Abstract
Skin cancer is a frequently occurring and possibly deadly disease that necessitates prompt and precise diagnosis in order to ensure efficacious treatment. This paper introduces an innovative approach for accurately identifying skin cancer by utilizing Convolution Neural Network architecture and optimizing hyperparameters. The proposed approach aims to increase the precision and efficacy of skin cancer recognition and consequently enhance patients' experiences. This investigation aims to tackle various significant challenges in skin cancer recognition, encompassing feature extraction, model architecture design, and optimizing hyperparameters. The proposed model utilizes advanced deep-learning methodologies to extract complex features and patterns from skin cancer images. We enhance the learning procedure of deep learning by integrating Standard U-Net and Improved MobileNet-V3 with optimization techniques, allowing the model to differentiate malignant and benign skin cancers. Also substituted the crossed-entropy loss function of the Mobilenet-v3 mathematical framework with a bias loss function to enhance the accuracy. The model's squeeze and excitation component was replaced with the practical channel attention component to achieve parameter reduction. Integrating cross-layer connections among Mobile modules has been proposed to leverage synthetic features effectively. The dilated convolutions were incorporated into the model to enhance the receptive field. The optimization of hyperparameters is of utmost importance in improving the efficiency of deep learning models. To fine-tune the model's hyperparameter, we employ sophisticated optimization methods such as the Bayesian optimization method using pre-trained CNN architecture MobileNet-V3. The proposed model is compared with existing models, i.e., MobileNet, VGG-16, MobileNet-V2, Resnet-152v2 and VGG-19 on the “HAM-10000 Melanoma Skin Cancer dataset". The empirical findings illustrate that the proposed optimized hybrid MobileNet-V3 model outperforms existing skin cancer detection and segmentation techniques based on high precision of 97.84%, sensitivity of 96.35%, accuracy of 98.86% and specificity of 97.32%. The enhanced performance of this research resulted in timelier and more precise diagnoses, potentially contributing to life-saving outcomes and mitigating healthcare expenditures.
Similar content being viewed by others
Introduction
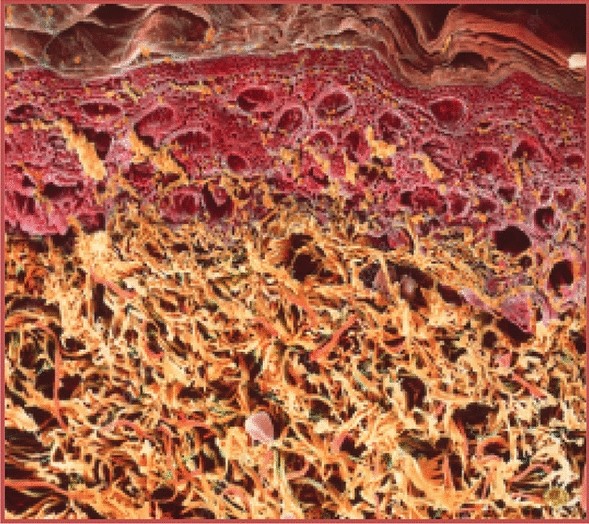
Skin cancer is considered one of the most widespread and significant forms of cancer globally, with its occurrence consistently rising in recent years. The prompt and precise identification of a medical condition is crucial for successfully implementing treatment strategies and enhancing patient results. Historically, dermatologists have traditionally depended on their professional knowledge and visual examination of skin lesions in order to detect possible malignancies. Nevertheless, this procedure is inherently subjective and prone to diagnostic inaccuracies1. In response to all these barriers, Computer-Aided Diagnosis (CAD) frameworks significantly improved medical dermatology. Deep learning models that fall into the category of "convolutional neural networks," also known as "CNNs," have shown remarkable promise for improving the accuracy of skin cancer recognition2. Figure 1 presents an image of a skin cancer sample.
Skin cancer sample23.
Melanoma and non-melanoma are the two primary subtypes of skin cancer, distinguished based on the cell that is transformed into a cancerous form. Various machine learning and deep learning frameworks and methodologies have been suggested to detect, classify, and segment skin cancer. Examples of these include Support Vector Machines (SVM), Decision Trees (DT), Fuzzy C-means, Recurrent Neural Networks (RNN), Convolutional Neural Networks (CNN) and Deep Neural Networks (DNN)3. CNN is a widely employed algorithm for automated feature learning and extraction, known for its exceptional performance in detection tasks4. Moreover, the training stage for deep learning networks often necessitates a substantial volume of data. Therefore, using transfer learning to refine a pre-existing network on comparable tasks can reduce training complexity, expedite convergence, and decrease training duration5.
Additionally, it is possible to utilize pre-trained deep learning models as feature extractors without additional training, provided they have already been trained on tasks or domains that are similar or related6. The deep learning model may acquire features that contain noise, thereby impacting the accuracy of the final classification. This can be attributed to the inclusion of non-relevant features and the naturally high dimensionality of the characteristics learned. Therefore, utilizing optimization techniques, specifically metaheuristic methods, can provide a viable approach for selecting elements. This approach involves identifying and choosing the most pertinent features, thereby enhancing the precision of recognition7.
This research paper introduces a comprehensive methodology to handle the complex issues related to skin cancer detection. This research presents a novel skin cancer recognition model based on optimized CNN architecture. This research utilizes deep learning and advanced optimization techniques to improve skin cancer detection's precision and effectiveness. The motivation behind this research originates from the critical requirement to deal with the primary healthcare problem related to dermatological cancer. Millions of people worldwide have skin cancer, and the disease's incidence is still rising. The prompt and precise identification of a condition or disease is crucial to administer the correct therapy and, finally, to preserve human life. Conventional diagnostic techniques, dependent on individual observation, are subjective and may change in precision based on the training and experience of the medical professional8.
The presence of subjectivity and the possibility of error underscore the utmost significance of advancing the development of more accurate and automated mechanisms for identifying skin cancer. The primary motivation behind our research stems from the pressing demand for enhanced techniques in detecting skin cancer. We harness their capabilities by harnessing deep learning and optimization methodologies to address this objective. Furthermore, the emergence of deep learning methods, i.e., CNNs, has shown the capacity for transformation in analyzing healthcare images. The capability of CNNs to identify complicated characteristics from visuals and to make decisions based on information presents an exciting chance for improvement in the discipline of skin diseases9. The convergence of urgent medical necessity and state-of-the-art technology constitutes the primary impetus for our investigation, compelling us to construct a sophisticated model for identifying skin cancer that harnesses the capabilities of deep learning and optimization methodologies.
The primary contributions of our research encompass innovative model architecture, meticulous hyperparameter optimization, persuasive experimental findings, and significant clinical implications. These collective achievements propel the current state of advancement in dermatological examinations and contribute to the enhancement of the treatment of patients. The proposed research presents several significant contributions to the domain of skin cancer detection and healthcare:
-
We enhance the learning procedure of deep learning by integrating Standard U-Net and Improved MobileNet-V3 with optimization techniques, which allows the model to accomplish better differentiation among malignant and benign skin cancers.
-
Our research focuses on the meticulous examination of hyperparameter optimization, a crucial factor that substantially influences the efficacy of deep learning models. Advanced optimization techniques, i.e., Bayesian optimization and grid search, are utilized to optimize the hyperparameter of the model effectively.
-
The optimization of hyperparameters is of utmost importance in enhancing the efficiency of deep learning models. To fine-tune the model's hyperparameter, we employ sophisticated optimization methods such as the Bayesian optimization method using pre-trained CNN architectures, i.e., MobileNet-V3, on the “HAM-10000 Melanoma Skin Cancer” dataset.
-
The proposed hybrid MobileNet-V3 model outperforms existing techniques based on high precision of 97.84%, sensitivity of 96.35%, accuracy of 98.86%, and specificity of 97.32%.
The article is organized in the following way: after an introductory part that provides an overview of the motivation and aims, a comprehensive examination of existing literature on skin cancer detection is presented in section two. The methodology section three offers a thorough account of the procedures employed for data collection, preliminary processing, and the development of a hybrid architecture specifically designed to detect skin cancer. Additionally, it includes a detailed explanation of the process of hyperparameter optimization. Section four provides a detailed description of the experimental setup, presents the results and performance indicators obtained, and compares them to existing methods. An extensive examination of the consequences, advantages, and drawbacks of the proposed method follows. The conclusion section five serves the purpose of combining the main findings of the research and highlighting their potential clinical significance.
Literature review
Previous research was investigated concerning the categorization of Skin Cancer using deep learning techniques. In the context of the categorization of Skin Cancer utilizing deep learning techniques, scholars generated skin lesion images sourced from publicly available websites.
Data augmentation methods were employed alongside five-fold cross-validation methods to enhance the dataset. The investigators conducted experiments to evaluate the performance of pre-trained VGG-16, ResNet50, and InceptionNet-V3 models in classifying Skin Cancer diseases. The ResNet50 model was selected due to its superior accuracy rate compared to the other models. The ResNet50 model achieves an F1 Score of 0.82, as reported in reference10. The researchers used the Xception training model with the Grad-Cam and the LIME algorithm techniques to predict skin cancer11. The Xception and the DenseNet models have implemented an integrated strategy utilizing unity. The research involved the analysis of the efficiency scores retrieved from experiments conducted on a publicly accessible dataset. These experiments were carried out using this suggested ensemble strategy. The results indicated an average recall, precision, F1 score, and accuracy rate of 86.74%, 85.8%, 86.24%, and 88.93%, respectively.
The article12 presents research on the utilization of YOLOv4-DarkNet along with active contour techniques to localize and segment melanoma. The method was evaluated on the International Skin Imaging Collaboration (ISIC) datasets for 2016 and 2018. The values of one and the reported Jaccard coefficient were 1 and 0.989, respectively. The paper13 discusses the topology of FC-DPN segmentation. The construction of the network involved the implementation of a dual-path and fully convolutional architecture. In the revised ISIC 2017 test dataset, the suggested approach achieved a Jaccard index of 81.32% and an average dice coefficient of 87.2%.
