Abstract
The changes in aging plus the pathology of diseases can influence the changes in severity levels. This study aimed to examine the changes in levels of severity in patients while waiting to see a doctor. The study was conducted at an outpatient clinic in northeastern Thailand with a total of 421 patients who were assessed twice for levels of severity using the Emergency Severity Index. The 38 triage nurses screened patients, and 18 were interviewed when severity level changes were observed. Data were collected April 1–30, 2021. Quantitative data were analyzed by Chi-square test, Fisher's exact test, and logistic regression. Qualitative data were analyzed by content analysis. Most patients were female, between 18 and 59 years old. Most patients did not change their level of severity. However, increasing levels of severity were found in older adults. Factors related to the changes in severity levels were age group, chronic disease, chief complaint, educational level, the duration of travel to the outpatient clinic, type of vehicle, aging process and comorbidity, pathology of diseases, reassessment interval, nurse's experience, bypassing the patient triage process, patient's self-preparation, management of triage nurses, and assignment of direct healthcare staff until the end of the treatment. Increased severity was more frequently found in older adults, so closely monitored during waiting times at a clinic is needed. Setting rescreening as a policy and having sensitive screening guidelines and tools specific to older adults would contribute to early detection and immediate treatment of deteriorating symptoms and illness to help reduce complications and morbidity.
Trial registration: https://osf.io/fp3j2.
Similar content being viewed by others
Introduction
As people age, the signs and symptoms of illness and responses to treatment are affected by the normal physiological changes of the aging process. These changes and responses in older people become more pronounced during illness and can be differentiated from those of adults1. When nurses need to evaluate an older person, there is an acronym that helps to remind them what to consider in the assessment. The acronym RAMPS describes five clinical features associated with aging in older adults who present with an illness: R is for the reduced body reserve in which there is a decline in the body’s energy reserve; A is for the atypical presentation of signs and symptoms for various diseases that are nonspecific to older adults; M is for the multiple pathologies and chronic problems that may be present; P is for polypharmacy or the concurrent use of multiple medications; and S is for the social adversities or unfavorable social changes that may occur as a consequence of aging2.
Background
The changes in aging associated with RAMPS, especially an atypical presentation and reduced body reserve, can influence the nurses’ assessment and determination of a level of illness severity. The atypical presentation in older adults may differ from adults and affect patient screening. For example, pneumonia without fever or acute myocardial infarction without chest pain complicates problem identification in making a diagnosis. Older adults with reduced body reserve become sick more easily, report more severe or worsening symptoms, and experience fluctuations in their symptoms. When older adults are waiting for medical care services, their instability of symptoms can influence nurses’ assessments of severity levels compared to adults in a similar situation1,3.
A common issue for health care in outpatient clinics and hospital emergency services is the crowding and congestion of people waiting to be seen. This occurs when the immediate demand for health care services exceeds the supply of medical resources. In these situations, healthcare service capacity is limited. For example, the ratio of patients to populations who visited emergency rooms in 2020 was 421:1,000 in the United States, 412:1,000 in England, 331:1,000 in Australia, and 458:1,000 in Thailand4. In the same year, patients in Thailand visited outpatient departments 164 million times, for an average of 3.45 times/person/year, or approximately 679 per 1,000 population5. These large numbers resulted in congestion in service areas and a delay in receiving medical treatment. Outpatient clinics have particularly longer wait times than emergency departments, and this may result in a change in symptoms in older adults and an increase in illness severity and mortality outcomes6,7.
Triage nurses need to be able to distinguish the differences between adults and older adults during classifying their severity of illness because it is easier for older adults to experience changes in levels of severity while waiting for treatment7,8. Lack of staff, insufficient resources, and the congestion of patients due to longer wait times may directly affect changes in levels of illness severity for this group7,8,9. Changes in symptoms and illness severity may lead to increased complications, morbidity, and mortality8,10. This is particularly true for older adults for whom an assessment is likely to show that the levels of severity can easily change from non-urgent to emergency and resuscitation11.
In Thailand, most hospitals have triage zones for prioritizing the patients’ level of care on arrival, including those with outpatient clinic appointments5. If patients have an existing clinical appointment and immediate care is not required, a nurse will perform a second assessment, either immediately or after waiting for the results of laboratory tests. Changes in severity are a known occurrence between initial triage and reassessment. Because it can be difficult for nurses to accurately assess symptoms that fluctuate, changes in severity can easily occur during the time interval. For older adults who are susceptible to RAMPS, the changes in levels of severity between the two assessment periods may cause problems with treatment planning at the clinic1,11.
