Abstract
Type 2 diabetes interferes with bone remodeling mechanisms, requiring studies to reverse this damage, and resveratrol is a polyphenol with rich properties. This study aimed to characterize the long bone morphology and peri-implant biomechanics of normoglycemic and type 2 diabetic animals treated with resveratrol. Thirty-two male Wistar rats were used and divided into normoglycemic and diabetic with or without treatment. They had the installation of implants in the tibia and treatment with oral resveratrol within 45 days. Resveratrol was responsible for weight homeostasis and decreased glycemic levels in rats with type 2 diabetes. The three-point bending testing, resveratrol showed positive effects on the biomechanics of long bones, corroborating a more resistant bone in comparison to untreated diabetics. Micro-ct revealed how bone metabolism is affected by systemic disease, decreasing bone quality. The counter-torque of normoglycemic animals showed superior osseointegration to diabetes, with no differences in the administration of the polyphenol, showing the sovereignty of the deleterious effects of the disease when there is a tissue lesion and an inflammatory picture installed. Overall, resveratrol acted positively in the etiopathogenesis of type 2 diabetes and revealed positive effects on the strength of long bones.
Similar content being viewed by others
Introduction
In an increasingly obese population, with poor eating habits, resulting in an unhealthy lifestyle, type 2 diabetes becomes a major global public health problem, with 463 million people with diabetes, where 50.1% of adults are undiagnosed and type 2 is responsible for 90–95% of patients1. This is characterized by insulin resistance. As there is no proper functioning, glucose levels continue to rise and release more insulin, insufficient to restore normal levels and generate hyperglycemia2. It acts multi-systemically and with great comorbidity, promoting cardiovascular, retinal, renal, and neurological complications3, and also acting on bone health, which according to the Brazilian Society of Diabetics is not infrequently neglected4.
Individuals with type 2 diabetes have lower bone quality and bone strength, being at a higher risk of bone fractures, where high blood glucose levels damage the mineral matrix, through altered cellular function and bone remodeling and an accumulation of advanced glycation end products (AGEs)5, The pathological effect of AGEs is related to their ability to modify physical and chemical properties of various structures6,7, causing deterioration of collagen and changes in bone microstructure8,9. In the literature, besides type 2 diabetes being associated with an increased risk of fractures, there is also an influence on oral health. The oral cavity is compromised through the increase of infections, bone loss, and periodontal disease, promoting a delay in remodeling and alveolar bone repair10,11, and especially tooth loss12. According to the World Health Organization, type 2 diabetes is late diagnosed due to its silent symptoms, and is often discovered in middle age, where, in dentistry, there is a higher prevalence of implant installation. Understanding the structural characteristics and reversing the pathophysiological changes of bone is of great importance to increase the success of rehabilitative treatment, since diabetes leads to a greater loss of implants when compared to normoglycemic patients13.
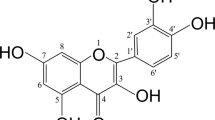
Due to this condition, studies have been searching for alternative therapies, such as herbal medicines, which lead to favorable results without side effects. Resveratrol is a polyphenol (3,5,4ʹ-trihydroxy-trans-stilbene), typically found in the skin of purple grapes, wines, and other plants14. It has anti-inflammatory, antioxidant, cardioprotective, and antidiabetic properties15. It has been a widely accepted choice for the treatment of type 2 diabetes by preventing glucose intolerance, significantly decreasing body weight, and body mass index in obese people, and increasing lean body mass16. Studies have demonstrated the beneficial effect of resveratrol on bone tissue, preventing bone loss, acting on structures, volume, and bone microarchitecture15, and also showing effects on post-surgical repair14,15,16,17. Thus, the aim was to characterize the long bones from the morphological and functional point of view, and the peri-implant biomechanics of normoglycemic and type 2 diabetic animals, treated or not with resveratrol.
Methods
This study was approved by the Ethics Committee on the Use of Animals (CEUA) of São Paulo State University (UNESP), School of Dentistry, Araçatuba, Brazil (#00153-2019, approved in February 15th, 2019), following the Animal Research: Reporting of In Vivo Experiments (ARRIVE) guidelines, and following the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (Institute of Laboratory Animal Resources [U.S.])18.
Animals
Thirty-two male rats (Rattus norvegicus albinus, Wistar), weighing an average of 395 g and aged 3 months, were divided into four groups (n = 8 per group): Normoglycemic (NG); Normoglycemic + resveratrol (NGrvt); Type 2 diabetes (T2D); and Type 2 diabetes + resveratrol (T2Drvt). The animals were kept in cages in a stable temperature environment (22 °C ± 2 °C, light control cycle 12 h light, 12 h dark) and a balanced diet (NUVILAB, 1.4% Ca and 0.8% P + water with libitum) based on previous results already published10: the averages used for the calculation were 3.06 and 4.898 and the standard deviations were 0.26 and 0.024, with a significance level of 5% and a power of 95% in a one-tailed hypothesis test. The animals were identified by numbers and randomly separated by Microsoft Office Excel software (Microsoft, Redmond, WA, USA), respecting a 1:1 allocation rate for each group. The data obtained from the proposed analyses were submitted to statistical analysis by the software GraphPad Prism 7.01 (GraphPad Software, La Jolla, USA).
