Abstract
We explored the joint effects of different metabolic obesity phenotypes on all-cause and disease-specific mortality risk among the American population. Data were obtained from the National Health and Nutrition Examination Survey (NHANES) 1999–2018. Mortality outcome data were from mortality files linked to National Death Index record and follow-up information was up to December 31, 2019. 50,013 participants were finally included. Four metabolic obesity phenotypes were defined based on obesity and metabolic status: metabolically healthy obese (MHO), metabolically unhealthy obese (MUO), metabolically healthy non-obese (MHNO), and metabolically unhealthy non-obese (MUNO). Population-weighted Cox proportional hazards models were used to explore the all-cause and disease-specific mortality risk of metabolic obesity phenotypes. The all-cause mortality risk of MUO and MUNO was significantly higher than MHNO. MUNO was associated with a significantly increased risk of death from heart disease (HR: 1.40, 95% CI 1.16–1.70), hypertension (HR: 1.68, 95% CI 1.34–2.12), diabetes (HR: 2.29, 95% CI 1.67–3.15), and malignant neoplasms (HR:1.29, 95% CI 1.09–1.53). Metabolic unhealth significantly increased the risk of all-cause mortality, regardless of obesity status. Among individuals with metabolic unhealthy status, obesity significantly reduced the risk of all-cause mortality (HR: 0.91, 95% CI 0.85–0.98). Our study highlights the importance of identifying and characterizing metabolic obesity phenotypes in obese and metabolically abnormal patients, as well as healthy adults. Comprehensive evaluation of obesity and metabolic status is necessary to adopt appropriate interventions and treatment measures and maximize patient benefit.
Similar content being viewed by others

Introduction
Obesity has become a critical public health problem worldwide. The World Health Organization (WHO) estimates that the global number of individuals with obesity has exceeded 600 million1. The reported age-adjusted prevalence of obesity in the United States (US) was 37.7% (95% confidence interval CI 36.1–39.7%) during 2013–2014 and has been continuously increasing each year2. Numerous epidemiological studies have established strong associations between obesity and non-communicable chronic diseases3, metabolic abnormalities4,5, and increased mortality rates6,7. A systematic review of 239 prospective studies demonstrated that overweight and obesity were significantly associated with increased mortality rates8. These findings have been corroborated in numerous studies and systematic reviews reporting that obese individuals have a significantly higher risk of cardiovascular disease9, type 2 diabetes10, malignant tumors11, and metabolic abnormalities, such as hypertriglyceridemia12 and insulin resistance13,14, compared with individuals of normal weight.
However, not all obese people have metabolic problems; on the other hand, a significant proportion of individuals with normal weight, those who were usually considered healthy, might develop metabolic abnormalities as well. Studies have indicated that approximately 30% of obese individuals in Europe have relatively healthy metabolic profiles, with normal glucose tolerance, blood pressure, and lipid levels15. The WHO estimates that approximately 200 million people worldwide fall into the category of "obese but metabolically healthy"16. Researchers have defined this phenotype as metabolically healthy obesity (MHO). A study using National Health and Nutrition Examination Survey (NHANES) data from 1999 to 2018 found that the standardized prevalence of MHO in the US population increased significantly from 3.2% (95% CI 2.6–3.8%) during 1999–2002 to 6.6% (95% CI 5.3–7.9%) during 2015–201817. Some researchers consider MHO to be a benign condition15, but this remains controversial, and a considerable number of studies refute this claim. A large-scale population-based study in Korea found that obese individuals, regardless of metabolic status, had an increased risk of all-cause mortality and cardiovascular events in the long term18. Researchers have found that normal weight individuals with significant metabolic abnormalities have lower insulin sensitivity, higher oxidative stress levels, and higher blood pressure levels similar to those observed in obese individuals19,20. Epidemiological studies have also suggested that in Asian populations, people who are metabolically unhealthy and non-obese (MUNO) have significantly higher risks of all-cause mortality and non-fatal and fatal cardiovascular events compared with metabolically healthy non-obese (MHNO) individuals18,21.
