Abstract
The risk of having atrial fibrillation (AF) is associated with alcohol intake. However, it is not clear whether sudden cardiac arrest (SCA) and ventricular arrhythmia (VA) including ventricular tachycardia, flutter, or fibrillation have similar associations with alcohol. We aimed to evaluate the association of alcohol intake with all-cause death, new-onset AF, VA, and SCA using single cohort with a sufficient sample size. A total of 3,990,373 people without a prior history of AF, VAs, or SCA was enrolled in this study based on nationwide health check-up in 2009. We classified the participants into four groups according to weekly alcohol consumption, and evaluated the association of alcohol consumption with each outcome. We observed a significant association between mild (hazard ratio [HR] = 0.826; 95% confidence interval [CI] = 0.815–0.838) to moderate (HR = 0.930; 95% CI = 0.912–0.947) drinking with decreased risk of all-cause mortality. However heavy drinking (HR = 1.108; 95% CI = 1.087–1.129) was associated with increased all-cause death. The risk of new-onset AF was significantly associated with moderate (HR = 1.129; 95% CI = 1.097–1.161) and heavy (HR = 1.298; 95% CI = 1.261–1.337) drinking. However, the risk of SCA showed negative association with all degrees of alcohol intake: 20% (HR = 0.803; 95% CI = 0.769–0.839), 15% (HR = 0.853; 95% CI = 0.806–0.902), and 8% (HR = 0.918; 95% CI = 0.866–0.974) lower risk for mild, moderate, and heavy drinkers, respectively. Mild drinking was associated with reduced risk of VA with moderate and heavy drinking having no associations. In conclusion, the association between alcohol and various outcomes in this study were heterogeneous. Alcohol might have different influences on various cardiac disorders.
Similar content being viewed by others
Introduction
Sudden cardiac arrest (SCA) is one of the leading causes of cardiovascular mortality worldwide, accounting for approximately half of all deaths from cardiovascular disease1. The majority of people with SCA had no previous history of heart disease making it a challenging task to assess the risk or establish strategies for prevention2,3.
According to previous studies, various factors such as hypertension, diabetes mellitus, or metabolic syndrome are known to increase the risk for SCA1,4,5,6,7. Ventricular arrhythmias (VA) such as ventricular tachycardia (VT), ventricular flutter (VFL), or ventricular fibrillation (VF) are the main cause of SCA and share similar risk factors2,8. The impact of alcohol on VA and SCA is controversial. A prior prospective cohort study of 7,735 men showed that heavy drinking is associated with a two-fold increased risk of sudden cardiac death9. In contrast, Albert et al. reported that men who consumed low-to-moderate alcohol (2–6 drinks per week) had a significantly lower risk of sudden cardiac death compared with rare-to-never drinkers10. In that study, the risk of sudden cardiac death was not increased in people who drank daily10. A recent observational study of 408,712 individuals showed that total alcohol consumption has a U-shaped association with SCA but not with VA11.
Even though ‘low-to-moderate’ consumption of alcohol is associated with lower cardiovascular mortality, alcohol can have various toxic effects on the heart12. Long-term heavy alcohol consumption can cause increased left ventricular mass, dilation of the ventricles, thinning of walls, and reduced contractility, which is known as alcoholic cardiomyopathy13. Atrial cardiomyocytes are also subject to the toxic effects of alcohol, and particularly heavy or frequent alcohol consumption is considered a strong risk factor for atrial fibrillation (AF)14,15. It is not clear why alcohol has a different influence on AF vs. VA.
We performed this nationwide population-based analysis to (i) determine the impact of alcohol on VA and SCA and (ii) compare the influence of alcohol on AF vs. VA and SCA.
Methods
Study participants
This study used the database from the National Health Insurance Service of the Republic of Korea (K-NHIS). This database can represent the entire population of the Republic of Korea since all citizens are mandatory subscribers to the service. The K-NHIS offers a regular health screening to all subscribers and accumulates the results in the database. Therefore, the database comprises various health-related information collected from nationwide health check-ups; for example, a health questionnaire about alcohol consumption habits, smoking status, and exercise level; medical measurements for body weight, height, and blood pressure; results of laboratory tests such as fasting blood glucose or lipid profiles. The K-NHIS database contains the reports of International Classification of Disease, 10th edition (ICD-10) diagnostic codes of AF, VT, VFL, VF, SCA, and other medical conditions throughout the entire nation. Mortality data is also stored in the K-NHIS database. Since subscription fee is determined by the income of the subscriber, the K-NHIS has data on income level of its subscribers. Due to the mandatory subscription, it offers data with a sufficient duration of follow-up, while being free of follow-up losses except immigrations.
