Abstract
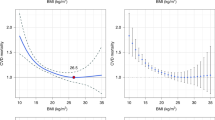
Previous studies on Chinese showed mixed results describing the relationship between obesity and mortality. The optimum levels of body mass index (BMI) and waist circumference (WC) are inconsistent. In the Guangzhou Biobank Cohort Study, after excluding ever smokers and those with poor health, 19,405 Chinese (50+ years) recruited from 2003 to 2008 were followed-up until 2017. During an average follow-up of 11.5 (standard deviation = 2.3) years, 1,757 deaths were recorded. All-cause mortality showed a J-shaped association with BMI, with the lowest mortality risks at 22.5 kg/m2 for both men and women. In those with BMI ≥ 22.5 kg/m2, an increase of 5 kg/m2 was associated with 29% higher all-cause mortality (hazard ratio (HR) = 1.29, 95% confidence interval (CI) 1.15–1.46), 30% higher cancer mortality (1.30, 95% CI 1.08–1.57), and 37% higher cardiovascular disease (CVD) mortality (1.37, 95% CI 1.13–1.67) after adjustment for potential confounders. In this first cohort study in one of the most economically developed cities in China, the lowest all-cause mortality was observed for a BMI of 22.5 kg/m2 in all participants, and a WC of 78 cm in men and 72 cm in women.
Similar content being viewed by others
Introduction
The global emergence of the obesity epidemic has serious adverse health effects. WHO Global Health Observation data shows that at least 2.8 million deaths and 35.8 million of Disability Adjusted Life Years are attributable to adiposity each year globally1. Most of the estimates above are based on studies in high-income countries several decades ago. As developing countries have only recently experienced a short period of obesity, the adverse population effects on morbidity or mortality have not been evident and tend to be underestimated. The effect in the low-to-middle income and high-income countries needs to be examined separately and the disease burden updated urgently.
China is now in the first stage of the obesity epidemic2, as indicated by a relatively low prevalence of obesity3,4 and obesity attributable mortality risk4,5,6. Although the prevalence is increasing rapidly7, its effect on mortality has yet to be elucidated. Moreover, previous studies of obesity and mortality did not comprehensively account for pre-existing illnesses, which, if ignored, may result in reverse causality. For example, unmeasured underlying disease reduces body weight and leads to an observation that lower body weight was detrimental and obesity was protective8,9,10,11. Additionally, the obesity-mortality association is often confounded by smoking, and simply adjusting for smoking status does not eliminate such confounding12. Studies failing to account for reverse causality and smoking might underestimate the excess risk due to overweight and obesity especially in never smokers13. Note that previous studies of Chinese populations did not show an adverse effect of overweight or obesity (i.e., BMI ≥ 24 or 28 kg/m2, respectively) on all-cause and cause-specific mortality9,10,11,14,15.
Although useful on a population level, for individuals BMI has some limitations due to its low discrimination of fat distribution. WC has also been used as a simple surrogate marker for central adiposity, yet the optimal WC varies across different ethnicities. Due to these uncertainties in the adiposity-mortality association and the optimal BMI and WC levels in Chinese, we used data from the Guangzhou Biobank Cohort Study (GBCS), a well-established population-based cohort of 30,000 people living in Guangzhou, China to examine the association between adiposity and mortality, accounting for reverse causation and smoking, and to identity the levels of BMI and WC with the lowest mortality risk.
Subjects and Methods
Study subjects
All participants of the GBCS were recruited from 2003 to 2008. Details of the GBCS have been reported elsewhere16,17. Briefly, all participants of the GBCS was from “The Guangzhou Health and Happiness Association for the Respectable Elders” (GHHARE). GHHARE is a community social and welfare organization unofficially aligned with the Guangzhou government. Membership is open to local residents aged 50+ years for a minimal nominal fee (sabout 50 US cents) per month. GHHARE included about 7% of residents in this age group, with branches in all districts of Guangzhou, a mega city in southern China. The baseline examination included a computer-based face-to-face interview by nurses. Information of demographic characteristics, lifestyle factors, family and personal medical history, and detailed assessment of anthropometrics, blood pressure, fasting plasma glucose, lipids and inflammatory markers was collected.
