Abstract
Solute carrier family (SLC) transporters are expressed in the digestive system and play important roles in maintaining physiological functions in the body. In addition, SLC transporters act as oncoproteins or tumor-suppressor proteins during the development, progression, and metastasis of various digestive system cancers. SLC22A18, a member of the SLC22 gene family, is an orphan transporter with an unknown endogenous substrate. Previous study revealed that SLC22A18 is downregulated in colorectal cancer tissues and that it acts as a suppressor in colorectal cancer, although the effects of SLC22A18 variants on colon cancer cell proliferation, migration, and invasion are unknown. Therefore, in this study, we identified SLC22A18 variants found in multiple populations by searching public databases and determined the in vitro effects of these missense variations on transporter expression and cancer progression. Our results indicated that three missense SLC22A18 variants—p.Ala6Thr, p.Arg12Gln, and p.Arg86His—had significantly lower cell expression than the wild type, possibly owing to intracellular degradation. Furthermore, these three variants caused significantly higher proliferation, migration, and invasion of colon cancer cells than the wild type. Our findings suggest that missense variants of SLC22A18 can potentially serve as biomarkers or prognostic tools that enable clinicians to predict colorectal cancer progression.
Similar content being viewed by others
Introduction
Colorectal cancer ranks as the second most common cancer in women and the third most common in men worldwide1. In the United States, it is the third most diagnosed cancer in both sexes, with the third-highest overall cancer mortality rate. Despite a slight decrease in the overall incidence rate, there is a persistent rise in colorectal cancer cases among individuals under 55 years of age. Notably, despite an overall decline in colorectal cancer mortality, there has been an annual increase ranging from 0.5 to 3% among those under 50 years of age. Within the United States, colorectal cancer is the second leading cause of cancer-related deaths in men under 50 years of age2.
Transporters belonging to the solute carrier family (SLC) play crucial roles in maintaining physiological functions within the digestive system. These SLC transporters actively regulate nutrient absorption and facilitate the transportation of nutrients among cellular organelles3. Numerous studies have highlighted associations between the underexpression or overexpression of SLC transporters and the occurrence or progression of various digestive system cancers4. Notably, the overexpression of SLC7A5, SLC29A2, or SLC38A1 is significantly associated with poor survival in patients with hepatocellular carcinoma5,6.
SLC22A18, which belongs to the SLC22 gene family, is an orphan transporter with an unknown endogenous substrate, though it may be involved in transporting chloroquine and quinidine7. SLC22A18 expression is methylation-dependent, and the transcription factor Sp1 transactivates the SLC22A18 promoter8,9.
SLC22A18 reportedly acts as a suppressor in various cancers, including prostate cancer, Wilms’ tumor, glioma, breast cancer, and colorectal cancer10,11,12,13,14,15. Particularly, Jung et al.15 revealed that SLC22A18 is downregulated in colorectal cancer tissues, exerting suppressive effects by inhibiting colony formation and inducing G2/M arrest. They further reported a significant correlation between low SLC22A18 expression and a poor long-term prognosis in patients with colorectal cancer. In contrast, SLC22A18 is overexpressed in pancreatic cancer16.
Although many case–control studies aimed at gaining a better understanding of SLC22A18 have been conducted, relatively few molecular and functional studies of SLC22A18 genetic variants have been reported. In this study, we investigated the effects of four missense SLC22A18 variants on transporter expression and the progression of colon cancer cells using various in vitro assay systems.
Results
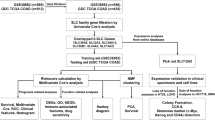
Frequencies of SLC22A18 missense variants
We examined common missense variants of SLC22A18 using data from the Database of Single Nucleotide Polymorphisms (dbSNP) of the National Center for Biotechnology Information (NCBI) (https://www.ncbi.nlm.nih.gov/snp/) and identified four variants, namely p.Ala6Thr (rs1048046), p.Arg12Gln (rs1048047), p.Arg86His (rs78838117), and p.Trp324Cys (rs1129782). Subsequently, the frequencies of these variants in four different ethnic groups—661 Africans, 347 North Americans, 504 East Asians, and 503 Europeans—were obtained using frequency data from the 1000 Genomes Project (phase 3; https://www.ensembl.org/; Table 1). The wild type SLC22A18 mRNA sequence was based on the reference SLC22A18 mRNA sequence (GenBank accession number NM_183233.3).
