the Asia–Pacific guidelines; (2) T2DM; or (3) metabolic dysregulation characterized by at least two out of seven metabolic anomalies: WC ≥ 90 cm for men or ≥ 80 cm for women, prediabetes (HbA1c levels between 5.7% and 6.4%, FPG between 100 and 125 mg/dL, or 2-h post-load glucose levels between 140 and 199 mg/dL), hypertension or use of antihypertensive medications (blood pressure ≥ 130/85 mmHg), reduced high-density lipoprotein cholesterol (HDL-C < 40 mg/dL for men and < 50 mg/dL for women), elevated triglycerides (TG ≥ 150 mg/dL or on specific medication), insulin resistance as indicated by a HOMA-IR score ≥ 2.5, and elevated high-sensitivity C-reactive protein (hs-CRP > 2 mg/L).
FLI, a validated surrogate marker of hepatic steatosis, was utilized for predicting fatty liver disease (FLD). The FLI algorithm incorporates variables including BMI, TG, GGT levels, and WC, calculated as follows: FLI = ey / (1 + ey) * 100, y = 0.953 * loge (TG) + 0.139 * BMI + 0.718 * loge (GGT) + 0.053 * WC − 15.745. An FLI score below 30 excludes, scores from 30 to 60 are inconclusive for, and scores above 60 confirm the presence of fatty liver38.
Participants exhibiting metabolic dysfunction were dichotomized into the MAFLD and non-MAFLD groups based on their baseline FLI scores. Individuals with an FLI ≥ 60 were categorized under the MAFLD group, whereas those with an FLI < 30 were allocated to the non-MAFLD group. Subsequent classification into vitamin D sufficiency and insufficiency was based on serum levels, with the threshold set at 20 ng/mL, in alignment with the Food and Nutrition Board of the Institute of Medicine's definition of vitamin D insufficiency39.
Statistical analysis
We utilized STATA software, version 14.0 (StataCorp LLC, College Station, Texas, USA), and R, version 3.4.4 (R Foundation for Statistical Computing, Vienna, Austria; URL: http://www.R-project.org/), to conduct our statistical analyses. To compare baseline characteristics between the groups with sufficient and insufficient vitamin D levels, we employed the independent t-test for continuous variables and the Chi-square test for categorical variables. Data are reported as mean ± standard deviation (SD) for continuous measures and as count and percentage (n, %) for categorical measures. The relationship between vitamin D insufficiency and the incidence of fatty liver disease in individuals with metabolic dysfunction was assessed using binary logistic regression models. To control for baseline confounders, we applied a series of models with incremental adjustments. Model 1 was adjusted for age, and Model 2 further included the year and quarter of the health checkup. Model 3 was expanded to adjust for alcohol consumption levels (never, moderate, or heavy). The final model, Model 4, included adjustments for physical activity levels (inactive, moderately active, or HEPA active) and smoking status (never, former, or current). Subgroup analyses were performed to investigate the impact of vitamin D status on the incidence of MAFLD within specific cohorts. Sensitivity analyses were also conducted using a lower FLI cut-off of 30, in recognition of studies suggesting a more appropriate threshold for the Korean population compared to Western cohorts. All statistical tests were two-sided, and a P value of less than 0.05 was considered to indicate statistical significance.
Data availability
The datasets generated and analyzed during this study are not publicly available due to restrictions pertaining to patient consent and institutional guidelines for data sharing. However, the datasets are available from the corresponding author upon reasonable request.
References
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84. https://doi.org/10.1002/hep.28431 (2016).
Stepanova, M., Rafiq, N. & Younossi, Z. M. Components of metabolic syndrome are independent predictors of mortality in patients with chronic liver disease: A population-based study. Gut 59, 1410–1415. https://doi.org/10.1136/gut.2010.213553 (2010).
Eslam, M., Sanyal, A. J., George, J. & International Consensus, P. MAFLD: A consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 158, 1999–2014. https://doi.org/10.1053/j.gastro.2019.11.312 (2020).
Eslam, M. et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 73, 202–209. https://doi.org/10.1016/j.jhep.2020.03.039 (2020).
Villanova, N. et al. Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology 42, 473–480. https://doi.org/10.1002/hep.20781 (2005).
Völzke, H. et al. Hepatic steatosis is associated with an increased risk of carotid atherosclerosis. World J. Gastroenterol. 11, 1848–1853. https://doi.org/10.3748/wjg.v11.i12.1848 (2005).
