Abstract
Dyslipidemia is highly prevalent and an important modifiable risk factor of cardiovascular disease in China. However, there is little information on the dyslipidemia in Shangcheng district, eastern China. Therefore, this study aims to investigate the prevalence and associated factors of dyslipidemia among community adults in this area. A community based cross-sectional study was conducted from August 1 to November 30, 2020. The study utilized a multi-stage probability sampling method to enroll permanent residents (those who have resided in this region for 6 months or more) who were 18 years old or above. Firstly, five streets were selected randomly, and then two communities were randomly selected from each of the chosen streets, finally, systematic sampling at the household level was conducted. All participants were interviewed by trained investigators and underwent anthropometric and biochemical measurements using standard criteria. LASSO (least absolute shrinkage and selection operator) and multivariate binary logistic regression were employed to identify the factors associated with dyslipidemia. In total, 3153 participants were enrolled into this study, resulting in a response rate of 93.28%. 33 subjects were excluded because of incomplete data. Finally, 3120 participants with a mean age of 55.26 (SD = 17.97) years were included into analysis. The overall prevalence of dyslipidemia was 35.96%. 21 variables were screened to multivariate binary logistic regression through the implementation of LASSO method. The multivariate binary logistic regression analysis revealed that individuals aged 40–49 [adjusted odds ratio (aOR) = 2.197, 95% confidence interval (CI) 1.445–3.341], 50–59 (aOR = 3.213, 95% CI 2.121–4.868), 60–69 (aOR = 4.777, 95% CI 3.169–7.201), and 70 and above (aOR = 5.067, 95% CI 3.301–7.777), with an educational level of junior middle school (aOR = 1.503, 95% CI 1.013–2.229), with an educational level of senior middle school (aOR = 1.731, 95% CI 1.25–2.397), with an educational level of under graduate and above (aOR = 2.125, 95% CI 1.46–3.095), without hypertension (aOR = 0.627, 95% CI 0.517–0.76), without diabetes (aOR = 0.625, 95% CI 0.498–0.785), obesity (aOR = 1.887, 95% CI 1.13–3.154), frequent smoking (aOR = 1.727, 95% CI 1.293–2.308), frequent drinking (aOR = 0.738, 95% CI 0.556–0.981), without family history of CVD (aOR = 0.505, 95% CI 0.342–0.744), and daily seafood intakes between 42.87 and 71.43 g (aOR = 1.31, 95% CI 1.05–1.634) were significantly associated with dyslipidemia. Gender-stratified analyses showed that aged 70 and above (aOR = 2.127, 95% CI 1.195–3.785), without hypertension (aOR = 0.643, 95% CI 0.484–0.854), without diabetes (aOR = 0.603, 95% CI 0.436–0.834), without CVD (aOR = 0.494, 95% CI 0.309–0.791), without stroke (aOR = 1.767, 95% CI 1.036–3.012), frequent smoking (aOR = 1.951, 95% CI 1.415–2.691), former smoking (aOR = 1.703, 95% CI 1.16–2.502) were significantly associated with dyslipidemia in male. Aged 40–49 (aOR = 3.51, 95% CI 1.789–6.887), 50–59 (aOR = 7.03, 95% CI 3.584–13.791), 60–69 (aOR = 15.728, 95% CI 8.005–30.9), and 70 and above (aOR = 12.929, 95% CI 6.449–25.921), with an educational level of senior middle school (aOR = 1.926, 95% CI 1.288–2.881), with an educational level of under graduate and above (aOR = 2.91, 95% CI 1.75–4.837), without hypertension (aOR = 0.592, 95% CI 0.45–0.779), without diabetes (aOR = 0.619, 95% CI 0.443–0.865), without family history of CVD (aOR = 0.429, 95% CI 0.251–0.733), without family history of cancer (aOR = 0.542, 95% CI 0.316–0.929), daily vegetables intakes between 251 and 500 g (aOR = 0.734, 95% CI 0.545–0.99), daily seafood intakes between 42.87 and 71.43 g (aOR = 1.421, 95% CI 1.04–1.942) were significantly associated with dyslipidemia in female. In the age-stratified analyses, it was found that without hypertension (aOR = 0.522, 95% CI 0.375–0.727) or diabetes (aOR = 0.445, 95% CI 0.267–0.744), obesity (aOR = 2.956, 95% CI 1.258–6.942), frequent smoking (aOR = 1.826, 95% CI 1.196–2.787), showed a significant association with dyslipidemia in individuals aged younger than 60 years. Female (aOR = 1.764, 95% CI 1.316–2.366), with an educational level of junior middle school (aOR = 1.793, 95% CI 1.169–2.749), with an educational level of senior middle school (aOR = 2.002, 95% CI 1.406–2.849), with an educational level of under graduate