Adiposity measures
Anthropometric measures including standing height, body weight and WC were measured with light indoor clothing and no shoes according to a standard protocol. Height was measured to the nearest 0.1 cm and weight was measured to the nearest 0.1 kg16. BMI was calculated as weight divided by height squared (kg/m2). The Chinese-specific cut-offs for general adiposity, as per the World Health Organization (WHO) recommendation, were used, with underweight defined as BMI lower than 18.5 kg/m2, normal weight as BMI 18.5–24.9 kg/m2, overweight as BMI 25.0–27.4 kg/m2 and general obesity as BMI ≥ 27.5 kg/m218. According to Asian-specific cut-offs suggested by WHO, central obesity was defined by WC ≥ 90 cm in men and ≥80 cm in women19. Waist circumference (WC) was measured to the nearest 0.1 cm, using a non-stretch tape horizontally around the narrowest part of the torso between the lowest rib and the iliac crest.
Mortality
Information on underlying causes of deaths up to December 2017 was obtained via record linkage with the Death Registry of the Center for Disease Control and Prevention (CDC) in Guangzhou. Causes of death were coded by trained nosologists in each hospital. Causes of death were verified by CDC as part of their quality assurance programme by cross-checking past medical history and conducting verbal autopsy when the death certificates were not issued by medical institutions. Ten verbal autopsy meetings were conducted in the Guangzhou 12th Hospital to verify the deaths with uncertain causes. Coding of the endpoints in this study was shown in the Supplementary Table 1.
Statistical analysis
Analysis of variance or Chi-square tests were used to compare baseline characteristics by BMI/WC groups. Associations between BMI/WC and mortality were estimated by Cox regression giving hazard ratios (HRs) and 95% confidence intervals (CI). Potential confounders including age (as continuous), sex (except for breast cancer mortality), education (primary and below, secondary school, and college or above), occupation (manual, non-manual, and others), family income (<30,000 CNY/year, ≥30,000 CNY/year, and not known; US$1 = 7 CNY), International Physical Activity Questionnaire assessed physical activity (inactive, moderate and active)20, alcohol use (never, former, and current drinkers) and self-rated health (very good, good, poor and very poor). To limit biases that could be caused by underlying illnesses, the main analysis was done by excluding participants who reported poor health status and were ever smokers (including current and former smokers) at baseline. Poor health status at baseline was defined as any of the following conditions: (1) regular use of medication for chronic diseases, such as diabetes, hypercholesterolaemia, or vascular diseases, or (2) any hospital admission during past 6 months, or (3) self-reported cardiovascular disease history, or (4) self-reported cancer history3. Sensitivity analyses were also done in all participants (including ever and current smokers as well as those with poor health), as in most other studies5,6,21. All analysis was performed by STATA/IC 16.0.
Ethical considerations
This study was approved by the Guangzhou Medical Ethics Committee of the Chinese Medical Association. All participants signed informed consent before participation. The study was performed in accordance with the Declaration of Helsinki.
Results
At baseline, of the 30,430 participants, 391 lost to follow-up and 150 did not measure BMI or WC were excluded, giving 29,981 participants (21,698 women and 8,283 men). Of them, 5,830 participants who were former or current smokers, and 4,746 participants with poor health were excluded from the main data analysis of this paper, giving 16,840 women and 2,565 men. The mean (standard deviation) age of 19,405 participants was 62 (7.1) years. During the average follow-up of 11.5 (SD = 2.3) years or 225,867 person-years, 1,757 (women 1,371 (8.2%) and men 386 (15.1%)) deaths were recorded.
Most (62.4%) participants had a normal BMI of 18.5 to <25 kg/m2; 4.4% had a lower BMI (<18.5 kg/m2) and 33.2% had a greater BMI of ≥25 kg/m2 (Table 1). Participants with a lower BMI were older, more likely to be men, had higher education, and less likely to have lower manual occupation, be alcohol users and in good self-reported health (all P < 0.01) (Table 1). Similarly, participants with higher WC was older, less likely to be men, had lower education, more likely to have manual occupation and higher family income, be physically active and in good self-rated health (all P < 0.01, Table 1).