It is important to fully consider both obesity and metabolic status, as well as their combined effects, when estimating mortality risks. Previous studies have predominantly focused on the health effects of the MHO phenotype, with results showing considerable heterogeneity. Furthermore, there is limited research on the mortality risks associated with other metabolic obesity phenotypes in the US population. We aimed to address these knowledge gaps using large-scale survey data from NHANES, which are representative of the US population, to investigate the joint effects of obesity and metabolic status.
Results
Baseline characteristics
Among 50,013 participants, there were 24,141 men and 25,872 women. 45,184 participants with complete information on main evaluation indicators and covariables were included in the analysis model. The MUNO phenotype group was the largest (n = 16,966), and the MHO (n = 5063) was the smallest (Table 1). The SBP, DBP, FPG, and TG values of metabolically unhealthy participants were significantly higher than those of metabolically healthy individuals, but HDL-C levels were significantly lower. There were significant differences in the distribution of demographic characteristics (including age, sex, race, family income, and education level) among the different metabolic obesity phenotypes (p < 0.001).
Risk of mortality with different metabolic obesity phenotypes
According to Table 2, the weighted median and inter-quartile range (IQR) follow-up time for four metabolic obesity phenotypes were 8.75 (9.33) years for MUO, 9.83 (9.67) years for MUNO, 8.50 (9.58) years for MHO, and 9.58 (9.58) years for MHNO, respectively, with a total of 7544 deaths. The distribution of follow-up time for four metabolic obesity phenotypes was shown in Supplementary Fig. 1. There were significant differences in survival status among participants with different metabolic obesity phenotypes (Fig. 1). Among them, the MUNO group had the highest weighted all-cause mortality rate (16.38/person year) and the MHNO group had the lowest rate (5.66/person year). For deaths from heart disease, hypertension, and malignant neoplasm, the weighted mortality rates, which were calculated using constructed 20-year sampling weights to ensure the representativeness of overall American population, in the MUNO phenotype were higher than those in the other groups. For diabetes mortality, the MUO group had the highest risk of mortality.
Compared with the MHNO phenotype, the all-cause mortality risks of the MUO (HR: 1.28, 95% CI 1.16–1.41) and MUNO groups (HR: 1.39, 95% CI 1.27–1.52) were significantly increased after adjusting for confounders; there was no significant difference between the MHO and MHNO phenotypes (Table 3). The risks of various causes of mortality in the MUNO group were significantly higher than those in the MHNO group, even after adjusting for the covariates. For participants with the MUO phenotype, the risks of heart disease, hypertension, and diabetes mortality were 1.55 (95% CI 1.27–1.88), 1.67 (95% CI 1.30–2.15), and 3.86 (95% CI 2.70–5.51) times higher than those in the MHNO group, respectively. There was no significant difference in the risk of malignant neoplasm mortality between MUO and MHNO phenotypes.
Subgroup analysis and sensitivity analysis
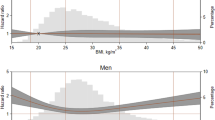
In this study, interaction and subgroup analysis were carried out according to metabolic status and BMI (Fig. 2). The results suggested that BMI modified the risk of all-cause death of metabolic abnormalities in the fully adjusted model (p for interaction = 0.025). Among participants with a metabolically healthy phenotype, obesity increased the risk of diabetes mortality but had no significant effect on all-cause mortality or other causes of death. For those with metabolic unhealthy status, we found that obesity had a protective effect on the risk of all-cause death (HR: 0.91, 95% CI 0.85–0.98) but significantly increased the risk of diabetes mortality (HR: 2.14, 95% CI 1.56–2.94). However, metabolic abnormalities significantly increased the risk of death from all causes and multiple causes in non-obese people; similar effects of metabolic abnormalities could be seen in obese people (except for the risk of death owing to malignant tumors).
