Abstract
A comprehensive understanding of the dynamics of Streptococcus pneumoniae colonization in conjunction with respiratory virus infections is essential for enhancing our knowledge of the pathogenesis and advancing the development of effective preventive strategies. Therefore, a case–control study was carried out in Addis Ababa, Ethiopia to investigate the colonization rate of S. pneumoniae and its coinfection dynamics with respiratory viruses among children under the age of 5 years. Samples from the nasopharyngeal and/or oropharyngeal, along with socio-demographic and clinical information, were collected from 420 children under 5 years old (210 cases with lower respiratory tract infections and 210 controls with conditions other than respiratory infections.). A one-step Multiplex real-time PCR using the Allplex Respiratory Panel Assays 1–4 was performed to identify respiratory viruses and bacteria. Data analysis was conducted using STATA software version 17. The overall colonization rate of S. pneumoniae in children aged less than 5 years was 51.2% (215/420). The colonization rates in cases and controls were 54.8% (115/210) and 47.6% (100/210), respectively (p = 0.14). Colonization rates were observed to commence at an early age in children, with a colonization rate of 48.9% and 52.7% among infants younger than 6 months controls and cases, respectively. The prevalence of AdV (OR, 3.11; 95% CI [1.31–8.19]), RSV B (OR, 2.53; 95% CI [1.01–6.78]) and HRV (OR, 1.7; 95% CI [1.04–2.78]) tends to be higher in children who tested positive for S. pneumoniae compared to those who tested negative for S. pneumoniae. Further longitudinal research is needed to understand and determine interaction mechanisms between pneumococci and viral pathogens and the clinical implications of this coinfection dynamics.
Similar content being viewed by others
Introduction
Acute Lower Respiratory Infections (ALRIs) remain one of the leading causes of morbidity and mortality among children under 5 years old globally, with sub-Saharan Africa bearing a disproportionate burden1. Streptococcus pneumoniae is recognized as a primary pathogen responsible for ALRIs accounting for a higher number of deaths compared to all other etiologies combined, and contributes to a staggering total of 1,189,937 deaths in 2016 in people of all ages, worldwide2.
Colonization of the nasopharynx by S. pneumoniae is considered to be a prerequisite to pneumococcal disease development and transmission within communities3,4. The introduction of pneumococcal conjugate vaccines (PCV) has had a notable influence on the colonization dynamics of S. pneumoniae; numerous research studies indicate that the introduction of PCV can result in shifts in the prevalence of circulating serotypes, as non-vaccine serotypes may emerge or become more prevalent following a reduction in targeted serotypes due to vaccination-induced effects5,6,7,8.
In recent years, there has been growing interest in understanding the coinfection dynamics between S. pneumoniae colonization and respiratory viruses9,10,11,12. Coinfection by pneumococci and respiratory viruses often leads to increased disease severity10. As an example, it is widely believed that a significant number of fatalities during the 1918–1919 influenza pandemic were primarily caused by secondary bacterial pneumonia, with S. pneumoniae being the most prevalent bacteria associated with these cases13. It is hypothesized that interactions between pneumococci and respiratory viruses could potentially amplify pathogenicity or modify immune responses, thereby contributing to the development of more severe symptoms or complications12.
In a previous report, we highlighted the notable impact of RSV, Influenza A, and PIV 1 viruses on acute lower respiratory infections (ALRIs) among children under 5 years in Addis Ababa, Ethiopia14. Understanding the dynamics of S. pneumoniae colonization alongside respiratory virus infections is crucial for improving our knowledge about pathogenesis and developing effective preventive strategies such as vaccines or antiviral therapies. The objective of this study was to investigate S. pneumoniae colonization rate and the coinfection dynamics with respiratory viruses in children under 5 years old.
Materials and methods
Study area and period
A prospective case–control study was conducted in Addis Ababa, Ethiopia, from September 2019 to May 2022, involving two major governmental hospitals: St. Paul Hospital Millennium Medical College and ALERT Comprehensive Specialized Hospital. However, data collection was temporarily halted from February 2020 to July 2020 due to the COVID-19 pandemic.
Study population
The case population consisted of children under 5 years old with LRTIs, defined as an acute respiratory illness with a history of fever or measured fever of ≥ 38 °C and cough within the past 10 days that required hospitalization. Controls were also children under five who were admitted to the same hospital for conditions other than respiratory infections such as injury, skin infections, gastrointestinal infections, or genitourinary infections. Participants who were above 60 months of age were excluded from both the cases and controls. Additionally, children with ARTIs that had an onset beyond 10 days were also excluded from the cases. Throughout the study period, both cases and controls were enrolled based on age group and month of sample collection using marginal frequency matching techniques.