Older adults over 65 years of age may have some alterations in their physical conditions, organ functions, and a weakened immune system12. One large outpatient department in northeastern Thailand reported the following numbers and percentages of patients who changed their levels of severity from non-urgency to emergency between the first and second assessment: 186 (0.48%), 261 (0.64%), and 413 (0.98%) in 2017, 2018, and 2019 fiscal years, respectively. Among those annual numbers, there were 98 (52.7%), 155 (59.4%), and 321 (77.9%) older adults13. During the three years, there were three non-urgent older adults whose symptoms deteriorated and required resuscitation while in the clinic’s waiting area. Although that number was low, the impact was substantial.
Other than internal hospital documents, there is little research in the published literature that explores to what extent adult and older adult patients change in severity levels and the factors related to those changes. Only the quantitative study might partially fill the gap; however, the qualitative study can answer both what and how questions. When the levels of severity change, the factors related to that change should be explored and guided for future prevention. The combination design can shed light on levels of severity change and factors related to those changes. The results from this study will guide policy change regarding the rescreening system and improve the triage system by increasing the quality of triage service for patients, especially older adults. Finally, we conducted this study to explore the factors related to severity change by applying the embedded mixed-method study.
Aims
This study aimed to examine the incidence and changes in levels of illness severity in adult and older adult patients at an outpatient clinic. Factors related to the changes in levels of illness severity will also be explored.
Methods
Design
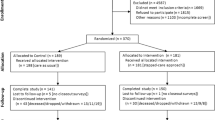
This study took an embedded mixed-method approach by first examining quantitative data collected from patients using research instruments to explore the severity level and its changes. Then, interviews with triage/assessment registered nurses (RNs) were conducted using open-ended questions in case severity changes were found to explore factors associated with the changes and provide complete reasons to answer the research questions and clarify the level of severity change phenomenon.
Setting and sampling
The population of interest was adult and older adult patients who had scheduled clinic appointments at an outpatient internal medicine clinic from a large tertiary regional hospital in northeastern Thailand. A systematic random sample of patients (every other person) was drawn. The level of illness severity was firstly assessed at a hospital’s triage zone and secondly assessed at the internal medicine clinic by triage RNs. To ensure the triage nurse can provide the same screening quality, they should be trained, and interrater reliability should be demonstrated before conducting this study. The triage RNs had completed the Thai Ministry of Public Health’s two-day triage education training course and reached 93% agreement on severity screening (interrater reliability between 92 and 94%).
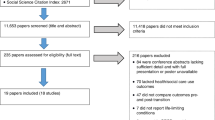
The sample size was calculated using a formula to estimate the proportion of the population with a 1.96 confidence coefficient. The proportion of patients with changes in levels of severity from a similar study was 0.476, with a tolerance of 0.05, and statistical significance set at the 0.05 level14. After including 10% to account for potential missing data, the estimated sample size was 421 participants, 220 adults (52.3%) and 201 older adults (47.7%). The proportion of adults to older adults was divided based on the proportion of those who received treatment at this clinic13.
Inclusion criteria were (a) patients aged ≥ 18 years with any health conditions, (b) triaged two times by an RN, and (c) willingness to participate in the study. The exclusion criterion was an unwillingness or inability to provide complete information.
For the qualitative data, inclusion criteria were triage nurses at the triage zone and the internal medicine clinic who gave informed consent to participate in the study. The exclusion criterion was an unwillingness or inability to provide complete information. Finally, The 18 triage nurses who found levels of severity changes were selected for interview. This criterion was set because these triage nurses could give information and details related to severity changes since they assessed the patients and had direct experience with patient severity level changes.
Ethical considerations
The research received approval from the Khon Kaen University Ethics Committees for Human Research based on the Declaration of Helsinki and the International Conference on Harmonization (ICH) Good Clinical Practice Guidelines. The Approval number was HE642016 on March 30, 2021. Following the ethical principles of the Declaration of Helsinki, the primary investigator provided research information, and the research assistant obtained the signed informed consent forms before data collection. Finally, the data were analyzed anonymously.