Type 2 diabetes induction
The combination of the cafeteria diet associated with low-dose streptozotocin (STZ) application was used only in T2D and T2Drvt groups. The cafeteria diet followed the model of Gomez-Smith19 and Carillon20, mimicking a poor diet that promotes insulin resistance and obesity in rats, which are predisposing factors for type 2 diabetes20. The cafeteria diet started on day 0 and each animal received 30 g of this diet, consisting of 10 g of stuffed crackers, 10 g of wafer crackers, 10 g of corn snacks, and a bottle of sugar water with a concentration of 12% sucrose (50 mL daily) (Table 1). After 3 weeks of the cafeteria diet, drug induction of type 2 diabetes occurred through the Srinivasan model21, where animals of T2D and T2Drvt groups, were anesthetized by intramuscular infiltration of 5 mg/kg xylazine hydrochloride (Dopaser ®—Laboratórios Calier do Brazil Ltd.a., Osasco, Brazil) and 50 mg/kg ketamine hydrochloride (Vetaset®—Fort Dodge Animal Health Ltd.a., Campinas, Brazil), antisepsis of the scrotal region was done with 70% alcohol and a low dose of streptozotocin (STZ—Sigma©, Merck KGaA, Darmstadt, Germany and/or its affiliates) was injected into the penile vein (35 mg/kg), dissolved in a vehicle (0.1 M sodium citrate solution, pH = 4.5) and the NG and NGrvt animals received only the vehicle. The low dose STZ used in this study causes partial destruction of beta cells and accelerates the development of the type 2 diabetes condition10,19. In specific and strategic data, the animals were weighed on a conventional scale and their glycemic levels were measured. Periods: the beginning of the diet (day 0), STZ application (day 21), the type 2 diabetes confirmation and the start of resveratrol treatment (day 28), implant surgery (day 43), and euthanasia (day 73). To perform the glycemic evaluation, the animals were fasted for 2 h after consuming the oral solution containing glucose (2 g glucose), and, using a n°11 scalpel blade a blood sample was taken from the caudal vein through a small perforation. The blood sample should be a compatible drop for reading the glucose meter22. Type 2 diabetes was determined with concentrations greater than 198 mg/dL after 2 h of oral glucose administration22,23. This study model showed that a cafeteria diet and a low dose of STZ are effective in generating an animal model that reproduces a common type of natural and metabolic history of diabetes 2 in humans19 (Fig. 1).
Resveratrol treatment
After confirmation of type 2 diabetes (day 28) in animals of T2D and T2Drvt groups, the systemic treatment with resveratrol (Aphoticário Pharmacy of Manipulation Ltda, Araçatuba, São Paulo, Brazil) was started in animals of NGrvt and T2Drvt groups until the end of the experiment, totaling 45 days of treatment. It was administered orally, by gavage technique, at a concentration of 100 mg/kg/day dissolved in Dimethyl Sulfoxide (DMSO)23 and the animals in NG and T2D groups, to undergo the same stress, received only the vehicle.
Implant surgery
The surgery to install implants (day 43) was performed fifteen days after the beginning of resveratrol treatment, the animals were forced to fast for 8 h where animals of all and then sedated, as described previously. The medial portion of the left tibia was trichotomized and the region to be incised was treated with antiseptic. With a number 15 blade, an incision was made in the region of the left tibial metaphysis, and then the soft tissue was divulsion in its total thickness and detached, exposing the bone to receive the implants.
Each animal received 1 implant (Medens, São Paulo, Brazil), in the region of the left tibial metaphysis, with a total of 32 titanium implants with double acid etched, 2.0 mm in diameter, and 4.0 mm in height, sterilized by gamma rays. For this purpose, the milling will be performed with a 1.6 mm diameter spiral cutter mounted on an electric motor (BLM 600®; Driller, São Paulo, SP, Brazil), at a speed of 1000 rpm, under irrigation with isotonic 0.9% sodium chloride solution (Fisiológico®, Laboratórios Biosintética Ltda®, Ribeirão Preto, SP, Brazil), and counter-angle (Angular Part 3624N 1:4, Head 67RIC 1:4, KaVo®, Kaltenbach & Voigt GmbH & Co, Biberach, Germany), with a 16:1 reduction and a depth of 3.0 mm, with initial blocking and stability. The tissues were sutured in planes with absorbable thread with continuous stitches in the deep plane and with monofilament thread with interrupted stitches in the outermost plane. In the immediate postoperative period, each animal received a single intramuscular dose of 0.2 ml of veterinary antibiotic (Pentabiotic Small Veterinary, Fort Dodge Saúde Animal Ltda., Campinas, São Paulo, Brazil) and analgesia with Dipyrone Sodium (1 mg/kg/day, (1 mg/kg/day, Ariston Indústrias Químicas e Farmacêuticas Ltda, São Paulo, Brazil)24.
Sample processing
Animals were euthanized by an anesthetic overdose of xylazine hydrochloride and ketamine hydrochloride 30 days after implant installation, with the tibia still in vivo, and counter-torque analysis was performed. The femurs were collected and fixed in formaldehyde 10% for 48 h, then washed in running water for 24 h and immersed in alcohol at 70° at room temperature, to be scanned for computed microtomography analysis. The femurs used for Three-points bending testing were removed, washed in saline to remove blood and immediately, conserved in saline at the refrigerator. Only on the day of the biomechanical tests were the specimens thawed.