Similarly, for the PH2 dataset, a Jaccard index of 84.3% and an average dice coefficient of 91.76% were obtained. The paper discusses a CNN model for the classification of skin cancer14. The dataset was initially gathered and subsequently categorized into four distinct groups of skin cancer images. Later, augmentation techniques were employed to expand the dataset's size. During the testing phase, the algorithm developed by the researchers achieved an accuracy of 96.28%, surpassing the accuracy of the GoogleNet and MobileNet models by 1.76% and 1.12%, respectively.
The application of deep learning techniques for skin cancer detection has been the subject of considerable investigation in recent academic literature. Several deep learning techniques, including CNNs, have been utilized to categorize skin lesions as either cancerous or non-cancerous precisely. The authors of15 present a unique deep learning network called the Dual Optimisation Utilising Deep Learning Network. This network was designed for skin cancer identification using dermoscopic images and achieved an impressive precision of 98.76%. This paper presents a thorough examination of conventional and deep-learning methodologies employed in the prompt identification of skin cancer. It critically evaluates the performance of these techniques and examines the datasets utilized for training and testing purposes16. The authors have developed a deep learning system using a CNN to detect melanoma lesions. This system has demonstrated superior performance regarding diagnostic accuracy compared to existing methods, as reported in reference17. The research proposes using convolutional-based neural networks with deep reinforcement learning to identify cancer-affected skin. It aims to overcome the challenges related to generalizability by implying the adoption of ensemble models to achieve optimal output, as indicated by reference18.
Recent studies have utilized various types of classification and preliminary processing methods to conduct morphological change examines on grey-level skin cancer images. These images were obtained from the PH2 repository and were subjected to classification and clustering procedures using a pre-trained Levenberg-Mean neural network6. Transfer learning has been utilized to forecast skin cancer visuals from the HAM10000 database precisely using the MobileNet CNN19. The recent research on the application of CNN in predicting skin cancer has identified significant challenges in incorporating the entire spectrum of the patient population and various melanoma subtypes20. In addition, ongoing efforts are being made to develop optimization algorithms that enhance accuracy by adjusting hyperparameters21. Moreover, recent studies have put forth methods to identify instances of shortcut development during the training of models based on convolutional neural networks on both the ISIC Storage collection. Recent research has also emphasized using comprehensible deep-learning techniques for the multi-class separation and categorization of skin lesion images22.
Predicting skin diseases using AI holds enormous promise for better early detection and treatment results23. This study offered a new way to improve skin disease prediction models by addressing class imbalance utilizing data balancing using class weighting and transfer learning approaches. They have also investigated the usefulness of data balancing using class weighting to boost TL performance for skin disease prediction. Experiments and performance evaluations have yielded important insights and outcomes, proving that the suggested method works. Optimized kernel-enhanced Resnet-dropped extended short-term memory technique for varicose vein disease detection was addressed in24. After processing 11,350 photos of leg veins, the experiment was evaluated using metrics such as accuracy, precision, kappa, mean square error (MSE), and time complexity. With a time complexity of 25.36 ms, a kappa of 95.77%, a precision of 98.69%, and an MSE of 1.73, the suggested model attained an accuracy of 98.5%.
Although skin cancer is dangerous, it is successfully treatable if caught early. A procedure is involved in the suggested approach25. Improving the quality and extracting useful information from the raw photos is the first step in the pre-processing phase. The next step is to feed the pre-processed pictures into a GRU Network, a deep-learning model that excels at capturing sequential information. The GRU Network was fine-tuned by the author using an improved version of the Orca Predation Algorithm (OPA). In comparison to previous approaches, the GRU/IOPA system achieved better results in terms of accuracy (0.96), sensitivity (0.95), specificity (0.97), PPV (0.95), and NPV (0.96). When compared to more conventional methods, these findings show that the suggested technique is superior in detecting skin cancer.
In order to better identify skin lesions or cancer, researchers have built an upgraded machine-learning framework26. This study segments and categorizes skin diseases and cancers using a machine-learning framework and an optimization method derived from fruit flies. The proposed method provides enhanced classification efficiency with a 98% accuracy rate, 99% specificity, 96% sensitivity, 95% JSI, and 99% DSC.
In27, we looked at a framework for multi-class skin disease classification that uses an LSTM, a sophisticated CNN, and MobileNet-V2 to improve the reliability and accuracy of cancer diagnoses. The proposed method leverages CNNs' self-learning discriminative features from unprocessed skin photos and long short-term memory (LSTM) capability to manage multi-class classification problems. The hybrid model showed promise in the experiments for improving the accuracy and efficiency of skin disease classification across a variety of categories.
The authors of28 laid up a two-pronged approach to skin lesion categorization. First, during the image pre-processing phase, two distinct techniques were suggested for picture segmentation and feature extraction. Finally, S-MobileNet, a model for a deep convolutional neural network, is being developed with the intention of classifying seven distinct skin lesion types. When it comes to skin lesion picture classification in the HAM10000 dataset, the suggested deep learning-based S-MobileNet model is the way to go, according to experimental results.
In29, the authors provide a deep-learning architecture that can identify Melanoma and multi-class skin cancers. Four main phases make up the suggested architecture: pre-processing images, extracting and fusing features, selecting features, and finally, classification. Using the picture luminance data, a new method for enhancing contrast was suggested. The next step is to train two pre-trained deep models, DensNet-201 and DarkNet-53, using transfer learning to modify them with respect to a residual block at the end. The last step in the classification process was to use machine learning classifiers on the features that were chosen. For this experiment, we used two datasets: ISIC2018 and ISIC201929,30. This dataset achieved the highest precision of 85.4%, whereas the other achieved 98.80%. Table 1 presents a comparative analysis of existing skin cancer research using a deep learning model.
Materials and methods
Skin cancer dataset
This research utilizes the online ‘HAM-10000’ skin cancer dataset33. The dataset HAM-10000, referred to as 'Human against the machine', with 10,000 images used for training, is a collection of images of skin lesions utilized in skincare research. The dataset comprises visual representations of diverse dermatological disorders, encompassing Melanoma, nevus, and several related afflictions. The provided dataset is used to classify and diagnose skin diseases. As mentioned earlier, deep learning models trained on the dataset can discern different types of skin cancer, including malignant tumours that may exhibit malignant characteristics.
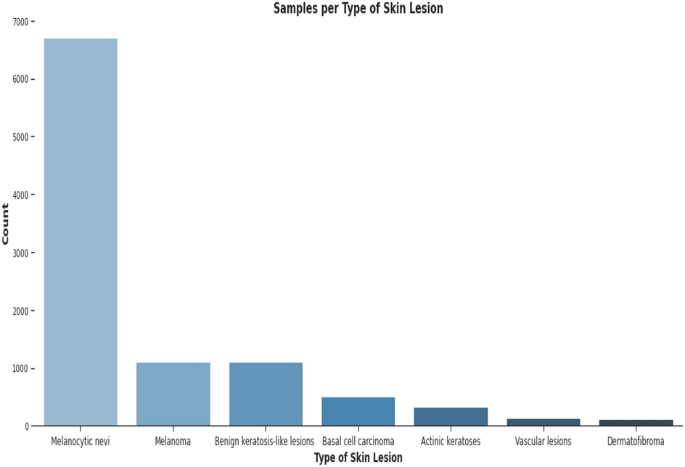
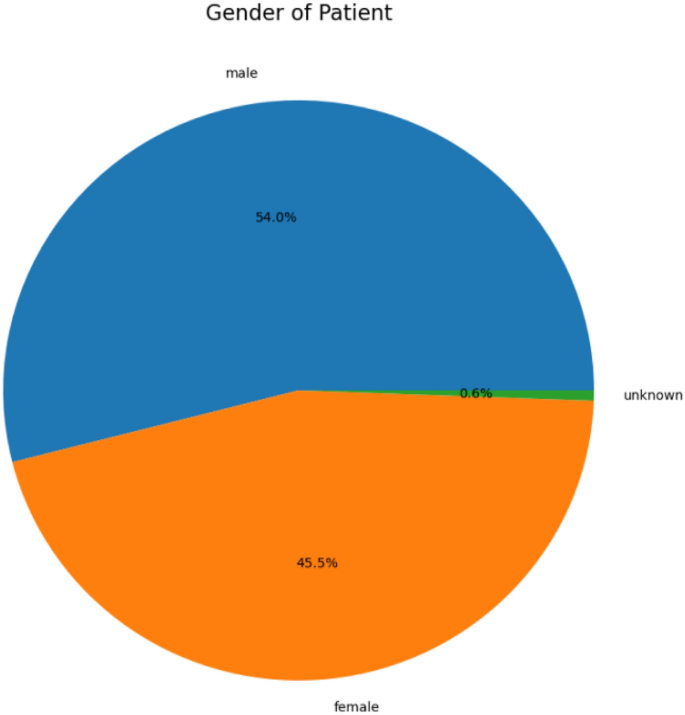
This dataset contains 10,015 dermatoscopic images with size (450*600) pixels. The dataset comprises seven diagnostic Skin cancer categories. The dataset classes include classes from zero to six, names as ‘melanoma’, ‘melanocytic nevus’, ‘basal cell carcinoma’, ‘actinic keratosis’, ‘benign keratosis’, ‘dermatofibroma’ and ‘vascular lesion’. Figure 2 presents the details of skin cancer classes and counts, and Fig. 3 illustrates the gender-wise distribution of skin cancer infection, including a 54% male, 45.5% Female and 0.5% unknown patient distribution in the dataset.