BMI and mortality
After excluding current and former smokers and those with poor health status, BMI showed a J-shaped association with the risk of all-cause mortality, with the lowest mortality risks at a BMI of 20 to <22.5 kg/m2. Compared with participants with BMI of 20 to <22.5 kg/m2, and with adjustment of age, sex, occupation, personal income, physical activity, alcohol use and self-rated health, participants with BMI of 27.5 kg/m2 and above (i.e., meeting the definition of obesity in China) had a 38% greater risk for all-cause mortality (HR 1.38, 95% CI 1.17–1.62), a 50% greater risk for cardiovascular disease mortality (HR 1.50, 95% CI 1.14–1.97), a 65% greater risk for ischemic heart disease (IHD) mortality (HR 1.65, 95% CI 1.06–2.56) and a 37% greater risk for cancer mortality (HR 1.37, 95% CI 1.06–1.78) (Table 2).
Figure 1 shows that, BMI in men and women at about 22.5 kg/m2 and WC at about 78 cm in men and 72 cm in women showed the lowest risk for all-cause mortality. Table 2 shows that in those with a BMI ≥ 22.5 kg/m2, an increase of 5 kg/m2 was associated with 29% greater all-cause mortality (HR 1.29, 95% CI 1.15–1.46), 37% higher CVD mortality (HR 1.37, 95% CI 1.13–1.67), 37% higher stroke mortality (HR 1.37, 95% CI 1.01–1.85), 30% higher all cancer mortality (HR 1.30, 95% CI 1.08–1.57) and 83% higher colorectal cancer mortality (HR 1.83, 95% CI 1.19–2.82). Further adjusting for WC or excluding those aged > = 85 years showed higher risks for low BMI but lower risks for high BMI (Supplementary Tables 2 and 3). Using the conventional Chinese-specific cut-offs for general obesity status, relative to normal weight (18.5 ≤ BMI < 25 kg/m2), general obesity (BMI ≥ 27.5 kg/m2) was associated with 30% (HR 1.30, 95% CI 1.13–1.50) greater risk of al-cause mortality, 35% greater risk of CVD mortality (HR 1.35, 95% CI 1.07–1.70), 32% greater risk of all cancer mortality (HR 1.32, 95% CI 1.06–1.65), and almost 2-fold risk of colorectal cancer (HR 1.86, 95% CI 1.09–3.18) (Supplementary Table 4). After adjustment for potential confounders related to baseline BMI groups (Supplementary Table 5), the patterns for BMI groups remained in all 29,981 participants including those who were smokers and with poor health, with slightly attenuated hazard ratios (Supplementary Table 6).
Association of body mass index (BMI) and waist circumference with all-cause mortality in 19,405 participants of the Guangzhou Biobank Cohort Study recruited during 2003–8 and followed up till December 2017, after excluding ever smokers and those with poor health status. All hazard ratios were adjusted for age, sex, occupation, personal income, physical activity, alcohol use and self-rated health.
WC and mortality
In men with WC of 78+ cm and women with WC of 72+ cm, after adjusting for age, sex, occupation, personal income, physical activity, alcohol use and self-rated health, each 10 cm greater WC was associated with 18% higher all-cause mortality (adjusted HR 1.18, 95% CI 1.10–1.27), 16% greater risk of CVD mortality (adjusted HR 1.16, 95% CI 1.03–1.30), 17% higher cancer mortality (adjusted HR 1.17, 95% CI 1.04–1.32) and 98% higher diabetes mortality (adjusted HR 1.98, 95% CI 1.20–3.27) (Table 3).
Sensitivity analyses showed that the HRs for WC groups attenuated slightly in all 29,981 participants including those who were ever smokers and with poor health (Supplementary Tables 7) Individuals who were classified as having central obesity were associated with an 18% greater risk of all-cause mortality (HR 1.18, 95% CI 1.07–1.30) (Supplementary Table 4). Changing the reference group to those with the lowest WC (Supplementary Table 8), or further adjusted for BMI or excluding participants with BMI < 18.5 kg/m2 showed similar results (Supplementary Tables 9 and 10).