and above (aOR = 2.849, 95% CI 1.791–4.532), without hypertension (aOR = 0.604, 95% CI 0.477–0.764), without diabetes (aOR = 0.63, 95% CI 0.486–0.818), without CVD (aOR = 0.66, 95% CI 0.473–0.921), frequent smoking (aOR = 1.513, 95% CI 1.02–2.245), former smoking (aOR = 1.647, 95% CI 1.089–2.491), without family history of CVD (aOR = 0.406, 95% CI 0.239–0.692), daily seafood intakes between 42.87 and 71.43 g (aOR = 1.376, 95% CI 1.018–1.859) were significantly associated with dyslipidemia among participants aged 60 and above. Dyslipidemia is a prevalent condition observed among adults residing in Shangcheng district. Risk factors such as gender, age, education, hypertension, diabetes, cardiovascular disease, stroke, obesity, smoking, drinking, family history of cardiovascular disease, family history of cancer, daily vegetables intakes, daily seafood intakes were associated with dyslipidemia and varied across population of different gender and age groups. Enhancing education and promoting self-awareness regarding the necessity of behavior modification and regular medication intake would be beneficial in reducing the occurrence of dyslipidemia among adults in the Shangcheng district.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is a leading cause of death worldwide, accounting for 31% mortality globally in 20161. Compared to the significant decline in cardiovascular disease (CVD) mortality observed in developed western nations2, China is currently facing a notable rise in the incidence and death rates associated with CVD, coinciding with rapid societal and economic development. Research indicated that the estimated cases of cardiovascular disease was 93.8 million in 2016, which is more than twice those in 1990. Moreover, there was an increase in cardiovascular disease-related mortality from 2.51 million to 3.97 million between 1990 and 20163.
Dyslipidemia is one of the most indisputable risk factors for developing and progressing the atherosclerosis4, it is modifiable by medication and lifestyle changes. For CVD patients, it is generally agreed upon by guideline that serum lipid control is necessary. Dyslipidemia is a metabolism disorder characterized by any or a combination of the following: elevated blood levels of total cholesterol (TC), elevated triglycerides (TG), elevated low-density lipoprotein cholesterol (LDL-C), and reduced concentrations of high-density lipoprotein cholesterol (HDL-C). The prevalence of dyslipidemia among adults in China experienced a significant rise from 18.60% in 2002 to 40.40% in 2012, indicating a increase of 21.8 percent over the decade5,6. The prevalence of dyslipidemia in China is notably higher than that of other Asian countries with similar economies, such as the Republic of Korea and Japan7,8. Managing population lipid levels has garnered increased attention, as the optimal management of dyslipidemia is crucial for the prevention of cardiovascular disease (CVD)9.In July 2019, the Chinese government introduced the "Healthy China Action (2019–2030)", which encompasses 'Action against cardiovascular disease' as one of the fifteen key initiatives, with a specific emphasis on expanding lipid testing across the nation10.
Shangcheng district, located in the capital city of Hangzhou in Zhejiang province, is characterized by a stable population with a significant aging problem. The district has been designated as one of the initial national chronic disease prevention and control demonstration areas as well as the first demonstration site for blood lipid prevention and control in Hangzhou. However, there is scarce epidemiological data on the prevalence of dyslipidemia among adults in this area. Due to the significant variation in diets and lifestyles across China11, it is not feasible to extrapolate directly from data obtained in other regions. While a number of studies have examined the epidemiology of dyslipidemia in Zhejiang province, these studies were constrained by specific populations or insufficient estimation12,13,14. On the other hand, the epidemiology of dyslipidemia is dynamic phase, precise ongoing data about lipid status in community population had more practical value. In light of these circumstances, we intend to conduct a community-based cross-sectional study to assess the burden of dyslipidemia among community adults in Shangcheng district, and to identify potential associated factors.