Death risk of metabolic obesity phenotypes stratified by metabolic syndrome and obesity categories. MH metabolically healthy, MU metabolically unhealthy, NO non-obesity, O obesity, MetS metabolic syndrome. HRs were calculated based on weighted cox regression model after adjusting for age, gender, race, smoking status, drinking habit, socioeconomic status and education level. p for interaction was calculated based on Wald test. All-cause mortality, p for interaction = 0.025; Heart disease mortality, p for interaction = 0.644; Hypertension mortality, p for interaction = 0.984; Diabetes mortality, p for interaction = 0.601; Cancer mortality, p for interaction = 0.257. *Statistically significant.
Subgroup analysis was conducted stratified by age, sex, and race (Table 4). Compared with the reference MHNO phenotype, the MUO and MUNO phenotypes had a higher risk of all-cause mortality among adults aged 20–40 years. The MHO phenotype also increased the risk of death in adults aged 40–60 years; only the MUNO phenotype increased the risk of death in people over 60 years old. For participants of different sexes, the effects of metabolic phenotypes on the risk of all-cause mortality were similar to those of the general public. The risk of mortality varied greatly among different race groups. The association between metabolic obesity phenotypes and mortality was not statistically significant for Hispanic people.
Discussion
We defined four metabolic obesity phenotypes to distinguish obesity from its usual metabolic consequences and explore their joint effects on mortality. The study findings showed that the MUNO phenotype had the highest risk of all-cause mortality, followed by the MUO phenotype, and both had a significantly increased risk of mortality compared with the MHNO group. In contrast, the MHO phenotype showed no significant difference in risk compared with MHNO. Specifically, we found that obesity reduced the risk of all-cause mortality in people with metabolic abnormalities.
In recent years, several studies have focused on the mortality risk of metabolic obesity phenotypes among different populations. Our study was consistent with several large-scale prospective population studies conducted in multiple countries22,23,24,25. A community survey in the United Kingdom found that the risk of all-cause and cardiovascular disease mortality was significantly higher in participants with at least two metabolic abnormalities (regardless of obesity status) than in those with MHNO phenotype23. Another systematic review based on 13 cohort studies in European and American countries reached a similar conclusion26.
There is a view that the MHO phenotype does not exist as a distinct metabolic obesity phenotype but is rather a transient metabolic state that will gradually develop into MUO27,28. Researchers have found a significant association between the severity and duration of obesity and the incidence of metabolic abnormalities29, and individuals with the MHO phenotype have a higher risk of coronary heart disease, cerebrovascular disease, and heart failure than those with the MHNO phenotype30. Another view holds that MHO is a benign state and refers to this metabolic phenotype as "benign obesity"15. Population-based studies have reported that the risk of all-cause mortality in participants with the MHO phenotype showed no significant difference from that in participants with the MHNO phenotype, and a protective effect of the MHO phenotype on mortality has even been found in some studies. For example, Ortega et al. found that the risk of all-cause and cardiovascular disease mortality in individuals with MHO was 30–50% lower than that in individuals with the MUO phenotype15. In our study, we did not find any difference in the risk of all-cause mortality, heart disease, and hypertension mortality between the MHO phenotype and the control group (MHNO), which was consistent with the findings of Ortega et al.
However, we also find that MHO significantly increased the risk of diabetes mortality, which might be owing to misclassification of the MHO phenotype. One study suggested that 30% of BMI-defined obese participants were classified as MHO based on fasting blood glucose levels, but impaired glucose tolerance or even type 2 diabetes was detected when participants underwent oral glucose tolerance tests31, indicating that one-third of obese patients who were considered metabolically healthy actually had glucose metabolism disorders. BMI might lead to misclassification of obesity owing to its lack of sensitivity in distinguishing between fat and muscle tissue32, classifying as obese a healthy person with well-developed muscles or a person with relatively low visceral fat accumulation but a BMI above normal. It has been reported that body fat percentage is superior to BMI in identifying participants with impaired glucose tolerance33. Thus, indicators to more accurately evaluate obesity are necessary.
