Abstract
The lymph node involvement in the posterior to level V (PLV) region is mainly observed in nasopharyngeal carcinoma (NPC). Recently, we have reported the distribution of metastatic lymph nodes in the PLV region and there are correlations between the neck node levels (NNL) of NPC, but what is the boundary of the PLV region and how to delineate it remains unclear, and we further to elaborate whether the bilateral level Va should be covered as intermediate-risk nodal regions (CTVn2, about 60 Gy equivalent) for all T and N categories based on these correlations. A total of 1021 consecutive NPC patients with N1-3 stage from January 2012 to December 2020 were reviewed. The lymph node metastasis level of each patient was evaluated according to the updated guidelines proposed in 2013. According to the distribution pattern of lymph node metastasis and the anatomical structure in the PLV region, the boundaries of PLV region was delineated, and whether it is appropriate to cover the bilateral level Va as CTVn2 for all the NPC patients was further discussed. The correlations of level Va with other NNL were studied using logistic regression model. The cranial boundary of PLV region is the caudal border of cricoid cartilage, the caudal boundary is the plane serratus anterior muscle begins to appear, the anterior boundary is the anterior border of trapezius, and the posterior boundary is the convergence of levator scapulae and trapezius. Laterally, the PLV region is limited by the medial edge of trapezius and medially by the lateral surface of levator scapulae. The nodal spread in level Va is based on the lymph node metastasis of level IIb in NPC. The PLV region is a missing NNL of head and neck tumors, especially in NPC. The proposed boundaries of the PLV region can provide a preliminary proposal for the further revision of NNL in head and neck tumors. It is theoretically feasible to reduce the prophylactic irradiation dose of the bilateral level Va in patients with N0 stage or with isolated metastases in level VIIa.
Similar content being viewed by others
Introduction
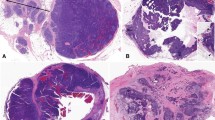
Nasopharyngeal carcinoma is a malignant tumor with a high rate of cervical lymph node metastasis1,2,3. Grégoire V et al. reported the recommendation for delineation of neck node target volumes based on the surgical experience in 20004. A set of consensus guidelines for the delineation of NNL in node negative patients was published in 20035, but not all the NNL were described in this consensus. A new consensus of the delineation of NNL for head and neck tumors was proposed in 2013 and accepted throughout the world (referred to as the 2013 guidelines)6. In the 2013 guidelines, 10 nodal groups were defined in accordance with the TNM atlas for cervical lymph nodes. However, there is no description of PLV region in the 2013 guidelines, and the PLV region is located in a deep gap between levator scapulae and trapezius. The metastatic lymph nodes can be observed in this region of some NPC patients (Fig. 1). Several studies have reported the metastasis rate of PLV region is 1.3–4.9%7,8,9. Unfortunately, the PLV region is often overlooked. We have reported the correlations between the PLV region and other NNL, the distribution of metastatic lymph nodes in the PLV region in our previous studies9,10, but what is the boundary of PLV region and how to delineate it is still unclear.
The yellow line represents trapezius, the red line represents levator scapulae, the green line presents the serratus anterior muscle, and the purple line presents the supraspinatus. (A, B) The PLV region in the CT scans, which is between levator scapulae and trapezius. The white arrows indicate the metastatic lymph nodes. (C, D) There is no space between levator scapulae and trapezius when the serratus anterior muscle appears on the CT image.
The international guideline recommended covering the bilateral level Va as CTVn2 for all the NPC patients11. Wang et al. had reported the lymph node metastasis rate of level Va in NPC is 21.5%7. Do we really need to cover the bilateral level Va of all the NPC patients within CTVn2 just because there are 21.5% of the patients have lymph node involvement in level Va? and there is no report.
This study aims to describe the boundaries of PLV region and to show how the PLV region is delineated. We hope to provide a preliminary proposal of boundary setting for the further revision of NNL in head and neck tumors. In addition, we further discuss whether it is appropriate to cover the bilateral level Va within CTVn2 for all the NPC patients.