Measurements/instruments
Four research instruments were used to collect quantitative and qualitative data. An 8-item demographic data sheet collected patients’ personal and clinical data using fill-in-the-blank and a checklist. A second 8-item general questionnaire was completed by the triage RNs who assessed or reassessed the patients, also fill-in-the-blank and a checklist.
The third instrument was the Emergency Severity Index (ESI). The ESI version 4 is a triage tool to determine priorities for emergency services. The ESI consists of five levels of illness severity: 1 (Resuscitation), 2 (Emergency), 3 (Urgent), 4 (Semi-urgent), and 5 (Nonurgent). The interrater reliability with Cohen’s κ was 0.8915.
The fourth instrument was a semi-structured interview form to collect qualitative data. Two examples of open-ended questions were, “How did the severity of the patient change?” and “What were the causes of the change in severity?” All research instruments were proved by the five experts including two medical doctors, two emergency registered nurses, and one faculty member who is an expert in gerontological nursing which content validity indexes ranked between 0.90 and 1.00.
Data collection/procedure
From April 1 to April 30, 2021, the primary investigator collected data from adult and older adult patients during their first visit to the triage zone. Then, the second screening was performed at the outpatient internal medicine clinic. If a patient had a change in the level of illness severity, the primary investigator interviewed the RN, who recorded the severity change as soon as possible to find the reason or cause of severity level changes and explain the study phenomenon. This embedded mixed-method study was used to shed light on qualitative data to deeply understand not only the incidence and changes in levels of illness severity in adult and older adult patients at an outpatient clinic but also factors or reasons related to the changes in levels of illness severity will also be explored. Finally, the average interview time was approximately 30–60 min.
Data analysis
Quantitative data were analyzed using IBM® SPSS® version 28 under a university license. General information was analyzed using descriptive statistics, and relationships between characteristics of adults and older adults were calculated using Chi-square and Fisher’s exact tests. Three logistic regression models were performed to ascertain the effects of changes in the level of illness severity.
Qualitative data were the interviews transcribed verbatim from tape recordings. A mind-mapping software program assisted with content analysis in capturing the key points and identifying themes to understand and clarify the quantitative results.
Results
Demographic information
Patients' age ranged between 18 and 94 years. Most (52.0%) were female, 51.3% completed primary education, 33.6% came by ambulance, 43.2% came for clinic appointments, 51.5% had more than one chronic disease, the mean, median, and standard deviation of reassessment were 75.77, 62.00, and 37.50 min, respectively, the mean, median, and standard deviation of travel duration to the hospital were 75.00, 60.00, and 15.43 min, and 22.3% prepared unnecessary actions. Of 38 triage RNs, all were female and had bachelor's degrees, 55.3% aged 31–40 years, 95% had over ten years of service, 86.9% had never received specialized training except ESI training, 50% had experience in using the ESI tool, but about 5% had worked in the accident and emergency department (Table 1).
Patients’ triage assessments
The most common ESI levels for both adult and older adult patients for the first and second times were level 4 (n = 270 & n = 214, Nonurgent), followed by level 3 (n = 146 & n = 176, Semi-urgent), respectively (Table 2). The level of severity changes were divided into two subgroups: increased and decreased. Among the older adults, 89 (44.3%) increased their level of severity (Table 3).
Quantitative results
Factors related to changes in levels of severity
Older adults were over five times more likely to experience changes in severity than adult patients. Patients having more than one chronic disease, coming to the hospital when experiencing symptoms related to diseases, spending a longer travel time, reassessment interval over an hour, arriving by ambulance, and arriving after 12:01 for the triage, were more likely to have changes in levels of illness severity. Factors related to increased severity were also the same. Moreover, patients who were less educated were four times more likely to have increased levels of severity. Finally, factors related to decreased severity were older adults and having more than one chronic disease (Table 4).
Factors predicting levels of illness severity changes
The first logistic regression model was statistically significant and explained 23.2% (Nagelkerke R2) of the variance in the level of severity change and correctly classified 73.2% of cases. Factors with significant odds ratios affecting change in the level of illness severity were age (older adults), having more than one chronic disease, coming to the hospital when experiencing symptoms related to diseases, reassessment interval over an hour, and time of the reassessment later in the day/afternoon. A second logistic regression model examined factors associated with an increase in severity levels. The model was statistically significant and explained 33.3% (Nagelkerke R2) of the variance and correctly classified 76.2% of cases. Factors affecting an increase in severity level were being an older adult, coming to the hospital when experiencing symptoms related to diseases, reassessment interval over an hour, and the time of the reassessment. Unfortunately, the third logistic regression model examined neither being an older adult nor having a chronic disease was statistically significant (Table 5).