Data pre-preprocessing
A critical first step in getting a skin cancer dataset ready for training a skin cancer identification framework is data preliminary processing. In addition to promising that the data is in a format appropriate for training, proper data pre-processing can enhance model performance31. The skin cancer dataset is pre-processed using the following crucial steps.
Data augmentation
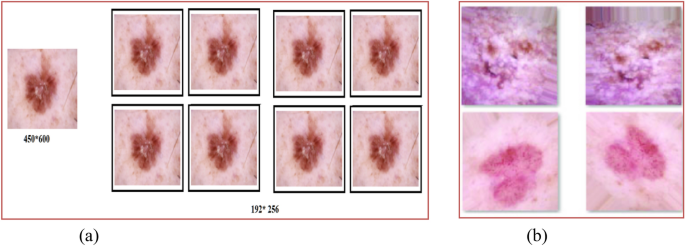
Since there are unequal numbers of images in each category, data balancing is used to balance all types before the training procedure. Data augmentation techniques are used for data balancing. In this process, the following ranges are used: (a) rotation 25 degrees; (b) width and height shifting 15%; (c) shearing 15%; (d) employing flipping in both the vertical and horizontal directions; and (5) adjusting brightness within the [0.9: 1.5] range. Data augmentation is also applied to the images during the learning and optimization stages to prevent over-fitting and boost diversity. Table 2 presents the parameters used for the skin cancer dataset. After pre-processing, the images of (450*600) pixels were converted into 192*256 pixels. Figure 4 presents data augmentation results. Table 3 shows the data count after the data pre-processing steps for class 0 to class 6.
We use Eq. (1) for horizontal flipping operation, i.e., x-axis, 2 for rotation and 3 for shifting, 4 for shearing, and 5 for zooming. In these equations, h represents the rotating angle, tx represents the amount of shifting in tandem with the x-axis, ty represents the shifting in tandem with the y-axis, shx represents the shear factor in tandem with the x-axis, shy represents the shear factor together the y-axis, and Cx represents the zoom factor together the x-axis, and Cy represents the zoom factor in tandem the y-axis32. Here, FM is the flipping Matrix, RM is the rotation Matrix, SM is the shifting Matrix, SheM is the shearing Matrix, and ZM is the zooming Matrix.
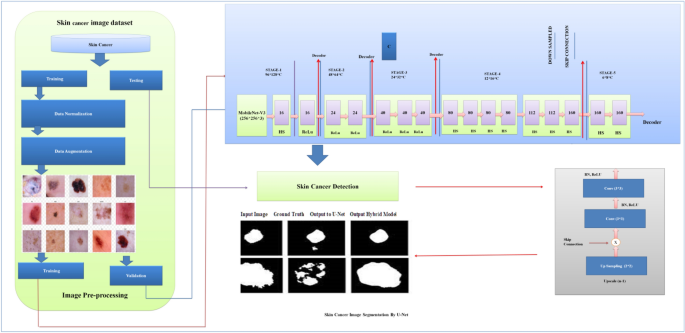
Proposed model architecture
The proposed model is based on Standard U-Net and Improved MobileNet-V3 with optimization techniques, i.e., the Bayesian optimization method. Standard U-Net performs semantic segmentation activities in the proposed model, and MobileNet-V3 is used as a Feature Extractor. We also utilize a Bayesian optimization method for hyperparameter optimization. This method can identify the most promising hyperparameters by prioritizing those that have shown favourable outcomes in previous results. Figure 5 shows the architecture of the proposed hybrid model.
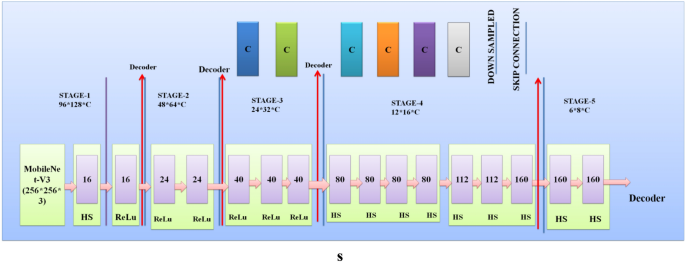
Improved MobileNet-V3
In the proposed hybrid model, the existing MobileNet-V3 model is improved. The Improved MobileNet-V3 worked as an encoder in the proposed skin cancer prediction and segmentation model. The steps below enhanced the MobileNet-V3 structure for skin cancer recognition and segmentation. Figure 6 presents the architecture of the proposed MobileNet-V331.
Architectural level Improvements: The following fundamental changes were performed at the existing MobileNet-V3 architecture32.
-
Deeper Model A deeper MobileNet-V3 model's depth (layer counts) is determined by the model's structural preferences. MobileNet-V3 is available in two predetermined sizes: "large" or "small," with "large" featuring more layers and greater capacity than "small." The "large" variant of MobileNet-V3 generally includes 157 layers. Depthwise separable convolution layers and flipped residuals using growing and squeeze-and-excitation (SE) segments are formed.
-
Wider Model MobileNet-V3 predominantly employs the flipped residual block and SE block. A depthwise convolution component is subsequently followed by a point-wise convolution layer to form the inverted residual block. The point-wise convolution changes the width (number of channels). Adjust the point-wise convolution layer output channels to widen a layer. This is typically accomplished by multiplying the total amount of channels through a scaling factor. Modulating channel-wise dependencies is done with the SE block. Although it cannot naturally regulate layer width, it can be utilized on layers to enhance model performance and adjust to particular tasks. Fully connected layers (FCL), Global average pooling (GAP), and element-wise scaling (EMS) comprise the SE block. The number of channels present in the map of input features is used as a criterion to establish the size of the SE block. MobileNet-V3 allows you to modify the range of channels within the starting convolutional layer with the last classification layer to adjust the total width of the resulting model for skin cancer analysis.
-
Attention Method We substituted the crossed-entropy loss function of the Mobilenet-v3 mathematical framework with a bias loss function that enhanced accuracy. The model's SE component was replaced with the adequate channel attention (ECA) component to achieve parameter reduction. Integrating cross-layer connections among Mobile modules has been proposed to leverage synthetic features effectively. The dilated convolutions were incorporated into the model to enhance the receptive field.
Regularization method
The following Regulization techniques were applied to improve the MobileNet-V3 model32.
-
Dropout Implement dropout layers inside the MobileNet-V3 structure to prevent overfitting throughout training. Dropout arbitrarily eliminates a portion of the neurons throughout each forward pass to improve the model's generalization ability.
-
L2 regularization's weight decay Applying a weight decay component to the model's loss function for the L2 regularization's weight decay step. Weight decay promotes the reduction of model weights, preventing unnecessary complexity and overfitting.
Normalization method
The following Normalization techniques were applied for improvements in the MobileNet-V3 model.
-
Batch Normalization To stabilize training, employ batch normalization layers to normalize the activations throughout each mini-batch. Batch normalization can boost the model convergence process and boost training.
-
Layer Normalization We have applied a layer normalization method that helps
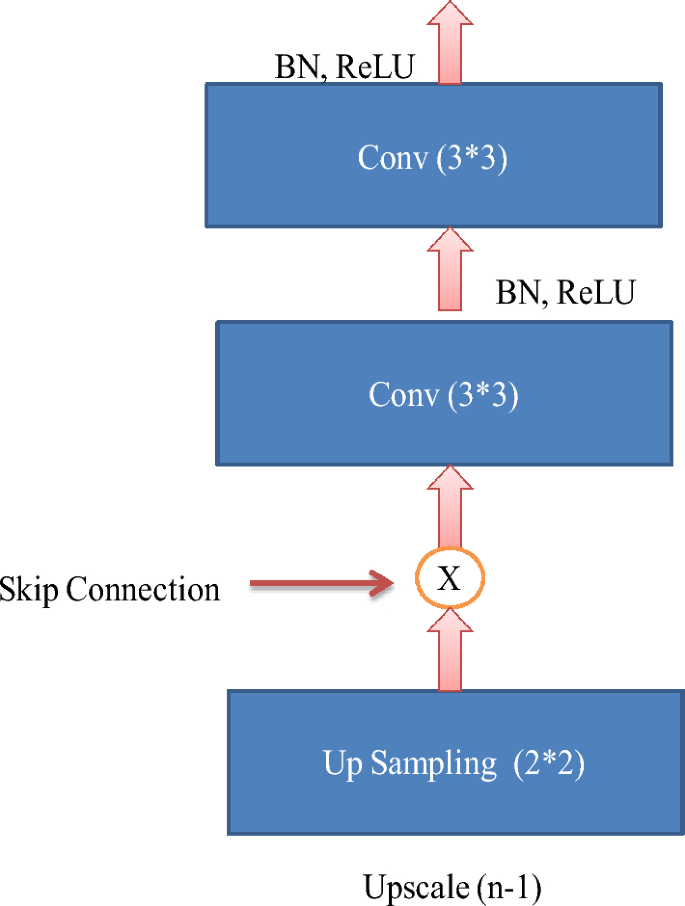
Standard U-Net architecture
The Standard U-Net architecture is a convolutional neural network specifically developed for semantic segmentation tasks. The algorithm demonstrates exceptional proficiency in partitioning regions of interest within medical images, rendering it highly suitable for the analysis of skin cancer. The Standard U-Net architecture is distinguished by incorporating skip connections and embedded skip procedures, which efficiently capture multi-scale context-relevant data33.
Four Standard U-Net patterns, identical to U-Net, are used to complete the segmentation assignment. Batch normalization and GeLU for the hidden activation mechanism are utilized in the additional configuration, while the architecture described in10 is used in the initial setup. Batch normalization (BN) mainly creates batches of a specific size. Along with batch normalization and the GeLU hidden activation function, the third and fourth patterns use VGG-19 and DenseNet-201 as their backbone. In the case of configuration four, deep supervision is not enabled. Figure 7 presents the standard U-Net architecture.