Methods
Patient population
The study was retrospective in character and all methods were carried out in accordance with the ethical principles derived from the Declaration of Helsinki and its subsequent amendments (permission was obtained from the medical ethics committee of The General Hospital of Western Theater Command, the informed consent was exempted due to the retrospective nature of the study). There are 13 independent variables in our manuscript, and the lymph node metastasis rate of level Va is 21.5%7. The sample size was calculated by using the PASS software package (version 15.0, Power: 0.9, Alpha: 0.05, P0: 0.027, P1: 0.25) and the result is about 138 cases. We enrolled 1021 NPC patients whose records were retrospectively reviewed. The inclusion criterion was the patients had been pathologically confirmed as having NPC with any T and N1-3 stage according to the 8th edition of the AJCC/UICC staging system for NPC12, the tumor stages were also classified according to this staging system, and the exclusion criterion was the patients with N0 stage. All the patients were performed MRI scan before treatment.
The diagnostic criteria of lymph node involvement
All the MRI and contrast-enhanced CT images of the patients were reviewed. The metastatic NNL for each patient were assessed according to the 2013 guidelines6. The diagnosis of lymph node metastasis was evaluated according to the following criteria13: (1) minimal axial diameter ≥ 5 mm in the retropharyngeal region, and ≥ 10 mm for all other cervical nodes. (2) Any size of the lymph node with necrosis or ring enhancement. (3) Any size of the lymph node with extracapsular invasion or fusion. (4) More than three contiguous lymph nodes with the shortest diameter of 8–10 mm. We also referred to the PET/CT images if the patients underwent this examination.
Delineation of the boundaries in PLV region
The contrast-enhanced CT simulation images of an NPC patient with N0 stage were obtained before treatment. According to the distribution pattern of nodal spread and the anatomical structure in the PLV region, we delineated the cranial boundary, the caudal boundary, the anterior boundary, the posterior boundary, the lateral and medial boundary of PLV region on these CT images, respectively.
Ethical approval and consent to participate
As the images in our manuscript were obtained from patients, the presented study was reviewed and approved by the medical ethics committee of The General Hospital of Western Theater Command.
The medical ethics committee of the General Hospital of Western Theater Command approved the study (2023EC2-KY003). The informed consent was exempted due to the retrospective nature of the study. All methods were carried out in accordance with ethical principles derived from the Declaration of Helsinki and its subsequent amendments.
Statistical analysis
The logistic regression model was used to evaluate the correlations between level Va nodes and other NNL, and the exact conditional test was used for the quasi-complete separation of data points. The Hosmer–Lemeshow test was used to clarify the goodness of fit in logistic regression (p value > 0.05 showed good estimation of logistic model). Levels with less than a 3% metastatic rate were excluded in the logistic regression to avoid the bias. The SPSS 20.0 software and SAS software (SAS Institute Inc., Cary, NC, USA) was used to analyzed the data, statistical significance was defined as p < 0.05.
Results
Patient characteristics
There were 738 males and 283 females among 1021 NPC patients. The number of patients with T1, T2, T3, and T4 stage is 294 (28.8%), 198 (19.4%), 282 (27.6%), and 247 (24.2%), respectively. The number of patients with N1, N2, and N3 stage is 381 (37.3%), 452 (44.3%), and 188 (18.4%), respectively. The number of patients with stage II, III, IVa, and IVb is 192 (18.8%), 421 (41.2%), 389 (38.1%), and 19 (1.9%), respectively. All the patients’ baseline characteristics are listed in Table 1.
The patterns of lymph node involvement
The most common levels of lymph node metastasis are VIIa (86.2%), IIb (84.6%), and the metastasis rate of other NNL are as follows: IIa (62.6%), III (48.9%), Va (27.8%), IVa (16.8%), Vb (7.6%), Ib (5.9%), and PLV region (5.2%). The rate of lymph node involvement in levels IVb, VIIb, and VIII is less than 5.0%, and there is no nodal spread in levels Ia, VI, IX, and X. The patterns of lymph node involvement are shown in Supplementary Table 1.
The boundaries of PLV region
The cranial boundary of PLV region is the caudal border of cricoid cartilage, the caudal boundary is the plane serratus anterior muscle begins to appear, the anterior boundary is the anterior border of trapezius, and the posterior boundary is the convergence of levator scapulae and trapezius. Laterally, the PLV region is limited by the medial edge of trapezius and medially by the lateral surface of levator scapulae. The boundaries of PLV region are summarized in Table 2. A set of CT scans are provided to show how the PLV region is delineated in Figs. 2 and 3.