Effects of SLC22A18 variations on its expression
We constructed vectors encoding wild type SLC22A18 or four variants and generated separate stable cell lines expressing each gene. Subsequently, we investigated the expression levels of the wild type SLC22A18 protein and each variant via surface biotinylation assays. Three of the four missense variants—p.Ala6Thr, p.Arg12Gln, and p.Arg86His—showed significantly decreased SLC22A18 expression, with the expression levels of the p.Ala6Thr, p.Arg12Gln, and p.Arg86His variants being 27.6, 43.0, and 69.5% lower in HCT-116 cells, respectively, than that of the wild type (Fig. 1a). Significant expression decreases (32.8, 43.1, and 65.5%, respectively) were also observed in SW620 cells (Fig. 1b). The expression of p.Trp324Cys was comparable with that of the wild type in both types of cells (Fig. 1). Additionally, we examined the effect of each variant on SLC22A18 mRNA expression using quantitative real-time polymerase chain reaction (qRT-PCR) analysis. We observed that the mRNA expression levels of the variants were comparable with that of the wild type (Supplementary Fig. 3). These results indicate that the decreased SLC22A18 expression of the three variants has resulted from post-transcriptional events.
Effect of SLC22A18 variants on SLC22A18 expression. A surface biotinylation assay was conducted using HCT-116 (a) or SW620 (b) cells stably expressing wild type SLC22A18 or the its variant. Cropped images are displayed in this figure, and full-length images are presented in Supplementary Fig. 1. The data are presented as the mean ± standard deviation (SD) of three independent experiments analyzed using one-way analysis of variance followed by Dunnett’s two-tailed test; **p < 0.01, ***p < 0.001 versus wild type. EV, empty vector.
To elucidate the mechanisms underlying the reduced membrane expression of SLC22A18 variants, we conducted immunoblotting following pre-treatment with MG132 (a proteasomal proteolysis inhibitor) and bafilomycin A1 (a lysosomal degradation inhibitor). Post-MG132 treatment, the expression levels of the p.Ala6Thr, p.Arg12Gln, and p.Arg86His variants in HCT-116 cells recovered to 91.0%, 95.6%, and 92.6%, respectively, compared with that of the wild type (Fig. 2a). Additionally, the expression of these variants in HCT-116 cells recovered to 96.6%, 99.1%, and 91.8%, respectively, of that of the wild type after bafilomycin A1 treatment (Fig. 2b). In SW620 cells, expression of the p.Ala6Thr, p.Arg12Gln, and p.Arg86His variants significantly recovered to 94.9%, 95.6%, and 91.0%, respectively, following MG132 treatment (Fig. 2c) and to 99.6%, 95.9%, and 89.1%, respectively, after bafilomycin A1 treatment (Fig. 2d). Our findings suggest that p.Ala6Thr, p.Arg12Gln, and p.Arg86His are susceptible to intracellular degradation, and the diminished expression of these SLC22A18 variants may be attributed to proteasomal or lysosomal degradation. Additionally, we performed immunofluorescence staining to confirm the expression of the SLC22A18 variants on the plasma membrane. We observed that the SLC22A18 expression of the three variants, p.Ala6Thr, p.Arg12Gln, and p.Arg86His, was decreased on the plasma membranes of both HCT-116 and SW620 cells (Fig. 3a,b, respectively). Expression of the p.Arg86His variant was particularly decreased. Larger factions of the p.Ala6Thr and p.Arg12Gln variants were present in the endoplasmic reticulum compared with that of the wild type.
Effect of MG132 or bafilomycin A1 on SLC22A18 expression. Immunoblotting was performed following treatment with MG132 (a, c) or bafilomycin A1 (b, d) using stable HCT-116 (a, b) or SW620 (c, d) cells. Images were cropped, and full-length blots are presented in Supplementary Fig. 2. Data are presented as the mean ± SD of three independent experiments as determined using Student’s t-test; *p < 0.05, **p < 0.01, ***p < 0.001 versus native SLC22A18 expression without MG132 or bafilomycin A1 treatment. EV, empty vector.