This study included patients who received a nationwide health screening in 2009. The screening period was set from January 2002 to December 2008 to identify baseline medical history of the included patients. The endpoint of the study was a new onset of AF, VA (VT, VFL, VF), or SCA. Patients were excluded if they were (1) aged less than 20 years at the 2009 health screening; (2) previously diagnosed with AF, VA, or SCA during the screening period; or (3) had missing data on alcohol consumption. The current study and the protocol were approved by the official review committee of the K-NHIS and the institutional review board of Korea University Medicine Anam Hospital. Written informed consent was waived by institutional review board of Korea University Medicine Anam Hospital due to the retrospective nature of the study. The legal regulations of the Republic of Korea and the ethical guidelines of the 2013 Declaration of Helsinki were strictly followed.
Alcohol intake
This study uses two parameters included in the questionnaire of the national health screening: the number of days per week a respondent drinks and the amount a respondent consumes in a drinking session. We defined a standardized cup as a different volume for each type of alcoholic beverage but can hold a similar amount of alcohol (ethanol). For example, a 220 mL-sized standard cup for beer and a 50 mL-sized cup for Soju (a traditional Korean alcohol) can be calculated to hold about 8 g of alcohol each15. Based on the exact amount of alcohol intake measured, the total amounts of alcohol consumed per week were calculated, and participants were classified into four groups: (i) non-drinkers: 0 g per week; (ii) mild drinkers: less than 105 g per week; (iii) moderate drinkers: less than 210 g per week; (iv) heavy drinkers: equal to or more than 210 g per week (Supplementary Table S1).
Definitions
The diagnoses of AF, VA (VT, VFL, VF), and SCA were based on the record of International Classification of Disease, 10th revision codes (ICD-10) in the K-NHIS database. The exact ICD-10 diagnostic codes for diseases related to this study are described in Supplementary Table S2. The strategy of ICD-10 code-based diagnosis is validated in our multiple publications6,7,16,17. The incidence of new-onset AF, VT, VFL, VF, or SCA was calculated as the number of newly diagnosed cases of each disease per 1,000 patient-years of follow-up. Smoking habit, diabetes mellitus, hypertension, and dyslipidemia were classified into three groups in this study, which is described in Supplementary Table S3. The status of regular physical activity was evaluated according to the self-questionnaire during the 2009 K-NHIS checkup. People who had one or more sessions in a week with moderate- or high-intensity activity were considered as having regular exercise. Chronic kidney disease (CKD) was defined as estimated glomerular filtration rate (eGFR) less than 60 mL/min/1.73m2, calculated by the Modification of Diet in Renal Disease (MDRD) equation. Thyroid disease, liver cirrhosis, and cancer were defined based on relevant ICD-10 codes. Heart failure was also based on ICD-10 codes but only those reported during inpatient admission were counted. The robustness of the definitions stated above has been validated in our prior publications6,7,16,17.
Statistical analysis
Comparison between continuous variables was performed by Student’s t-test and ANOVA, the results of which are presented as mean ± standard deviation. Chi-square test was used to make a comparison between categorical values, and the results are described as percentile values. The hazard ratio (HR) and 95% confidence interval (CI) were analyzed by multivariate Cox regression analysis. Multivariate model 1 is adjusted for age and sex; model 2 for model 1 plus body-mass index (BMI), smoking status, regular exercise habit, and income level; model 3 for model 2 plus hypertension, diabetes mellitus, dyslipidemia, and CKD; and model 4 for model 3 plus history of heart failure and thyroid disease. Covariates that showed significance difference among groups stratified by alcohol consumption amount were included in the model. Variables that were associated with the risk of SCA in our prior work was also included in the model18. For all multivariate adjustments, non-drinkers were set as the reference group. All significance tests were two-tailed, and p-values less than 0.05 were considered statistically significant.