Biomechanical analysis of counter-torque
The animals were euthanized by anesthetic overdosage of xylazine hydrochloride (Dopaser®—Laboratórios Calier do Brazil Ltda., Osasco, Brazil) and ketamine hydrochloride (Vetaset®—Fort Dodge Animal Health Ltd.a., Campinas, Brazil) 30 days after the implant installation. The tibia was accessed to expose the implants and a digital torque meter (Homis, São Paulo, SP, Brazil) coupled with a 1.2 mm hexagonal digital key was used (Medens, São Paulo, SP, Brazil). A counterclockwise motion was applied until rotation of the implant within the bone tissue and complete rupture of the bone/implant interface. The maximum value for rupture was recorded on the torque meter (N.cm) and noted25.
Three-points bending testing
Biomechanical tests provide some properties of bone tissue26, given when stimulus are applied to bone and the intensity of this stimulus necessary to break the bone as well as the behavior of the bone when is broken are evaluated. All of these parameters are measured through: Maximum force (N) that corresponds to the greatest force to completely break the femoral bone, obtained in the region of the femoral shaft. Rupture force (N) corresponds to the force required to break the bone marrow area of the femurs. The deformation at maximum force (mm) corresponds to how much the bone deforms during the application of the maximum force and, finally, the deformation at rupture (mm), which corresponds to the deformation of the bone at the moment of rupture. The test was performed on the EMIC/Mod DL3000 Universal Testing Machine, in which femur specimens, one at a time, were positioned horizontally on a two-support platform in the machine, with a distance between supports of 20 mm, with the femur head facing the left side and the patellar surface facing the right. The load application tip (200 kg load cell with a capacity of 2000 N)27 was positioned in the center of the femur and a vertical compression force was applied in the anteroposterior direction with a load application speed (force) of 0.25 mm/min until the moment of bone rupture. The values were recorded in the manufacturer's computer systems, which directly provided the maximum force values admitted by the femur. In the analysis, the bone resistance was evaluated using the force x displacement curve, analyzing the maximum force (N) admitted by the bone tissue and the stiffness (x103N/m)28.
Computed microtomography analysis (micro-ct)
For micro-ct analysis, the samples were scanned and in the Data Viewer software (SkyScan, Version 1.4.4 64-bit) the images were reconstructed to fit the standard positioning for all samples and can be observed in three planes (transverse, longitudinal, and sagittal). Then, using CTAnalyser—CTAn software (2003-11SkyScan, 2012 Bruker MicroCT Version 1.12.4.0), two regions of interest (ROI) were standardized in the distal portion of the femur for trabecular bone (Upper boundary: 150 slices below the growth plate; Lower boundary: 100 slices from the upper boundary (900 µm). The volumes of interest (VOI) were automatically delimited, using the analysis software, for the trabecular bone (Boundaries of the inner border of the medullary cortex). In the trabecular portion, bone volume percentage (Tb. BV/TV), structure model index (Tb. SMI), trabecular number (Tb. N), trabecular thickness (Tb. Th), and trabecular separation (Tb. Sp) were analyzed. In the cortical portion, the volume of closed pores Po.V(cl), the volume of open pores Po.V(op), and the percentage of cortical porosity Po(tot) were evaluated26.
Statistical analysis
GraphPad Prism 7.03 (GraphPad Software, La Jolla, USA) was used for statistical analysis. The homoscedasticity was assessed via the Shapiro–Wilk test to distinguish the parametric. Homocedasticity was assessed via the Shapiro–Wilk test, confirming the normal distribution of the data ANOVA one-way test was chosen to determine if there were differences among the groups. Holm Sidak post-test was performed to indicate the differences in the direct comparisons of the groups. A significance level of 5% was considered for all tests.
Results
Body weight and glycemic level
With the results of the average body weight, the NG and NGrvt groups had a gradual increase in weight, as expected, during the periods of the experiment. In addition, the NGrvt group maintained a lower weight gain at the time of euthanasia when compared to the NG group, while in the T2D group, there was an increase in body weight after 3 weeks of administration of the cafeteria diet. In addition, there was a greater variation in weight during the periods when compared to the T2Drvt group, which maintained a homeostasis in body weight, with no statistical difference between the periods (Table 2).
Concerning the mean blood glucose results, the NG and NGrvt groups had hyperglycemia results, since the results were below 198 mg/dL. There was less control of blood glucose in the NGrvt group, as there was no statistical difference from the beginning to the end of the experiment. Even without a statistical difference, both diabetic groups had an increase in blood glucose 3 weeks after starting the cafeteria diet. One week after the induction of type 2 diabetes, the T2D and T2Drvt groups had a statistically significant increase in glucose levels, with values above 198 mg/dL, proving the establishment of the disease. The T2D group maintained high glycemic values with no statistical difference from the moment of induction to the moment of euthanasia. However, the T2Drvt group showed a gradual and statistically significant decrease in blood glucose after 1 week of treatment until the time of euthanasia (Table 3).
