Abstract
To elucidate the relationship between the interval from cardiopulmonary resuscitation initiation to return of spontaneous circulation (ROSC) and neurologically favourable 1-month survival in order to determine the appropriate duration of basic life support (BLS) without advanced interventions. This population-based cohort study included patients aged ≥ 18 years with 9132 out-of-hospital cardiac arrest of presumed cardiac origin who were bystander-witnessed and had achieved ROSC between 2018 and 2020. Patients were classified into two groups based on the resuscitation methods as the “BLS-only” and the “BLS with administered epinephrine (BLS-AE)” groups. Receiver operating characteristic (ROC) curve analysis indicated that administering BLS for 9 min yielded the best neurologically outcome for patients with a shockable rhythm [sensitivity, 0.42; specificity, 0.27; area under the ROC curve (AUC), 0.60] in the BLS-only group. Contrastingly, for patients with a non-shockable rhythm, performing BLS for 6 min yielded the best neurologically outcome (sensitivity, 0.65; specificity, 0.43; AUC, 0.63). After propensity score matching, multivariate analysis revealed that BLS-only resuscitation [6.44 (5.34–7.77)] was associated with neurologically favourable 1-month survival. This retrospective study revealed that BLS-only intervention had a significant impact in the initial minutes following CPR initiation. Nevertheless, its effectiveness markedly declined thereafter. The optimal duration for effective BLS-only intervention varied depending on the patient's initial rhythm. Consequently, advanced interventions should be administered within the first few minutes to counteract the diminishing effectiveness of BLS-only intervention.
Similar content being viewed by others
Introduction
The survival rate from out-of-hospital cardiac arrests (OHCA) widely varies among countries. High-quality cardiopulmonary resuscitation (CPR) with minimal interruption of chest compressions increases the survival chances of patients with OHCA1. Moreover, maintaining the quality of chest compressions increases the likelihood of achieving a prehospital return of spontaneous circulation (ROSC)2, which is associated with favorable neurological outcomes. A previous study reported a negative correlation between the time of on-scene emergency medical service (EMS) arrival with ROSC achievement and survival3, with the yield of survivors per minute of resuscitation declining after 8 min.
For adult patients in cardiac arrest, epinephrine administration in the early stage and after the third shock is recommended for non-shockable and shockable rhythms, respectively4. Another study showed that administering epinephrine within 10 min after scene arrival was associated with improved survival among patients with OHCA5. However, the required intravenous access and other advanced interventions may negatively impact the quality of chest compressions6. Additionally, simulation studies have suggested that introducing advanced life support can decrease the chest compression fraction7. To address these challenges and maintain CPR quality, a teamwork approach that prioritizes CPR and defibrillation within the first 6–8 min after scene arrival has been shown to improve outcomes in several regions8.
Based on this evidence, it is recommended that EMS personnel focus on providing chest compressions and defibrillation within minutes of scene arrival before initiating advanced interventions to maintain the quality of resuscitation. However, the optimal timing to transition from the basic life support (BLS) phase to the advanced intervention phase, including epinephrine administration, remains unclear. This study aimed to elucidate the relationship between the interval from CPR initiation to ROSC and neurologically favorable 1-month survival to determine the appropriate duration of BLS without advanced interventions.
Methods
Study design
This retrospective, population-based cohort study included patients aged ≥ 18 years with OHCA of presumed cardiac origin who were bystander-witnessed and had achieved ROSC. The study followed all the methods that were performed in accordance with the relevant guidelines and regulations. This study protocol was approved by the Ethics Committee of the Niigata University of Health and Welfare (No. 19068-230602).
Study population and settings
Japan has a population of approximately 127 million people, living in an area of 378,000 km2. As of 2018, Japan had 726 fire headquarters, 1719 fire stations, and 5215 ambulances. Each municipality primarily operates its fire headquarters, which falls under the jurisdiction of the Ministry of Internal Affairs and Communications. Although similar to first responder systems where specifically trained citizens rush to the scene of resuscitation, such systems are generally not present in Japan.