Bayesian optimization method
Bayesian optimization is an approach that employs probabilistic algorithms to search accurately for the most practical combination of hyperparameters to support a model built using deep learning. It functions by analyzing an ambiguous objective function within this instance, which evaluates the model's effectiveness as a Gaussian procedure, enabling it to make well-informed choices about where to start sampling the target function subsequently. The following describes the operation of Bayesian optimization in the hyperparameter optimization for skin cancer6.
-
Step 1: Initial Random Sampling To create an initial substitute framework for the objective function, Bayesian optimization usually begins with a few random specimens taken through the hyperparameter space. The function's behaviour can be partially understood because of these arbitrary specimens.
-
Step 2: Surrogate Model The algorithm generates a probabilistic substitute model using the initial specimens, generally a Gaussian procedure (GP). The GP prototypes the objective function's allocation and predicts the function's behaviour throughout the hyperparameter area. This substitute model encompasses average forecasting and an uncertainty determination (variance) at every point within the hyperparameter space.
-
Step 3: Acquisition Function Bayesian optimization utilizes an acquisition function for identifying the subsequent objective function specimen location. Typical acquisition functions consist of Probability of Improvement (PI), Expected Improvement (EI), and Upper Confidence Bound (UCB). These features balance examinations (sample collection in spaces of uncertainty) and exploitation (sampling in spots that are likely to produce more effective results).
-
Step 4: Next Sample Selection The acquisition function directs the selection of the subsequent collection of hyperparameters to be assessed. The method chooses hyperparameter values that maximize the acquisition function, indicating promising regions within the hyperparameter space for enhancing the objective function.
-
Step 5: Evaluate Objective Function The chosen hyperparameters are utilized for training and evaluating a deep learning framework via the skin cancer dataset. The objective function (including model precision and loss) gets calculated according to the model's efficiency.
-
Step 6: Update Surrogate Model: After assessing the objective function based on the chosen hyperparameter, the procedure upgrades the substitute model (GP) along with the newly acquired data point, including the evaluation results, to minimize uncertainty within the substitute model.
-
Step 7: Iteration Steps 3 through 6 are carried out for an established amount of iterations or until convergence is achieved. The method improves the substitute model iteratively and chooses a hyperparameter to enhance the model's accuracy.
-
Step 8: Final Result The Bayesian optimization method produces the hyperparameters, which generate the best objective function importance according to the model's behaviour.
Transfer learning
ImageNet is used as a pre-training dataset for the MobileNet-V3 model, and then the Ham-10000 skin cancer dataset is used to fine-tune the model's parameters. Transfer learning enables the predictive algorithm to utilize features acquired within a broader context before becoming proficient in the skin cancer recognition assignment34.
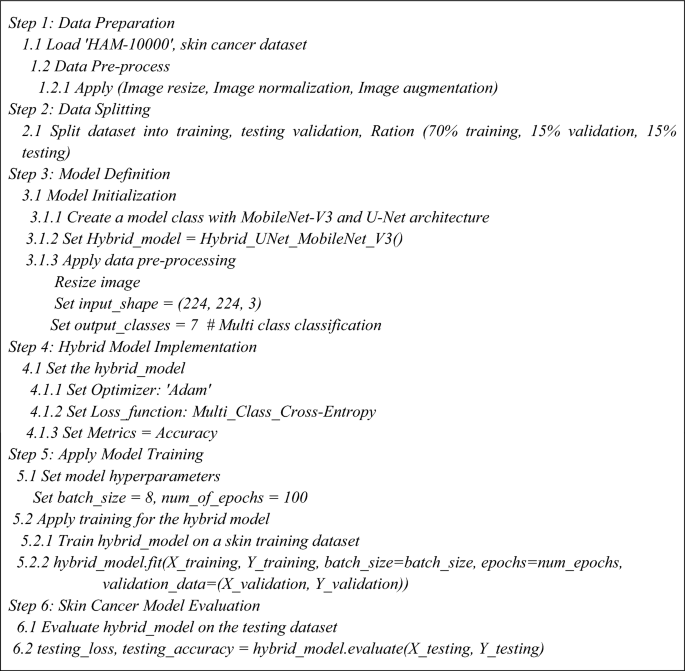
Pseudo code for the proposed model
Algorithm 1 presents the steps for skin cancer analysis with the hybrid U-Net and MobileNet-V3 models35.
Performance measuring parameters
We use parameters like accuracy, precision, F-measure, the area under the curve (AUC), and confusion metrics6,31,32,33 to determine how to determine the present model and the one we have suggested works. The components of the confusion matrix, including TP (true positive), TN (true negative), FP (false positive), and FN (false negative), have been utilized in its construction. The subsequent passage comprehensively explains the previously referenced statistics34.
-
Precision (Prc) This illustrates the proportion of individuals who test positive correctly (true positives) and incorrectly (false positives) concerning the total number of positive individuals as described in Eq. (6).
$$Prc=[\frac{TP}{(TP+FP)} ]$$(6) -
Recall (RC) or Sensitivity The calculation of recall, also known as true positive rate35, involves dividing the number of true positives by the total number of instances that ought to be considered anticipated as positive, as described in Eq. (7).
$$RC=[\frac{TP}{\left(TP+FN\right)} ]$$(7) -
F-Measure (FMs) The F-score, often referred to as the 'F1 score' or 'F-measure'36, serves as an empirical metric for assessing the effectiveness of a deep learning model. The integration of recall and precision results in an integrated score, as described in Eq. (8).
$$FMs=\{2*[\frac{ Prc \times RC}{ Prc+RC}] \}$$(8) -
Accuracy (ACR) The evaluation of classification models often involves the consideration of various metrics, with accuracy being one of them37. In a more formal context, accuracy can be defined as the proportion of correct predictions our model makes, as described in Eq. (9).
$$ACR=\{\frac{(TP+TN)}{[(TP+FN)+(TP+FP)]} \}$$(9) -
Area Under the Curve (AUC) AUC refers to measuring the extent or size of two areas under a curve, which refers to the region bounded by the curve and the coordinate axes33,38. To determine this area, one can divide it into infinitesimally small rectangles and sum their areas. By incorporating the limit of this summation, as the rectangles become infinitely small, the total area under the curve can be calculated.
Ethical approval and consent to participate
No ethical approval is required, and the authors consent to participate in the paper.
Experimental results and evaluation
This section covers the simulation results of the existing and proposed model.
Experimental setup
The proposed and existing techniques, i.e., MobileNet, Resnet-152v2, VGG-16, MobileNet-V2, and VGG-19, were implemented using software and hardware components. Table 4 presents the parameters used in experimental analysis for proposed and existing models. Table 5 shows the Configuration parameters of Standard U-Net architecture used in a proposed hybrid model for image segmentation39,40,41,42,43.
Simulation results and discussion
The HAM-10000 Skin cancer dataset serves as the training ground for the proposed model and several existing deep learning models, i.e., MobileNet, Resnet-152v2, VGG-16, MobileNet-V2, and VGG-19. The dataset was divided into training, testing and validation with a ratio of 70:15:15. The experimental results and discussion are as follows.
Table 6 presents the experimental results of the testing dataset for 100 epochs for existing and proposed models. The combined utilization of the U-Net and MobileNet-V3 models yielded exceptional results in classifying skin cancer diseases.
Table 7 presents the experimental results of the validation dataset for 100 epochs for existing and proposed models. The proposed model demonstrated validation results with an accuracy of 98.03%, wherein the precision, recall, and F1-score all surpassed 94%.