Method
Study population
The sample size was estimated based on the following formula:
The confidence interval (u) used in this study is set at 95%, with the corresponding value of u = 1.96. The rate of disease (p) in this context refers to the prevalence of diabetes mellitus in Zhejiang Province, which is reported to be 7.37%6. The design efficiency (deff) for the present study is set at a value of 1.4. The error tolerance (d) is set at 20%. To account for potential non-response, an additional 10% was added to the minimum sample size. The gender-ratio of individuals aged 18 years and older data for the Shangcheng district in 2020, provided by public security authorities, was used to calculate the sample size, the sample size calculated to be 3380. A multi-stage sampling method was utilized, first, five streets were chosen randomly, second, two communities were randomly selected from each of the chosen streets. Resident registration information was obtained from the selected Community residents' committee, and systematic sampling at the household level was conducted. Survey participants included all family members over 18 years in the sampled households. The inclusion criteria for the study participant were: (a) aged 18 years old and above; (b) living in the selected areas 6 months and above. The exclusion criteria were: (a) physical disability; (b) living in the selected areas less than 6 months and (c) psychological or mental health issues.
Ethical approval was obtained from Academic Review Board (ARB) of Center for Disease Control and Prevention of Shangcheng District, (approval number 202007, dated June 2020). Written informed consent was obtained from the participant before the survey.
Questionnaire investigation
Study was conducted from August 1 to November 30, 2020. Trained interviewers conducted a face-to-face interview at a local community health center using structured questionnaires. The questionnaires covered socio-demographic characteristics, health-related information, lifestyle information, and the frequency and consumption of various food items. Information regarding dietary consumption was collected through food frequency questionnaire (FFQ) that is widely employed in mainland China15,16. Participants were required to report their frequency of consumption of various food weekly over the past year, as well as the quantity of each food item consumed during each instance. All completed questionnaires were subjected to review by supervisors and entered into the system using a parallel double-entry method.
Anthropometric measurements
Trained investigators performed the physical examination, the anthropometric measurements of each participants were performed using a standardized protocol. Height, weight and waist circumference were measured with participants wearing light indoor clothing and no shoes. Participants' weight was measure in kilogram(kg) to the nearest 0.1 kg and height was measured to the nearest 0.1 cm using statiometer, Participants' waist circumference was measured to the nearest 0.1 cm using waist measuring tape. BMI was calculated as an individual's weight in kilograms divided by height in meters squared. A standardized automatic electronic sphygmomanometer was used to measure blood pressure of the participants. A resting period of at least 5 min was required before measurement was taken. The measurement was performed three times and the average value was used in the analysis.
Biochemical measurement
The blood samples of 10 ml were taken from the antecubital vein will be obtained after an overnight fast(≥ 10 h). The blood samples clotted and centrifuged, then freezed and stored below − 20 °C and send to local medical center laboratory for testing immediately. The level of glucose, TC, TG, HDL-C, and LDL-C were measured. All laboratory measurements were done as per guideline. The standardized procedures were strictly followed during the blood sample collection, storage and analysis. The entire process is done by trained medical staff.
Definition of variables
Dyslipidemia: total cholesterol (TC) ≥ 6.2 mmol/L and/or triglyceride (TG) ≥ 2.3 mmol/L and/or high-density lipoprotein cholesterol (HDL-C) ≤ 1.0 mmol/L and/or low-density lipoprotein cholesterol (LDL-C) ≥ 4.1 mmol/L or currently using lipid-lowering agents, or previously diagnosed with dyslipidemia by a doctor17 .
Diabetes: FBG ≥ 7.0 mmol/L, oral glucose tolerance test (OGTT-2 h) ≥ 11.0 mmol/L plasma glucose or self-reported use of anti-diabetic medication in the 2 weeks prior to the examination or self-reported prior diagnosis of diabetes by a doctor18.