Another important finding is that weighted all-cause mortality and mortality owing to heart disease, hypertension, diabetes, and malignant tumors were higher in participants with the MUNO phenotype than in those with the MUO phenotype. Stratified analysis showed that regardless of obesity status, metabolic abnormalities significantly increased the risk of all-cause mortality as well as mortality rates from heart disease, hypertension, and diabetes, after adjusting for confounding factors. Obesity is significantly associated with the reduced risk of all-cause mortality in participants with metabolic abnormalities, which can explain why the risk of all-cause mortality in the MUNO phenotype was higher than that in the MUO phenotype. This result supports the existence of the “obesity paradox,” which has been reported in several studies34,35. Among people aged 60 years and older, only the risk of all-cause mortality in the MUNO phenotype was significantly increased; the risk of all-cause mortality in the MUO and MHO groups did not differ significantly from that in the MHNO phenotype. Better nutritional status, healthier cardiopulmonary function, and more medical interventions might be among the reasons explaining the obesity paradox. However, this does not mean that weight gain should be encouraged to reduce the risk of all-cause mortality because metabolic and cardiovascular complications are not the only adverse effects of obesity on health. In fact, the NCEP-ATP III considers overweight and obesity to be direct targets for metabolic syndrome intervention36. Additionally, the obesity paradox has also been widely questioned in recent years37. One viewpoint is that obesity is not the cause of obese people's reduced risk of mortality. Compared with emaciated people, obesity may not protect humans and reduce the risk of death. On the one hand, most people were greatly ill before they dead, such as cancer, and caused great losses in weight, while people who were still in normal weight or overweight at the time of death might not suffer from disease, resulting in a lower risk of death. On the other hand, patient's metabolic profiles could be different, even for the same BMI, and this profile could influence survival.
Currently, several popular hypotheses have been proposed to explain the differences in mortality risk among individuals with different metabolic phenotypes. First, lifestyle characteristics are important factors. Matheson et al. found that individuals who adopt healthy lifestyle habits (including moderate alcohol consumption, non-smoking, at least 30 min of exercise per day, and daily consumption of fruits and vegetables) had no significant difference in mortality rates compared with individuals who had normal BMI, even if they were obese38. It has been shown that lifestyle can change the body's energy metabolism processes, and exercising while consuming a high-energy diet can increase fatty acid oxidation. Additionally, insulin sensitivity is positively correlated with the ability to extract energy from fat tissue39. Second, visceral and ectopic fat accumulation and impaired fatty acid supply might also be possible reasons. It is generally believed that body fat distribution and adipose tissue dysfunction in abdominal fat are better predictors of obesity-related metabolic abnormalities than total fat mass itself40,41. However, under the current definition of the metabolic obesity phenotype, it is not possible to accurately determine the fat distribution, leading to heterogeneity across studies. Additionally, mechanisms such as insulin resistance, dysregulation of inflammatory regulation, and gut microbiota might also play a role4,42.
This study has some limitations. First, it has been shown that the duration of obesity is also an important predictor of metabolic risk in adults43, but our study lacked information regarding dynamic changes in BMI. Weight changes could have occurred over the follow-up period. Similar problems also existed in the evaluation of metabolic status. Second, a risk of misclassification was present. On the one hand, BMI lacks sensitivity to distinguish between fat and muscle, which may lead to inaccurate classification of obesity. On the other hand, the definition of metabolic abnormalities in this study relied only on the results of a single blood biochemistry test. Blood composition could be influenced by various short-term exposure factors, which might lead to misclassification of metabolic status. Additionally, we did not focus on specific types of metabolic abnormalities when defining metabolic unhealthy, which may have different effects on long-term risk estimation.
Our study emphasizes the importance of identifying and characterizing metabolic obesity phenotypes and the need to comprehensively evaluate the obesity and metabolic status of individuals, to adopt appropriate early interventions and treatment measures that maximize patient benefit. Our conclusions require further clinical and laboratory research with higher levels of evidence to elucidate the underlying mechanisms.
Methods
Participants and data collection
Data were obtained from NHANES, which uses a complex, multi-stage sampling design to ensure representativeness of the US population. Detailed sampling information can be obtained from the NHANES website44,45,46,47. The present research has been approved by the Ethics Committee48.