Results
Study participants
A flowchart describing the enrollment of study participants is presented in Fig. 1. After exclusion by age, prior diagnosis, or missing data, 3,990,373 people were included in this study. Participants were classified into non-drinkers, mild drinkers, moderate drinkers, and heavy drinkers, and their baseline demographics are summarized in Table 1. Non-drinkers were more often older, female, and smoked less. In addition, they had lower BMI, waist circumference, and blood pressure; higher low-density lipoprotein (LDL); less regular exercise habits; and higher prevalence of CKD, heart failure, and thyroid disease (Table 1).
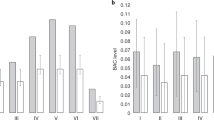
All-cause mortality
Incidences (per 1,000 person*year follow-up) of death, regardless of the cause, were 5.80, 3.06, 3.77, and 5.61 for non-drinkers, mild drinkers, moderate drinkers, and heavy drinkers, respectively. After adjustment of covariates (multivariate model 4), mild drinkers (HR = 0.83; 95% CI = 0.82–0.84; p < 0.01; Table 2 and Fig. 2) and moderate drinkers (HR = 0.93; 95% CI = 0.91–0.95; p < 0.01; Table 2 and Fig. 2) showed significantly decreased risks of all-cause mortality. On the other hand, heavy drinkers had a 10.8% increased risk of all-cause death (HR = 1.11; 95% CI = 1.09–1.13; p < 0.01; Table 2 and Fig. 2). The impact of various covariates on all-cause death is depicted in Fig. 3 (multivariate model 3). Old age, male sex, smoking, lack of regular exercise, high income, hypertension, diabetes mellitus, and CKD were major risk factors for all-cause mortality. Presence of dyslipidemia did not increase the risk, and high BMI was associated with lower risk (Fig. 3a).
Influence of alcohol consumption Incidence is per 1,000 person*year follow-up. AF: atrial fibrillation; CI: confidence interval; HR: hazard ratio; VA: ventricular arrhythmia; VF: ventricular fibrillation; VFL: ventricular flutter; VT: ventricular tachycardia; SCA: sudden cardiac arrest Alcohol consumption demonstrated different associations with all-cause mortality, atrial fibrillation, ventricular arrhythmias, and sudden cardiac arrest. HRs are adjusted for age, sex, body mass index, smoking status, regular exercise, income level, hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, heart failure, and thyroid disease.
Risk factors for all-cause death, AF, VA, and SCA. Male, non-smoker, no regular exercise, non-hypertensive, non-diabetic, and no dyslipidemia were set as reference values for each set of comparison. For values regarding income, low income (lowest quintile) was set as the reference for all-cause mortality, while high income was set as the reference for the rest of the diseases in interest.
Atrial fibrillation
We observed a considerably higher incidence of AF in people who drink large amounts of alcohol. The incidence of AF was 2.42, 1.53, 1.83, and 2.42 for non-drinkers, mild drinkers, moderate drinkers, and heavy drinkers, respectively. After adjustment of covariates (multivariate model 4), moderate drinking (HR = 1.13; 95% CI = 1.10–1.16; p < 0.01; Table 2 and Fig. 2) and heavy drinking (HR = 1.30; 95% CI = 1.26–1.34; p < 0.01; Table 2 and Fig. 2) were associated with significantly increased risk of AF. Mild drinkers had a similar risk of AF compared with non-drinkers (HR = 1.01; 95% CI = 0.99–1.03; p = 0.30; Table 2 and Fig. 2). Other factors associated with increased risk of AF were old age, male sex, smoking, high BMI, lack of regular exercise, hypertension, diabetes mellitus, and CKD. Dyslipidemia did not show any consistent association with AF (Fig. 3b).
Ventricular arrhythmias
The association between alcohol and VAs was different from that of AF. In comparison with non-drinkers, mild drinkers showed significantly lower risk of VA (HR = 0.87; 95% CI = 0.82–0.92; p < 0.01; Table 2 and Fig. 2). Moderate drinking and heavy drinking were associated with numerically, but not statistically, lower risk of VA (Table 2 and Fig. 2). Risk factors associated with increased risk of VA were old age, male sex, current smoker, lack of regular exercise, hypertension, diabetes mellitus, dyslipidemia, and CKD (Fig. 3c).