Qualitative findings: factors related to changes in levels of severity
Based on the quantitative results, the causes of levels of severity change were deeply explored to explain the phenomenon. Findings from quantitative results and the in-depth interview were merged into the themes to explain why they were changed in severity levels. These themes included the aging process and comorbidity, unstable illness, reassessment interval, nurses’ clinical experiences, bypassing the initial triage process, self-preparation of patients, management of triage RNs, and assigned nurse staff. The reasons and coding words for each theme were provided as follows.
Aging process and comorbidity
The quantitative results indicated that changes in severity levels, significantly increased levels, were found among older patients. In-depth interviews explored this change, and it found that atypical presentations associated with the five clinical features (RAMPS) were not detected in some older adults at the hospital’s triage zone and caused difficulties and inaccuracies in the RNs’ deciding the appropriate severity level. Changes were found because patients had a reduced energy reserve, multiple chronic diseases, and unclear symptoms at the time of admission.
This elderly patient with comorbidity did not show any obvious severe symptoms at first, but when waiting for the blood results, it was found that the symptoms were not the same--increased fatigue, drowsiness, and a thready pulse. We needed to send the patient to the emergency room. The risk is likely to come from the vulnerability of aging and comorbidity. Changes in symptoms can occur easily in older adults. (NU03056413)
Unstable illness
Changes in the levels of illness severity may have been caused by the unstable condition of the illness’ pathology, especially cardiovascular and respiratory diseases. The instability was likely to have increased the severity between the two assessment periods.
When I assessed at the time of admission, the patient did not show any abnormalities. During the waiting period, the patient's symptoms changed-sweating and drowsiness. The relatives told that the patient did not stop taking medicines, and symptoms were normal. Therefore, I think [the changes were] due to [the] severe pathology of the disease. The most common cases were patients with heart and lung diseases. The time of the increased severity is quite unpredictable. (NU05056405)
Reassessment interval
Changes in severity level, especially increased level of severity, were found in the duration between the first and the second time over an hour. Assessment of levels of severity should be periodically monitored because changes in severity can occur at any time, especially during waiting time. Reassessment interval should be minimally delayed for patient safety. The in-depth interview found that this interval affected changes in severity.
Reassessment is critical in the screening process and treatment planning. There were occasions when resources were insufficient to serve recipients under normal operations. The other day, some staff members were on leave, but there were a lot of [patients]. It took almost an hour to call the patients for reassessment. [Because of the] delay, the severity of the patient’s disease had progressed-possibly resulted in the increased level of severity. If the symptoms could be reassessed early, changes would be detected earlier. (NU05056405)
Nurses' clinical experiences
Nurses' experiences and understanding of both the ESI tool and older adults’ clinical features could have resulted in a more accurate assessment and improved the ability to anticipate and manage care appropriately. This could have reduced the changes in the severity of patients.
The other thing is the experience of predicting the symptoms. The anticipation for patients with cardiac symptoms was that it was riskier for patients to walk to each service point. Patients should be provided with a wheelchair or a stretcher because they required several steps of treatment. The outpatient building is quite large, so walking to each point can make patients feel tired. Patients should stay in a wheelchair or a stretcher to prevent changes in symptoms [and] to enhance safety. [Patients who] receive care like this usually have no changes in their levels of severity. (NU04056404)
Bypassing the initial triage process
Some patients bypassed the triage zone and went directly to the internal medicine clinic. In doing so, they missed the assessment of illness severity so that appropriate care and referral services could be given. However, on arrival at the clinic, they received an initial assessment that was re-evaluated while waiting in the queue. Because of delays in waiting, levels of severity could have increased.
Patients were bypassing the first screening point. The nursing staff was unable to thoroughly provide care, causing patients and their relatives not to realize that their symptoms were at a level of urgency. In addition, the symptoms became worse before the staff had made a reassessment. (NU07056413)
Self-preparation of patients
Preparing for the clinic exam before traveling to the hospital was a factor affecting an increased severity. Although there was no statistical difference in the quantitative results, there was a noticeable clinical effect. Over 40% of the patients who improperly prepared for their clinic visit experienced worsening symptoms.