Three-points bending testing
For the mechanical test parameters, results were obtained for maximum force; deformation at maximum force; rupture force, and deformation at rupture. For maximum force, there was a statistically significant difference between the NG vs. NGrvt group (p = 0.0202). The NGrvt group (137.2 N) required greater maximum force, in other words, greater force to completely break the femoral bone in the diaphysis region when compared to the NG group (115.4 N). In addition, the T2Drvt group (141.7 N) required more maximum force than the NG group, with a statistically significant difference (p = 0.0057). As for the maximum force deformation results, the comparison between the groups was statistically significant when comparing the T2D group (1.356 mm) vs. the T2Drvt group (1.108 mm) (p = 0.076). This showed that the femurs in the T2D group deformed more during the application of the maximum force compared to the T2Drvt group.
In the rupture force results, there was a statistically significant difference between the NG group (113.3 N) vs. T2Drvt (139.5 N) (p = 0.0284), between the NGrvt group (99.96 N) vs. T2Drvt (p = 0.0010) and T2D group vs. T2Drvt (p = 0.0200). The results showed that the T2Drvt group required more force to break the femoral marrow when compared to the other groups. Finally, concerning deformation at rupture, there was a statistically significant difference between groups NG (1.66 mm) vs. T2Drvt (10.53 mm) (p = 0.0127) and T2D (1.575 mm) vs. T2Drvt (1.053 mm) (p = 0.0199). This shows that the femurs of the NG and T2D groups deformed more at the moment of rupture when compared to the T2Drvt group (Fig. 2).
Graphs showing Three-points testing. Maximum force: The NGrvt group demanded more force to break the bone compared to the NG group, with a statistically significant difference between the group. The T2Drvt group demanded more force compared to the NG group, with a statistically significant difference between the groups. Deformation at maximum force: The T2D group deformed more compared to the T2Drvt group, with a statistically significant difference between the group. Rupture force: the T2Drvt group demanded more force to rupture the medullary when compared to all other groups, with a statistically significant difference between the group. Deformation at rupture: NG and T2D deformed more compared to T2Drvt. Symbols: Eros bar; letters indicate a statistical difference between the periods (p < 0.05).
Computed microtomography analysis (micro-ct)
The results of the micro-ct, where the trabecular portion of the femur was assessed. For the bone volume percentage parameter (Tb. BV/TV), the NG group had a higher bone volume percentage (BV/TV = 45.24%) compared to the T2Drvt group (BV/TV = 36.72%) (p = 0.0468). For the structure model index parameter (Tb. SMI), the T2Drvt group (Tb. SMI = 1.098) had a higher number of rods and plates in the trabecular bone when compared to the NG group (Tb. SMI = 0.5027) (p = 0.0156) and also higher when compared to the T2D group (Tb. SMI = 0.5533) (p = 0.0249). For the number of trabeculae (Tb. N) there was a statistically significant difference among all the groups. The NG group (Tb. N = 3.969 1/mm) only had a higher number of trabeculae when compared to the T2Drvt group (3.592 1/mm) (p = 0.0017). In the other groups, NG had a lower number of trabeculae compared to NGrvt (Tb. N = 4.457 1/mm) (p = 0.0002) and T2D (Tb. N = 4.194 1/mm) (p = 0.485). The presence of resveratrol caused a decrease in the number of trabeculae in the T2Drvt group when compared to the NG (p = 0.0017), NGrvt (p = < 0.0001) and T2D (p = < 0.001) groups. For trabecular thickness (Tb. Th), there was no statistically significant difference for this parameter (p = 0.6277). For trabecular separation (Tb. Sp), the NGrvt group (Tb. Sp = 0.1471 mm) had greater separation of the trabeculae when compared to the T2Drvt group (Tb. Sp = 0.2074 mm) (p = 0.0077) (Fig. 3).
Showing Micro-CT results. BV/TV: NG group showed a higher percentage of bone volume compared to the T2Drvt group, with a statistically significant difference between the groups. Tb. SMI: T2Drvt group showed a better result compared to the NG group and T2D, with statistically significant differences between the groups. Tb. N: NGrvt group showed a higher result compared to the NG, with a statistically significant difference between the groups, and the T2Drvt group had a lower result compared to T2D, with a statistically significant difference between the groups. Tb. Th: there was no statistically significant difference between the groups. Tb. Sp: The T2Drvt group showed better results compared to the NGrvt, with statistically significant differences between the groups. Symbols: Eros bar; letters indicate a statistical difference between the periods (p < 0.05).
The results of the micro-ct, in which the cortical portion of the femur was evaluated. There was no statistical difference in the volume of closed pores (Po.V(cl)) between the groups. Concerning the volume of open pores, the T2D group (Po.V(op) = 0.799 mm3) had a greater volume of open pores in the cortical bone when compared to the NG group (Po.V(op) = 0.2246 mm3) (p = 0.0087). For the percentage of cortical porosity, the results were lower for the NG group when compared to all the other groups. The NG group obtained lower values (Po (tot) = 2.025%) for the percentage of cortical porosity when compared to the NGrvt (Po (tot) = 5.086%) (p = 0.0143), T2D (Po (tot) = 6.431%) (p = 0.0016) and T2Drvt (Po (tot) = 4.558%) (p = 0.376) groups (Fig. 4).