Effects of SLC22A18 variants on the proliferation, migration, and invasion of colon cancer cells
We conducted colony formation, wound healing, and invasion assays to investigate whether the SLC22A18 variants might affect the proliferation, migration, and invasion of colon cancer cells. Colony formation was dramatically lower in HCT-116 and SW620 cells expressing wild type SLC22A18 than in those expressing the empty vector (Fig. 4a,b, respectively). These results are consistent with previous findings showing that SLC22A18 can suppress colorectal cancer15. The p.Ala6Thr, p.Arg12Gln, and p.Arg86His showed 1.8-, 2.1-, and 2.9-fold higher colony formation, respectively, than that of the wild type in HCT-116 cells (Fig. 4a). In addition, the variants in SW620 cells increased colony formation by 2.0-, 2.3-, and 3.0-fold, respectively, relative to the wild type (Fig. 4b). Our wound healing assays revealed that post-scratch wound coverage was lower in HCT-116 cells expressing the wild type protein (12.0%) compared with that of the empty vector (54.9%) (Fig. 5a). Similar results were observed in experiments with SW620 cells (9.3% and 49.5% coverage, respectively; Fig. 5b). In HCT-116 cells, the p.Ala6Thr, p.Arg12Gln, and p.Arg86His variants significantly increased wound coverage by 26.0%, 30.8%, and 54.8%, respectively (Fig. 5a). In SW620 cells, the respective wound coverages increased significantly to 16.9%, 20.9%, and 47.0%, respectively (Fig. 5b). Finally, we observed that invasion was markedly lower with HCT-116 or SW620 cells expressing the wild type protein than the empty vector (Fig. 6). The p.Ala6Thr, p.Arg12Gln, and p.Arg86His variants significantly increased HCT-116 cell invasion by 1.7-, 2.0-, and 2.5-fold, respectively, compared with that of wild type protein (Fig. 6a). In SW620 cells, the variants increased cell invasion by 5.1-, 6.4-, and 10.9-fold, respectively, compared with that of the wild type (Fig. 6b).
Effects of SLC22A18 variants on the proliferation of colon cancer cells. Stable HCT-116 (a) or SW620 (b) cells were cultured for 10 days, the colonies were stained with crystal violet solution, and the colonies were counted. Data are presented as the mean ± SD of three independent experiments as determined via one-way analysis of variance followed by Dunnett’s two-tailed test; ###p < 0.001 versus empty vector; ***p < 0.001 versus wild type.
Effects of SLC22A18 variants on the migration of colon cancer cells. Stable HCT-116 (a) or SW620 (b) cells were cultured to 80–90% confluency, and the monolayers were gently scratched with a scratcher. Images were acquired after 0, 24, and 48 h. Data after 48 h are presented as the mean ± SD of three independent experiments, as determined via one-way analysis of variance followed by Dunnett’s two-tailed test; ###p < 0.001 versus empty vector; *p < 0.05, ***p < 0.001 versus wild type.
Effects of SLC22A18 variants on the invasion of colon cancer cells. After incubating stable HCT-116 (a) or SW620 (b) cells on inserts in invasion chambers for 48 h, they were stained with the staining solution for 20 min. Subsequently, the number of cells was counted. Data are presented as the mean ± SD of three independent experiments, as determined via one-way analysis of variance followed by Dunnett’s two-tailed test; ##p < 0.01, ###p < 0.001 versus empty vector; **p < 0.01, ***p < 0.001 versus wild type.
Effects of the SLC22A18 variants on oxaliplatin sensitivity
A previous report showed that low SLC22A18 expression correlated significantly with oxaliplatin resistance17. In this study, we examined the effects of the SLC22A18 variants on oxaliplatin sensitivity by performing cell viability assays after treatment of various doses (0, 150, and 300 µM) of oxaliplatin. Then, the cell viabilities observed with 150 or 300 µM oxaliplatin were calculated and statistically analyzed relative to those observed in the absence of oxaliplatin. The viability of cells expressing the wild type protein was significantly lower than that of empty vector. Two variants (p.Arg12Gln and p.Arg86His) were associated with significantly increased cell viabilities than the wild type. The viability of cells expressing the p.Ala6Thr variant tended to be higher than that of cells expressing the wild type protein, and this difference was statistically significant after treatment with 300 µM oxaliplatin, whereas p.Trp324Cys and wild type showed similar viabilities (Fig. 7).
Effects of SLC22A18 variants on the sensitivity to oxaliplatin. Various doses (0, 150, or 300 µM) of oxaliplatin were added to stable HCT-116 (a) or SW620 (b) cells. After 24 h, cell viability assays were performed. Data are presented as the mean ± SD of three independent experiments, as determined via one-way analysis of variance followed by Dunnett’s two-tailed test; ##p < 0.01, ###p < 0.001 versus empty vector; *p < 0.05, **p < 0.01, ***p < 0.001 versus wild type.
Discussion
Various SLC transporters are expressed in the digestive system, wherein they help maintain normal physiological functions by transporting various molecules, such as ions, metals, glucose, amines, and amino acids18,19,20. Many previous reports showed significant associations between SLC transporters and the occurrence and prognosis of digestive system cancers4. In particular, many SLC transporters, such as SLC5A8, SLC11A2, SLC12A2, SLC12A5, SLC22A18, SLC25A22, SLC26A2, SLC26A3, and SLC40A1, have been associated with colorectal cancer15,21,22,23,24,25,26,27,28. Among them, SLC5A8, SLC22A18, SLC26A3, and SLC40A1 were either downregulated in colorectal cancer or found to protect against colorectal cancer by acting as tumor suppressors15,21,22,27,28,29. The remaining transporters are known for being overexpressed in colorectal cancer or being associated with the progression and poor prognosis of colorectal cancer23,24,26,30,31.