Visualization of simulation results
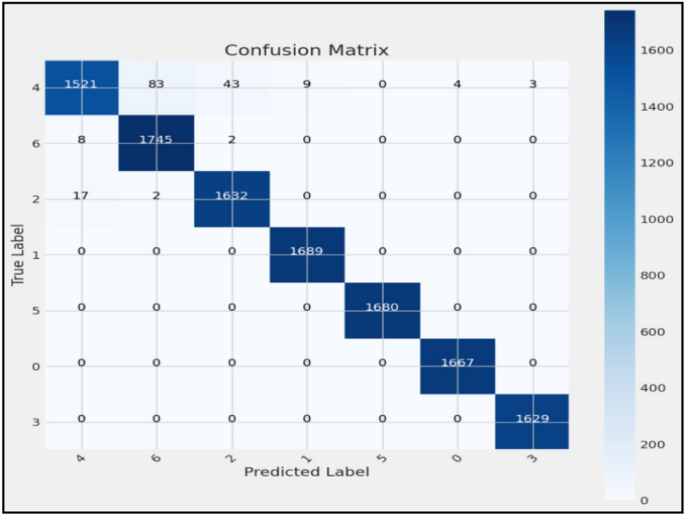
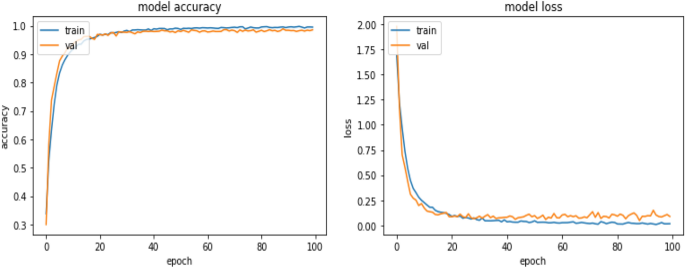
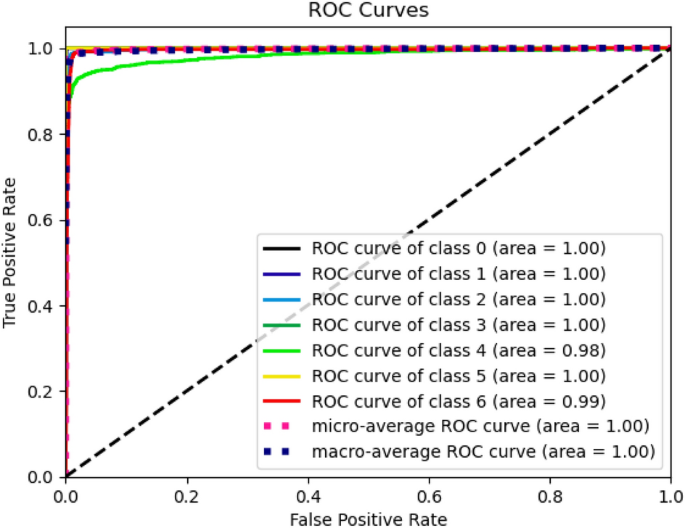
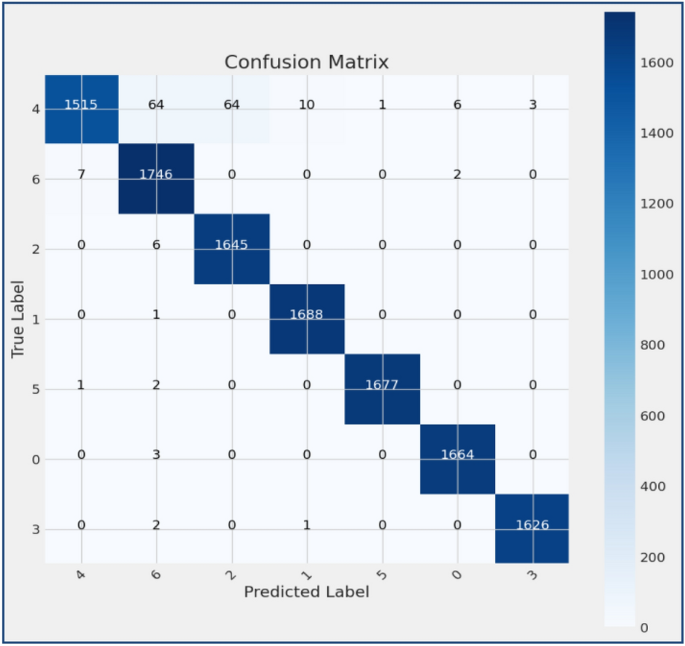
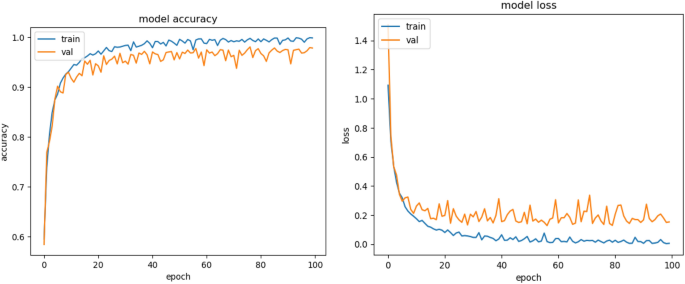
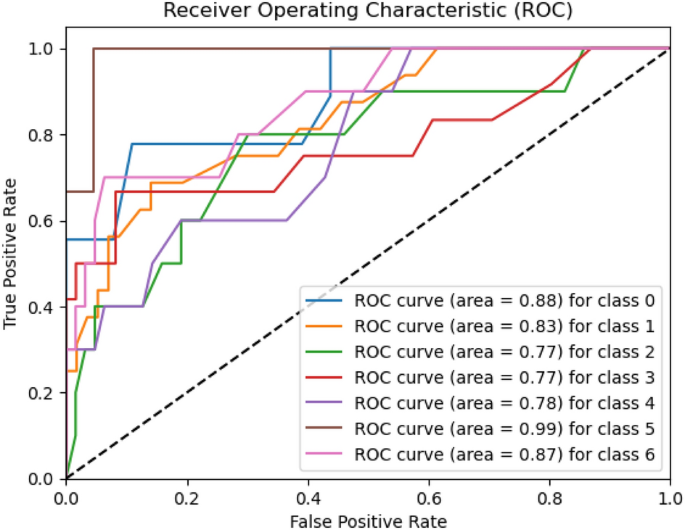
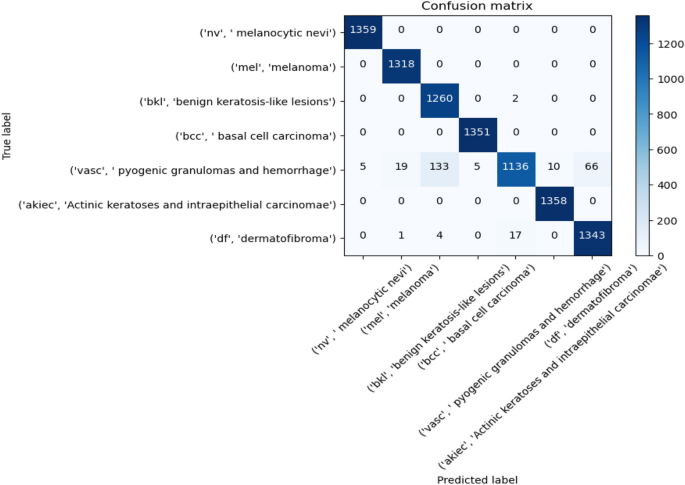
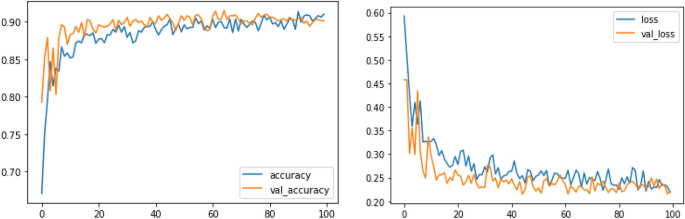
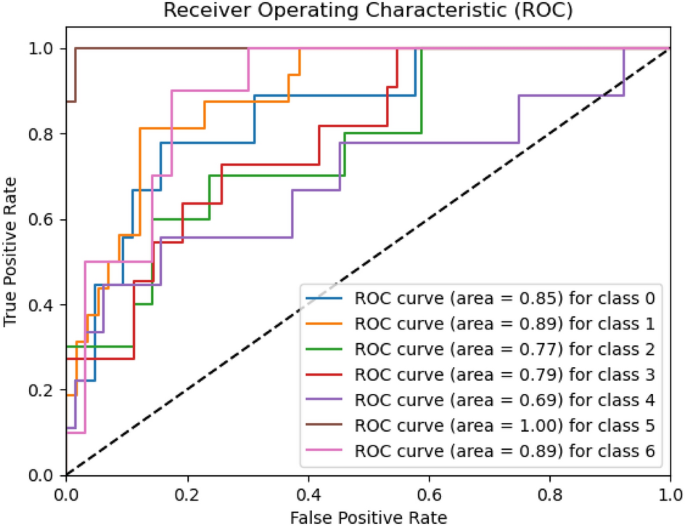
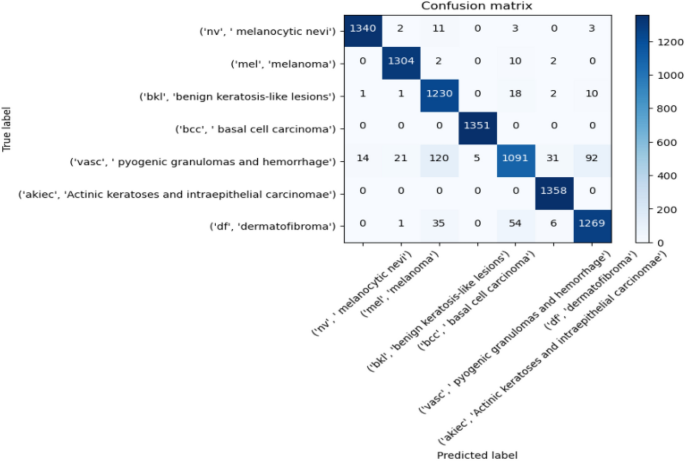
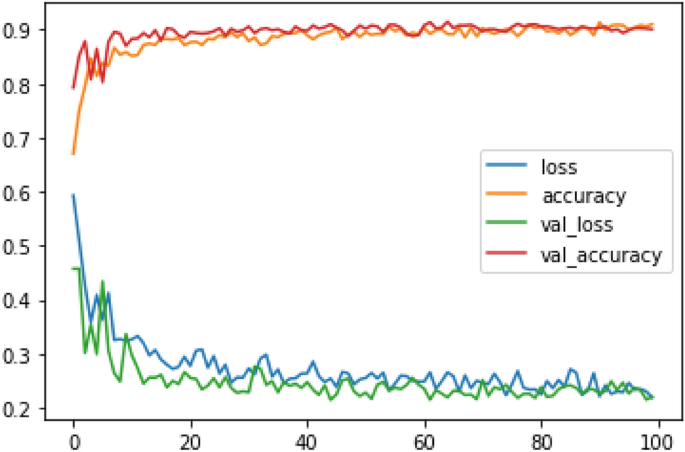
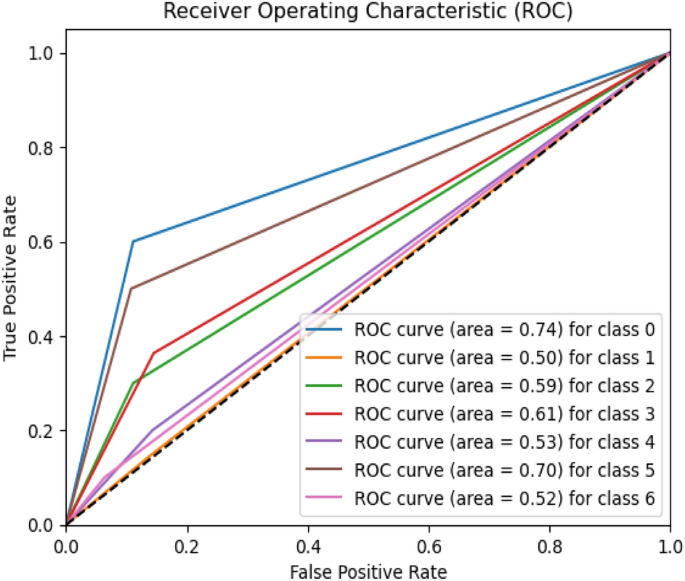
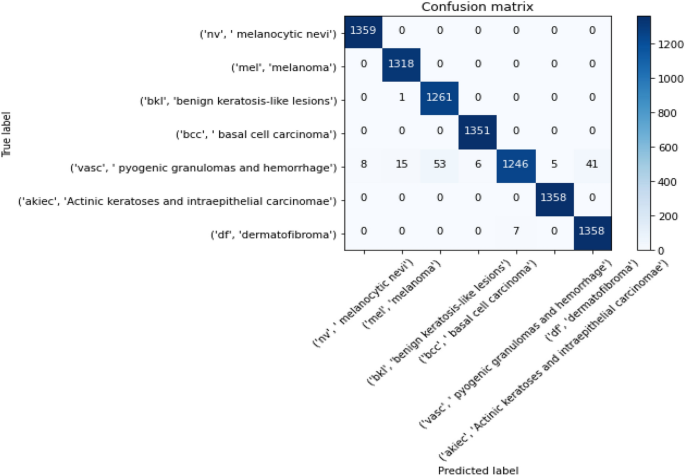
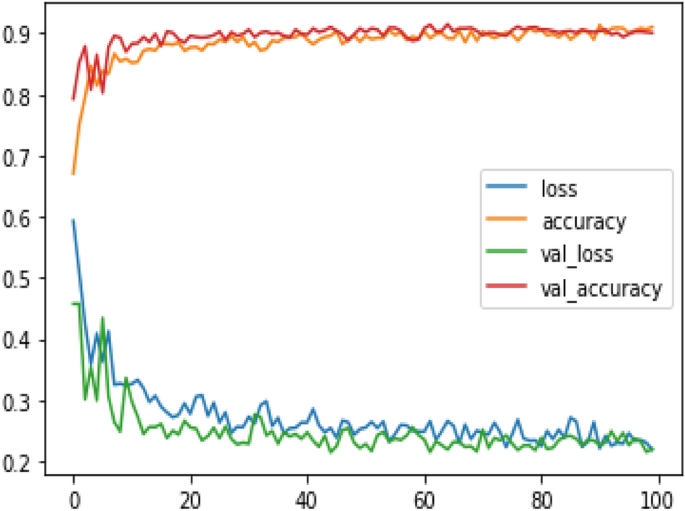
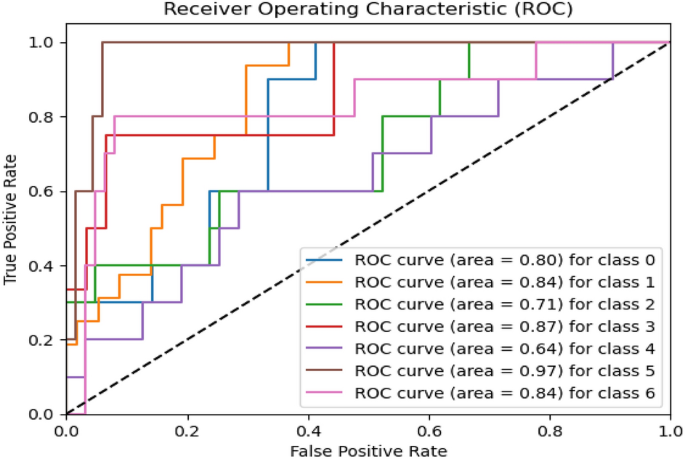
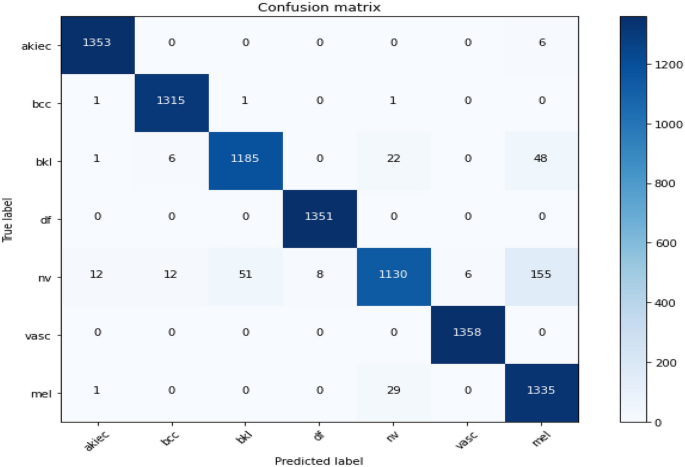
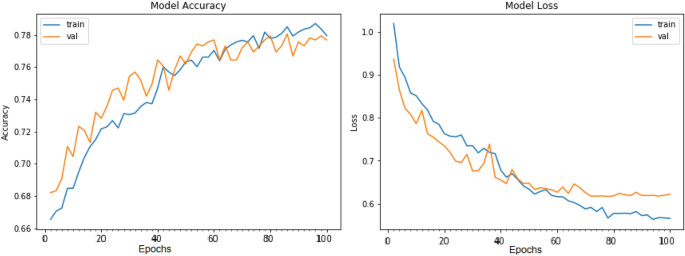
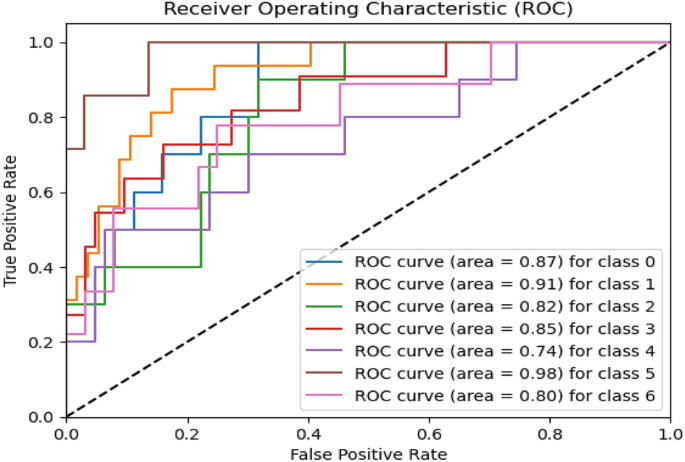
Figures 8, 9, 10 present a visualization of simulation results for the proposed model on the “HAM-10000” skin cancer dataset. Figure 8 presents the Confusion Matrix of the Proposed Model, Fig. 9 illustrates the Model Accuracy and Loss of the Proposed Model, and Fig. 10 shows an ROC Curve of the Proposed Model. Figures 11, 1213 present a visualization of simulation results for the MobileNet Model on the “HAM-10000” skin cancer dataset. Figure 11 presents the Confusion Matrix of the MobileNet Model, Fig. 12 illustrates the Model Accuracy and Loss of the MobileNet Model, and Fig. 13 shows an ROC Curve of the MobileNet Model.
Figures 14, 15, 16 present a visualization of simulation results for the MobileNet-V2 Model on the “HAM-10000” skin cancer dataset. Figure 14 presents the Confusion Matrix of the MobileNet-V2 Model, Fig. 15 shows the Model Accuracy and Loss of the MobileNet-V2 Model, and Fig. 16 illustrates an ROC Curve of the MobileNet-V2 Model.