The patient was sent from a community hospital for an endoscopy and abstained from water and food on the expectation that the doctor would perform an endoscopy that day. However, it was necessary to diagnose first, not to do it right away. [On arrival at] the hospital, the patient fainted because of hypoglycemia (Dtx=45 mg%). Another case was the patient forgot to take the medications for high blood pressure because he had to wake up at 4:00 a.m. to queue early for avoiding not having a car to go home. His BP was 190/110 mmHg. Both needed emergency care (NU11056410)
Management of triage RNs
At the triage zone, the key issue was assessing for life-threatening conditions. When patients were found to be at risk of a change in severity, the management by triage RNs was placing triage tags on the patients. They would be monitored during their time and this management caused a positive impact on patient safety.
One patient with late-stage lymphoma was bedridden with a tracheostomy. His ESI was almost level 2 because of the risk of hypoxia. The patient was placed with a triage tag, and the information was forwarded to the first aid room. Oxygen was given and symptoms had been monitored. For this management, there was no increase in severity. Communicating information at each point is of great importance to prevent changes in severity. (NU27056415)
Assigned nursing staff
In some patients, the level of severity was borderline at the triage zone, i.e., symptoms did not meet all criteria needed to be sent to the emergency room. For these individuals, it was necessary to assign someone to watch them carefully and speed up the process from admission through the end of treatment. This could ensure patient safety and the result would be a positive outcome.
This patient was triaged at ESI almost level 2. The symptoms had not yet been stabilized, but he had to wait to see a cardiologist. The staff had already coordinated with one another. The method of assigning staff to take care of him and enter the fast track was used to reduce the waiting time and prevent changes. Based on the reassessment, the severity level had not changed. He had received proper care [throughout] the treatment. The symptoms had been relieved without increased severity. (NU17056417)
Discussion
We found that most patients with increased severity were older adults. This is consistent with other studies that have reported similar findings16,17. Our qualitative results also show that changes in symptoms can occur easily in older adults. Older patients with comorbidities did not show any obvious severe symptoms at first, but the symptoms were not the same during the waiting time. The change is likely to come from the vulnerability of aging and comorbidity. Because of the aging process, older people tend to have changes in increased severity due to having a reduced energy reserve and fragility1. Suamchaiyaphum et al. 10 reported that age influences severity assessment and that age could predict the possibility of different outcomes at reassessment. In another study, up to 34% of the participants aged 65–84 changed their level of severity at reassessment by 1.71 times, compared to other age groups17.
Most of the older adults in our study had multiple pathologies with one or more chronic diseases. Patients with chronic diseases or comorbidities were more likely to increase their severity level at reassessment. This is consistent with Hasadsree et al. 18 who found that comorbidities resulted in greater severity and shock. Similarly, Suamchaiyaphum et al. 10 reported that two or more comorbidities had an increased impact on illness severity and pathology. Mirhaghi et al. 19 also found that comorbidities and various symptoms affected the patient triage, changes in symptoms, and treatment difficulties.
Symptoms related to cardiovascular and respiratory diseases as chief complaints were important factors affecting changes in severity. The quantitative results found that patients with heart and lung diseases were the most common cases with changing severity levels. The time of the increased severity is quite unpredictable for these health problems. Hinson et al. 17 found that the chief complaints of syncope, chest pain, and dyspnea were associated with changes in severity. Krongthong et al. 20 and Suamchaiyaphum et al. 10 confirmed that the chief complaint related to the cardiovascular and respiratory systems correlated with changes in severity. Therefore, if the chief complaint is related to impaired cardiovascular and respiratory systems, there should be a fast track for this group of patients to reduce worsening severity levels.
The patient's educational level was related to changes in levels of severity. People with low levels of education often have obstacles in accessing medical services. These include poor reading and listening skills, failure to listen to advice on treatment protocols and fear of being scolded by service providers. This can result in either miscommunication or the perception of misinformation that leads to unproductive and unhealthy behaviors21. Nilnate et al. 22 reported that health literacy scores among older adults were low to moderate. They had deterioration of their ears and eyes that can affect self-care management skills and competency for accessing, understanding, and reporting health knowledge. These circumstances might affect the process of history taking during triage, causing incomplete health data and determination of the correct ESI level.