Ambulance crew
In Japan, each ambulance crew comprises three members, with at least one specially trained emergency medical technician (EMT), who is referred to as a "paramedic" in other countries. The EMS comprises a one-tiered ambulance system that includes both BLS and advanced life support. EMTs are not permitted to terminate resuscitation in the field until the patient exhibits obvious post-mortem changes. EMTs are responsible for securing an intravenous route and airway access using a supraglottic airway device in patients with cardiac arrest. Furthermore, specially trained EMTs administer epinephrine and intubate patients in cardiac arrest, as well as administer glucose solution to patients before cardiac arrest or administer fluids to correct shock in patients based on the medical director's direct instructions. The EMTs commence ventilation using a bag-valve-mask device. If ventilation is expected to be difficult with the standard procedure, they liaise with the medical director. Following this, they perform tracheal intubation or use a supraglottic device based on the medical director's instructions. The use of mechanical chest compression devices is at the discretion of each EMT. However, similar to other studies, the specific timing of their use is not reported9 and this information is not included in the database.
Data collection
This nationwide Japanese study included baseline data obtained for 18,889,552 EMS-transported cases and 379,845 OHCA cases handled by the Fire and Disaster Management Agency between January 2018 and December 2020 as the most recent three-year data. These data comprised all core data items recommended by the Utstein-style reporting guidelines10 for cardiac arrests, including sex, age, initial cardiac rhythm, bystander CPR status, resuscitation status by EMTs (BLS-only or BLS with epinephrine administration), date and time of cardiac arrest, level of hospital to which the patient was transported, time series related to EMS activities, ROSC, 1-month survival, and 1-month neurological status.
All patients were followed up for up to 1 month by the fire station staff. Further, 1-month neurological outcomes were assessed using the Cerebral Performance Category (CPC) scale, which ranges from 1 (good cerebral performance) to 5 (brain death)11. CPC categories 1 and 2 (disabled but independent) were defined as indicative of favorable neurological outcomes.
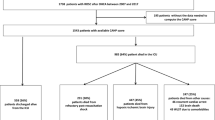
Participants
We analyzed 9132 cases that met the inclusion criteria, involving bystander-witnessed cardiac events in patients aged ≥ 18 years of cardiac origin and without any physician involvement at the scene where ROSC was achieved. Cases that did not meet the inclusion criteria were excluded: cases with inconsistent binding between data sets (n = 5306), cases without successful ROSC (n = 335,642), cases witnessed by EMS staff (n = 5809), cases not witnessed by bystanders (n = 10,521), cases with a non-cardiac origin (n = 9070), cases involving patients aged < 18 years (n = 137), cases with physician involvement at the scene (n = 2716), and cases with missing data or no time records (n = 1512). (Fig. 1).
Outcomes
The primary outcome was the neurologically favorable 1-month survival rate. The secondary outcome was the achievement of early ROSC.
Statistical analysis
Patients were classified into two groups based on the resuscitation methods employed by EMTs as follows: the “BLS-only group” and the “BLS with administered epinephrine (BLS-AE) group”. Since defibrillation is recognized as a component of BLS in the resuscitation guidelines, the defibrillation intervention was included in the 'BLS-only group12.