Although many investigators have commented on the association between SLC transporters and digestive system cancers, few have revealed the roles played by different transporters in the occurrence or progression of cancer. The tumor-suppressor role played by SLC5A8 in colorectal cancer is one example of a known mechanism. SLC5A8 transports bacterial products (butyrate and propionate) and a ubiquitous metabolite (pyruvate) within the body. Evidently, the SLC5A8 transporter ultimately helps suppress colorectal cancer by transporting these substances, which inhibit histone deacetylase in cancer cells29,32,33,34,35,36. In contrast to SLC5A8, SLC25A22 reportedly plays a tumor-promoter role in colorectal cancer. Wong et al.25 revealed that SLC25A22 was essential for the biosynthesis of aspartate, which metabolizes into asparagine, an amino acid involved in the migration of colorectal cancer cells via the mitogen-activated protein kinase (MEK)/extracellular-signal-regulated kinase (ERK) pathway. Another metabolite of aspartate, oxaloacetate (which promotes intracellular glycolysis and reduces oxidative stress), is also involved in the proliferation and survival of colorectal cancer cells. In addition, SLC25A22 promoted the development and metastasis of colon cancer in mice, and colorectal cancer patients overexpressing SLC25A22 have a shorter survival time than patients with low SLC25A22 expression.
Several previous reports showed that SLC22A18 may suppress various cancers, including prostatic cancer, Wilms’ tumor, glioma, breast cancer, and colorectal cancer10,11,12,13,14,15. A previous report showed that SLC22A18 expression was significantly lower in patients with colorectal cancer and that low SCL22A18 expression correlated with lower long-term survival in these patients15. In this report, the authors also revealed that SLC22A18 inhibited colony formation by colon cancer cells and induced cell-cycle arrest in the G2/M phase. Furthermore, SL22A18 inhibited the growth of HCT-116 xenograft tumors in a mouse model. Recently, another report showed that low SLC22A18 expression in patients with colorectal cancer correlated significantly with oxaliplatin resistance and that this resistance could be overcome by inhibiting the ERK pathway17.
In this study, we examined the expression levels of four missense variants of SLC22A18 and their effects on the progression of colon cancer cells. We observed that three variants—p.Ala6Thr, p.Arg12Gln, and p.Arg86His—had significantly lower cell expression than the wild type, and these variants increased the proliferation, migration, and invasion of colon cancer cells. Our results are consistent with those of a previous report indicating that SLC22A18 may suppress colorectal cancer15. Furthermore, we observed that p.Ala6Thr, p.Arg12Gln, and p.Arg86His significantly affected the sensitivity of cells to oxaliplatin. Therefore, disease progression and responses to oxaliplatin in patients with colorectal cancer may vary depending on the presence or absence of SLC22A18 variants. To confirm this possibility, additional analysis of clinical patient data based on genetic variations will be necessary.
Screening for colorectal cancer via colonoscopy has reduced the incidence and mortality rates of colorectal cancer by approximately 40–60%, respectively37,38,39. Recently published statistical data indicate that although the overall annual incidence of colorectal cancer appears to be slightly decreasing, it has been increasing by 1–2% per year in people under 55 years of age. Moreover, even though the overall mortality rate of colorectal cancer is decreasing every year, the mortality rates for people under 50 years of age have been increasing by 0.5 to 3% each year. Additionally, colorectal cancer is often diagnosed at more advanced stages than in the past2. Thus, to reduce the incidence and mortality rates of colorectal cancer, especially in people under 50–55 years of age, continual efforts should be undertaken to develop biomarkers that can help diagnose colorectal cancer more accurately and quickly, as well as more effective treatment methods. Numerous studies have been conducted to search for useful screening biomarkers for colorectal cancer, which have identified many molecular markers. For example, various types of microRNAs and long non-coding RNAs in blood or stool samples have been significantly correlated with colon cancer, and some tissue biomarkers (including caudal type homeobox 2, special AT-rich sequence-binding protein 2, and glycoprotein A33) have been identified. Recently, the methylated gene, septin 9 (mSEPT9) was approved by the Food and Drug Administration as a new biomarker for colorectal cancer40.