Data and naso/oropharyngeal swab collection
Experienced pediatric nurses identified eligible cases and controls. They obtained informed consent from parents/guardians, collected sociodemographic and clinical information, and gathered samples using naso/oropharyngeal swabs.
Nasopharyngeal and oropharyngeal swabs were obtained from all the children participating in the study. Nasopharyngeal specimens were obtained by inserting flocked swabs (Copan) into the posterior nasopharynx and rotating 180° for 2–3 s. Subsequently, oropharyngeal specimens were collected using MWE Swabs, targeting both tonsillar pillars and the posterior oropharynx for several seconds15. Following collection, the swabs from both sites were placed together in a 3-mL vial containing universal transport media (SIGMA VCM). Then the samples were transported to the Armauer Hansen Research Institute (AHRI) and stored at − 80 °C until further testing.
Laboratory procedures
The laboratory procedures were conducted as described in our previous report14. In summary, nucleic acid extraction from naso/oropharyngeal samples was performed manually using the Ribospin_vRD Viral RNA/DNA Extraction kit (GeneAll, South Korea) following the manufacturer's protocol. Subsequently, respiratory virus detection was carried out using Allplex Respiratory Panel 1–3 Assays for viral detection and Panel 4 for bacterial detection (Seegene, South Korea) (Table 1). Amplification was done using a CFX96 thermocycler (BioRad, Hercules CA, USA), and PCR setup and result analysis were managed with the CFX real-time PCR detection system (CFX Manager Software-IVD v1.6). A Ct value of ≤ 42 (as determined by the manufacturer) was used to define positivity for each virus and S. pneumoniae.
Data analysis
The data analysis was conducted using Stata software version 17. To examine the characteristics of the S. pneumoniae positive and negative population, as well as to assess the coinfection dynamics with respiratory viruses, odds ratios (OR) were calculated. Additionally, the mean Cycle threshold (CT) values for each detected virus were determined and the Two-sample Wilcoxon rank-sum (Mann–Whitney) test was used to investigate any associations between viral load and the presence of S. pneumoniae in the upper respiratory tract (URT).
Ethical review and regulation
The ethical review committees of AHRI and Addis Ababa University granted approval for this study. Prior to enrollment, written informed consent was obtained from all parents or guardians of the participating children, which was documented through their signatures.
All methods and processing of personal data strictly adhered to the Armauer Hansen Research Institute establishment regulation no. 530/2023 and Federal Civil Servants Proclamation No. 1064/2017 issued by the council of ministers of the federal government of Ethiopia.
Ethics statement
Approval for this study was granted by the ethical review committees of AHRI and Addis Ababa University. Before enrolling participants, written informed consent was obtained from the parents or guardians of the children involved. This consent was documented through their signatures.
Results
Prevalence of pneumococcal colonization rate
The overall colonization rate of S. pneumoniae in children aged less than 5 years was 51.2% (215/420). The colonization rates in cases and controls were 54.8% (115/210) and 47.6% (100/210), respectively (p = 0.14). Very few samples tested positive for other respiratory bacteria in both the case and control groups (Table 2). Table 3 provides the characteristics of both the population colonized and non-colonized by S. pneumoniae. Generally, there is no statistically significant difference between the two groups.
The mean Cycle threshold (CT) values were compared between individuals who tested positive for S. pneumoniae colonization in the cases and control groups, serving as an indirect measure of bacterial load (Fig. 1). The Two-sample Wilcoxon rank-sum (Mann–Whitney) test did not show any statistically significant differences in the mean CT values between the two groups (p = 0.5). Furthermore, the analysis of the percentage of pneumococcal positive samples with CT values < 35, between 35 and 40, and > 42 did not reveal any significant statistical difference between the case and control groups (p = 0.84) (Table 4).
Colonization rates of S. pnuemoniae across ages
The colonization rate across the different age groups of the control population ranges between 40 and 49%; whereas in the case groups, it ranges between 53 and 58% (Fig. 2). No statistically significant differences (p > 0.05) were observed in the colonization rates between children in the cases and control groups across different age groups. Colonization rates of S. pneumoniae were observed to commence at an early age in children, with a colonization rate of 22 (48.9%) and 29 (52.7%) among infants younger than 6 months controls and cases, respectively.