Figures 17, 18, 19 present a visualization of simulation results for the VGG-16 Model on the “HAM-10000” skin cancer dataset. Figure 17 presents the Confusion Matrix of the VGG-16 Model; Fig. 18 illustrates the Model Accuracy and Loss of the VGG-16; Fig. 19 shows an ROC Curve of the VGG-16 Model.
Figures 20, 21, 22 present a visualization of simulation results for the VGG-19 Model on the “HAM-10000” skin cancer dataset. Figure 20 presents the Confusion Matrix of the VGG-19 Model; Fig. 21 illustrates the Model Accuracy and Loss of the VGG-19; Fig. 22 shows an ROC Curve of the VGG-19 Model. Figures 23, 24, 25 present a visualization of simulation results for the Resnet-152v2Model on the “HAM-10000” skin cancer dataset. Figure 23 presents the Confusion Matrix of the Resnet-152v2 Model; Fig. 24 illustrates the Model accuracy and loss of the Resnet-152v2; Fig. 25 shows an ROC Curve of the Resnet-152v2 Model. Based on the analysis of the results, it’s clearly proven that the proposed model has better simulation outcomes than existing models.
Results and discussion
The HAM-10000 Skin cancer dataset is utilized for the proposed model and several existing deep learning models, i.e., MobileNet, Resnet-152v2, VGG-16, MobileNet-V2, and VGG-19. Table 6 presents the experimental results of the testing dataset for 100 epochs for existing and proposed models. The combined utilization of the U-Net and MobileNet-V3 models yielded exceptional results in classifying skin cancer diseases. The model demonstrated a set of validation results with an accuracy of 98.86%, wherein the precision, recall, and F1-score all surpassed 95%. The model's capability to distinguish between cancerous and non-cancerous tumours is demonstrated by the ROC-AUC score of 98.45%, indicating excellent performance. The model consistently demonstrated a strong performance on the test set, achieving an accuracy rate of 98.45%.