Vanni, E. et al. From the metabolic syndrome to NAFLD or vice versa?. Dig. Liver Dis. 42, 320–330. https://doi.org/10.1016/j.dld.2010.01.016 (2010).
Eliades, M. & Spyrou, E. Vitamin D: A new player in non-alcoholic fatty liver disease?. World J. Gastroenterol. 21, 1718–1727. https://doi.org/10.3748/wjg.v21.i6.1718 (2015).
Barchetta, I., Cimini, F. A. & Cavallo, M. G. Vitamin D supplementation and non-alcoholic fatty liver disease: Present and future. Nutrients 9, 1015. https://doi.org/10.3390/nu9091015 (2017).
Liu, S. et al. Association between Vitamin D status and non-alcoholic fatty liver disease: A population-based study. J. Nutr. Sci. Vitaminol. 65, 303–308. https://doi.org/10.3177/jnsv.65.303 (2019).
Zhu, S. et al. The level of vitamin D in children and adolescents with nonalcoholic fatty liver disease: A meta-analysis. Biomed. Res. Int. 2019, 7643542. https://doi.org/10.1155/2019/7643542 (2019).
Lee, H., Lee, H. W., Kim, S. U. & Chang Kim, H. Metabolic dysfunction-associated fatty liver disease increases colon cancer risk: A nationwide cohort study. Clin. Transl. Gastroenterol. 13, e00435. https://doi.org/10.14309/ctg.0000000000000435 (2022).
Lee, H., Lee, Y. H., Kim, S. U. & Kim, H. C. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: A nationwide cohort study. Clin. Gastroenterol. Hepatol. 19, 2138–2147. https://doi.org/10.1016/j.cgh.2020.12.022 (2021).
Cesari, M., Incalzi, R. A., Zamboni, V. & Pahor, M. Vitamin D hormone: A multitude of actions potentially influencing the physical function decline in older persons. Geriatr. Gerontol. Int. 11, 133–142. https://doi.org/10.1111/j.1447-0594.2010.00668.x (2011).
Khammissa, R. A. G. et al. The biological activities of vitamin D and its receptor in relation to calcium and bone homeostasis, cancer, immune and cardiovascular systems, skin biology, and oral health. Biomed. Res. Int. 2018, 9276380. https://doi.org/10.1155/2018/9276380 (2018).
Arteh, J., Narra, S. & Nair, S. Prevalence of vitamin D deficiency in chronic liver disease. Digest Dis. Sci. 55, 2624–2628. https://doi.org/10.1007/s10620-009-1069-9 (2010).
Kitson, M. T. & Roberts, S. K. D-livering the message: The importance of vitamin D status in chronic liver disease. J. Hepatol. 57, 897–909. https://doi.org/10.1016/j.jhep.2012.04.033 (2012).
Dasarathy, J. et al. Hypovitaminosis D is associated with increased whole body fat mass and greater severity of non-alcoholic fatty liver disease. Liver Int. 34, e118–e127. https://doi.org/10.1111/liv.12312 (2014).
Seo, J. A. et al. Low vitamin D status is associated with nonalcoholic fatty liver disease independent of visceral obesity in Korean adults. PLoS ONE 8, e75197. https://doi.org/10.1371/journal.pone.0075197 (2013).
Sharifi, N., Amani, R., Hajiani, E. & Cheraghian, B. Does vitamin D improve liver enzymes, oxidative stress, and inflammatory biomarkers in adults with non-alcoholic fatty liver disease? A randomized clinical trial. Endocrine 47, 70–80. https://doi.org/10.1007/s12020-014-0336-5 (2014).
Pacifico, L., Osborn, J. F., Bonci, E., Pierimarchi, P. & Chiesa, C. Association between vitamin D levels and nonalcoholic fatty liver disease: Potential confounding variables. Mini-Rev. Med. Chem. 19, 310–332. https://doi.org/10.2174/1389557518666181025153712 (2019).
Jaruvongvanich, V., Ahuja, W., Sanguankeo, A., Wijarnpreecha, K. & Upala, S. Vitamin D and histologic severity of nonalcoholic fatty liver disease: A systematic review and meta-analysis. Dig. Liver Dis. 49, 618–622. https://doi.org/10.1016/j.dld.2017.02.003 (2017).
Pittas, A. G., Lau, J., Hu, F. B. & Dawson-Hughes, B. The role of vitamin D and calcium in type 2 diabetes. A Systematic review and meta-analysis. J. Clin. Endocrinol. Metabolism 92, 2017–2029. https://doi.org/10.1210/jc.2007-0298 (2007).