Several SLC transporters are either overexpressed or underexpressed in colorectal cancer, and differences in some of their expression have been associated with the prognoses of patients with colorectal cancer15,21,22,23,24,25,26,27,28,29,30,31. Therefore, genetic variants that significantly affect the expression or function of SLC transporters can be used as biomarkers for diagnosing or predicting the progression of colorectal cancer. In addition, as exemplified by the association between SLC22A18 and oxaliplatin resistance, genetic variants may be used to predict drug resistance or select drugs during chemotherapy in patients with colorectal cancer17.
To the best of our knowledge, this study is the first to investigate the effects of missense variants of SLC22A18 on transporter expression, colon cancer cell progression, and oxaliplatin sensitivity. Further studies are needed to evaluate the clinical utility of the variants that showed significant effects in vitro.
Methods
Genetic analysis of SLC22A18 missense variants
Data from the dbSNP of NCBI were used to identify common missense variants of SLC22A18. Next, the frequencies of each variant in four different ethnic groups were obtained from the 1,000 Genomes Project (phase 3). The numbers of people represented in each group, the population descriptions, and the population codes are as follows: 661 Africans (African Caribbean in Barbados [ACB], African Ancestry in Southwest US [ASW], Esan in Nigeria [ESN], Gambian in Western Division, The Gambia–Mandinka [GWD], Luhya in Webuye, Kenya [LWK], Mende in Sierra Leone [MSL], and Yoruba in Ibadan, Nigeria [YRI]); 347 Americans (Colombian in Medellin, Colombia [CLM], Mexican Ancestry in Los Angeles, California [MXL], Peruvian in Lima, Peru [PEL], and Puerto Rican in Puerto Rico [PUR]]; 504 east Asians (Chinese Dai in Xishuangbanna, China [CDX], Han Chinese in Beijing, China [CHB], Han Chinese South [CHS], Japanese in Tokyo, Japan [JPT], and Kinh in Ho Chi Minh City, Vietnam [KHV]); and 503 Europeans [Utah residents with Northern and Western European ancestry [CEU], Finnish in Finland [FIN], British in England and Scotland [GBR], Iberian populations in Spain [IBS], and Toscani in Italy [TSI]).
Plasmid construction
Complementary DNA (cDNA) encoding wild type SLC22A18 (SC319659, OriGene) was subcloned into the p3XFLAG-CMV vector. The variant-bearing plasmids were generated using a QuikChange® II Site-Directed Mutagenesis Kit (Agilent Technologies). The sequences of all primers used for plasmid construction are listed in Supplementary Table 1. The DNA sequences of all plasmids were confirmed via direct sequencing.
Selection of stable cell lines
To generate cell lines stably expressing wild type SLC22A18 or its variants, plasmids encoding wild type SLC22A18 or its variants were separately transfected into HCT-116 (human colorectal carcinoma) or SW620 (human Caucasian colon adenocarcinoma) cells (Korean Cell Line Bank, Korean Cell Line Research Foundation) using the Lipofectamine® LTX and Plus™ reagents (Invitrogen Corporation). The cells were then cultured for 5 days in medium containing 8 mg/ml of neomycin antibiotic G418 (InvivoGen). Individual colonies were isolated and cultured with decreasing concentrations of G418.
Surface biotinylation assay
Biotinylation assays were performed using a Cell Surface Protein Isolation Kit (Thermo Fisher Scientific) according to the manufacturer’s protocol. A rabbit polyclonal anti-Na+/K+ ATPase α-1 antibody (Merck) was used as an internal standard. The signal was acquired using ImageQuant LAS 4000 mini (GE Healthcare), and the intensity of each band was measured using ImageJ software (National Institute of Health).
Immunoblotting
Immunoblotting was performed using a mouse anti-FLAG M2 primary antibody (Sigma-Aldrich) or a rabbit anti-β-actin antibody (Merck). Cells were treated with 10 µM MG132 (Sigma-Aldrich) or 10 nM bafilomycin A1 (MedChemExpress) at 24 h post-transfection to examine their effects on expression of the SLC22A18 variants. Signals were obtained using an ImageQuant LAS 4000 mini, and the intensity of each band was measured using ImageJ software.
qRT-PCR analysis
Total RNA was extracted from cells with TRIzol (Invitrogen Corporation) according to the manufacturer’s protocol. Subsequently, reverse transcription was performed using 1 µg of RNA and the iScript cDNA Synthesis Kit (Bio-Rad). mRNA expression of wild type SLC22A18 or each variant was analyzed via qRT-PCR. qRT-PCR was conducted with SYBR Green Real-time PCR Master Mix (Toyobo) and QuantStudio™ 3 Real-Time PCR machine (Thermo Fisher Scientific). mRNA expression levels were normalized to that of GAPDH mRNA. The sequences of the primers used for the qRT-PCR step (Cosmogenetech) are shown in Supplementary Table 1.