Our study included participants in 10 NHANES cycles from 1999 to 2018, excluding those who were aged less than 20 years (n = 46,325), those who were ineligible for mortality follow-up (n = 136), those who lacked essential information for calculating body mass index (BMI) and defining metabolic status (n = 4069), and those with BMI < 18.5 kg/m2 (n = 863). Finally, 50,013 participants were enrolled in this study (Fig. 3). Participants with missing information on covariates (n = 4829) would be removed from the regression analysis. Sensitivity analysis using indicator variables for missing data was also performed to avoid potential selection bias.
All participants signed an informed consent form.
Data collection
Information on demographic characteristics, lifestyle habits, and results of physical examinations and laboratory tests was collected. Demographic characteristics included age, gender, race, family income status, and education level. Smoking and drinking status, as well as medication history, were also recorded. The data above were self-reported by the participants themselves through face-to-face household interviews. Physical examination and blood sample collection were carried out in standardized mobile medical centers (MECs) by trained nurses49. Researchers developed strict quality control measures and standard operating procedures to ensure the reliability of data collection. Height and weight measurements were used to calculate the BMI. Blood pressure (BP) and serological indicators (fasting plasma glucose, triglyceride, and high-density lipoprotein cholesterol) were used to define the metabolic status.
Metabolic obesity phenotype criteria
BMI ≥ 30 kg/m2 was defined as obesity50. Metabolic status was defined according to the standardized definition proposed by National Cholesterol Education Program—Adult Treatment Panel III (NCEP-ATP III)36. Participants were defined as metabolic unhealthy if they had at least one of the four following components: (1) elevated blood pressure (BP; systolic BP [SBP] ≥ 130 mm Hg, diastolic BP [DBP] ≥ 85 mm Hg); (2) elevated fasting plasma glucose (FPG ≥ 110 mg/dL); (3) reduced high-density lipoprotein cholesterol (HDL-C < 40 mg/dL for men and < 50 mg/dL for women); or (4) elevated triglycerides (TG ≥ 150 mg/dL). Waist circumference was not included in the definition criteria owing to its strong collinear relationship with BMI17. Non-obese participants without metabolic abnormalities were defined as MHNO, and those with metabolic unhealthy were defined as MUNO. Participants with obesity who met the metabolic unhealthy criteria were classified as metabolically unhealthy obese (MUO) and those without metabolic problems were classified as MHO.
Outcomes and follow-up time
The National Center for Health Statistics (NCHS) links data collected from NHANES 1999–2018 with death certificate records from the National Death Index and releases a restricted-use version of the linked mortality files (LMF) to the public, which are available through the NCHS Research Data Center website51,52. The public-use LMF provides mortality follow-up data from the date of survey participation through December 31, 2019.
The primary outcome of the study was all-cause mortality. Secondary outcomes included mortality owing to heart disease (International Classification of Diseases Tenth Revision [ICD-10] codes 54–68) and malignant neoplasms (ICD-10 codes 19–43). Additionally, we analyzed the mortality rates of hypertension and diabetes, which are available from the current public-use LMF. Follow-up times were calculated using person-years from the date of the interview to the date of death or the end of the mortality period. Those with no final outcome events as of December 31, 2019 are treated as censored.
Covariates
We adjusted for demographic characteristics (including age, sex, race, family income, and education level) and lifestyle factors (including smoking and drinking habits) when exploring the association between mortality and different metabolic and obesity phenotype combinations. Race/ethnicity was divided into four categories (Non-Hispanic White, Non-Hispanic Black, Hispanic, and other races). Family income level was calculated by the ratio of household income to poverty ratio (IPR), and IPR greater than 1.3 was defined as a better socioeconomic condition53. Education level was categorized into three levels (less than high school, high school graduates or general education development, and some college or above). Smoking status was divided into non-smokers, former smokers, and current smokers. Participants who had drunk alcoholic beverages at least 12 times in the past year were considered to have a history of drinking.
Statistical analysis
We used SAS 9.4 (SAS Institute, Cary, NC, USA) for data analysis. We constructed 20-year combined MEC complex survey design weights for analysis according to the NHANES analytic guidelines. Continuous variables are described using weighted mean and standard deviation, and comparison between groups are conducted through weighted linear regression analysis. Categorical variables are summarized using number and percentage, and are compared based on Rao-Scott χ2 test.