The evaluation metrics, precision, accuracy, recall, ROC-AUC and F1-score, exhibited remarkable performance on the testing dataset, surpassing 95% for each metric. The ROC-AUC result of 98.45% reaffirms the model's robustness compared to the proposed model, existing MobileNet achieved, reaching 89% for each performance metric. Resnet-152V2 was achieved, surpassing 88% for each performance metric; VGG-16 was achieved, exceeding 89% for each performance metric. MobileNet-V2 achieved, exceeding 90% for each performance metric, and VGG-19 achieved, surpassing 90.50% for each performance metric. These results indicate that the proposed model achieved outstanding results over existing deep learning models.
Table 7 presents the experimental results of the validation dataset for 100 epochs for existing and proposed models. The proposed model demonstrated validation results with an accuracy of 98.03%, wherein the precision, recall, and F1-score all surpassed 94%. The model's capability to distinguish between cancerous and non-cancerous tumours is demonstrated by the ROC-AUC score of 97.09%, indicating excellent performance. The evaluation results show precision, accuracy, recall, ROC-AUC, and F1-score, exhibiting remarkable performance on the validation dataset, surpassing 94% for each metric. The ROC-AUC result of 97.09% reaffirms the model's robustness. As compared to the proposed model, the existing model, i.e., MobileNet achieved, surpassing 87% for each performance metric, Resnet-152V2 achieved, surpassing 87.02% for each performance metric VGG-16 achieved, reaching 88% for each performance metric, MobileNet-V2 achieved, exceeding 89% for each performance metric, and VGG-19 achieved, surpassing 88.50% for each performance metric. These results indicate that the proposed model achieved outstanding results over existing deep learning models.
Figures 8, 9, 10 present a visualization of simulation results for the proposed model, Figs. 11, 12, 13 present a visualization of simulation results for the MobileNet Model, Figs. 14, 15, 16 present a visualization of simulation results for the MobileNet-V2 Model, Figs. 17, 18, 19 shows a visualization of simulation results for the VGG-16 Model, Figs. 20, 21, 22 present a visualization of simulation results for the VGG-19 Model on the “HAM-10000” skin cancer dataset. Similar Figs. 23, 24, 25 present a visualization of simulation results for the Resnet-152v2Model on the “HAM-10000” skin cancer dataset. Based on the analysis of the results, it’s clearly proven that the proposed model has better simulation outcomes than existing models. Existing models such as MobileNet, VGG-16, MobileNet-V2, ResNet-152v2, and VGG-19 did not perform as well as the Hybrid U-Net, and Improved MobileNet-V3 model with hyperparameter optimization did on the "HAM-10000 Melanoma Skin Cancer dataset." There are several reasons for this.
-
Architecture of U-Net The U-Net architecture has gained recognition for its efficacy in the field of image segmentation, particularly in tasks related to skin cancer detection, where the objective is to delineate skin tumours from the tissue that surrounds them accurately. The U-Net's capacity to effectively capture intricate details and delineations contributes to enhanced feature extraction and superior classification outcomes.
-
Improved MobileNet-V3 MobileNet-V3 is a CNN architecture that has been specifically developed to prioritize both efficiency and accuracy. The enhanced iteration of the dataset takes into account alterations and refinements that render it better suited for the unique attributes of the skin malignancies dataset.
-
Feature extraction by Hybrid Model The hybrid models were created by integrating the advantageous features of both U-Net and MobileNet-V3. The provided system offers precise segmentation masks, whereas MobileNet-V3 efficiently extracts features from the segmented regions. The integration of these characteristics enhances the model's comprehension of images related to skin cancer.
-
Optimization of Hyperparameter The utilization of hyperparameter optimization techniques enables the refinement of the model's parameters and structural decisions, specifically tailored to the skin cancer dataset. In comparison with models with standard hyperparameters, this led to better performance and broad applicability.
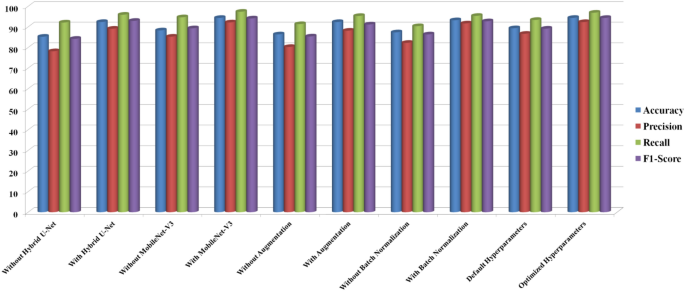
Ablation analysis
We performed ablation research to determine the effect of critical parameters in the proposed skin cancer analysis model. To check the proposed model performance, we have conducted an ablation analysis with various conditions, which include (a) with and without Hybrid U-Net, (b) with and without MobileNet-V3, (c) with and without Augmentation, (d) with and without Batch Normalization, (e) with and without Hyperparameters. After methodically removing and testing with every single subsequent component eliminated, the following observations were found.
Various factors on the skin dataset were compared in the ablation analysis, as shown in Table 8 and Fig. 26. For example, when it came to identifying complicated characteristics inside skin lesions, performance metrics dropped when the Hybrid U-Net was not used. There has been a significant gain in accuracy, suggesting that the Hybrid U-Net is vital in lowering the model's false positive rate and improving its capacity to detect cancerous tumours accurately. Improving MobileNet-V3 is crucial for efficient feature extraction since its absence significantly reduced total accuracy. There is strong evidence from the improved accuracy that Improved MobileNet-V3 helps cut down on false positives.
Results showed that model resilience was reduced in the absence of data augmentation, highlighting the need for dataset augmentation for improved generalizability. Increases in accuracy and F1-score demonstrate how data augmentation enhances the model's capacity to categorize cancerous tumours accurately. A decrease in overall model performance and a slowdown in training convergence were the outcomes of removing batch normalization layers. Improving the model's capacity to distinguish between benign and malignant lesions and stabilizing the training process are both achieved using batch normalization, as seen by the significant gains in accuracy and F1-score. We found that the model's sensitivity to distinguishing between benign and malignant lesions is greatly affected by the ideal values of the hyperparameters. These enhanced precision and accuracy show how critical hyperparameter adjustment is for getting the most out of a model. All of the steps and parts of our skin cancer diagnostic methodology are vital, as these results show. In addition to shedding light on the model, the ablation research provides valuable information for making future upgrades and enhancements. Here are some practical ways to improve the model's diagnostic accuracy and reliability: observe the changes in performance measures.
Conclusion and future works
The proposed research integrates Hybrid U-Net and Improved MobileNet-V3 features to formulate a new hybrid model for skin cancer detection. Our model, showcasing superior diagnostic accuracy, emphasizes the pivotal roles of Hybrid U-Net and Improved MobileNet-V3 through a comprehensive assessment involving an ablation study and a comparison with state-of-the-art models. Beyond delivering a high-performing model, the study offers insightful directions for future research, contributing to the advancements in automated skin cancer detection. The observed enhancements, coupled with our competitive standing against current models, suggest a potentially significant therapeutic impact. According to the authors, this study introduces new possibilities for research and development in medical image analysis, promising faster and more accurate skin cancer diagnostics.
This research introduces an innovative skin cancer detection method incorporating U-Net and MobileNetV3 architecture, employing hyperparameter optimization strategies. By combining advanced deep learning techniques and meticulous parameter optimization, the result is a highly accurate and efficient system for diagnosing skin cancer. This work significantly improves skincare and medical services by providing a valuable tool for skin specialists and doctors to enhance the timely detection of skin malignancies and improve patient outcomes. The proposed model is compared with existing models, namely MobileNet, VGG-16, MobileNet-V2, Resnet-152v2, and VGG-19 on the "HAM-10000 Melanoma Skin Cancer dataset".
To fine-tune the model's hyperparameter, we employ sophisticated optimization methods such as the Bayesian optimization method using the pre-trained CNN architecture MobileNet-V3. Empirical findings demonstrate that the proposed optimized hybrid MobileNet-V3 model outperforms existing skin cancer detection and segmentation techniques, achieving high precision (97.84%), sensitivity (96.35%), accuracy (98.86%), and specificity (97.32%). The enhanced performance of this research can lead to timelier and more precise diagnoses, potentially contributing to life-saving outcomes and mitigating healthcare expenditures. The developed model holds significant potential in terms of clinical relevance, as suggested by its precision and recall scores, making it a valuable tool for dermatologists in the early detection of skin cancer. The elevated accuracy level presents a potential avenue for mitigating misdiagnoses and improving patient outcomes.
In the proposed model, computational demands during training and inference may arise as a consequence of integrating two complicated designs. This limitation should be taken into account, particularly in situations when resources are limited. Also, interpretability is a common issue for deep learning models like the proposed model. In clinical situations, the model's interpretability is limited because, despite its good performance, comprehending the precise elements underlying the classification judgments might be difficult.
In order to reduce computing complexity, future studies should concentrate on improving the model. To improve the practicality of deployment, it may be worthwhile to investigate model compression approaches or lightweight designs. Solving problems with interpretability might be crucial. Healthcare providers may gain confidence and knowledge of the model's decision-making process with the use of explainable AI approaches. Future research in the area of automated skin cancer detection will be guided by this balanced approach, which adds to the current conversation in the field. Future research should explore incorporating supplementary clinical data, developing interpretability methods tailored for medical professionals, and addressing the ethical implications associated with implementing artificial intelligence models for skin cancer diagnosis. Our commitment to innovation remains central as we aim to make a significant impact within dermatology. While the proposed model exhibits exemplary performance on the HAM-10000 dataset, it is crucial to recognize that real-world medical records may show unforeseen variations. Additional validation is necessary to extend the model's capabilities to datasets and situations in healthcare that have not been previously encountered.
Data availability
The data supporting the research results of the present research can be obtained by contacting the corresponding author.