Showing Micro-CT cortical results. Po.V(cl): There was no statistical difference between the groups. Po.V(op): The T2D group showed a greater result when compared to the NG group. Po(tot): The NG group showed statistically lower results when compared to all the other groups. Symbols: Eros bar; letters indicate statistical difference between periods (p < 0.05).
Biomechanical analysis of counter-toque
For the biomechanical parameters of counter-torque analysis, there was only a statistical difference between the normoglycemic and type 2 diabetic groups, regardless of the administration of resveratrol. The NG group (7.54 N/cm) showed a higher counter-torque value than the T2D (4.45 N/cm) (p = 0.0151) and T2Drvt (2.252 N/cm) groups (p = 0.0003). The NGrvt group (7.5 N/cm) showed a higher counter-torque value when compared to the T2D (p = 0.0164) and T2Drvt (0.0004) groups. As for the diabetic groups, there was also no statistical difference between them (p = 0.1582) (Fig. 5).
Discussion
In addition to being involved in the etiopathogenesis of type 2 diabetes, obesity also has a pathophysiological impact29, being one of the main risk factors, along with the presence of foods rich in sugar, fat, and sodium30, the latter mimicked in this study by the cafeteria diet. Resveratrol, the phytochemical used in this study, has been widely studied31, as it is a great candidate for adjuvant therapy of type 2 diabetes32,33,34,35. Studies have shown that resveratrol has a positive effect on lipid homeostasis and the reduction of fat mass36, which can be partially explained by both the activation of lipolysis through adipose triglyceride lipase and the inhibition of lipogenesis37,38,39,40. This action on lipid hemostasis was observed in this study, as the NGrvt group maintained a lower weight gain when comparing the first to the last day of the experiment compared to the NG group. On the other hand, in the diabetic groups that received the cafeteria diet, T2D showed the greatest statistical variation in body weight during the experimental period. There was a significant increase in weight after starting the cafeteria diet and a slight reduction in weight after the injection of streptozotocin, which may be related to the application of the drug, as well as to acute hyperglycemia22. Unlike the T2Drvt group, which received treatment with resveratrol, which showed weight homeostasis, represented by no statistical difference between the dates. This shows the effect of resveratrol on weight stability, energy expenditure, and reduction of adiposity41.
Concerning glycemic levels, both normoglycemic groups showed the expected normal values, below 100 mg/dl. On the other hand, in the diabetic groups, only the cafeteria diet, although with no statistical difference, was able to raise glucose levels. This shows that a nutrient-poor diet is a risk factor because it increases glycemic patterns10,30. After the induction of type 2 diabetes, there was a significant increase in blood glucose in the T2D and T2Drvt animals, with values higher than 198 mg/dL, proving the onset of the disease and demonstrating the efficacy of streptozotocin in this animal model of type 2 diabetes. In this study, in addition to observing the beneficial action of the systemic administration of resveratrol on weight, there was an action mainly on glycemic patterns. The resveratrol, from the start of its administration in the T2Drvt group, was responsible for drastically and statistically reducing glycemic levels until the end of the experiment. Unlike the T2D group, which maintained high blood glucose levels after induction until euthanasia. These results corroborate studies that show improved insulin sensitivity in type 2 diabetic rats when resveratrol is administered42,43,44, through the potent activation of Sirt1, increasing insulin sensitivity and protecting against metabolic damage. Studies in the literature show that activation of AMP-activated protein kinase (AMPK) is used to mediate some of the effects of resveratrol in regulating insulin sensitivity and insulin secretion in pancreatic β-cells and in increasing glucose uptake45.
The flexion analysis showed the beneficial effects of resveratrol in the normoglycemic group and also in the diabetic animals. In the NGrvt group, resveratrol contributed to increased stiffness, which required greater force to completely break the bone when compared to the untreated normoglycemic group. In the T2Drvt group, greater force was required to break the entire medullary femurs when compared to all the other groups. This may be explained by the additional beneficial effects of resveratrol and the greater bone density in type 2 diabetics46. These results corroborate studies showing that resveratrol, even under hyperglycemic conditions, is capable of modulating osteogenic and osteoclastogenic mechanisms in the bone remodeling process during healing, as well as preventing the loss of bone density47. It can also be seen that resveratrol reduces bone deformation in the T2Drvt group, both in terms of deformation at maximum force and deformation at break. This shows that the bone in the T2Drvt group has a stiffness improvement, requiring an increasing strength to break the femur. Results express the promising effects of resveratrol in improving the mechanical properties of bone48 and its protective effects that seem to be mediated by the increased bone formation of osteoblasts, possibly due to reduced inflammation49.
In the micro-ct analysis, in the medullary portion, the T2Drvt group showed a lower number of trabeculae, with greater separation between them. However, this data did not influence trabecular thickness, possibly because it had a higher structure model index, which means a higher relative prevalence of plates and rods. As there is a greater separation of these trabeculae, it is to be expected that the bone volume would be smaller in T2Drvt, as it is a more porous bone. As for the cortical portion, type 2 diabetes negatively affected the cortical structure of the bone, with a greater volume of open pores and a higher percentage of cortical porosity when compared to the normoglycemic group. These results are already known in the literature, where the most consistent alteration of diabetes is the increase in cortical bone porosity50. This damage is attributed to the morphology and function of osteocytes, which are known to act as organizers of bone metabolism51. About the DM2 groups, resveratrol was not statistically capable of improving cortical quality. However, these structural changes did not have a sufficient influence on the biomechanics of the femur. In the three-point bending test, there was no loss of strength in the presence of type 2 diabetes.