We used Kaplan–Meier survival curves to describe the survival status of different metabolic obesity phenotypes. Cox proportional hazards regression models were applied to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of all-cause mortality associated with different metabolic obesity phenotypes. The proportional hazards assumption was examined through goodness-of-fit test and no significant deviation from the assumption was found. Two models were performed. Model 1 was unadjusted; Model 2 was adjusted for age, sex, race, smoking status, drinking habits, socioeconomic status, and education level. Observations with missing information on covariates will be removed from the analytical model. Competing-risks Cox regression analysis54 was performed to explore the associations among mortality from heart disease, hypertension, diabetes, malignant neoplasms, and different metabolic obesity phenotypes.
We further investigated the interaction effects of BMI and metabolic status on all-cause and various cause of mortality in the whole-population model. Subsequently, we performed subgroup analyses stratified by metabolic status, obesity groups, and demographic characteristics (age, sex, race), respectively, to explore the relationship among metabolic status, obesity and various mortality outcomes. Interaction and subgroup analysis were both fully adjusted, expect for the stratified factor itself in the subgroup analysis. Several sensitivity analyses were also performed. First, we excluded participants who died with less than 2 years of follow-up to eliminate the effects of death owing to other factors on metabolic obesity phenotypes and mortality associations. Second, participants with existing lung or heart disease and malignant neoplasms at baseline were excluded. Additionally, participants from last two survey cycles (NHANES 2015–2016 and 2017–2018) were excluded due to the short follow-up time. Finally, another newly-proposed metabolic syndrome definitions by the International Diabetes Federation (IDF) Task Force on Epidemiology and Prevention was used to evaluate metabolic status55.
Two-sided p ≤ 0.05 was considered statistically significant. All analysis were performed in accordance with the NHANES analytic guidelines56.
Institutional review board statement
The protocols of NHANES were approved by the National Center for Health Statistics and Center for Disease Control and Prevention Ethics Review Board. The reference number can be found on the NHANES website (https://www.cdc.gov/nchs/nhanes/irba98.htm).
Informed consent
Informed consent was obtained from all participants involved in the study.
Data availability
The datasets used and/or analyzed in the study are available from the NHANES website: (https://www.cdc.gov/nchs/nhanes/index.htm).
References
WHO. Obesity and overweight (2015).
Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315, 2284–2291 (2016).
Bauer, U. E., Briss, P. A., Goodman, R. A. & Bowman, B. A. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet 384, 45–52 (2014).
Blüher, M. Metabolically healthy obesity. Endocr. Rev. https://doi.org/10.1210/endrev/bnaa004 (2020).
Elagizi, A. et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 61, 142–150 (2018).
Chen, C., Ye, Y., Zhang, Y., Pan, X. F. & Pan, A. Weight change across adulthood in relation to all cause and cause specific mortality: Prospective cohort study. BMJ (Clin. Res. Ed.) 367, l5584 (2019).
Peeters, A. et al. Obesity in adulthood and its consequences for life expectancy: A life-table analysis. Ann. Intern. Med. 138, 24–32 (2003).
BMIMC Global et al. Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet (London, England) 388, 776–786 (2016).
Powell-Wiley, T. M. et al. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 143, e984–e1010 (2021).
Kahn, S. E., Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006).
Hopkins, B. D., Goncalves, M. D. & Cantley, L. C. Obesity and cancer mechanisms: Cancer metabolism. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 34, 4277–4283 (2016).
Simha, V. Management of hypertriglyceridemia. BMJ (Clin. Res. Ed.) 371, m3109 (2020).
Koren, D. & Taveras, E. M. Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metab. Clin. Exp. 84, 67–75 (2018).
Vishvanath, L. & Gupta, R. K. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. J. Clin. Investig. 129, 4022–4031 (2019).
Ortega, F. B. et al. The intriguing metabolically healthy but obese phenotype: Cardiovascular prognosis and role of fitness. Eur. Heart J. 34, 389–397 (2013).