We found that patients who came to the internal medicine clinic with a long journey and had long intervals between triage and reassessments resulted in changes in illness severity. Time length in traveling plus a long wait period may cause fatigue, a patient deterioration, and require earlier service procedures. This is consistent with the study of Hasadsree et al. 18 who found that the duration of travel/being transferred to the hospital that took longer than 60 min resulted in changes in illness severity and were related to shock. Another study also found that a prolonged time interval between assessments results in delays and adverse effects on treatment, leading to changes in severity23. The reassessment should be completed within 60 min of the first assessment, and ongoing observation and monitoring of symptoms would have a positive effect on detecting changes in severity.
We found that patients who arrived by referral ambulance were more vulnerable to changes in their symptoms. Similarly, Suksawang 24 reported that patients who came by emergency medical services or referral ambulance had the severity of symptoms at ESI levels 1 and 2. These patients required medical attention and close monitoring from RNs.
The clustering of patients at certain appointment times limited the triage RNs’ ability to assess them effectively. Arkun et al. 25 also found that there was only one triage RN at the facility at certain times because the RNs needed to leave for lunch or take a break. This finding is similar to our qualitative result in that some staff members were on leave, but there were many patients. It took almost an hour to call the patients for reassessment. Having many patients and a limited number of nurses produced delays in patient triage and a decrease in the effectiveness of patient triage, causing changes in illness severity.
The qualitative findings showed that nurses' clinical experiences affected decision-making and accurate prediction of the symptoms. In Thailand, new nurses with no experience are not assigned to triage the patients; they should have experience in nursing and be prepared to be sensitive to serious health problems and perform accurate screening results to detect and help patients with acute and emergency health problems. This finding is consistent with the study of Tonsaur et al. 26 and Wachiradilok et al. 9, who reported that staff members who had less than five years of service never used the ESI tool nor had been in a unit using the ESI tool for patient triage, might lack confidence in performing accuracy of triage. Those with more experience working and using the ESI tool could use it proficiently, make accurate assessments, anticipate what might happen to the patients, and create a management plan more efficiently.
Some patients who bypassed the triage zone reported changes in their levels of illness severity. Our qualitative results found that because patients were bypassing the first screening point, the nursing staff was unable to thoroughly provide care, causing patients and their relatives not to realize that their symptoms were at a level of urgency. In addition, the symptoms became worse before the staff had made a reassessment. Thesprasit 27 also reported that patients who were not initially triaged had changes in severity and developed worse symptoms while waiting for examination. Patients who provided inappropriate self-preparation before arriving at the clinic experienced changes in severity levels. Some patients from this study abstained from water and food before being admitted to the hospital for endoscopy. However, it was necessary to diagnose first, not to do it on the first day of admission. The abstaining from water and food caused their severity to increase during the waiting time. Suksawang 24 also reported that more than half of the patients in a study had improper practices before coming to the hospital, so their symptoms worsened while waiting for treatment.
Good management and the assignment of nursing staff to observe specific patients until the end of the treatment process can have a positive effect on safety and may reduce the severity of the patient’s symptoms. Although the triage process has clear operating guidelines, Suksawang 24 identified desirable characteristics of triage RNs. When immediate problems arise, triage RNs should remain flexible and manage solutions that focus on the benefit and safety of the patients. Good management by RNs for patients with late-stage lymphoma who are bedridden with a tracheostomy was demonstrated by our study. Good management promptly provided safety for the patients.
Limitations
Because the ESI tool guidelines do not specify the interval between triage and reassessment time nor the appropriate time for reassessment at each severity level, we conducted the study in an outpatient department context by reassessing immediately upon the patient's arrival at the internal medicine clinic. Therefore, the interval between the triage of the patient and reassessment varied for each patient.
Conclusion and recommendations
Although most of the patients had no change in severity, those with changes that increased their level of severity were more frequently found in older adults. Factors related to changes in severity from both quantitative and qualitative data were age group, chronic disease, chief complaint, travel time, type of vehicle, time of assessment, aging process and comorbidity, unstable illness, reassessment interval, nurse's experience, bypassing the patient triage process, patient's self-preparation, management of triage RNs, and assignment of direct healthcare staff until the end of the treatment. The factors related to changes in level of severity and what should be done in this situation were summarized and provided (Fig. 1).