The biomechanical analysis using the three-point bending test and micro-ct showed that the presence of type 2 diabetes could not cause significant changes in the biomechanics and microstructure of the long bones. The increased risk of fracture in long bones is more evident in the case of type 1 diabetes, as they have reduced bone mass52. This factor is not found in type 2 diabetes, where patients have greater bone density. This is due to the anabolic effect of hyperinsulinemia, which favors osteoblastic activity, leading to increased bone density46. In addition, studies report that a higher incidence of fracture in type 2 diabetic patients is related to chronic complications, which are responsible for causing greater functional limitation52, as well as the use of some medications that can reduce bone density53.
The results show the superiority of the normoglycemic groups in the osseointegration of the bone/implant interface in the tibia compared to the diabetic groups, demonstrating the relevance of the systemic interference of type 2 diabetes in bone metabolism when there is tissue injury. In normal repair, tissues progress through discrete phases, including hemostasis, inflammation, proliferation, and remodeling, but in diabetes, progression through these phases is impaired, resulting in a sustained inflammatory state and dysfunctional epithelialization in the wound54. There are also alterations in microvascularization which decrease the immune response, reduce bone remodeling, and compromise the vascularization of the flap, delaying healing and providing a gateway for infections55. Although some studies have highlighted the benefits of using resveratrol as a therapeutic agent to improve peri-implant bone healing in the presence of diabetes mellitus56, the administration of resveratrol made no statistical difference in this study.
The results in long bones revealed promising effects of resveratrol in improving bone microstructure and mechanical properties, being able to improve strength and resistance parameters in femurs. Scientific evidence shows that type 2 diabetes is detrimental to the bone metabolism of long bones, however in this study, little evidence was obtained. It was possible to observe that type 2 diabetes is more harmful when there is tissue damage, such as in the presence of implants. Peri-implant osseointegration in type 2 diabetic animals was worse when compared to control groups. This is a problem that arises in dental practices when surgical procedures such as implant installation are required, as osseointegration may be impaired. The systemic administration of resveratrol was unable to reverse the peri-implant results. However, it is very effective in etiopathogenesis, acting on weight homeostasis and especially in reducing glycemic levels in diabetic rats. Therefore, new studies will be carried out to evaluate resveratrol locally, by functionalizing implants with resveratrol.
Conclusion
Resveratrol acted positively in type 2 diabetes, reducing hyperglycemia and acting on weight homeostasis. Resveratrol in the long bones of type 2 diabetics showed positive biomechanical effects on strength and endurance parameters. However, resveratrol was unable to improve the microstructure of diabetic long bones and its systemic administration did not bring positive results in the quality of osseointegration at the bone-implant interface, when tissue damage and the inflammatory process were already present. Revealing that resveratrol supplementation can be used in conjunction with dietary therapy and in a preventive manner. And exposing the need for further work to detect its local effects on the implant surface.
Data availability
The datasets generated and/or analyzed are available from the corresponding author upon reasonable request.
References
Saeedi, P. et al. IDF Diabetes atlas committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 157, 107843. https://doi.org/10.1016/j.diabres.2019.107843 (2019).
Diabetes Mellitus fact sheet. World health organization. http://www.who.int/health-topics/diabetes (2002).
Silva, A. G. & Lazaretti-Castro, M. Diabetes mellitus, thiazolidinediones, and fractures: An unfinished story. Arq. Bras. Endocrinol. Metabol. 54, 345–351 (2010).
Sever, M. D. Bone disease in diabetes mellitus. Brazilian diabetes society. https://diabetes.org.br/diabetes-mellitus-e-saude-ossea/ (2021).
Hernandez, C. J. et al. Trabecular microfracture and the influence of pyridinium and non-enzymatic glycation-mediated collagen cross-links. Bone. 37, 825–832 (2005).
Liao, C. C. et al. Increased risk of fracture and postfracture adverse events in patients with diabetes: two nationwide population-based retrospective cohort studies. Diabetes Care 37, 2246–2252 (2014).
Jackuliak, P. & Payer, J. Osteoporosis, fractures, and diabetes. Int. J. Endocrinol. 2014, 820615. https://doi.org/10.1155/2014/820615 (2014).
Rubin, M. R. Bone cells and bone turnover in diabetes mellitus. Curr. Osteoporosis Rep. 13, 186–191 (2015).
Carnevale, V., Romagnoli, E., D’Erasmo, L. & D’Erasmo, E. Bone damage in type 2 diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 24, 1151–1157 (2014).
Pitol-Palin, L. et al. Different stages of alveolar bone repair process are compromised in the type 2 diabetes condition: An experimental study in rats. Biology. 9, 471 (2020).
Lecka-Czernik, B. Diabetes, bone, and glucose-lowering agents: Basic biology. Diabetologia. 60, 1163–1169 (2017).
Genco, R. J. et al. Effects of periodontal disease on glycemic control, complications, and incidence of diabetes mellitus. Periodontology. 83, 59–65 (2020).