Hypertension was defined as systolic pressure > 140 mmHg or diastolic pressure > 90 mmHg or self-reported current use of antihypertensive medication, or prior diagnosis of hypertension by a doctor19.
Body mass index (BMI) was calculated by dividing the weight by the square of the height(kg/m2), obesity status was defined in accordance with the obesity standards in China (< 18.5 kg/m2 for underweight, 18.5–23.9 kg/m2 for normal, 24–27.9 kg/m2 for overweight, ≥ 28 kg/m2 for obese)20.
Waist circumference (WC) was measured at the midpoint between the iliac crest and the lower rib. Men with waist circumference ≥ 90 cm or women with waist circumference ≥ 85 cm were defined as high20.
In present study, the smoking status is categorized into four distinct groups: never, occasional, frequent and former. The term ‘frequent’ denotes individuals who have smoked at least one cigarette per day for a period of six months or more, and are presently continuing to smoke. Meanwhile, ‘occasional’ smokers are those who still engage in smoking but do not consume at least one cigarette per day21.
Secondhand smoke is the inhalation of smoke by individuals who do not smoke cigarettes21.
In the current study, the consumption of alcohol is categorized into four groups: never, occasional, frequent and former. The term ‘frequent’ denotes individuals who consume alcohol at least once a week and continue to drink. ‘occasional’ drinker is one who still consumes alcohol but does less than once per day22.
A history of CVD, stroke and cancer was defined as self-report of any previous diagnosis of CVD, stroke and cancer by a healthcare professional or currently undergoing treatment.
A family history of CVD, hypertension, diabetes, stroke and cancer was defined as a positive response on the survey to questions regarding their parents or siblings being diagnosed with disease mentioned above23.
Dietary information: participants were requested to remember how often they consumed different food items on a weekly and the quantity of each item. These responses were then converted into daily intake amounts. The food categories primarily consisted of grains, vegetables, fruits, meat, seafood, eggs, and dairy products. We utilized the quartile method for categorization because of the non-normal distribution of the dietary data.
Statistics
Data analysis was performed using SPSS software (version 23.0) and R statistical software (version 3.6.2). Data were divided into two groups based on the presence or absence of dyslipidemia. Continuous variables are expressed as either mean ± standard deviation (SD) or median(first quartile-third quartile). The Student’s t-test is employed to assess variables that adhere to a normal distribution, while the Mann–Whitney U test is utilized for variables that do not adhere to a normal distribution. Categorical variables were represented as frequencies and percentages, and the chi-squared test was employed to compare disparities between groups. We utilized the LASSO (Least absolute shrinkage and selection operator) method, a modern and reliable statistical technique, to screen factors associated with dyslipidemia. Ten-fold cross-validation was used to select the penalty term λ. The λ value corresponding to the minimum binomial deviance was chosen, and factors were filtered. The LASSO analysis was performed using the "glmnet" package with R software. The entire variables selected through LASSO were incorporated into multivariate binary logistic regression analyses. Additionally, stratified analyses by gender and age were analyzed, with age groups categorized based on a 60 year cut-off, due to the sample sizes after grouping. P < 0.05 was considered statistically significant.
Results
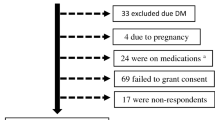
3153 participants were enrolled into present study, with response rate of 93.28% (3153/3380). 33 were excluded due to incomplete data. Finally, 3120 participants aged from 18 to 95 were included in the analysis, the flowchart of population selection was shown in Fig. 1. The general characteristics of the participants are presented in Table 1. The dyslipidemia group and the non-dyslipidemia group had a similar pattern of demographic characteristics with a majority of those not secondhand smoker, without stroke, without cancer, without family history of diabetes or family history of stroke. Participants with dyslipidemia were more likely to have hypertension, diabetes, obesity .
Table 2 shows the lipid levels in the subgroups by gender and age. Male had higher levels of TG than female, while female had higher level of TC, HDL-C and LDL-C than male. Compared to the 18–29 years group, the level of TC, TG and LDL-C increased with age and were highest in the 50–59 year. HDL-C tended to decrease with age.