Discussion
In this well-characterised population-based cohort of middle-aged to older Chinese, greater BMI and WC were associated with increased risk of all-cause mortality. The lowest all-cause mortality was among those with a BMI of 22.5 kg/m2, with no difference between men and women; the optimal WC varied by sex, being about 78 cm in men, and 72 cm in women. Adiposity above the optimum levels was associated with greater excess mortality risks, with dose response associations, for cardiovascular disease, cancer and stroke. The excesses were slightly smaller when current and former smokers and those with ill health were included, suggesting that reverse causality would lead to under-estimates of the excess risks.
The optimal BMI level of 22.5 kg/m2 in our study was lower than those of previous reports from China showing an optimal level of about 25 kg/m2 2,6,9. A previous meta-analysis including mostly studies from developed countries and decades ago21 or studies from China6,22 suggested individuals with overweight or grade 1 obesity (BMI 30–35 kg/m2) had a lower risk of all-cause mortality than those with normal BMI. For example, a recent large cohort study in China including more than 120,000 Chinese workers found a greater mortality risk in people with low BMI (<18.5 kg/m2) but no association for people with overweight (BMI ≥ 25 kg/m2) or general obesity (BMI ≥ 28 kg/m2), compared to normal weight (BMI 18.5–24.9)9. This study, as some other previous studies23,24,25,26, did not exclude those with pre-existing disease and smoking9, which might mask the BMI-mortality risk association. Moreover, inappropriate adjustment for mediating factors for the associations between BMI and major health endpoints (i.e., CVD), such as glycaemia, triglycerides and low-density lipoprotein cholesterol will attenuate the result towards the null9,27. One recent study in China also showed no association between greater BMI groups (i.e., BMI > 26, 28 or 30 kg/m2) and all-cause mortality, in subgroups by glycaemic status or in the whole sample15. Another recent study showed that after excluding participants with baseline metabolic abnormalities (hypertension, diabetes and/or dyslipidaemia), those with greater BMI (>28 kg/m2) had a greater risk of all-cause and CVD mortality, although the results were not statistically significant (HR 1.56, 95% CI 0.85–2.86 and 1.40, 95% CI 0.56–3.51)14. Our study, being the first in China to have excluded current and former smokers and those with poor health from a developed city in China, where the obesity epidemic may have progressed to a more advanced stage3, clearly showed that greater BMI (>27.5 kg/m2) was associated with a greater risk of all-cause, cancer and CVD mortality. Moreover, in our study, a 5 kg/m2 greater BMI was significantly associated with 37% risk of CVD mortality. This finding is well consistent with a recent large Mendelian randomization study showing a SD increase (1 SD = 4.5 kg/m2) in BMI was causally associated with 44% greater risk of CHD27.
Overweight and obesity have been associated with an increased risk of total cancer, where a 5 kg/m2 greater BMI is typically associated with a greater risk by about 30%13,28. However, the evidence showing adiposity causes cancer, to date, has come mainly from Caucasian populations28, with few data from Asians in whom body fat proportions can be substantially greater for a given BMI29,30. We found only a single prospective cohort study in Chinese men reporting no association between BMI and cancer in those with BMI of 23.5 kg/m2 or greater (HR 0·94, 95% CI 0·76–1·16)5. The discrepancies of the BMI-cancer association in different settings may be partly explained by differences in the prevalence of lifestyle factors (i.e., smoking and diet) and sex hormone in different ethnicities31. For example, meta-analyses of the Asia-Pacific Cohort Studies Collaboration (APCSC)13 and a few Asian studies showed that, elevated BMI was associated with greater risks of colorectal cancer, but not some sex hormone-related cancer, such as prostate cancer in populations from Asia32,33,34. In a study from China, greater BMI was associated with a greater risk of colorectal cancer in men but not women34. The authors suggested that mechanisms underlying this sex difference could be related to sex steroid hormone exposures34. Other large cohort studies in China did not report a significant association between obesity and colorectal cancer, probably due to the short duration of obesity (i.e., almost all Chinese were thin before the Open Door Policy since 40 years ago) in subjects included in the previous studies5,6. Our results support the statement from the World Cancer Research Fund that adiposity was causally associated with greater risk of colorectal cancer mortality5,6. Furthermore, our study demonstrated a significantly increased risk of cancer mortality from greater BMI. Our results indicate that the statement that obesity is “only a negligible cause of cancer overall”5 in China needs to be reviewed and updated. We did not have enough events to analyse prostate cancer as few deaths from prostate cancer were observed in our cohort.