Immunofluorescence
HCT-116 or SW620 stable cells were grown in 4-well chamber slides (Thermo Fisher Scientific) and allowed to attach for 1 day. Cells were fixed and permeabilized with 100% methanol (prechilled at − 20 °C) at room temperature for 5 min and blocked with 1% bovine serum albumin for 1 h. Then, the cells were incubated with anti-FLAG M2, anti-BiP (Abcam), or anti-giantin (Abcam) antibodies. After washing cells with phosphate-buffered saline (PBS), they were incubated with secondary Alexa Fluor® 488-conjugated rabbit anti-mouse IgG or Alexa Fluor® 594-conjugated goat anti-rabbit IgG (Thermo Fisher Scientific) antibodies. Nucleic acids were stained with 4′,6-diamidino-2-phenylindole (Vector Laboratories). Images were acquired using a confocal laser-scanning microscope and analyzed using an LSM image examiner (Carl Zeiss).
Colony formation assay
Stable HCT-116 or SW620 cells were seeded into 6-well plates (500 cells/well) and cultured for 10 days. The cells were then washed with PBS and fixed with methanol and acetic acid. The colonies were stained with crystal violet solution (Sigma-Aldrich) for 30 min at room temperature, and then the colonies were counted.
Wound healing assay
Stable HCT-116 or SW620 cells were cultured to 80–90% confluence, after which their monolayers were gently scratched with a scratcher (SPL Lifesciences), and the floating cells were removed. Images were acquired using an IN300T-FL microscope (AmScope) after 0, 24, and 48 h.
Cell invasion assay
Cell invasion was studied using a QCM ECMatrix Cell Invasion Assay, 24-Well (8 µm), Colorimetric Kit (EMD Millipore) according to the manufacturer’s protocol. Briefly, after incubating stable HCT-116 or SW620 cells on the inserts in invasion chambers for 48 h, they were stained with 500 µl of staining solution for 20 min. Finally, the number of cells was counted under an inverted microscope (TE-300, Nikon).
Cell viability assay after oxaliplatin treatment
Stable HCT-116 or SW620 cells were grown in 96-well plates. Various doses (0, 150, or 300 µM) of oxaliplatin (Sigma-Aldrich) were added to the HCT-116 or SW620 cells growing in the 96-well plates. After 24 h, cell viabilities were measured using Cell Counting Kit-8 (Dojindo Laboratories).
Statistical analyses
Statistical analyses were performed using GraphPad Prism 8.0 (GraphPad Software). We calculated p values to compare the results obtained before and after MG132 or bafilomycin A1 treatment using Student’s t-test. Other p values were calculated using one-way analysis of variance, followed by Dunnett’s two-tailed test. The threshold for statistical significance was set to p < 0.05.
Data availability
All data generated or analyzed during the current study are included in this article (and its supplementary information files).
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
Siegel, R. L., Wagle, N. S., Cercek, A., Smith, R. A. & Jemal, A. Colorectal cancer statistics, 2023. CA Cancer J. Clin. 73, 233–254. https://doi.org/10.3322/caac.21772 (2023).
Nwosu, Z. C., Song, M. G., di Magliano, M. P., Lyssiotis, C. A. & Kim, S. E. Nutrient transporters: Connecting cancer metabolism to therapeutic opportunities. Oncogene 42, 711–724. https://doi.org/10.1038/s41388-023-02593-x (2023).
Xie, J., Zhu, X. Y., Liu, L. M. & Meng, Z. Q. Solute carrier transporters: Potential targets for digestive system neoplasms. Cancer Manag. Res. 10, 153–166. https://doi.org/10.2147/CMAR.S152951 (2018).
Park, Y. Y. et al. Yes-associated protein 1 and transcriptional coactivator with PDZ-binding motif activate the mammalian target of rapamycin complex 1 pathway by regulating amino acid transporters in hepatocellular carcinoma. Hepatology 63, 159–172. https://doi.org/10.1002/hep.28223 (2016).
Chen, C. F. et al. Overlapping high-resolution copy number alterations in cancer genomes identified putative cancer genes in hepatocellular carcinoma. Hepatology 52, 1690–1701. https://doi.org/10.1002/hep.23847 (2010).
Reece, M. et al. Functional characterization of ORCTL2—An organic cation transporter expressed in the renal proximal tubules. FEBS Lett. 433, 245–250. https://doi.org/10.1016/s0014-5793(98)00907-7 (1998).