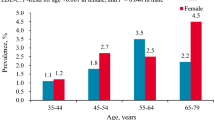
The prevalence of various types of dyslipidemia is presented in Table 3. The overall prevalence of dyslipidemia was 35.96%. It demonstrated an increasing trend with age (Ptrend < 0.001), which is also observed in low HDL-C measurement (Ptrend < 0.001), The prevalence of high TC, high TG and high LDL-C initially rose, and the declined with age(Ptrend < 0.001). There was no statistically significant difference in the overall prevalence of dyslipidemia between male and female (P = 0.356), but high TC and high LDL-C were significantly higher in female than male, while low HDL-C was significantly higher in male than female.
Table 4 displays the data for variables related to dyslipidemia identified through LASSO regression. The model achieved minimum binomial deviance when λ = 0.006544998, 21 variables remain in the model (i.e. are non-zero) (Fig. 2). The LASSO regression method was used to identify potential risk factors for dyslipidemia, including age, gender, education, hypertension, diabetes, cardiovascular disease, stroke, waist circumference, BMI, smoking, secondhand smoker, drinking, family history of hypertension, cardiovascular disease, and cancer, daily intake of grains, vegetables, fruits, seafood, milk and dairy products and eggs.
Selection of significant parameters in variables associated with dyslipidemia. (A) Ten time cross-validation for tuning parameter selection in the LASSO model. (B) LASSO coefficient profiles. The LASSO was used for regression of high dimensional predictors. The method uses an L1 penalty to shrink some regression coefficients to exactly zero. The binomial deviance curve was plotted versus log (λ), where λ is the tuning parameter (A). LASSO coefficient profiles of variables (B). LASSO least absolute shrinkage and selection operator.
The associated factors of dyslipidemia are shown in Table 5. Results of multivariate binary logistic regression reveals that age, education, hypertension, diabetes, obesity, smoking, drinking, family history of CVD and daily seafood intakes were associated with dyslipidemia.
The findings from the analyses stratified by age and sex can be found in Table 6. In both male and female, the prevalence of dyslipidemia rises with advancing age, with a more noticeable age-related pattern observed in females.Hypertension and diabetes are associated with an increased risk of dyslipidemia in both male and female . CVD, stroke and smoke were associated with dyslipidemia in male while family history of CVD, family history of cancer, daily vegetables intakes and daily seafood intakes were associated with dyslipidemia in female. Hypertension, diabetes, obesity, and frequent smoking were related to dyslipidemia in participants younger than 60. gender, education level, hypertension, diabetes, CVD, frequent smoking, former smoking, family history of CVD and daily seafood intakes were associated with dyslipidemia in participants aged 60 and older.
Discussion
The present study investigated the prevalence and risk factors of dyslipidemia among community adults in Shangcheng district. The findings revealed that the overall prevalence of dyslipidemia in this region was 35.96%. Chinese National Nutrition and Health Survey (CNNHS) conducted in 2002, providing appropriate comparison data for our study, revealed that the prevalence of dyslipidemia in present study was nearly double that of the national data (18.6%)24. The median level of TC, TG, HDL-C, and LDL-C were 4.78, 1.38, 1.38, and 2.64 mmol/L, exhibiting an increase when compared to the findings of the previous study25. A positive association between age and dyslipidemia has presented in both full-sample data analyses and gender-stratified analyses,which has also been observed in other city in China26. Previous research has reported that men have a higher risk of dyslipidemia than women27, which is contrary to the findings of our study. Our study found that women are more likely to be affected by dyslipidemia, especially those aged 60 years and above . This might be due to that menopause is a significant risk factor of dyslipidemia in older women. Study reveals that menopause leads to changes in lipid profile through reducing HDL-C, and elevating TC, TG and LDL-C28. The study showed positive association between education level with dyslipidemia prevalence ,which is in the line with previous study29, the possible explanation for this result is that participants with higher education levels may spend more time sitting in the office, have little time to exercise, frequently consume high fat foods, and suffer from a work-related mental health problem30. The present study also identified several common risk factors such as hypertension, diabetes, smoking and obesity in our study population, which is consistent with previous studies31,32,33,34. A family history of CVD and cancer may also lead to an increased risk of dyslipidemia, which has been confirmed in previous study35,36. It was interested that alcohol consumption was negatively associated with dyslipidemia, the possible reason may be that alcohol reduced the activity of cholesterol ester transformation from HDL to atheromatic molecules, subsequently increased the circulating levels of HDL-C37. However, this association was not observed in the analyses stratified by age and sex. Further studies are needed to validate this findings and to investigate the potential mechanisms. A negative association between dyslipidemia and stroke in male was found in present study, which is consistent with previous studies conducted on female38,39, however, the relationship between lipid level and stroke remains controversial and the mechanism has not been elucidated. Further gender specific research is needed.