Prevalence of viruses in children tested positive and negative for S. pneumoniae
The prevalence of AdV (OR, 3.11; 95% CI [1.31–8.19]), RSV B (OR, 2.53; 95% CI [1.01–6.78]) and HRV (OR, 1.7; 95% CI [1.04–2.78]) tends to be higher in children who tested positive for S. pneumoniae compared to those who tested negative for S. pneumoniae (Fig. 3). These results indicate a significant association between Adenovirus, RSV B and HRV infections with S. pneumoniae colonization in children under 5 years old in the study population.
Prevalence of viruses in children who tested positive for S. pneumoniae compared to those who tested negative [Left] ORs with 95% CIs for detection of respiratory viruses in S. pneumoniae positive children compared with negatives [Right]. Flu A, Influenza A virus; Flu B, Influenza B virus; RSV A, Respiratory syncytial virus A; RSV B, Respiratory syncytial virus B; AdV, Adenovirus; PIV 1, Parainfluenza virus 1; PIV 3, Parainfluenza virus 3; PIV 4, Parainfluenza virus 4; HEV, Enterovirus; NL63, Coronavirus NL63; HRV, Human rhinovirus; HBoV, Bocavirus 1/2/3/4; MPV, Metapneumovirus.
The mean Cycle threshold (CT) values for each detected virus were compared between individuals who tested positive and negative for S. pneumoniae colonization, serving as an indirect measure of viral load (Fig. 4). The p values calculated using the Two-sample Wilcoxon rank-sum (Mann–Whitney) test did not show any statistically significant differences in the mean CT values between the two groups (p = 0.50).
A box plot of Mean Cycle threshold (CT) values for each detected virus (A). Flu A, Influenza A virus; Flu B, Influenza B virus; RSV A, Respiratory syncytial virus A; RSV B, Respiratory syncytial virus B; AdV, Adenovirus; PIV 1, Parainfluenza virus 1, 2, 3, and 4; HEV, Enterovirus; CoV, Coronavirus NL63, OC43, and 229E; HRV, Human rhinovirus; HBoV, Bocavirus 1/2/3/4; MPV, Metapneumovirus NB: the line crossed the box represent the mean CT value, the dots in the figures are the outliers.
Seasonality of S. pneumoniae and respiratory viruses
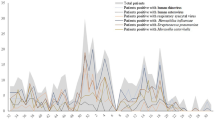
Our finding indicates that S. pneumoniae and respiratory viruses occur throughout the year in Addis Ababa, Ethiopia (Fig. 5). Viral coinfection was observed frequently in the samples, with 199 (47.4%). However, in the graph, we included the detection rates of each virus, whether they were detected as a single infection or as part of a coinfection. In the first two months of sample collection (September and October 2019), there was notably a high prevalence of RSV B. The absence of data from March to June 2020 and beyond is attributed to the impact of the COVID-19 pandemic in Ethiopia. It was also observed that individual children were infected by at least two respiratory pathogens in the sampling period.
Seasonal patterns of S. pneumoniae and respiratory viruses in Addis Ababa, Ethiopia. SP, S. pneumoniae; Flu A, Influenza A virus; Flu B, Influenza B virus; RSV A, Respiratory syncytial virus A; RSV B, Respiratory syncytial virus B; AdV, Adenovirus; PIV, Parainfluenza virus 1, 2, 3, and 4; HEV, Enterovirus; CoV, Coronavirus; HRV, Human rhinovirus; HBoV, Bocavirus 1/2/3/4; MPV, Metapneumovirus.
Discussion
This study revealed that a significant portion of both cases and control children carried S. pneumoniae in their upper respiratory tract, 54.8% and 47.6%, respectively. In previous studies conducted in Africa, it was observed that the rate of S. pneumoniae detection was higher in both cases and controls; among cases, the detection rates ranged from 57.5 to 85.0%, while in control children, the detection rates varied from 48 to 88.6%16,17,18,19,20,21,22,23,24,25. Understanding the factors influencing the high colonization rate of S. pneumoniae is essential for implementing effective prevention and control strategies, such as vaccination programs and antimicrobial stewardship. Additionally, further research is necessary to explore the interactions between host factors, environmental conditions, and the bacterium itself to gain insights into the dynamics of S. pneumoniae colonization.