Organization, W.H. Obesity and overweight fact sheet, Vol. 2023 (2013).
Wang, J. S. et al. Trends in the prevalence of metabolically healthy obesity among US adults, 1999–2018. JAMA Netw. Open 6, e232145 (2023).
Sung, K. C. et al. All-cause and cardiovascular mortality among Koreans: Effects of obesity and metabolic health. Am. J. Prev. Med. 49, 62–71 (2015).
Dvorak, R. V., DeNino, W. F., Ades, P. A. & Poehlman, E. T. Phenotypic characteristics associated with insulin resistance in metabolically obese but normal-weight young women. Diabetes 48, 2210–2214 (1999).
Lee, S. H. et al. Identifying metabolically obese but normal-weight (MONW) individuals in a nondiabetic Korean population: The Chungju Metabolic disease Cohort (CMC) study. Clin. Endocrinol. 75, 475–481 (2011).
Yang, H. K. et al. Obesity, metabolic health, and mortality in adults: A nationwide population-based study in Korea. Sci. Rep. 6, 30329 (2016).
Calori, G. et al. Prevalence, metabolic features, and prognosis of metabolically healthy obese Italian individuals: The Cremona Study. Diabetes Care 34, 210–215 (2011).
Hamer, M. & Stamatakis, E. Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J. Clin. Endocrinol. Metab. 97, 2482–2488 (2012).
Ogorodnikova, A. D. et al. Incident cardiovascular disease events in metabolically benign obese individuals. Obesity (Silver Spring, Md.) 20, 651–659 (2012).
Vander, A. D., Nooyens, A. C., Van Duijnhoven, F. J., Verschuren, M. M. & Boer, J. M. All-cause mortality risk of metabolically healthy abdominal obese individuals: The EPIC-MORGEN study. Obesity (Silver Spring, Md.) 22, 557–564 (2014).
Fan, J., Song, Y., Chen, Y., Hui, R. & Zhang, W. Combined effect of obesity and cardio-metabolic abnormality on the risk of cardiovascular disease: A meta-analysis of prospective cohort studies. Int. J. Cardiol. 168, 4761–4768 (2013).
Soriguer, F. et al. Metabolically healthy but obese, a matter of time? Findings from the prospective Pizarra study. J. Clin. Endocrinol. Metab. 98, 2318–2325 (2013).
Mathew, H., Farr, O. M. & Mantzoros, C. S. Metabolic health and weight: Understanding metabolically unhealthy normal weight or metabolically healthy obese patients. Metab. Clin. Exp. 65, 73–80 (2016).
Hwang, Y. C. et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int. J. Obes. 2005(39), 1365–1370 (2015).
Caleyachetty, R. et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J. Am. Coll. Cardiol. 70, 1429–1437 (2017).
Gómez-Ambrosi, J. et al. Increased cardiometabolic risk factors and inflammation in adipose tissue in obese subjects classified as metabolically healthy. Diabetes Care 37, 2813–2821 (2014).
Okorodudu, D. O. et al. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2005(34), 791–799 (2010).
Gómez-Ambrosi, J. et al. Body adiposity and type 2 diabetes: Increased risk with a high body fat percentage even having a normal BMI. Obesity (Silver Spring, Md.) 19, 1439–1444 (2011).
Horwich, T. B., Fonarow, G. C. & Clark, A. L. Obesity and the obesity paradox in heart failure. Prog. Cardiovasc. Dis. 61, 151–156 (2018).
Lennon, H., Sperrin, M., Badrick, E. & Renehan, A. G. The obesity paradox in cancer: A review. Curr. Oncol. Rep. 18, 56 (2016).
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 285, 2486–2497 (2001).
Dramé, M. & Godaert, L. The obesity paradox and mortality in older adults: A systematic review. Nutrients 15, 1780 (2023).
Matheson, E. M., King, D. E. & Everett, C. J. Healthy lifestyle habits and mortality in overweight and obese individuals. J. Am. Board Fam. Med. JABFM 25, 9–15 (2012).