Sudden cardiac arrest
The incidences were 0.53, 0.35, 0.44, and 0.57, for non-drinkers, mild drinkers, moderate drinkers, and heavy drinkers, respectively. Multivariate analysis demonstrated that alcohol consumption was associated with lower risk of SCA regardless of the amount: (i) Mild drinkers: HR = 0.80; 95% CI = 0.77–0.84; p < 0.01, (ii) Moderate drinkers: HR = 0.85; 95% CI = 0.81–0.90; p < 0.01, and (iii) Heavy drinkers: HR = 0.92; 95% CI = 0.87–0.97; p = 0.01 (Table 2 and Fig. 2). Old age, male sex, smoking, lower BMI, lack of regular exercise, low income, hypertension, diabetes mellitus, and CKD were risk factors significantly associated with SCA. Dyslipidemia showed an inconsistent association (Fig. 3d).
Heart failure admission
Mild drinkers showed 15.3% decreased risk of heart failure admission compared with non-drinkers (HR = 0.85; 95% CI = 0.83–0.86; p < 0.01). Moderate drinking was also associated with lower risk of heart failure (HR = 0.88; 95% CI = 0.86–0.90; p < 0.01). However, heavy drinking was associated with similar risk of heart failure admission compared with non-drinking (HR = 1.00; 95% CI = 0.98–1.03).
Subgroup analysis
The interaction between alcohol consumption and sex on each outcome was evaluated (Table 3). Increased risk of AF in drinkers was more pronounced in males. However, females were more vulnerable to alcohol in terms of all-cause death. No remarkable interactions were observed between alcohol and sex in ventricular arrhythmias and SCA. Age also did not show any meaningful interactions with alcohol consumption in all outcomes.
Discussion
In this study, we analyzed the relationship between the amount of alcohol intake and all-cause mortality, AF, VA (VT, VFL, or VF), and SCA. The principal findings of this study are as follows. (i) The association between alcohol consumption and risk of all-cause mortality is U-shaped. Compared to non-drinkers, mild to moderate drinkers had lower risk, while heavy drinkers had higher risk. (ii) Moderate to heavy drinkers had a significantly increased risk of AF compared with non-drinkers. (iii) Alcohol intake, regardless of amount, was associated with lower risk of SCA. (iv) Mild drinkers had lower risk of VA compared with non-drinkers. The strong points of our study are a large sample size, adjustment of various covariates, and analysis of all-cause mortality, AF, VA, and SCA in the same cohort. In this way, we were able to reveal the different influence of alcohol on AF vs. VA and SCA.
Alcohol and cardiac arrhythmias
The association between alcohol and AF is demonstrated in multiple prior studies14,15. The lower risk of all-cause mortality in mild to moderate drinkers was also observed in other observational studies12. Our study showed similar results in a different ethnic group with a larger sample size utilizing nationwide health insurance data.
It has long been discussed that alcohol intake and the risk of VA and SCA may have a specific relationship, but this has not been clarified19. Prior studies of VA with limited sample sizes showed inconsistent results11,20,21. One study of patients with myocardial infarction who did not receive thrombolytic therapy stated that frequency of drinking was not associated with an increased risk of VA20, while another study of patients without cardiovascular disease concluded that heavy consumption of alcohol is a major risk factor for VA21. Using the UK Biobank cohort, a recent study gathered a much larger and more generalized population11. The study reported a U-shaped relationship such that those who drank less than 208 g of alcohol per week (in the current study, mild and moderate drinkers) had less risk of SCA, while the conclusion for VAs was not statistically significant11. In our study, not only mild to moderate drinkers, but also heavy drinkers had a significantly lower risk of SCA. For VAs, mild drinkers had a significantly lower risk compared with non-drinkers. Moderate and heavy drinkers had numerically, but not statistically significant, lower risk of VAs. To our knowledge, this is the study with the largest sample size (n = 3,990,373) to evaluate the associations between alcohol and various cardiac disorders simultaneously.
Biological mechanism
Alcohol consumption can cause pathophysiological changes to the heart, such as alterations in the atrial effective refractory period or the autonomic nervous system15,22,23. Elevation in blood pressure, obesity, and direct toxic effects on cardiomyocytes are other explanations for the association between alcohol consumption and increased risk of new-onset AF15,24,25.