Our study had several limitations. The first limitation was that only baseline measures of adiposity were used in the current analysis. Information of weight fluctuation (i.e., weight gain or weight loss during the follow-up) and obesity duration was not included. Second, as all participants in our study were aged 50 years or above, generalizability of the results to younger populations, or to non-Chinese may be limited. Third, our sample size is not large compared to other studies on obesity and mortality conducted mainly in the West12,21. However, with sufficient follow-up and carefully accounting for reverse causality and confounding, we were able to demonstrate that, in such a less obese population with a relatively short obesity duration, obesity-induced mortality risk has been substantial and become comparable to the more developed settings12, suggesting the obesity epidemic is expanding and may have come to an advanced stage in large cities in China (i.e., Guangzhou) before an obvious epidemic can be observed in the whole country. While we expect further follow up of our cohort and future studies may show greater excess risks from adiposity with the expanding of the obesity epidemic2, our results highlight that previous studies could have under-estimated the risks, and the cut-off values for over-weight and obesity for Chinese need to be reviewed urgently to support public health actions for obesity control. Our results also forewarn the expanding obesity epidemic in other rapidly developing countries in Asia and elsewhere. Strengths of this study included large sample size compared with other studies in Asia, long follow-up duration, comprehensive assessment of adiposity and lifestyle factors, accurate information about the causes of deaths, and the city-wide representative sample which should have minimized selection bias.
In conclusion, this first cohort study on non-smoking healthy Chinese in one of the most economically developed city in China found that greater BMI or WC was associated with increased risk of all-cause mortality. The lowest all-cause mortality was observed at a BMI of 22.5 kg/m2 in all participants, and a WC of 78 cm in men and 72 cm in women. Our results showed that the obesity epidemic in China, which is still at an early stage, may have come to a more advanced stage in large cities. Many other low- and middle-income countries are developing rapidly and our results can forewarn the expanding obesity epidemic and the related disease burden, especially in large cities. Urgent and more stringent actions are needed to halt the epidemic of obesity in the China and globally.
Data availability
Due to ethical restrictions protecting patient privacy, data available on request from the Guangzhou Biobank Cohort Study Data Access Committee. Please contact us at gbcsdata@hku.hk for fielding data accession requests.
References
Global Health Observatory (GHO) data. http://www.who.int/gho/ncd/risk_factors/obesity_text/en/ [Access on August 2nd, 2016]. (2016).
Xu, L. & Lam, T. H. Stage of obesity epidemic model: Learning from tobacco control and advocacy for a framework convention on obesity control. J Diabetes, https://doi.org/10.1111/1753-0407.12647 (2018).
Xu, L. et al. Changes in adiposity in an older Chinese population in rapid economic transition. Obes. 24, 2217–2223, https://doi.org/10.1002/oby.21599 (2016).
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781, https://doi.org/10.1016/S0140-6736(14)60460-8 (2014).
Chen, Z. et al. Body mass index and mortality in China: a 15-year prospective study of 220 000 men. Int. J. Epidemiol. 41, 472–481, https://doi.org/10.1093/ije/dyr208 (2012).
Gu, D. et al. Body weight and mortality among men and women in China. JAMA 295, 776–783, https://doi.org/10.1001/jama.295.7.776 (2006).