The chi-square test was used to evaluate categorical variables, whereas the nonparametric Mann–Whitney U test was used for the two group comparisons to evaluate continuous variables. Nonparametric comparisons were due to the confirmation of a non-normal distribution through the use of a histogram for assessing the normality of the continuous variables. Receiver operating characteristic (ROC) curves were used to plot the ability of ROSC to predict outcomes as a function of increasing the pre-ROSC resuscitation time points. First, we performed a multiple logistic regression to identify factors related to the early CPR-to-ROSC interval, which was defined using a cut-off value. Finally, we performed propensity score matching to identify factors associated with the neurologically favorable 1-month survival. The propensity score prediction model comprised the following independent variables using multiple logistic regression analysis: resuscitation method (BLS-only or BLS-AE), age (continuous value), sex (male or female), initial cardiac rhythm (shockable or unshockable), bystander CPR status (provided or not provided), level of hospital to which the patient was transported, day of the week (weekday or weekend), and time of day [night-time (23:00–6:59) or daytime (7:00–22:59)] when the cardiac arrest occurred, the EMS response time (continuous value), time intervals between patients ‘ collapse and CPR initiation by EMS (continuous value), the on-scene time (continuous value) and the transport time (continuous value)13. The EMS response time was defined as the interval duration between the 119 calls and the on-scene arrival of the EMTs. The on-scene time was defined as the interval between the on-scene arrival of EMTs and the departure of the ambulance. Transport time was defined as the interval from ambulance departure to arrival at a hospital. All statistical analyses were performed using JMP Pro® ver.17 for Windows (SAS Institute, Cary, NC, USA). Statistical significance was set at p < 0.05.
Ethics approval and consent to participate
This study was approved by the Niigata University of Health and Welfare Ethics Committee (19068-230602).
Inform consent
Due to the retrospective nature of the study, the need of informed consent was waived off by Niigata University of Health and Welfare Ethics Committee.
Report format
All the methods were performed in accordance with relevant guidelines and regulations.
Results
Characteristics of patients with OHCA
The results are shown in Table 1. Compared with the BLS-AE group, the BLS-only group had a higher proportion of male patients (72.9% vs. 64.8%, p < 0.01), provision of bystander CPR (65.8% vs. 57.1%, p < 0.01), initial shockable rhythms (54.3% vs. 21.3%, p < 0.01), and transport to high-level hospitals (51.7% vs. 45.6%, p < 0.01).
Additionally, compared with the BLS-AE group, the BLS-only group had significantly longer time intervals between patients’ collapse and CPR initiation by EMS [median: 10 min (25–75%: 8–15) vs. 10 min (7–13), p < 0.01], shorter time intervals between EMT-administered CPR and ROSC achievement [6 min (4–11) vs. 15 min (12–19), p < 0.01] and a shorter on-scene time [11 min (8–14) vs. 14 min (11–17), p < 0.01].
Contrastingly, compared with the BLS-only group, the BLS-AE group had a higher proportion of OHCA occurrence at night (17.3% vs. 21.2%, p < 0.01) and older patients [70 years (59–80) vs. 78 years (70–86), p < 0.01]; furthermore, the BLS-AE group had a statistically significantly longer EMS response [8 min (7–10) vs. 9 min (7–11), p < 0.01] and transport times [10 min (7–14) vs. 12 min (8–16), p < 0.01].
ROC curve and cut-off analysis results
The neurologically favorable 1-M survival rates were 50.9% [2468/4845] for the BLS-only group and 6.9% [296/4287] for the BLS-AE group (p < 0.01). The results of the ROC curve and the cut-off analysis are shown in Fig. 2. The ROC curve analysis indicated that administering BLS for 9 min yielded the best neurologically favorable 1-M survival rate for patients with a shockable initial rhythm [sensitivity, 0.42; specificity, 0.27; area under the ROC curve (AUC), 0.60] in the BLS-only group. In contrast, for patients with a non-shockable initial rhythm, performing BLS for 6 min yielded the best neurologically favorable 1-M survival rate (sensitivity, 0.65; specificity, 0.43; AUC, 0.63).
Among patients who received epinephrine, administering BLS for 15 min yielded the best neurologically favorable 1-M survival rate for patients with shockable (sensitivity, 0.52; specificity, 0.30; AUC, 0.64) and non-shockable (sensitivity, 0.61; specificity, 0.31; AUC, 0.68) rhythms.