Ventricular arrhythmias can be initiated by various factors, but the main cause is acute ischemia of the heart or pre-existing ischemia-related scar26. Coronary artery disease is also a main cause of SCA. It is widely perceived that a moderate alcohol intake can have a protective effect on coronary artery disease27,28, and one systematic review reported that the risk significantly decreases when consuming more than 30 g of alcohol per day28, a criterion classified as heavy drinking (> 210 g per week) in the current study. This effect can be explained by changes in cholesterol levels and coagulation factors, both related to atherosclerosis and thrombogenesis in the coronary arteries. Intake of alcohol is associated with higher synthesis and slower decrease in high-density lipoprotein (HDL) level, thereby maintaining an upregulated level of HDL29,30. Furthermore, our study revealed an inverse linear association between amount of alcohol intake and LDL level (Table 1). High HDL and low LDL can have a prohibitory effect on the underlying inflammatory process of atherosclerosis; as a result, the risk of coronary artery disease might decrease as well as the risk of VAs and SCA. Although investigated at a cellular level, alcohol is also proven to have an effect on upregulating expression and synthesis of fibrinolytic proteins such as tissue plasminogen activator, which can prohibit the formation of thrombi31,32.
Clinical implications
Ventricular arrhythmia is strongly connected to the risk of SCA, a major socioeconomic burden. Due to a narrow therapeutic window, most SCA events have low chance of neurologically intact survival33. Atrial fibrillation is another major burden for the general population since its prevalence is up to 2%34. Primary prevention of both diseases will have a significant impact on public health. Although alcohol consumption was associated with significantly lower risk of SCA, the risk of new-onset AF was significantly increased. Furthermore, significantly increased risk of all-cause death was observed in the heavy-drinker group. Mild to moderate intake of alcohol might have benefits in terms of prevention of SCA and all-cause death. However, due to potential bias originating from retrospective analysis, heterogeneous effect of alcohol on individuals, and non-cardiac hazardous effects such as carcinogenesis, we cannot conclude whether mild to moderate intake of alcohol will be beneficial for public health35,36. Regarding the risk of new-onset AF, cessation or reducing alcohol intake might be helpful for the prevention in the general population.
Limitations
This study was based on the database of K-NHIS, which exclusively comprises East Asian ethnicity, so it is necessary to consider ethnic differences when applying the result to other ethnic groups. Also, not just one, but multiple measurements of alcohol consumption habits should be considered in future studies since changes in alcohol intake habits can have independent association with cardiac arrhythmia and SCA. Since this study was based on a claim database, unmeasured confounders and coding inaccuracies might exist. Despite vigorous efforts to adjust various confounders in the multivariable models, residual confounders can exist. Diagnosis of AF, VT, and VF was based on reports of relevant ICD-10 codes and electrocardiography documentation was not possible.
Conclusion
New-onset AF and SCA (including VAs) showed different directions of association with alcohol intake. Opposite association with alcohol intake suggests that AF and SCA (including VAs) have different pathophysiology. All-cause death was lower in mild to moderate drinkers but higher in heavy drinkers. Since the risk of SCA in heavy drinkers was higher than in mild and moderate drinkers, despite being lower than in non-drinkers, heavy drinking should be avoided.
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author. The raw data cannot be shared due to legal regulation of Republic of Korea and policy of the K-NHIS.
Abbreviations
- AF:
-
Atrial fibrillation
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- HDL:
-
High-density lipoprotein
- HR:
-
Hazard ratio
- ICD:
-
International classification of disease
- K-NHIS:
-
Korean National Health Insurance Service
- LDL:
-
Low-density lipoprotein
- SCA:
-
Sudden cardiac arrest
- VA:
-
Ventricular arrhythmia
- VF:
-
Ventricular fibrillation
- VFL:
-
Ventricular flutter
- VT:
-
Ventricular tachycardia
References
Wong, C. X. et al. Epidemiology of sudden cardiac death: Global and regional perspectives. Heart Lung Circ. 28, 6–14. https://doi.org/10.1016/j.hlc.2018.08.026 (2019).
Kuriachan, V. P., Sumner, G. L. & Mitchell, L. B. Sudden cardiac death. Curr. Probl. Cardiol. 40, 133–200. https://doi.org/10.1016/j.cpcardiol.2015.01.002 (2015).
Wellens, H. J. et al. Risk stratification for sudden cardiac death: Current status and challenges for the future. Eur. Heart J. 35, 1642–1651. https://doi.org/10.1093/eurheartj/ehu176 (2014).