Comparing the mean CT values between the cases and controls provided information on potential variations in S. pneumoniae colonization levels. However, there was no significant difference detected in the mean CT values between the cases and controls of our study population. Several previous studies among children evaluated the use of pneumococcal colonization density as a marker of pneumococcal pneumonia26,27,28,29,30,31. Some of these studies have indicated a positive correlation between pneumococcal colonization density and severe pneumonia26,27,28,31. In contrast, other investigations did not identify any association between colonization density and the severity of pneumonia29,30. It is crucial to interpret these findings cautiously since additional factors such as sample size, population demographics, underlying health conditions, and antibiotic usage history may influence S. pneumoniae colonization dynamics and subsequent cycle threshold results. Further analysis considering these factors along with clinical outcomes will help determine whether variations observed in cycle threshold values have any meaningful associations with disease progression or prognosis within each group.
Our findings suggest that there is an association between Adenovirus and S. pneumoniae. Adenovirus is responsible for approximately 5–10% of ALRIs in children32. A study conducted in Tunisia reported that the co-detection of S. pneumoniae appears to exacerbate the severity of Adenovirus-associated ALRIs33. Furthermore, an animal model study demonstrated that adenovirus infection promotes middle ear infection caused by S. pneumoniae compared to non-adenovirus-infected animals34. Adenovirus infection may enhance the adherence of S. pneumoniae to mucosal cells35. Additional investigations are required to comprehend the underlying mechanisms of coinfection.
Our finding also indicated the presence of an association between RSV B and S. pneumoniae colonization in children under 5 years old in the study population, implying potential interactions and synergistic effects between these two pathogens. Numerous studies have documented interactions between S. pneumoniae and RSV10,36,37,38,39,40,41. The exact mechanisms underlying the co-infection dynamics are not fully understood; however, pneumococcus and RSV potentially have bidirectional interactions10,41. In vitro experiments showed enhanced adherence of S. pneumoniae to human epithelial cells infected with RSV39. Conversely, S. pneumoniae colonization can enhance subsequent RSV infection41,42. Furthermore, in a clinical trial, the administration of pneumococcal vaccination resulted in a 32% reduction in the incidence of hospitalization for pneumonia associated with RSV43. This co-infection dynamics highlights the need to consider both pathogens when diagnosing respiratory illnesses in young children and underscores the importance of preventive measures against both RSV B and S. pneumoniae infections.
One limitation of our study was the combination of nasopharyngeal and oropharyngeal swabs prior to testing. Additionally, as we used a commercial kit, the specific target gene for detecting S. pneumoniae was not disclosed. These factors could have potentially impacted the specificity of the test, as non-pneumococcal Streptococci present in the oral cavity may produce a false-positive signal for certain pneumococcal PCR targets44.
Conclusions
The colonization rate of S. pneumoniae in children aged less than 5 years, with and without ALRIs, was high. Our results also indicate a significant association between Adenovirus, RSV B and HRV infections with S. pneumoniae colonization in the study population, implying potential interactions and synergistic effects between respiratory pathogens. Further research is needed to understand the underlying mechanisms and clinical implications of this coinfection dynamics.
Data availability
The datasets during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Seidu, A.-A. et al. Prevalence and determinants of acute lower respiratory infections among children under-five years in sub-Saharan Africa: Evidence from demographic and health surveys. SSM Popul Health 8, 100443 (2019).
Troeger, C. et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet. Infect. Dis. 18, 1191–1210 (2018).
Nunes, M. C. et al. Acquisition of Streptococcus pneumoniae in pneumococcal conjugate vaccine-naive South African children and their mothers. Pediatr. Infect. Dis. J. 32, e192–e205 (2013).
Sleeman, K. L. et al. Acquisition of Streptococcus pneumoniae and nonspecific morbidity in infants and their families: A cohort study. Pediatr. Infect. Dis. J. 24, 121–127 (2005).
Cleary, D. W. et al. Changes in serotype prevalence of Streptococcus pneumoniae in Southampton, UK between 2006 and 2018. Sci. Rep. 12, 13332 (2022).
Gallagher, K. E. et al. Population immunity to pneumococcal serotypes in Kilifi, Kenya, before and 6 years after the introduction of PCV10 with a catch-up campaign: An observational study of cross-sectional serosurveys. Lancet Infect. Dis. https://doi.org/10.1016/s1473-3099(23)00206-2 (2023).