Xi, B. et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes. Rev. 13, 287–296, https://doi.org/10.1111/j.1467-789X.2011.00944.x (2012).
Lam, T. H. & Xu, L. Commentary: Fundamental limitations of meta-analysis of cohort studies, epidemiological challenges and the stage of obesity epidemic. Int. J. Epidemiol. 46, 547–548, https://doi.org/10.1093/ije/dyw309 (2017).
Sun, H. et al. Association between body mass index and mortality in a prospective cohort of Chinese adults. Med. 95, e4327, https://doi.org/10.1097/md.0000000000004327 (2016).
Wang, J. B. et al. Body Mass Index and Mortality: A 10-Year Prospective Study in China. Sci. Rep. 6, 31609, https://doi.org/10.1038/srep31609 (2016).
Wang, Y. F. et al. BMI and BMI Changes to All-cause Mortality among the Elderly in Beijing: a 20-year Cohort Study. Biomed. Environ. sciences: BES. 30, 79–87, https://doi.org/10.3967/bes2017.011 (2017).
Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. The Lancet, 388, 776–786, https://doi.org/10.1016/S0140-6736(16)30175-1 (2016).
Parr, C. L. et al. Body-mass index and cancer mortality in the Asia-Pacific Cohort Studies Collaboration: pooled analyses of 424 519 participants. Lancet Oncol. 11, 741–752, https://doi.org/10.1016/S1470-2045(10)70141-8 (2010).
Zhang, R. et al. Obesity, metabolic abnormalities, and mortality in older men. J. geriatric cardiology: JGC 15, 422–427, https://doi.org/10.11909/j.issn.1671-5411.2018.06.004 (2018).
Zhao, Y. et al. Body mass index and risk of all-cause mortality with normoglycemia, impaired fasting glucose and prevalent diabetes: results from the Rural Chinese Cohort Study. J. Epidemiol. Community Health 72, 1052–1058, https://doi.org/10.1136/jech-2017-210277 (2018).
Jiang, C. et al. Cohort profile: The Guangzhou Biobank Cohort Study, a Guangzhou-Hong Kong-Birmingham collaboration. Int. J. Epidemiol. 35, 844–852, https://doi.org/10.1093/ije/dyl131 (2006).
Xu, L. et al. Liver enzymes and incident diabetes in China: a prospective analysis of 10 764 participants in the Guangzhou Biobank Cohort Study. Journal of epidemiology and community health, jech-2015-205518, (2015).
WHO, E. C. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363, 157–163, https://doi.org/10.1016/s0140-6736(03)15268-3 (2004).
Alberti, K. et al. Harmonizing the Metabolic Syndrome A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
DENG, H. B. et al. Reliability and Validity of the IPAQ-Chinese: The Guangzhou Biobank Cohort Study. Med. Sci. Sports Exerc. 40, 303–307, https://doi.org/10.1249/mss.0b013e31815b0db5 (2008).
Flegal, K. M., Kit, B. K., Orpana, H. & Graubard, B. I. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309, 71–82, https://doi.org/10.1001/jama.2012.113905 (2013).
Chen, Z. et al. Body mass index and mortality in China: a 15-year prospective study of 220 000 men. Int. J. Epidemiol. 41, 472–481, https://doi.org/10.1093/ije/dyr208 (2012).
Prospective Studies, C. et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 373, 1083–1096, https://doi.org/10.1016/S0140-6736(09)60318-4 (2009).
Berrington de Gonzalez, A. et al. Body-mass index and mortality among 1.46 million white adults. N. Engl. J. Med. 363, 2211–2219, https://doi.org/10.1056/NEJMoa1000367 (2010).
Lin, W. Y. et al. Body mass index and all-cause mortality in a large Chinese cohort. CMAJ: Can. Med. Assoc. J. = J. de. l’Association medicale canadienne 183, E329–336, https://doi.org/10.1503/cmaj.101303 (2011).
Adams, K. F. et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N. Engl. J. Med. 355, 763–778, https://doi.org/10.1056/NEJMoa055643 (2006).