Comparison of survival curves according to duration of CPR Until ROSC
In the BLS-only group, patients with shockable and non-shockable rhythms showed the highest survival rate (8.7% and 4.7%, respectively) when the duration between CPR and ROSC was 4 min and 3 min, respectively, with the survival rate rapidly decreasing beyond this point (Fig. 3).
Factors associated with early ROSC achievement
Based on the ROC curve analysis results (Fig. 2), we defined early ROSC achievement as within 9 min and 6 min for patients with shockable and non-shockable rhythms, respectively. As shown in Table 2, multivariable analysis indicated that BLS-only resuscitation had the most significant impact on early ROSC achievement in patients with shockable [odds ratio (OR; 95% confidence interval (CI)) 9.95 (8.22–12.03) and non-shockable [28.95 (23.08–36.32)] rhythms.
Factors associated with neurologically favorable outcomes
Supplemental Table 1 shows the characteristics of patients with OHCA after propensity score matching (BLS-only group: n = 2696 and BLS-AE group: n = 2696). As shown in Table 3, after propensity score matching, the multivariable analysis revealed that the neurologically favorable 1-month survival was associated with BLS-only resuscitation [6.44 (5.34–7.77)], patient age [0.95 (0.94–0.96)], male sex [1.40 (1.17–1.66)], bystander CPR [1.54 (1.32–1.82)], initial shockable rhythms [3.00 (2.56–3.53)], transportation to level-3 hospitals [1.46 (1.25–1.70)], collapse-to-CPR interval [0.97 (0.96–0.99)], CPR-to-ROSC interval [0.95 (0.94–0.97)], and on-scene time [0.96 (0.95–0.98)].
Discussion
In this study, our findings indicated that administering BLS for 9 min and 6 min resulted in the best ROSC achievement as outcomes for patients with shockable and non-shockable rhythms, respectively. Moreover, the highest neurologically favorable survival rates were yielded when ROSC was achieved within 4 min and 3 min for patients with shockable and non-shockable rhythms, respectively, in the BLS-only subgroup. Finally, we confirmed that BLS-only resuscitation had the strongest correlation with early ROSC achievement and neurologically favorable outcomes.
The survival rate of patients undergoing resuscitation showed an initial increase followed by a decline after a few minutes3,14,15,16. Another previous study reported that the optimal on-scene time interval for resuscitation was 10 and 8 min in patients with shockable and non-shockable rhythms, respectively14. However, these previous studies notably included patients who underwent BLS with or without epinephrine. In our study, the BLS-AE group had a lower survival rate than the BLS-only group for patients with both shockable and non-shockable rhythms. Other studies have demonstrated diminished benefits of epinephrine if administered more than 10 min after the arrival of the BLS providers, and the combination of BLS and epinephrine administration is associated with the best outcomes; however, the studies did not consider the effect of the initial rhythms17,18. Based on our findings, we believe that an intervention strategy focusing on BLS should only be implemented for approximately the first 5–6 min after making contact with the patient. If ROSC is not achieved within this timeframe, immediate epinephrine administration is considered an effective intervention strategy.
In this study, the BLS-only intervention, used as a reference to BLS-AE, was associated with early ROSC (≤ 9 min and ≤ 6 min for patients with shockable and non-shockable rhythms, respectively). Notably, in the non-shockable cases, especially those treated with BLS-only intervention, compared to BLS-AE, a higher odds ratio for early ROSC achievement was observed. Guidelines for adult patients with cardiac arrest recommend prompt epinephrine administration to those with non-shockable rhythm10. Although it remains unclear at what time in the resuscitation process the decision to transport a patient with ongoing CPR should be made, several studies have recommended minimizing on-scene time and hastening transportation in cases without prehospital ROSC19,20. Therefore, to achieve ROSC, we suggest that the EMS should provide high-quality BLS within a shorter timeframe in non-shockable patients than in shockable patients. If this cannot be accomplished, epinephrine administration and transportation should be promptly initiated.