Moderate intake of vegetables contributed to lower blood lipids, which is confirmed in other researches40,41. Daily seafood intakes is positive associated with dyslipidemia, which is inconsistent with other studies. numerous studies have shown that seafood especially fish contained abundance of n-3 polyunsaturated fatty acids (n-3 PUFAs: eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA]) in fish oils, such as sardine and saury fish42, These elements had diverse cardioprotective effects. The conflicting results may be attributed to the heterogeneity of study designs and/or source of dietary seafood. Another possible explanation could be that individuals with dyslipidemia who adhere to a self-reported diet exhibit a more favorable dietary intake compared to the broader population. The present study was unable to provide a detailed breakdown of various seafood categories, which represents a limitation of the study and suggests a potential avenue for future research.
Our study possesses several strengths. Firstly, instead of employing principal component or factor analysis to examine the relationship between diet and blood lipid, we directly examined each food group, allowing for a more nuanced understanding of the role of each food item. Secondly, the sample of this study was obtained using a multistage random sampling technique to ensure the representative of the population in this region. The research was advantageous for the subjects as it involved a thorough medical assessment. Furthermore, the utilization of a standardized training manual to instruct the research aides facilitated a uniform and methodical approach to data gathering, thereby enhancing the reliability of the measurements. Finally, the abundance of health data, coupled with advanced statistical methods, presents an opportunity to uncover previously unrecognized relationships that were not apparent using traditional statistical methods and smaller datasets. This has the potential to enhance our understanding of the contributing factors of dyslipidemia and provide a more comprehensive insight into the condition. However, our study has several limitations. The inherent features of the cross-sectional design of the study limit any potential inference of causality and temporal relationship between the variables, despite rigorous training and questionnaire quality control of our surveyors, some self-reported items were inevitably subject to recall bias, such as smoke, drink. Additionally, the number of case samples did not allow for a detailed analysis of the different types of dyslipidemia, and some dietary categories could not be further refined. Future research with a larger sample size is needed to explore those factors associated with different types of dyslipidemia.
In summary, the prevalence of dyslipidemia remains high among population aged 18 years and above in this region. Risk factors such as gender, age, education, hypertension, diabetes, cardiovascular disease, stroke, obesity, smoking, drinking, family history of cardiovascular disease, family history of cancer, daily vegetables intakes, daily seafood intakes related to dyslipidemia and varied across age and gender groups.
Conclusion
According to our study, the overall prevalence of dyslipidemia among individuals aged 18 years and above in Shangcheng district remains high. Multiple factors are associated with dyslipidemia, emphasizing the need for heightened awareness and efficient measures to be adopted by local healthcare providers in order to reduce the prevalence of dyslipidemia among adults.
Data availability
Raw clinical data is not permitted for sharing according to the terms of the informed consent. The summary information or other non-subject level analyses for the datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Wijeysundera, H. C. et al. Association of temporal trends in risk factors and treatment uptake with coronary heart disease mortality, 1994–2005. JAMA 303(18), 1841–1847 (2010).
Sidney, S. et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 1(5), 594–599 (2016).
Liu, S. et al. Burden of cardiovascular diseases in China, 1990–2016: Findings from the 2016 Global Burden of Disease Study. JAMA Cardiol. 4(4), 342–352 (2019).
Stone, N. J., Levy, R. I., Fredrickson, D. S. & Verter, J. Coronary artery disease in 116 kind red with familial type II hyperlipoproteinemia. Circulation 49(3), 476–488 (1974).
Zhao, W. H. et al. Epidemiologic characteristics of dyslipidemia in people aged 18 years and over in China. Chin. J. Prevent. Med. 39(5), 306–310 (2005).