Usuf, E. et al. Persistence of nasopharyngeal pneumococcal vaccine serotypes and increase of nonvaccine serotypes among vaccinated infants and their mothers 5 years after introduction of pneumococcal conjugate vaccine 13 in The Gambia. Clin. Infect. Dis. 68, 1512–1521. https://doi.org/10.1093/cid/ciy726 (2019).
Gladstone, R. A. et al. Five winters of pneumococcal serotype replacement in UK carriage following PCV introduction. Vaccine 33, 2015–2021. https://doi.org/10.1016/j.vaccine.2015.03.012 (2015).
Bennett, J. C. et al. Streptococcus pneumoniae nasal carriage patterns with and without common respiratory virus detections in households in Seattle, WA, USA before and during the COVID-19 pandemic. Front. Pediatr. 11, 1198278. https://doi.org/10.3389/fped.2023.1198278 (2023).
Manna, S. et al. Synergism and antagonism of bacterial-viral coinfection in the upper respiratory tract. Msphere 7, e00984-21 (2022).
Amin-Chowdhury, Z. et al. Does the rise in seasonal respiratory viruses foreshadow the return of invasive pneumococcal disease this winter?. Lancet Respir. Med. 10, e1–e2. https://doi.org/10.1016/s2213-2600(21)00538-5 (2022).
Neu, U. & Mainou, B. A. Virus interactions with bacteria: Partners in the infectious dance. PLoS Pathog. 16, e1008234. https://doi.org/10.1371/journal.ppat.1008234 (2020).
Morens, D. M., Taubenberger, J. K. & Fauci, A. S. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: Implications for pandemic influenza preparedness. J. Infect. Dis. 198, 962–970. https://doi.org/10.1086/591708 (2008).
Wadilo, F. et al. Viral etiologies of lower respiratory tract infections in children < 5 years of age in Addis Ababa, Ethiopia: A prospective case–control study. Virol. J. 20, 163. https://doi.org/10.1186/s12985-023-02131-x (2023).
Kim, C. et al. Comparison of nasopharyngeal and oropharyngeal swabs for the diagnosis of eight respiratory viruses by real-time reverse transcription-PCR assays. PLoS ONE 6, e21610. https://doi.org/10.1371/journal.pone.0021610 (2011).
Bénet, T. et al. Etiology and factors associated with pneumonia in children under 5 years of age in Mali: A prospective case–control study. PLoS ONE 10, e0145447 (2015).
Zar, H. J. et al. Aetiology of childhood pneumonia in a well vaccinated South African birth cohort: A nested case–control study of the Drakenstein Child Health Study. Lancet Respir. Med. 4, 463–472 (2016).
Mwananyanda, L. et al. The etiology of pneumonia in Zambian children: Findings from the Pneumonia Etiology Research for Child Health (PERCH) Study. Pediatr. Infect. Dis. J. 40, S40 (2021).
Tapia, M. D. et al. The etiology of childhood pneumonia in Mali: Findings from the Pneumonia Etiology Research for Child Health (PERCH) study. Pediatr. Infect. Dis. J. 40, S18 (2021).
Awori, J. O. et al. The etiology of pneumonia in HIV-uninfected children in Kilifi, Kenya: Findings from the Pneumonia Etiology Research for Child Health (PERCH) study. Pediatr. Infect. Dis. J. 40, S29 (2021).
Howie, S. R. et al. The etiology of childhood pneumonia in The Gambia: Findings from the Pneumonia Etiology Research for Child Health (PERCH) study. Pediatr. Infect. Dis. J. 40, S7 (2021).
Moore, D. P. et al. The etiology of pneumonia in HIV-uninfected South African children: Findings from the Pneumonia Etiology Research for Child Health (PERCH) study. Pediatr. Infect. Dis. J. 40, S59 (2021).
Bénet, T. et al. Microorganisms associated with pneumonia in children < 5 years of age in developing and emerging countries: The GABRIEL pneumonia multicenter, prospective, case–control study. Clin. Infect. Dis. 65, 604–612 (2017).
Feikin, D. R. et al. Viral and bacterial causes of severe acute respiratory illness among children aged less than 5 years in a high malaria prevalence area of western Kenya, 2007–2010. Pediatr. Infect. Dis. J. 32, e14–e19 (2013).
Baillie, V. L. et al. Epidemiology and seasonality of endemic human coronaviruses in South African and Zambian children: A case–control pneumonia study. Viruses 13, 1513 (2021).
Albrich, W. C. et al. Pneumococcal colonisation density: A new marker for disease severity in HIV-infected adults with pneumonia. BMJ Open 4, e005953 (2014).