Ray, W. A., Chung, C. P., Murray, K. T., Hall, K. & Stein, C. M. Atypical antipsychotic drugs and the risk of sudden cardiac death. N. Eng. J. Med. 360, 225–235. https://doi.org/10.1056/NEJMoa0806994 (2009).
Baig, S. et al. Ventricular arrhythmia and sudden cardiac death in Fabry disease: A systematic review of risk factors in clinical practice. Europace. 20, f153–f161. https://doi.org/10.1093/europace/eux261 (2018).
Kim, Y. G. et al. Metabolic syndrome, gamma-glutamyl transferase, and risk of sudden cardiac death. J. Clin. Med. 11, 1781 (2022).
Kim, Y. G. et al. Hypertension and diabetes including their earlier stage are associated with increased risk of sudden cardiac arrest. Sci. Rep. 12(1), 12307 (2022).
Aro, A. L. et al. Electrical risk score beyond the left ventricular ejection fraction: Prediction of sudden cardiac death in the Oregon sudden unexpected death study and the atherosclerosis risk in communities study. Eur. Heart J. 38, 3017–3025. https://doi.org/10.1093/eurheartj/ehx331 (2017).
Wannamethee, G. & Shaper, A. G. Alcohol and sudden cardiac death. British Heart J. 68, 443–448. https://doi.org/10.1136/hrt.68.11.443 (1992).
Albert, C. M. et al. Moderate alcohol consumption and the risk of sudden cardiac death among US male physicians. Circulation. 100, 944–950. https://doi.org/10.1161/01.cir.100.9.944 (1999).
Tu, S. J. et al. Alcohol consumption and risk of ventricular arrhythmias and sudden cardiac death: An observational study of 408,712 individuals. Heart Rhythm. 19, 177–184. https://doi.org/10.1016/j.hrthm.2021.09.040 (2022).
Li, Y. et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. 138, 345–355 (2018).
Piano, M. R. Alcoholic cardiomyopathy: Incidence, clinical characteristics, and pathophysiology. Chest. 121, 1638–1650. https://doi.org/10.1378/chest.121.5.1638 (2002).
Larsson, S. C., Drca, N. & Wolk, A. Alcohol consumption and risk of atrial fibrillation: A prospective study and dose-response meta-analysis. J. Am. Coll. Cardiol. 64, 281–289. https://doi.org/10.1016/j.jacc.2014.03.048 (2014).
Kim, Y. G. et al. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: a nationwide population-based study. Europace. 22, 216–224. https://doi.org/10.1093/europace/euz256 (2020).
Kim, Y. G. et al. Different influence of blood pressure on new-onset atrial fibrillation in pre-and postmenopausal women: A nationwide population-based study. Hypertension. 77, 1500–1509 (2021).
Kim, Y. G. et al. Atrial fibrillation is associated with increased risk of lethal ventricular arrhythmias. Sci. Rep. 11, 1–9 (2021).
Kim, Y. G. et al. Obesity is indirectly associated with sudden cardiac arrest through various risk factors. J. Clin. Med. 12, 2068 (2023).
George, A. & Figueredo, V. M. Alcohol and arrhythmias: A comprehensive review. J. Cardiovasc. Med. Hagerstown. 11, 221–228. https://doi.org/10.2459/JCM.0b013e328334b42d (2010).
Mukamal, K. J., Muller, J. E., Maclure, M., Sherwood, J. B. & Mittleman, M. A. Lack of effect of recent alcohol consumption on the course of acute myocardial infarction. Am. Heart J. 138, 926–933. https://doi.org/10.1016/s0002-8703(99)70019-0 (1999).
Engstrom, G., Hedblad, B., Janzon, L. & Juul-Moller, S. Ventricular arrhythmias during 24-h ambulatory ECG recording: incidence, risk factors and prognosis in men with and without a history of cardiovascular disease. J. Intern. Med. 246, 363–372. https://doi.org/10.1046/j.1365-2796.1999.00509.x (1999).
Marcus, G. M. et al. Alcohol intake is significantly associated with atrial flutter in patients under 60 years of age and a shorter right atrial effective refractory period. Pacing. Clin. Electrophysiol. 31, 266–272. https://doi.org/10.1111/j.1540-8159.2008.00985.x (2008).