Xu, L., Borges, M. C., Hemani, G. & Lawlor, D. A. The role of glycaemic and lipid risk factors in mediating the effect of BMI on coronary heart disease: a two-step, two-sample Mendelian randomisation study. Diabetologia 60, 2210–2220, https://doi.org/10.1007/s00125-017-4396-y (2017).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–578, https://doi.org/10.1016/S0140-6736(08)60269-X (2008).
Deurenberg, P., Deurenberg-Yap, M. & Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 3, 141–146 (2002).
Rush, E. C., Freitas, I. & Plank, L. D. Body size, body composition and fat distribution: comparative analysis of European, Maori, Pacific Island and Asian Indian adults. Br. J. Nutr. 102, 632–641, https://doi.org/10.1017/S0007114508207221 (2009).
Xu, L., Au Yeung, S. L., Kavikondala, S., Leung, G. M. & Schooling, C. M. Testosterone concentrations in young healthy US versus Chinese men. Am. J. Hum. Biol. 26, 99–102, https://doi.org/10.1002/ajhb.22482 (2014).
Fowke, J. H. et al. Associations of body mass index, smoking, and alcohol consumption with prostate cancer mortality in the Asia Cohort Consortium. Am. J. Epidemiol. 182, 381–389, https://doi.org/10.1093/aje/kwv089 (2015).
Baade, P. D., Youlden, D. R., Cramb, S. M., Dunn, J. & Gardiner, R. A. Epidemiology of prostate cancer in the Asia-Pacific region. Prostate Int. 1, 47–58, https://doi.org/10.12954/PI.12014 (2013).
Li, H. et al. Body weight, fat distribution and colorectal cancer risk: a report from cohort studies of 134255 Chinese men and women. Int. J. Obes. 37, 783–789, https://doi.org/10.1038/ijo.2012.152 (2013).
Acknowledgements
The Guangzhou Biobank Cohort Study investigators include: Guangzhou No. 12 Hospital: WS Zhang, M Cao, T Zhu, B Liu, CQ Jiang (Co-PI); The University of Hong Kong: CM Schooling, SM McGhee, GM Leung, R Fielding, TH Lam(Co-PI); The University of Birmingham: P Adab, GN Thomas, KK Cheng (Co-PI). This work was supported by the National Key R&D Program of China (2017YFC0907100), the National Natural Science Foundation of China (NSFC: 81941019) and the Natural Science Foundation of Guangdong (2018A030313140). The Guangzhou Biobank Cohort Study was funded by The University of Hong Kong Foundation for Educational Development and Research (SN/1 f/HKUF-DC;C20400.28505200), the Health Medical Research Fund (Grant number: HMRF/13143241) in Hong Kong; the Guangzhou Public Health Bureau (201102A211004011) and the Guangzhou Science and Technology Bureau, Guangzhou, China (2002Z2-E2051; 2012J5100041; 2013J4100031; 201704030132); the University of Birmingham, UK.
Author information
Authors and Affiliations
Contributions
C.Q.J., L.X., T.H.L., K.K.C., W.S.Z., Y.L.J. and F.Z. have substantial contributions to conception and design, acquisition of funding, data and interpretation of data; C.Q.J., L.X. and T.H.L. analyzed the data, L.X., T.H.L. and C.Q.J. drafted the article, T.H.L. and K.K.C. revised it critically for important intellectual content, and all authors contributed to final approval of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, C.Q., Xu, L., Zhang, W.S. et al. Adiposity and mortality in older Chinese: an 11-year follow-up of the Guangzhou Biobank Cohort Study. Sci Rep 10, 1924 (2020). https://doi.org/10.1038/s41598-020-58633-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-58633-z
This article is cited by
-
Cereal intake and mortality in older Chinese: a 15-year follow-up of a prospective cohort study
European Journal of Nutrition (2023)
-
Association between spicy foods consumption and cardiovascular disease risk factors: Guangzhou Biobank Cohort Study
BMC Public Health (2022)
-
Fluctuations in waist circumference increase diabetes risk: a 4-year cohort study in 61,587 older adults
Nutrition & Metabolism (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.