Serrão, C. R. et al. Role of metformin in reversing the negative impact of hyperglycemia on bone healing around implants inserted in type 2 diabetic rats. Int. J. Oral Maxillofac. Implants 32, 547–554 (2017).
Miotto, P. M. et al. Combined high-fat-resveratrol diet and RIP140 knockout mice reveal a novel relationship between elevated bone mitochondrial content and compromised bone microarchitecture, bone mineral mass, and bone strength in the tibia. Mol. Nutr. Food Res. 60, 1994–2007 (2016).
Bo, S. et al. Effects of resveratrol on bone health in type 2 diabetic patients. A double-blind randomized controlled trial. Nutr. Diabetes 8, 51 (2018).
Tabrizi, R. et al. The effects of resveratrol intake on weight loss: A systematic review and meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 13, 1–16 (2018).
Caldarelli, I. A. et al. Resveratrol mimics insulin activity in the adipogenic commitment of human bone marrow mesenchymal stromal cells. Int. J. Biochem. Cell Biol. 60, 60–72 (2015).
Percie du Sert, N. et al. The arrive guidelines 2.0: Updated guidelines for reporting animal research. PLoS Biol. 14, e3000410. https://doi.org/10.1371/journal.pbio.3000410 (2020).
Gomez-Smith, M. et al. A physiological characterization of the cafeteria diet model of metabolic syndrome in the rat. Physiol. Behav. 167, 382–391 (2016).
Carillon, J. et al. Cafeteria diet induces obesity and insulin resistance associated with oxidative stress but not with inflammation: Improvement by dietary supplementation with a melon superoxide dismutase. Free Radic. Biol. Med. 65, 254–261 (2013).
Srinivasan, K., Viswanad, B., Asrat, L., Kaul, C. L. & Ramarao, P. Combination of high-fat diet and low-dose of streptozotocin-treated rat: A model for type 2 diabetes and pharmacological screening. Pharmacol. Res. 52, 313–320 (2005).
Correia-Santos, A. M. et al. Induction of type 2 diabetes by a low dose of streptozotocin and high-fat diet-fed in Wistar rats. Medicina (Ribeirão Preto). 45, 436–444 (2012).
Frendo-Cumbo, S., MacPherson, R. E. & Wright, D. C. Beneficial effects of combined resveratrol and metformin therapy in treating diet-induced insulin resistance. Physiol. Rep. 4, e12877. https://doi.org/10.14814/phy2.12877 (2016).
Palin, L. P. et al. Daily melatonin administration improves osseointegration in pinealectomized rats. J. Appl. Oral Sci. 10, e20170470. https://doi.org/10.1590/1678-7757-2017-0470 (2018).
Mulinari-Santos, G. et al. Losartan reverses impaired osseointegration in spontaneously hypertensive rats. Clin. Oral Implants Res. 29, 1126–1134 (2018).
Bouxsein, M. L. et al. Guidelines for assessment of bone microstructure in rodents using micro-computer tomography. J. Mineiro de Ossos Res. 25, 1468–1486 (2010).
Dalmolin, F. et al. Bone biomechanics and biomechanics essays—Theoretical foundations. Ciência Rural. 43, 1675–1682 (2013).
Suzuki, T. Y. U., Gomes-Filho, J. E., Bris, A. L. F., Assunção, W. G. & Santos, P. H. Influence of the depth of intraradicular dentin on the pushout bond strength of resin materials. J. Investig. Clin. Dent. 10, e12461. https://doi.org/10.1111/jicd.12461 (2019).
Chobot, A., Górowska-Kowolik, K., Sokołowska, M. & Jarosz-Chobot, P. Obesity and diabetes-not only a simple link between two epidemics. Diabetes Metab. Res. Rev. 34, e3042. https://doi.org/10.1002/dmrr.3042 (2018).
Ross, S. A. et al. Impact of weight gain on outcomes in type 2 diabetes. Curr. Med. Res. Opin. 27, 1431–1438 (2011).
Springer, M. & Moco, S. Resveratrol and its human metabolites-effects on metabolic health and obesity. Nutrients. 11, 143 (2019).
St Leger, A. S., Cochrane, A. & Moore, F. Factors associated with cardiac mortality in developed countries with particular reference to the consumption of wine. Lancet. 1, 1017–1020 (1979).
Renaud, S. & De Lorgeril, M. Wine, alcohol, platelets, and the french paradox for coronary heart disease. Lancet. 339, 1523–1526 (1992).
Frankel, E. N., Waterhouse, A. L. & Kinsella, J. E. Inhibition of human ldl oxidation by resveratrol. Lancet. 341, 1103–1104 (1993).
Jang, M. et al. Cancer chemopreventive activity of resveratrol, a natural product derivated from grapes. Science. 275, 2018–2020 (1977).
Chaplin, A., Carpéné, C. & Mercader, J. Resveratrol, metabolic syndrome, and gut microbiota. Nutrients. 3, 1651 (2018).
Kim, S., Jin, Y., Choi, Y. & Park, T. Resveratrol exerts anti-obesity effects via mechanisms involving down-regulation of adipogenic and inflammatory processes in mice. Biochem. Pharmacol. 81, 1343–1351 (2011).
Gracia, A. et al. Involvement of miR-539-5p in the inhibition of de novo lipogenesis induced by resveratrol in white adipose tissue. Food Funct. 7, 1680–1688 (2016).