Mandyam, M. C. et al. Alcohol and vagal tone as triggers for paroxysmal atrial fibrillation. Am. J. Cardiol. 110, 364–368. https://doi.org/10.1016/j.amjcard.2012.03.033 (2012).
Kallistratos, M. S., Poulimenos, L. E. & Manolis, A. J. Atrial fibrillation and arterial hypertension. Pharmacol. Res. 128, 322–326. https://doi.org/10.1016/j.phrs.2017.10.007 (2018).
Fuchs, F. D. & Fuchs, S. C. The effect of alcohol on blood pressure and hypertension. Curr. Hypertens. Rep. 23, 42. https://doi.org/10.1007/s11906-021-01160-7 (2021).
Doig, J. et al. Ventricular tachycardia in ischaemic heart disease: Insights into the mechanisms from cardiac mapping and implications for patient management. Eur. Heart J. 16, 1027–1035 (1995).
Klatsky, A. L. Alcohol and cardiovascular diseases. Expert. Rev. Cardiovasc. Ther. 7, 499–506. https://doi.org/10.1586/erc.09.22 (2009).
Piano, M. R. Alcohol’s effects on the cardiovascular system. Alcohol. Res. 38, 219–241 (2017).
De Oliveira, E. S. E. R. et al. Alcohol consumption raises HDL cholesterol levels by increasing the transport rate of apolipoproteins A-I and A-II. Circulation. 102, 2347–2352. https://doi.org/10.1161/01.cir.102.19.2347 (2000).
Huang, S. et al. Longitudinal study of alcohol consumption and HDL concentrations: A community-based study. Am. J. Clin. Nutr. 105, 905–912 (2017).
Grenett, H. E. et al. Ethanol transcriptionally upregulates t-PA and u-PA gene expression in cultured human endothelial cells. Alcohol. Clin. Exp. Res. 22, 849–853 (1998).
Booyse, F. M., Aikens, M. L. & Grenett, H. E. Endothelial cell fibrinolysis: transcriptional regulation of fibrinolytic protein gene expression (t-PA, u-PA, and PAI-1) by low alcohol. Alcohol. Clin. Exp. Res. 23, 1119–1124. https://doi.org/10.1111/j.1530-0277.1999.tb04235.x (1999).
Virani, S. S. et al. Heart disease and stroke statistics-2020 update: A report from the American heart association. Circulation. 141, e139–e596. https://doi.org/10.1161/CIR.0000000000000757 (2020).
Miyasaka, Y. et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 114, 119–125 (2006).
Brooks, P. J., Enoch, M.-A., Goldman, D., Li, T.-K. & Yokoyama, A. The alcohol flushing response: An unrecognized risk factor for esophageal cancer from alcohol consumption. PLoS medicine. 6, e1000050 (2009).
Holmes, M. V. et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. Bmj. 349, g4164 (2014).
Funding
This work was supported by a Korea University Grant (J-I.C); a grant from Korea University Anam Hospital, Seoul, Republic of Korea (J-I.C); and in part by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT, Ministry of Science and ICT) (No. 2021R1A2C2011325 to J-I.C). The funders had no role in data collection, analysis, or interpretation; trial design; patient recruitment; or any other aspect pertinent to the study.
Author information
Authors and Affiliations
Contributions
J.I.C. had full access to all data in this study and takes responsibility for data integrity and analytical accuracy. The concept and design of the study were developed by Y.G.K., K.D.H., J.I.C., and Y.H.K. Data analysis and interpretation were performed by Y.G.K., D.Y.K., S.Y.R., H.S.L., Y.Y.C., K.D.H., K.J.M., H.Y.C., and J.I.C. The manuscript was drafted by Y.G.K., D.Y.K., K.D.H., and J.I.C. Statistical analysis was performed by Y.G.K., D.Y.K., H.S.L., J.H.J., K.D.H., and J.I.C. Data collection was performed by Y.G.K., S.Y.R., J.H.J., K.J.M., K.D.H., J.S., and J.I.C.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Y.G., Kim, D.Y., Roh, SY. et al. Alcohol and the risk of all-cause death, atrial fibrillation, ventricular arrhythmia, and sudden cardiac arrest. Sci Rep 14, 5053 (2024). https://doi.org/10.1038/s41598-024-55434-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-55434-6
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.