Bureau of Disease Prevention and Control, National Health and Family Planning Commission. China's Population Nutrition and Chronic Disease Status Report 2015. (People’s Health Publishing House, 2015).
Kuwabara, M. et al. Different risk for hypertension, diabetes, dyslipidemia, and hyperuricemia according to level of body mass index in Japanese and American subjects. Nutrients 10(8), 1011 (2018).
Boo, S., Yoon, Y. J. & Oh, H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: A cross-sectional analysis. Medicine 97(51), e13713 (2018).
Chinese Joint Committee for the Revision of Guidelines for the Prevention and Treatment of dyslipidemia in adults. Chinese guideline for the management of dyslipidemia in adults . Chin. J. Cardiol. 44(10), 833–853 (2016).
National Health Commission of the People's Republic of China. Healthy China Initiative (2019–2030). http://www.nhc.gov.cn/guihuaxxs/s3585u/201907/e9275fb95d5b4295be8308415d4cd1b2.shtml.2019Nov (2016).
Huang, Y., Gao, L., Xie, X. & Tan, S. C. Epidemiology of dyslipidemia in Chinese adults: Meta-analysis of prevalence, awareness, treatment, and control. Popul. Health Metrics 12(1), 28 (2014).
Zhang, J. et al. Prevalence of dyslipidemia among non-overweight adults and related factors in Zhejiang. Chin. J. Epidemiol. 36(2), 105–109 (2016).
Wang, J. et al. High prevalence of cardiometabolic comorbidities among children and adolescents with severe obesity from a large metropolitan centre (Hangzhou, China). Front. Endocrinol. 13, 807380 (2022).
Zhang, H. et al. A cross-sectional survey on occupational stress and associated dyslipidemia among medical staff in tertiary public hospitals in Wenzhou, China. Brain Behav. 11(3), e02014 (2021).
Huang, L. Y. et al. A meta-analysis of the reproducibility and validity of food frequnecy questionnaires among Chinese Adults. Acta Nutr. Sin. 44(03), 293–300 (2022).
Li, Y. P. et al. Comparison of assessment of food intakes by using 3 dietary survey methods. Chin. J. Prevent. Med. 40(4), 273–280 (2006).
Guo, C. et al. Elevated lipoprotein(a) and risk of coronary heart disease according to different lipid profiles in the general Chinese community population: The CHCN-BTH study. Ann. Transl. Med. 9(1), 26 (2021).
Petersmann, A. et al. Definition, classification and diagnosis of diabetes mellitus. Exp. Clin. Endocrinol. Diabetes 127(S01), S1–S7 (2019).
Shen, Y. et al. Prevalence and risk factors associated with hypertension and prehypertension in a working population at high altitude in China: A cross-sectional study. Environ. Health Prevent. Med. 22(1), 19 (2017).
Chen, C., Lu, F. C., Department of Disease Control Ministry of Health, PR China. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. BES 17(Suppl), 1–36 (2004).
World Health Organization. Guidelines for Controlling and Monitoring the Tobacco Epidemic (World Health Organization, 1998).
Im, P. K. et al. Alcohol consumption and risks of more than 200 diseases in Chinese men. Nat. Med. 29(6), 1476–1486. https://doi.org/10.1038/s41591-023-02383-823 (2023).
Kim, S. J., Kwon, O. D. & Kim, K. S. Prevalence, awareness, treatment, and control of dyslipidemia among diabetes mellitus patients and predictors of optimal dyslipidemia control: Results from the Korea National Health and Nutrition Examination Survey. Lipids Health Dis. 20(1), 29 (2021).
Zhao, W. H. et al. Blood lipid profile and prevalence of dyslipidemia in Chinese adults. Biomed. Environ. Sci. BES 20(4), 329–335 (2007).
Sun, G. Z. et al. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis. 13, 189 (2014).
Chen, R., Xu, P., Li, F. & Song, P. Internal migration and regional differences of population aging: An empirical study of 287 cities in China. Biosci. Trends 12(2), 132–141 (2018).
Huang, C. et al. Prevalence and related factors of dyslipidemia among urban adults aged 35 to 79 years in Southwestern China. Sci. Rep. 11(1), 17579 (2021).