Lasa, A. et al. Resveratrol regulates lipolysis via adipose triglyceride lipase. J. Nutr. Biochem. 23, 379–384 (2012).
Alberdi, G. et al. Changes in white adipose tissue metabolism induced by resveratrol in rats. Nutr. Metab. 8, 29 (2011).
Miranda, P. J., DeFronzo, R. A., Califf, R. M. & Guyton, J. R. Metabolic syndrome: definition, pathophysiology, and mechanisms. Am. Heart J. 149, 33–45 (2005).
De Ligt, M., Timmers, S. & Schrauwen, P. Resveratrol and obesity: Can resveratrol relieve metabolic disturbances?. Biochim. Biophys. Acta. 1852, 1137–1144 (2015).
Mendez-del, V. M., Gonzalez-Ortiz, M., Martinez-Abundis, E., Perez-Rubio, K. G. & Lizarraga-Valdez, R. Effect of resveratrol administration on metabolic syndrome, insulin sensitivity, and insulin secretion. Metab. Syndr. Relat Disord. 12, 497–501 (2014).
Gonzalez-Rodriguez, A. et al. Resveratrol treatment restores peripheral insulin sensitivity in diabetic mice in a sirt1-independent manne. Mol. Nutr. Food Res. 59, 1431–1442 (2015).
Yar, A. S., Menevse, S. & Alp, E. The effects of resveratrol on cyclooxygenase-1 and -2, nuclear factor kappa beta, matrix metalloproteinase-9, and sirtuin 1 mRNA expression in hearts of streptozotocin-induced diabetic rats. Genet. Mol. Res. 10, 2962–2975 (2011).
Şahin, G. et al. Lumbar and femoral bone mineral density in type 2 turkish diabetic patients. Acta Med. 44, 141–143 (2001).
Bo, S. et al. Impact of sirtuin-1 expression on H3K56 acetylation and oxidative stress: A double-blind randomized controlled trial with resveratrol supplementation. Acta Diabetol. 55, 331–340 (2018).
Tresguerres, I. F. et al. Resveratrol as anti-aging therapy for age-related bone loss. Rejuvenation Res. 17, 439–445 (2014).
Durbin, S. M. et al. Resveratrol supplementation preserves long bone mass, microstructure, and strength in hindlimb-suspended old male rats. J. Bone Miner. Metab. 32, 38–47 (2014).
Corrêa, M. G. et al. Impact of resveratrol in the reduction of the harmful effect of diabetes on peri-implant bone repair: Bone-related gene expression, countertorque and micro-CT analysis in rats. Acta Odontol. Scand. 79, 174–181 (2020).
Cutler, C. W. et al. Defective neutrophil function in na insulin-dependent diabetes mellitus patient: A case report. J. Periodontol. 62, 394401 (1991).
Hofbauer, L. C. et al. Osteoporosis in patients with diabetes mellitus. J. Bone Miner. Res. 22, 1317–1328 (2007).
Silva, A. G. & Lazaretti-Castro, M. Diabetes mellitus, thiazolidinediones and fractures: An unfinished story. Arq. Bras. Endocrinol. Metabol. 54, 345–351 (2010).
Den Dekker, A. et al. Targeting epigenetic mechanisms in diabetic wound healing. Transl. Res. 204, 39–50 (2019).
Al Zahrani, S. & Al Mutairi, A. A. Crestal bone loss around submerged and nonsubmerged dental implants in individuals with type-2 diabetes mellitus: A 7-year prospective clinical study. Med. Princ. Pract. 28, 75–81 (2019).
Al-Askar, M., Ajlan, S., Alomar, N. & Al-Daghri, N. M. Clinical and radiographic per-iimplant parameters and whole salivary interleukin-1b and interleukin-6 levels among type-2 diabetic and nondiabetic patients with and without peri-Implantitis. Med. Princ. Pract. 27, 133–138 (2018).
Acknowledgements
The São Paulo State Foundation for Research (FAPESP) awarded Carolina Sayuri Wajima undergraduate student (#2019/19019-0) and Ms. Letícia Pitol-Palin, a graduate scholarship (#2019/01634-0). Multiuser Laboratory at FOA/UNESP (FINEP 01.12.0530.00–PROINFRA 01/2011), where micro-CT was performed. The company Medens is acknowledged for supplying customized implants.
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to this study. Conceptualization, C.S.W, L.P.P., and R.O.; Methodology, C.S.W., L.P.-P., P.H.S., F.R.S.B., D.H.M., and R.O.; Software, C.S.W, L.P.-P., and R.O.; Formal analysis, R.O., and P.H.S.; Investigation, C.S.W, L.P.-P., and R.O.; Resources, C.S.W, L.P.-P., and R.O.; Data cura-tion, R.O.; Writing, review, and editing, C.S.W, L.P.-P., and R.O.; Supervision, R.O.; Funding acquisition, C.S.W, L.P.-P., and R.O.; Project administration, R.O. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wajima, C.S., Pitol-Palin, L., de Souza Batista, F.R. et al. Morphological and biomechanical characterization of long bones and peri-implant bone repair in type 2 diabetic rats treated with resveratrol. Sci Rep 14, 2860 (2024). https://doi.org/10.1038/s41598-024-53260-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53260-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.