The results of multivariable analysis after propensity score matching revealed that factors associated with favorable 1-month survival were consistent with those in previous studies, including younger age, male gender, provision of bystander BCPR, patients with a shockable initial rhythm, shorter on-scene time, and transportation to a higher-level hospital21,22,23. An additional insight from this study was the significant impact of nighttime cardiac arrests on survival. However, recent meta-analyses have presented contrasting views. The study focused on non-cardiac origin arrests in individuals aged 18 and above, specifically targeting cases without unwitnessed events, cases where ROSC was achieved, and cases without on-scene physician involvement. The deviation from previous research results could be attributed to the differing study populations.
This study has several limitations. First, the findings may not be universally applicable. The median time interval between CPR initiation and epinephrine administration was 11 min, which was longer than the recommended guidelines in Japan10 and other regions. This suggests that instances involving the BLS-AE group encompass situations in which patients did not respond to achieve ROSC with BLS only. Indeed, the BLS-AE group had several unfavorable factors compared to the BLS-only group, including older patient age, lower frequency of BCPR provision, longer EMS response times, and a lower rate of shockable initial rhythm. If a similar investigation were conducted in regions where the time to drug administration initiation is shorter, it could potentially yield different results.
Second, the level of hospital to which patients are transported varies depending on the region and EMS protocols. Furthermore, the variations in emergency medical systems and healthcare levels pose an additional potential obstacle to generalizability. Furthermore, our study did not delve into the treatment procedures that patients experienced post-hospital admission. There is a possibility of yielding different results if these aspects were included, deviating from the conclusions drawn in this study.
Third, due to the retrospective nature of the present study, analyzing the quality of chest compressions was not feasible with our available data. Consequently, it remains unclear how the quality of chest compressions may have influenced the outcomes between the BLS-only group and the BLS-AE group. This aspect requires validation through prospective studies.
Lastly, based on the results of the ROC curve analysis, the highest survival rates for patients with shockable and non-shockable rhythms were observed when the time from CPR to ROSC was 4 min and 3 min, respectively. However, the AUC for each was lower than expected (0.6). It might be necessary to narrow down the cases to draw optimal ROC curves that enhance the survival rates for each patient.
Conclusion
This retrospective study revealed that BLS-only intervention had a significant impact in the initial minutes following CPR initiation. Nevertheless, its effectiveness markedly declined thereafter. The optimal duration for effective BLS-only intervention varied depending on the patient's initial rhythm. Consequently, advanced interventions should be administered within the first few minutes to counteract the diminishing effectiveness of BLS-only intervention.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bobrow, B. J. et al. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA 299, 1158–1165 (2008).
Christenson, J. et al. Chest compression fraction determines survival of patients with out-of-hospital ventricular fibrillation. Circulation 120, 1241–1247 (2009).
Grunau, B. et al. Relationship between time-to-ROSC and survival in out-of-hospital cardiac arrest ECPR candidates: When is the best time to consider transport to hospital?. Prehosp. Emerg. Care 20, 615–622 (2016).
Soar, J. et al. European resuscitation council guidelines 2021: Adult advanced life support. Resuscitation 161, 115–151 (2021).
Lupton, J. R. et al. Effect of initial airway strategy on time to epinephrine administration in patients with out-of-hospital cardiac arrest. Resuscitation 139, 314–320 (2019).
Dewolf, P. et al. Assessment of chest compression interruptions during advanced cardiac life support. Resuscitation 165, 140–147 (2021).
Tomte, O. et al. Advanced life support performance with manual and mechanical chest compressions in a randomized, multicentre manikin study. Resuscitation 80, 1152–1157 (2009).
Hopkins, C. L. et al. Implementation of pit crew approach and cardiopulmonary resuscitation metrics for out-of-hospital cardiac arrest improves patient survival and neurological outcome. J. Am. Heart Assoc. 5, e002892 (2016).