Pujia, A. et al. Individuals with metabolically healthy overweight/obesity have higher fat utilization than metabolically unhealthy individuals. Nutrients 8, 2 (2016).
Bays, H. E. Adiposopathy is “sick fat” a cardiovascular disease?. J. Am. Coll. Cardiol. 57, 2461–2473 (2011).
Bays, H. E. Current and investigational antiobesity agents and obesity therapeutic treatment targets. Obes. Res. 12, 1197–1211 (2004).
Iacobini, C., Pugliese, G., Blasetti Fantauzzi, C., Federici, M. & Menini, S. Metabolically healthy versus metabolically unhealthy obesity. Metab. Clin. Exp. 92, 51–60 (2019).
Janssen, I., Katzmarzyk, P. T. & Ross, R. Duration of overweight and metabolic health risk in American men and women. Ann. Epidemiol. 14, 585–591 (2004).
Curtin, L. R. et al. The National Health and Nutrition Examination Survey: Sample design, 1999–2006. Vital Health Stat. 2, 1–39 (2012).
Curtin, L. R. et al. National Health and Nutrition Examination Survey: Sample design, 2007–2010. Vital Health Stat. 2, 1–23 (2013).
Johnson, C. L., Burt, V. L. & Mohadjer, L. K. National Health and Nutrition Examination Survey: Sample design, 2011–2014. Vital Health Stat. 2, 1–33 (2014).
Chen, T. C., Riddles, M. K., Mohadjer, L. K. & Fakhouri, T. H. I. National Health and Nutrition Examination Survey, 2015–2018: Sample design and estimation procedures. Vital Health Stat. 2, 1–35 (2020).
Survey, N.H.a.N.E. NCHS Ethics Review Board (ERB) Approval., Vol. 2022 (2003).
Zipf, G. C. M. et al. National Health and Nutrition Examination Survey: Plan and operations, 1999–2010. Vital Health Stat. 1, 1–37 (2013).
Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series, 894, 1–253 (2000).
Epidemiology, N.C.f.H.S.D.o.A.a. Continuous NHANES Public-use Linked Mortality Files (2019).
Statistics, N.C.f.H. The Linkage of National Center for Health Statistics Survey Data to the National Death Index — 2019 Linked Mortality File (LMF): Linkage Methodology and Analytic Considerations (2022).
Fadeyev, K., Nagao-Sato, S. & Reicks, M. Nutrient and food group intakes among U.S. children (2–5 years) differ by family income to poverty ratio, NHANES 2011–2018. Int. J. Environ. Res. Public Health 18, 11938 (2021).
Allinson, J. P. et al. Early childhood lower respiratory tract infection and premature adult death from respiratory disease in Great Britain: A national birth cohort study. Lancet (London, England) 401, 1183–1193 (2023).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
National Center for Health Statistics, C.f.D.C.a.P. The National Health and Nutrition Examination Survey (NHANES) Analytic and Reporting Guidelines (2006).
Acknowledgements
We want to express our gratitude to all the participants, primary care doctors, and nurses who took part in the survey. We thank Analisa Avila, MPH, ELS, of Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the language of a draft of this manuscript.
Funding
This study was supported by National High Level Hospital Clinical Research Funding (2022-PUMCH-C-058), Research Foundation of Capital Institute of Pediatrics (ERB-2023-01), and Capital's Funds for Health Improvement and Research (CFH2024-2G-1136).
Author information
Authors and Affiliations
Contributions
F.L.C. and Y.P.S. drafted the manuscript. M.Y., T.X. and J.T.L. designed the study. F.L.C., Y.P.S. and M.Y. performed the data analysis. Y.H.H., T.L. and Y.J.C. accessed and verified the data. Y.H.H., T.L., Y.J.C., T.X. and J.T.L. critically revised the manuscript. All authors have approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, F., Shi, Y., Yu, M. et al. Joint effect of BMI and metabolic status on mortality among adults: a population-based longitudinal study in United States. Sci Rep 14, 2775 (2024). https://doi.org/10.1038/s41598-024-53229-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53229-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.