Bajaj, V., Singhmar, P. & Kumar, A. Promoter characterization and regulation of expression of an imprinted gene SLC22A18AS. Gene 424, 40–47. https://doi.org/10.1016/j.gene.2008.07.032 (2008).
Ali, A. M., Bajaj, V., Gopinath, K. S. & Kumar, A. Characterization of the human SLC22A18 gene promoter and its regulation by the transcription factor Sp1. Gene 429, 37–43. https://doi.org/10.1016/j.gene.2008.10.004 (2009).
Jacobs, D. I., Mao, Y., Fu, A., Kelly, W. K. & Zhu, Y. Dysregulated methylation at imprinted genes in prostate tumor tissue detected by methylation microarray. BMC Urol. 13, 37. https://doi.org/10.1186/1471-2490-13-37 (2013).
Abdel-Monem, M. M. et al. Gene expression analysis and the risk of relapse in favorable histology Wilms’ tumor. Arab. J. Urol. 21, 45–51. https://doi.org/10.1080/2090598X.2022.2127202 (2023).
Chu, S. H. et al. Promoter methylation and downregulation of SLC22A18 are associated with the development and progression of human glioma. J. Transl. Med. 9, 156. https://doi.org/10.1186/1479-5876-9-156 (2011).
Chu, S. H. et al. Correlation of low SLC22A18 expression with poor prognosis in patients with glioma. J. Clin. Neurosci. 19, 95–98. https://doi.org/10.1016/j.jocn.2011.04.032 (2012).
Ito, S., Fujino, Y., Ogata, S., Hirayama-Kurogi, M. & Ohtsuki, S. Involvement of an orphan transporter, SLC22A18, in cell growth and drug resistance of human breast cancer MCF7 cells. J. Pharm. Sci. 107, 3163–3170. https://doi.org/10.1016/j.xphs.2018.08.011 (2018).
Jung, Y. et al. Characterization of SLC22A18 as a tumor suppressor and novel biomarker in colorectal cancer. Oncotarget 6, 25368–25380. https://doi.org/10.18632/oncotarget.4681 (2015).
Mohelnikova-Duchonova, B. et al. The association between the expression of solute carrier transporters and the prognosis of pancreatic cancer. Cancer Chemother. Pharmacol. 72, 669–682. https://doi.org/10.1007/s00280-013-2246-2 (2013).
Kim, T. W. et al. Expression of SLC22A18 regulates oxaliplatin resistance by modulating the ERK pathway in colorectal cancer. Am. J. Cancer Res. 12, 1393–1408 (2022).
Li, Y., Lu, J. & Paxton, J. W. The role of ABC and SLC transporters in the pharmacokinetics of dietary and herbal phytochemicals and their interactions with xenobiotics. Curr. Drug Metab. 13, 624–639. https://doi.org/10.2174/1389200211209050624 (2012).
Colas, C., Ung, P. M. & Schlessinger, A. SLC transporters: Structure, function, and drug discovery. MedChemComm 7, 1069–1081. https://doi.org/10.1039/C6MD00005C (2016).
Chan, K. et al. Loss of function mutation of the Slc38a3 glutamine transporter reveals its critical role for amino acid metabolism in the liver, brain, and kidney. Pflugers Arch. 468, 213–227. https://doi.org/10.1007/s00424-015-1742-0 (2016).
Gurav, A. et al. Slc5a8, a Na+-coupled high-affinity transporter for short-chain fatty acids, is a conditional tumour suppressor in colon that protects against colitis and colon cancer under low-fibre dietary conditions. Biochem. J. 469, 267–278. https://doi.org/10.1042/BJ20150242 (2015).
Chua, A. C. et al. Dietary iron enhances colonic inflammation and IL-6/IL-11-Stat3 signaling promoting colonic tumor development in mice. PLoS ONE 8, e78850. https://doi.org/10.1371/journal.pone.0078850 (2013).
Zhang, Y. et al. Quantitative proteome analysis of colorectal cancer-related differential proteins. J. Cancer Res. Clin. Oncol. 143, 233–241. https://doi.org/10.1007/s00432-016-2274-5 (2017).
Xu, L. et al. Increased expression of Solute carrier family 12 member 5 via gene amplification contributes to tumour progression and metastasis and associates with poor survival in colorectal cancer. Gut 65, 635–646. https://doi.org/10.1136/gutjnl-2014-308257 (2016).