Sheraton, M. et al. Effectiveness of mechanical chest compression devices over manual cardiopulmonary resuscitation: A systematic review with meta-analysis and trial sequential analysis. West. J. Emerg. Med. 22, 810–819 (2021).
Nolan, J. P. et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the Utstein resuscitation registry template for in-hospital cardiac arrest: A consensus report from a task force of the international liaison committee on resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand council on resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, resuscitation council of Southern Africa, resuscitation council of Asia). Circulation 140, e746–e757 (2019).
Mak, M., Moulaert, V. R., Pijls, R. W. & Verbunt, J. A. Measuring outcome after cardiac arrest: Construct validity of cerebral performance category. Resuscitation 100, 6–10 (2016).
Panchal, A. R. et al. Adult basic and advanced life support writing group. Part 3: Adult basic and advanced life support: 2020 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 142, S366–S468 (2020).
Yamashita, A. et al. Temporal variations in dispatcher-assisted and bystander-initiated resuscitation efforts. Am. J. Emerg. Med. 36, 2203–2210 (2018).
Grunau, B. et al. Comparing the prognosis of those with initial shockable and non-shockable rhythms with increasing durations of CPR: Informing minimum durations of resuscitation. Resuscitation 101, 50–56 (2016).
Kurosaki, H., Takada, K. & Okajima, M. Time point for transport initiation in out-of-hospital cardiac arrest cases with ongoing cardiopulmonary resuscitation: A nationwide cohort study in Japan. Acute Med. Surg. 9, e802 (2022).
Grunau, B. et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA 324, 1058–1067 (2020).
Kurz, M. C. et al. Advanced vs. basic life support in the treatment of out-of-hospital cardiopulmonary arrest in the resuscitation outcomes consortium. Resuscitation 128, 132–137 (2018).
Hansen, M. et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation 137, 2032–2040 (2018).
Poppe, M. et al. Management of EMS on-scene time during advanced life support in out-of-hospital cardiac arrest: A retrospective observational trial. Eur. Heart J. Acute Cardiovasc. Care 9, S82–S89 (2020).
de Graaf, C., Beesems, S. G. & Koster, R. W. Time of on-scene resuscitation in out of-hospital cardiac arrest patients transported without return of spontaneous circulation. Resuscitation 138, 235–242 (2019).
Ishii, M. et al. Japanese Circulation Society with Resuscitation Science Study (JCS-ReSS) Investigators. Sex- and age-based disparities in public access defibrillation, bystander cardiopulmonary resuscitation, and neurological outcome in cardiac arrest. JAMA Netw. Open 6, e2321783 (2021).
Souers, A. et al. Bystander CPR occurrences in out of hospital cardiac arrest between sexes. Resuscitation 166, 1–6 (2021).
Kiyohara, K. et al. The association between public access defibrillation and outcome in witnessed out-of-hospital cardiac arrest with shockable rhythm. Resuscitation 140, 93–97 (2019).
Acknowledgements
We would like to express our gratitude to all the researchers affiliated with the Department of Emergency Medical Sciences at Niigata University of Health and Welfare. Additionally, we extend our thanks to all emergency medical personnel nationwide for their dedication to emergency operations in Japan.
Author information
Authors and Affiliations
Contributions
Y.T. had full access to all the data in the study and took responsibility for the integrity of the data and accuracy of the data analysis. Study Concept and Design: Y.T. Acquisition of data: K.O. Analysis and interpretation of data: All authors. Drafting of the manuscript: Y.T. and G.T. Statistical analysis: Y.T. Study supervision: Y.T. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Takei, Y., Toyama, G., Takahashi, T. et al. Optimal duration and timing of basic-life-support-only intervention for patients with out-of-hospital cardiac arrest. Sci Rep 14, 6071 (2024). https://doi.org/10.1038/s41598-024-56487-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-56487-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.