Carr, O. J. et al. Nasopharyngeal pneumococcal colonization density is associated with severe pneumonia in young children in the Lao People’s Democratic Republic. J. Infect. Dis. 225, 1266–1273 (2022).
Baggett, H. C. et al. Density of upper respiratory colonization with Streptococcus pneumoniae and its role in the diagnosis of pneumococcal pneumonia among children aged < 5 years in the PERCH study. Clin. Infect. Dis. 64, S317–S327 (2017).
Collins, A. M. et al. Pneumococcal colonization rates in patients admitted to a United Kingdom hospital with lower respiratory tract infection: A prospective case–control study. J. Clin. Microbiol. 54, 944–949 (2016).
Piralam, B. et al. Pneumococcal colonization prevalence and density among Thai children with severe pneumonia and community controls. PLoS ONE 15, e0232151 (2020).
Brotons, P. et al. Nasopharyngeal bacterial load as a marker for rapid and easy diagnosis of invasive pneumococcal disease in children from Mozambique. PLoS ONE 12, e0184762 (2017).
Zhang, J. et al. Pediatric adenovirus pneumonia: Clinical practice and current treatment. Front. Med. 10, 1207568 (2023).
Brini, I. et al. Human adenoviruses associated with respiratory illness in neonates, infants, and children in the Sousse area of Tunisia. J. Med. Virol. 92, 3081–3092 (2020).
Murrah, K. A. et al. Replication of type 5 adenovirus promotes middle ear infection by Streptococcus pneumoniae in the chinchilla model of otitis media. Pathog. Dis. 73, 1 (2015).
Håkansson, A., Kidd, A., Wadell, G., Sabharwal, H. & Svanborg, C. Adenovirus infection enhances in vitro adherence of Streptococcus pneumoniae. Infect. Immun. 62, 2707–2714 (1994).
Brealey, J. C. et al. Streptococcus pneumoniae colonization of the nasopharynx is associated with increased severity during respiratory syncytial virus infection in young children. Respirology 23, 220–227 (2018).
Mandelia, Y. et al. Dynamics and predisposition of respiratory viral co-infections in children and adults. Clin. Microbiol. Infect. 27(631), e631-631.e636 (2021).
Meskill, S. D. & O’Bryant, S. C. Respiratory virus co-infection in acute respiratory infections in children. Curr. Infect. Dis. Rep. 22, 1–8 (2020).
Hament, J.-M. et al. Enhanced adherence of Streptococcus pneumoniae to human epithelial cells infected with respiratory syncytial virus. Pediatr. Res. 55, 972–978 (2004).
Bosch, A. A., Biesbroek, G., Trzcinski, K., Sanders, E. A. & Bogaert, D. Viral and bacterial interactions in the upper respiratory tract. PLoS Pathog. 9, e1003057 (2013).
Nguyen, D. T. et al. Streptococcus pneumoniae enhances human respiratory syncytial virus infection in vitro and in vivo. PLoS ONE 10, e0127098 (2015).
Nguyen, D. T. et al. The synthetic bacterial lipopeptide Pam3CSK4 modulates respiratory syncytial virus infection independent of TLR activation. PLoS Pathog. 6, e1001049 (2010).
Madhi, S. A. & Klugman, K. P. A role for Streptococcus pneumoniae in virus-associated pneumonia. Nat. Med. 10, 811–813 (2004).
Simões, A. S. et al. lytA-based identification methods can misidentify Streptococcus pneumoniae. Diagn. Microbiol. Infect. Dis. 85, 141–148 (2016).
Acknowledgements
We would like to express our gratitude to the children and their parents/guardians who willingly participated in this study. Additionally, we would like to extend our appreciation to all the nurses and physicians who played a crucial role in identifying the study population and collecting the specimens.
Author information
Authors and Affiliations
Contributions
F.W.W., A.F.D., A.M., and A.M. conceived and designed the study and wrote the manuscript. F.W.W., T.S., K.M., and A.A. performed the experiments. W.M. and A.M. provided essential resources. F.W.W., A.M., and R.H. analyzed the data. All authors contributed to the manuscript revision and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wada, F.W., Desta, A.F., Gebre, M. et al. Pneumococcal colonization and coinfecting respiratory viruses in children under 5 years in Addis Ababa, Ethiopia: a prospective case–control study. Sci Rep 14, 4174 (2024). https://doi.org/10.1038/s41598-024-54256-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54256-w
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.