This study made reassessment immediately when patients arrived at the internal medicine clinic. Future studies should control or determine a time for reassessment clearly and consistently. Alternatively, different times of reassessment may be explored as an important variable for the outcome analysis, especially in older adults. In addition, the results of the study could form the basis of a nursing staff education plan to increase knowledge, competence, and awareness of aging processes about the assessment of severity levels. The ESI tool may need to be refined for more sensitivity in assessing older adults.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to prohibited laws (and/or rules, regulations, and contracts). However, they are available from the corresponding author upon reasonable request.
References
Assantachai, P. Concerted actions toward healthy aging in ASEAN countries. Siriraj Med. J. 73(9), 633–634. https://doi.org/10.33192/Smj.2021.81 (2021).
Limpawattana, P. Geriatric Syndromes and Interesting Health Issues 1st edn. (Geriatric Medicine Unit Department of Internal Medicine Faculty of Medicine Khon Kaen University, 2018).
McCabe, J. & Kennelly, S. P. Acute care of older patients in the emergency department: Strategies to improve patient outcomes. Open Access Emerg. Med. 7, 45–54. https://doi.org/10.2147/OAEM.S69974 (2015).
Paralee, P. & Pearkao, C. Factors predicting overcrowding in emergency room of a university hospital. Songklanagarind J. Nurs. 40(2), 52–65 (2020).
National Institute for Emergency Medicine. Requirements, guidelines for the development of Emergency Medical Dispatch Center. Standards and Criteria for Emergency Medical Systems Vol. 1. 2020. Nonthaburi [cited 2020 Jun 7]. p. 80. https://www.niems.go.th/1/Ebook/Detail/223?group=21. Thai
Opara, N. U., Hensley, B. M. & Judy, C. Evaluating the benefits of viral respiratory panel test in the reduction of emergency department throughput time for patients with acute exacerbation of chronic obstructive pulmonary disease. Cureus 13(11), e19213. https://doi.org/10.7759/cureus.19213 (2021).
Sarvari, A., Habibzadeh, H., Alilu, L. & Sheikhi, N. Effect of emergency severity index implementation on the waiting time for patients to receive health services in the emergency department. Acta Fac. Med. Naissensis 37(4), 369–380. https://doi.org/10.5937/afmnai2004369S (2020).
Byrne, D. et al. Mortality outcomes and emergency department wait times- the paradox in the capacity limited system. Acute Med. 17(3), 130–136 (2018).
Wachiradilok, P., Sirisamutr, T., Chaiyasit, S. & Sethasathien, A. A nationwide survey of Thailand emergency departments triage systems. Thai J. Nurs. Council 31(2), 96–108 (2016).
Suamchaiyaphum, K., Chanruangvanich, W., Thosingha, O. & Momsomboon, A. Factors influencing the accuracy of Emergency Severity Index-Based emergency patient triage. Thai J. Nurs. Council 34(4), 34–47 (2019).
Thatphet, P., Liu, S. W., Sri-On, J. & Wongtangman, T. Geriatric emergency medicine-related knowledge teaching among Thai emergency medicine residents. Thai J. Emerg. Med. 3(1), 1–18. https://doi.org/10.14456/tjem.2021.1 (2021).
Santoro, A., Bientinesi, E. & Monti, D. Immunosenescence and inflammation in the aging process: Age-related diseases or longevity?. Ageing Res. Rev. 71, 101422. https://doi.org/10.1016/j.arr.2021.101422 (2021).
Medical Emergency Department. An annual report of the outpatient department. 2020. Maharat Nakhon Ratchasima Hospital, Nakhon Ratchasima, Thailand. Thai
Soontorn, T., Sitthimongkol, Y., Thosingha, O. & Viwatwongkasem, C. Factors influencing the accuracy of triage by registered nurses in trauma patients. Pacific Rim. Int. J. Nurs. Res. 22(2), 120–30 (2018).
Gilboy, N., Tanabe, P., Travers, D. A., Rosenau, A. M., & Eitel, D. R. Emergency Severity Index, version 4: Implementation handbook. (AHRQ Publication No. 05–0046–2). 2005. Rockville, MD: Agency for Healthcare Research and Quality.
Malinovska, A., Pitasch, L., Geigy, N., Nickel, C. H. & Bingisser, R. Modification of the emergency severity index improves mortality prediction in older patients. West J. Emerg. Med. 20(4), 633–640. https://doi.org/10.5811/westjem.2019.4.40031 (2019).