Abbreviations
- DL:
-
Deep learning
- ISIC:
-
International skin imaging collaboration
- ADAM:
-
Adaptive moment optimization algorithm
- FC:
-
Fully connected
- DL:
-
Deep learning
- CNN:
-
Convolution neural network
- BN:
-
Batch normalization
- SVM:
-
Support vector machine
- ReLu:
-
Rectified linear unit
- TL:
-
Transfer learning
References
Ismail, W. N. & Alsalamah, H. A. Efficient Harris Hawk optimization (HHO)-based framework for accurate skin cancer prediction. Mathematics 11(16), 3601 (2023).
Mohakud, R. & Dash, R. A hybrid model for classification of skin cancer images after segmentation. Int. J. Image Graph. 31, 2550022 (2023).
Ogundokun, R. O. et al. Enhancing skin cancer detection and classification in dermoscopic images through concatenated MobileNetV2 and xception models. Bioengineering 10(8), 979 (2023).
Nancy, V. A., Osvin, P. P., Arya, M. S. & Shamreen Ahamed, B. Comparative research and analysis on skin cancer detection using machine learning and deep learning algorithms. Multim. Tools Appl. 82, 1–45 (2023).
Sharma, G., & Raman, C. An optimized predictive model based on deep neural network for detection of skin cancer and oral cancer. In 2023 2nd International Conference for Innovation in Technology (INOCON), 1–6 (IEEE, 2023).
Behara, K., Bhero, E. & Agee, J. T. Skin lesion synthesis and classification using an improved DCGAN classifier. Diagnostics 13, 2635 (2023).
Mampitiya, L. I., Rathnayake, N. & De Silva, S. Efficient and low-cost skin cancer detection system implementation with a comparative research between traditional and CNN-based models. J. Comput. Cogn. Eng. 2(3), 226–235 (2023).
Akilandasowmya, G., Nirmaladevi, G., Suganthi, S. U. & Aishwariya, A. Skin cancer diagnosis: Leveraging deep hidden features and ensemble classifiers for early detection and classification. Biomed. Signal Process. Control 88, 105306 (2023).
Salih, O. & Duffy, K. J. Optimization convolutional neural network for automatic skin lesion diagnosis using a genetic algorithm. Appl. Sci. 13(5), 3248 (2023).
Tabrizchi, H., Parvizpour, S. & Razmara, J. An improved VGG model for skin cancer detection. Neural Process. Lett. 55(4), 3715–3732 (2023).
Balaha, H. M. & Hassan, A.E.-S. Skin cancer diagnosis based on deep transfer learning and sparrow search algorithm. Neural Comput. Appl. 35(1), 815–853 (2023).
Anupama, C. S. S. et al. Sand cat swarm optimization with deep transfer learning for skin cancer classification. Comput. Syst. Sci. Eng. 47, 2 (2023).
Shamsi, A. et al. A novel uncertainty-aware deep learning technique with an application on skin cancer diagnosis. Neural Comput. Appl. 35(30), 22179–22188 (2023).
Adla, D. et al. A full-resolution convolutional network with a dynamic graph cut algorithm for skin cancer classification and detection. Healthcare Analytics 3, 100154 (2023).
Rajeshwari, J. & Sughasiny, M. Skin cancer severity prediction model based on modified deep neural network with horse herd optimization. Optic. Memory Neural Netw. 31(2), 206–222 (2022).
Shinde, R. K. et al. Squeeze-mnet: Precise skin cancer detection model for low computing IOT devices using transfer learning. Cancers 15(1), 12 (2022).
Prasad, V., Emil Selvan, G. S. R. & Ramkumar, M. P. ADTBO: Aquila driving training-based optimization with deep learning for skin cancer detection. Imag. Sci. J. 4, 1–19 (2023).
Mohakud, R. & Dash, R. Skin cancer image segmentation utilizing a novel EN-GWO based hyper-parameter optimized FCEDN. J. King Saud Univ. Comput. Inf. Sci. 34(10), 9889–9904 (2022).
Shetty, B. et al. Skin lesion classification of dermoscopic images using machine learning and convolutional neural network. Sci. Rep. 12(1), 18134 (2022).
Barburiceanu, S., & R. Terebeș. Automatic detection of melanoma by deep learning models-based feature extraction and fine-tuning strategy. In IOP Conference Series: Materials Science and Engineering, Vol. 1254, 012035 (IOP Publishing, 2022).
Houssein, E. H., Emam, M. M. & Ali, A. A. An optimized deep learning architecture for breast cancer diagnosis based on improved marine predators algorithm. Neural Comput. Appl. 34(20), 18015–18033 (2022).
Gouda, W., Sama, N. U., Al-Waakid, G., Humayun, M. & Jhanjhi, N. Z. Detection of skin cancer based on skin lesion images using deep learning. Healthcare 10(7), 1183 (2022).
El Gannour, O. et al. Improving skin diseases prediction through data balancing via classes weighting and transfer learning. Bull. Electr. Eng. Inf. 13(1), 628–637 (2024).
Arunkumar, M., Mohanarathinam, A. & Subramaniam, K. Detection of varicose vein disease using optimized kernel Boosted ResNet-Dropped long Short term Memory. Biomed. Signal Process. Control 87, 105432 (2024).
Zhang, L. et al. A deep learning outline aimed at prompt skin cancer detection utilizing gated recurrent unit networks and improved orca predation algorithm. Biomed. Signal Process. Control 90, 105858 (2024).
Sonia, R. et al. Segmenting and classifying skin lesions using a fruit fly optimization algorithm with a machine learning framework. Automatika 65(1), 217–231 (2024).
Deshmukh, A. A. et al. Multi-class skin diseases classification using hybrid deep convolutional neural network. Int. J. Intell. Syst. Appl. Eng. 11(10s), 11–22 (2023).
Sulthana, R., Chamola, V., Hussain, A., Hussain, Z. & Albalwy, F. A novel end-to-end deep convolutional neural network based skin lesion classification framework. Expert Syst. Appl. 246, 123056 (2023).
Bibi, S. et al. MSRNet: Multi-class skin lesion recognition using additional residual block based fine-tuned deep models information fusion and best feature selection. Diagnostics 13(19), 3063 (2023).
Awotunde, J. B. et al. An enhanced hyper-parameter optimization of a convolutional neural network model for leukemia cancer diagnosis in a smart healthcare system. Sensors 22(24), 9689 (2022).
Abdar, M. et al. Uncertainty quantification in skin cancer classification using three-way decision-based Bayesian deep learning. Comput. Biol. Med. 135, 104418 (2021).
Kilicarslan, S., Celik, M. & Sahin, Ş. Hybrid models based on genetic algorithm and deep learning algorithms for nutritional Anemia disease classification. Biomed. Signal Process. Control 63, 102231 (2021).
Sayed, G. I., Soliman, M. M. & Hassanien, A. E. A novel melanoma prediction model for imbalanced data using optimized SqueezeNet by bald eagle search optimization. Comput. Boil. Med. 136, 104712 (2021).
Tan, T. Y., Zhang, L. & Lim, C. P. Intelligent skin cancer diagnosis using improved particle swarm optimization and deep learning models. Appl. Soft Comput. 84, 105725 (2019).
ElGhany, S. A., Ibraheem, M. R., Alruwaili, M. & Elmogy, M. Diagnosis of various skin cancer lesions based on fine-tuned ResNet50 deep network. Comput. Mater. Cont. 68, 1 (2021).
Pham, T. C., et al. Improving binary skin cancer classification based on best model selection method combined with optimizing full connected layers of Deep CNN. In 2020 International conference on multimedia analysis and pattern recognition (MAPR), 1–6. (IEEE, 2020).
Gouda, W., Sama, N. U., Al-Waakid, G., Humayun, M. & Jhanjhi, N. Z. Detection of skin cancer based on skin lesion images using deep learning.". Healthcare 10(7), 1183 (2022).
Nour, A., & Boubakeur, B. Convolutional neural network strategy for skin cancer lesions classifications and detections. In Proceedings of the 11th ACM International Conference on Bioinformatics, Computational Biology and Health Informatics, 1–9 (2020).
Tan, T. Y., Zhang, L., Neoh, S. C. & Lim, C. P. Intelligent skin cancer detection using enhanced particle swarm optimization. Knowl. Syst. 158, 118–135 (2018).
Khan, M. A., Akram, T., Zhang, Y. D., Alhaisoni, M., Al Hejaili, A., Shaban, K. A., & Zayyan, M. H. SkinNet‐ENDO: Multi-class skin lesion recognition using deep neural network and Entropy‐Normal distribution optimization algorithm with ELM. Int. J. Imaging Syst. Technol. (2023).
Ajmal, M. et al. BF2SkNet: Best deep learning features fusion-assisted framework for multi-class skin lesion classification. Neural Comput. Appl. 35(30), 22115–22131 (2023).
Dillshad, V., Khan, M. A., Nazir, M., Saidani, O., Alturki, N., & Kadry, S. D2LFS2Net: Multi‐class skin lesion diagnosis using deep learning and variance‐controlled Marine Predator optimization: An application for precision medicine. CAAI Trans. Intell. Technol. (2023).
Hussain, M. et al. SkinNet-INIO: Multi-class skin lesion localization and classification using fusion-assisted deep neural networks and improved nature-inspired optimization algorithm. Diagnostics 13(18), 2869 (2023).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ideas and overarching research goals and aims by S.S. and A.B.; Methodology: Development and design of methodology by U.K.L. and V.V.R.M.R.; Software: Programming, software development by Y.K.S. and A.B.; Investigation and analysis: Conducting a research and investigation process and result analysis by; K.S.K.R. and K.B.V.B.R.; Supervision: Guidance and supervision for the research by U.K.L. Authors provide support for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kumar Lilhore, U., Simaiya, S., Sharma, Y.K. et al. A precise model for skin cancer diagnosis using hybrid U-Net and improved MobileNet-V3 with hyperparameters optimization. Sci Rep 14, 4299 (2024). https://doi.org/10.1038/s41598-024-54212-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54212-8
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.