Wong, C. C. et al. SLC25A22 promotes proliferation and survival of colorectal cancer cells with KRAS mutations and xenograft tumor progression in mice via intracellular synthesis of aspartate. Gastroenterology 151, 945-960 e946. https://doi.org/10.1053/j.gastro.2016.07.011 (2016).
Pitule, P. et al. Differential expression and prognostic role of selected genes in colorectal cancer patients. Anticancer Res. 33, 4855–4865 (2013).
Chapman, J. M., Knoepp, S. M., Byeon, M. K., Henderson, K. W. & Schweinfest, C. W. The colon anion transporter, down-regulated in adenoma, induces growth suppression that is abrogated by E1A. Cancer Res. 62, 5083–5088 (2002).
Schweinfest, C. W. et al. slc26a3 (dra)-deficient mice display chloride-losing diarrhea, enhanced colonic proliferation, and distinct up-regulation of ion transporters in the colon. J. Biol. Chem. 281, 37962–37971. https://doi.org/10.1074/jbc.M607527200 (2006).
Bhutia, Y. D. et al. SLC transporters as a novel class of tumour suppressors: Identity, function and molecular mechanisms. Biochem. J. 473, 1113–1124. https://doi.org/10.1042/BJ20150751 (2016).
Lauriola, M. et al. Identification by a digital gene expression displayer (DGED) and test by RT-PCR analysis of new mRNA candidate markers for colorectal cancer in peripheral blood. Int. J. Oncol. 37, 519–525. https://doi.org/10.3892/ijo_00000701 (2010).
Ostasiewicz, B., Ostasiewicz, P., Dus-Szachniewicz, K., Ostasiewicz, K. & Ziolkowski, P. Quantitative analysis of gene expression in fixed colorectal carcinoma samples as a method for biomarker validation. Mol. Med. Rep. 13, 5084–5092. https://doi.org/10.3892/mmr.2016.5200 (2016).
Miyauchi, S., Gopal, E., Fei, Y. J. & Ganapathy, V. Functional identification of SLC5A8, a tumor suppressor down-regulated in colon cancer, as a Na(+)-coupled transporter for short-chain fatty acids. J. Biol. Chem. 279, 13293–13296. https://doi.org/10.1074/jbc.C400059200 (2004).
Coady, M. J. et al. The human tumour suppressor gene SLC5A8 expresses a Na+-monocarboxylate cotransporter. J. Physiol. 557, 719–731. https://doi.org/10.1113/jphysiol.2004.063859 (2004).
Gupta, N., Martin, P. M., Prasad, P. D. & Ganapathy, V. SLC5A8 (SMCT1)-mediated transport of butyrate forms the basis for the tumor suppressive function of the transporter. Life Sci. 78, 2419–2425. https://doi.org/10.1016/j.lfs.2005.10.028 (2006).
Thangaraju, M., Carswell, K. N., Prasad, P. D. & Ganapathy, V. Colon cancer cells maintain low levels of pyruvate to avoid cell death caused by inhibition of HDAC1/HDAC3. Biochem. J. 417, 379–389. https://doi.org/10.1042/BJ20081132 (2009).
Ganapathy, V. et al. Sodium-coupled monocarboxylate transporters in normal tissues and in cancer. AAPS J. 10, 193–199. https://doi.org/10.1208/s12248-008-9022-y (2008).
Zauber, A. G. et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N. Engl. J. Med. 366, 687–696. https://doi.org/10.1056/NEJMoa1100370 (2012).
Nishihara, R. et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N. Engl. J. Med. 369, 1095–1105. https://doi.org/10.1056/NEJMoa1301969 (2013).
Doubeni, C. A. et al. Effectiveness of screening colonoscopy in reducing the risk of death from right and left colon cancer: A large community-based study. Gut 67, 291–298. https://doi.org/10.1136/gutjnl-2016-312712 (2018).
Zygulska, A. L. & Pierzchalski, P. Novel diagnostic biomarkers in colorectal cancer. Int. J. Mol. Sci. https://doi.org/10.3390/ijms23020852 (2022).
Acknowledgements
This work was supported by the National Research Foundation of Korea grants funded by the Korean government (MSIT) (2020R1A5A2019210 and NRF-2019R1F1A1054449).
Author information
Authors and Affiliations
Contributions
J.H.C. designed the study. H.S.S., S.Y.H., J.Y.K., and M.K. performed the experiments and analyzed the data. H.S.S. and J.H.C. wrote the manuscript. All the authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, H.S., Ha, S.Y., Kim, JY. et al. The effect of genetic variants of SLC22A18 on proliferation, migration, and invasion of colon cancer cells. Sci Rep 14, 3925 (2024). https://doi.org/10.1038/s41598-024-54658-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54658-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.