Hinson, J. et al. Accuracy of emergency department triage using the emergency severity index and independent predictors of under-triage and over-triage in Brazil: A retrospective cohort analysis. Int. J. Emerg. Med. 11(1), 1–10 (2018).
Hasadsree, N., Chanruangvanich, W., Thosingha, O. & Riyapan, S. Factors predicting shock in emergency patients. Thai J. Nurs. Council 34(3), 60–75 (2019).
Mirhaghi, A., Kooshiar, H., Esmaeili, H. & Ebrahimi, M. Outcomes for emergency severity index triage implementation in the emergency department. J. Clin. Diagn. Res. 9(4), OC04–OC07. https://doi.org/10.7860/JCDR/2015/11791.5737 (2015).
Krongthong, S., Krajaiklang, S., Surason, N. & Phromtuang, S. Development of STEMI fast track service model. Med. J. Srisaket. Surin. Buriram. Hosp. 33(1), 45–59 (2018).
Sittikan, S. & Jongudomkarn, D. Barriers to access of primary healthcare by people with low income in urban communities: A qualitative study. J. Nurs. Sci. Health 43(1), 19–29 (2020).
Nilnate, W., Hengpraprom, S. & Hanvoravongchai, P. Level of health literacy in Thai elders Bangkok, Thailand. J. Health Res. 30(5), 315–321 (2016).
Setthachanwit, S. Inter-rater agreement of emergency nurses and physicians in Emergency Severity Index (ESI) triage in emergency room. Research report. 2019. http://www.cbh.moph.go.th/app/intranet/files/km/1593598353_%E0%B8%84%E0%B8%A7%E0%B8%B2%E0%B8%A1%E0%B8%AA%E0%B8%AD%E0%B8%94%E0%B8%84%E0%B8%A5%E0%B9%89%E0%B8%AD%E0%B8%87%E0%B9%83%E0%B8%99%E0%B8%81%E0%B8%B2%E0%B8%A3%E0%B8%88%E0%B8%B3%E0%B9%81%E0%B8%99%E0%B8%81%E0%B8%9C%E0%B8%B9%E0%B9%89%E0%B8%9B%E0%B9%88%E0%B8%A7%E0%B8%A2%E0%B8%82%E0%B8%AD%E0%B8%87%E0%B9%81%E0%B8%9E%E0%B8%97%E0%B8%A2%E0%B9%8C%E0%B9%81%E0%B8%A5.pdf. Thai
Sukswang S. An evaluation report of ECS assessment team (AYECS). Phra Nakhon Si Ayutthaya: AYECS. (2018). Thai
Arkun, A. et al. Emergency department crowding: Factors influencing flow. West J. Emerg. Med. 11(1), 10–15 (2010).
Tonsaur, C., Vichakkanalan, W., Chaiyaprom, K., Thamsathan, P., Chanthapim, P., & Saensuk, P. The study on classification of emergency patients at the Accident and Suthavej Hospital Emergency Faculty of Medicine Mahasarakham University, in: The 7th National Academic Conference, Nakhon Ratchasima College. Nakhon Ratchasima, 2020; 1140–1148. Thai
Thesprasit, T. Development of a system for classification of patients in Outpatient and emergency departments at Chokchai Hospital. Reg. Health Promot. Center J. 15(36), 160–178. https://doi.org/10.14456/rhpc9j.2021.12 (2021).
Acknowledgements
We would like to express our gratitude to those who contributed to this study. A special thanks is extended to the adults and older adults who participated in the study. We also would like to acknowledge the hospital staff for their cooperation and participation during the research process. Lastly, special appreciation is extended to a native speaker and nursing professor for grammar proving and reviewing early drafts.
Funding
This research was supported by the Fundamental Fund of Khon Kaen University, has received funding support from the National Science, Research and Innovation Fund (NSRF) (Grant Number NSRF63-011). Appreciation is extended to these fundamental funds and the national science, research, and innovation fund for making this research possible.
Author information
Authors and Affiliations
Contributions
All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE: http://www.icmje.org/recommendation/): Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. Drafting the article or revising it critically for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Narongsanoi, P., Banharak, S., Panpanit, L. et al. Factors related to changes in severity among adult and older adult patients at an internal medicine department clinic: an embedded mixed-method study. Sci Rep 14, 3914 (2024). https://doi.org/10.1038/s41598-024-54266-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54266-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.