Ju, S. Y., Jeong, H. S. & Kim, D. H. Blood vitamin D status and metabolic syndrome in the general adult population: A dose–response meta-analysis. J. Clin. Endocrinol. Metab. 99, 1053–1063. https://doi.org/10.1210/jc.2013-3577 (2014).
Zeitz, U. et al. Impaired insulin secretory capacity in mice lacking a functional vitamin D receptor. FASEB J. 17, 1–14. https://doi.org/10.1096/fj.02-0424fje (2003).
Barchetta, I. et al. Hypovitaminosis D is independently associated with metabolic syndrome in obese patients. PLoS ONE 8, e68689. https://doi.org/10.1371/journal.pone.0068689 (2013).
Tilg, H. & Moschen, A. R. Evolution of inflammation in nonalcoholic fatty liver disease: The multiple parallel hits hypothesis. Hepatology 52, 1836–1846. https://doi.org/10.1002/hep.24001 (2010).
Barchetta, I. et al. Liver vitamin D receptor, CYP2R1, and CYP27A1 expression: Relationship with liver histology and vitamin D3 levels in patients with nonalcoholic steatohepatitis or hepatitis C virus. Hepatology 56, 2180–2187. https://doi.org/10.1002/hep.25930 (2012).
Roth, C. L. et al. Vitamin D deficiency in obese rats exacerbates nonalcoholic fatty liver disease and increases hepatic resistin and toll-like receptor activation. Hepatology 55, 1103–1111. https://doi.org/10.1002/hep.24737 (2012).
Vaidya, A., Williams, J. S. & Forman, J. P. The independent association between 25-hydroxyvitamin D and adiponectin and its relation with BMI in two large cohorts: The NHS and the HPFS. Obesity 20, 186–191. https://doi.org/10.1038/oby.2011.210 (2012).
Tilg, H., Adolph, T. E. & Moschen, A. R. Multiple parallel hits hypothesis in nonalcoholic fatty liver disease: Revisited after A decade. Hepatology 73, 833–842. https://doi.org/10.1002/hep.31518 (2021).
Farhangi, M. A., Mesgari-Abbasi, M., Hajiluian, G., Nameni, G. & Shahabi, P. Adipose tissue inflammation and oxidative stress: The ameliorative effects of vitamin D. Inflammation 40, 1688–1697. https://doi.org/10.1007/s10753-017-0610-9 (2017).
Ionica, M. et al. Vitamin D alleviates oxidative stress in adipose tissue and mesenteric vessels from obese patients with subclinical inflammation1. Can. J. Physiol. Pharmacol. 98, 85–92. https://doi.org/10.1139/cjpp-2019-0340 (2020).
Ma, M., Long, Q., Chen, F., Zhang, T. & Wang, W. Active vitamin D impedes the progression of non-alcoholic fatty liver disease by inhibiting cell senescence in a rat model. Clin. Res. Hepatol. Gas 44, 513–523. https://doi.org/10.1016/j.clinre.2019.10.007 (2020).
Lazo, M. et al. Association between endogenous sex hormones and liver fat in a multiethnic study of atherosclerosis. Clin. Gastroenterol. Hepatol. 13, 1686–1693. https://doi.org/10.1016/j.cgh.2014.12.033 (2015).
Mehta, S. P., Jarvis, A., Standifer, D. & Warnimont, C. International physical activity questionnaire. Crit. Rev. Phys. Rehab. Med. 30, 125–127. https://doi.org/10.1615/CritRevPhysRehabilMed.2018026180 (2018).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419. https://doi.org/10.1007/BF00280883 (1985).
Bedogni, G. et al. The Fatty Liver Index: A simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 6, 33. https://doi.org/10.1186/1471-230X-6-33 (2006).
Bouillon, R. & Carmeliet, G. Vitamin D insufficiency: Definition, diagnosis and management. Best Pract. Res. Clin. Endocrinol. Metab. 32, 669–684. https://doi.org/10.1016/j.beem.2018.09.014 (2018).
Author information
Authors and Affiliations
Contributions
Statistical analysis and writing the draft manuscript: S.L.; Data collection and study design: S.L.; Data collection, statistical analysis: M.H.J.; Study design, and critical revision of the manuscript: J.-H.Y.; All authors approved the final submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, Sb., Jin, M.H. & Yoon, JH. The contribution of vitamin D insufficiency to the onset of steatotic liver disease among individuals with metabolic dysfunction. Sci Rep 14, 6714 (2024). https://doi.org/10.1038/s41598-024-57380-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-57380-9
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.