Sharma, U. et al. Dyslipidemia and associated risk factors in a resettlement colony of Delhi. J. Clin. Lipidol. 7(6), 653–660 (2013).
Li, Y., Zhao, L., Yu, D. & Ding, G. The prevalence and risk factors of dyslipidemia in different diabetic progression stages among middle-aged and elderly populations in China. PLoS One 13(10), e0205709 (2018).
Thomas, F. et al. Combined effects of systolic blood pressure and serum cholesterol on cardiovascular mortality in young (<55 years) men and women. Eur. Heart J. 23(7), 528–535 (2002).
Wu, J., Wang, Y., Wang, A., Xie, J. & Zhao, X. Association between fasting triglyceride levels and the prevalence of asymptomatic intracranial arterial stenosis in a Chinese community-based study. Sci. Rep. 8(1), 5744 (2018).
Lin, H. Q. et al. Prevalence of dyslipidemia and prediction of 10-year CVD risk among older adults living in southeast coastal regions in China: A cross-sectional study. Clin. Intervent. Aging 14, 1119–1129 (2019).
Facchini, F., Chen, Y. D., Clinkingbeard, C., Jeppesen, J. & Reaven, G. M. Insulin resistance, hyperinsulinemia, and dyslipidemia in non-obese individuals with a family history of hypertension. Am. J. Hypertens. 5(10), 694–699 (1992).
Kim, S. J., Kwon, O. D., Lee, E. J., Ock, S. M. & Kim, K. S. Impact of a family history of cardiovascular disease on prevalence, awareness, treatment, control of dyslipidemia, and healthy behaviors: Findings from the Korea National Health and Nutrition Examination Survey. PloS One 16(7), e0254907 (2021).
Volcik, K. A., Ballantyne, C. M., Fuchs, F. D., Sharrett, A. R. & Boerwinkle, E. Relationship of alcohol consumption and type of alcoholic beverage consumed with plasma lipid levels: Differences between Whites and African Americans of the ARIC study. Ann. Epidemiol. 18(2), 101–107 (2008).
Mozaffarian, D. & Wu, J. H. Omega-3 fatty acids and cardiovascular disease: Effects on risk factors, molecular pathways, and clinical events. J. Am. Coll. Cardiol. 58(20), 2047–2067 (2011).
Rimm, E. B. et al. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: A science advisory from the American Heart Association. Circulation 138(1), e35–e47 (2018).
Bonaventure, A. et al. Triglycerides and risk of hemorrhagic stroke vs. ischemic vascular events: The Three-City Study. Atherosclerosis 210(1), 243–248 (2010).
Buring, P. M., Ridker, J. E., Kase, P. M., Kurth, C. S. & Rexrode, K. M. Lipid levels and the risk of hemorrhagic stroke among women. Neurology 92(19), e2286–e2294 (2019).
Oh, K. et al. Carbohydrate intake, glycemic index, glycemic load, and dietary fiber in relation to risk of stroke in women. Am. J. Epidemiol. 161(2), 161–169 (2005).
de Castro, T.G., Gimeno, S.G., Ferreira, S.R., Cardoso, M.A.; Japanese-Brazilian Diabetes Study Group. Association of dietary fiber with temporal changes in serum cholesterol in Japanese–Brazilians. J. Nutr. Sci. Vitaminol. (Tokyo) 52(3), 205–210 (2006).
Marques-Vidal, P., Vollenweider, P., Grange, M., Guessous, I. & Waeber, G. Patients with dyslipidemia on a self-reported diet have a healthier dietary intake than the general population. The CoLaus study. Clin. Nutr. ESPEN 11, e33–e39 (2016).
Author information
Authors and Affiliations
Contributions
M.S.: methodology, data curation, formal analysis, validation and writing original draft. X.Z.: conceptualization, formal analysis, validation and review and editing of manuscript. H.W.: data curation, investigation, supervision. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, M., Wang, H. & Zhang, X. Dyslipidemia and its associated factors among community adults located in Shangcheng district, Zhejiang province. Sci Rep 14, 4268 (2024). https://doi.org/10.1038/s41598-024-54953-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54953-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.