The PLV region and level V(a, b, c) was delineated in the axial, sagittal and coronal planes. The yellow line represents level Va, the red line represents level Vb, the blue line represents level Vc, the green line represents PLV region. (A, B) The axial planes. (C, D) The sagittal planes. (E, F) The coronal planes.
The number of patients with or without nodal spread in level Va simultaneously accompanied with nodal involvement in other NNL
The number of patients with or without nodal spread in level Va is 284 (27.8%) and 737 (72.2%), respectively. Among 61 patients with nodal involvement in level Ib, there are 37 (3.6%) and 24 (2.4%) patients accompanied with or without nodal spread in level Va, respectively. As calculated in this way, there are 236 (23.1%) and 403 (39.5%) patients in level IIa accompanied with or without nodal spread in level Va, there are 284 (27.8%) and 580 (56.8%) patients in level IIb accompanied with or without nodal spread in level Va. All the data are summarized in Table 3.
The correlations of level Va nodes with other NNL
There are 284 (27.8%) patients had nodal involvement in level Va. The p value of Hosmer–Lemeshow test was 0.807. The logistic regression analysis indicated level Va was correlated with level IIb (p < 0.0001, OR 1.519, 95% CI 0.765–+ infinity), III (p < 0.0001, OR 4.376, 95% CI 2.784–6.877), IVa (p < 0.0001, OR 3.437, 95% CI 2.089–5.655), Vb (p < 0.0001, OR 2.099, 95% CI 1.341–+ infinity), and PLV region (p < 0.0001, OR 2.071, 95% CI 1.269–+ infinity). The results were summarized in Supplementary Table 2.
Discussion
Nasopharyngeal carcinoma is one of head and neck tumors with a high rate of lymph node involvement14,15,16. Approximately 85% of the NPC patients were confirmed as having lymph node metastasis7,17. The PLV region is located in a deep gap between levator scapulae and trapezius, the metastatic lymph nodes can be observed in this region of some NPC patients, and the metastasis rate is 1.3–4.9%7,8,9, which was close to the metastasis rate of levels Ib and IVb in our study. However, there is no description of PLV region in the 2013 guidelines, which is a missing NNL for the head and neck tumors, especially in NPC. We think the accurate definition of PLV region can make the delineation of clinical target volumes (CTV) more accurately. The PLV region receives efferent lymphatics primarily from level V, the posterior neck and shoulder, and the lymph node involvement of PLV region is mainly associated with NPC. The PLV region extends from the anterior border of trapezius anteriorly to the convergence of levator scapulae and trapezius posteriorly, and from the caudal border of cricoid cartilage cranially to the plane serratus anterior muscle begins to appear caudally. We set the caudal border of cricoid cartilage as the cranial boundary of PLV region is because the space between levator scapulae and trapezius begins to appear at this plane. There is no space between levator scapulae and trapezius when the serratus anterior muscle begins to appear on the CT image, which we think is the caudal boundary of PLV region (Fig. 1), and we observed none of the involved lymph nodes in PLV region extended beyond this plane. The posterior boundary of levels Va and Vb is the anterior border of trapezius in the 2013 guidelines, which is the anterior boundary of PLV region in our study. There is no space behind the convergence of levator scapulae and trapezius, which is the posterior boundary of PLV region. The lateral and medial boundary of PLV region is the medial edge of trapezius and the lateral surface of levator scapulae, respectively. We observed all the involved lymph nodes in PLV region were distributed within the boundary range that we set. We must emphasize that the preliminary boundary setting of PLV region is based on the distribution pattern of nodal spread and the anatomical structure in this area from the 1021 NPC patients.
The 2013 guidelines subdivided level V into level Va, Vb, and Vc. We have reported all the correlations for the NNL of NPC in our previous study10. Unfortunately, we didn’t further elaborate whether level Va can be considered as CTVn2 for all NPC patients base on these correlations. Our study showed that the nodal involvement in level Va was related to levels IIb, III, IVa, Vb, and PLV region, but have no correlation with level VIIa. We observed all the patients with nodal involvement in level Vb or level Vc simultaneously had lymph node metastasis in level Va in our study, and all the 284 patients with nodal spread in level Va had lymph node metastasis in level IIb, there was no case with nodal involvement in level Va among the 157 patients who had no lymph node metastasis in level IIb (Table 3). A total of 144 patients had lymph node metastasis in level VIIa but without nodal involvement in level IIb in our study, and none of the 144 patients presented with nodal spread in level Va. There was no case who presented with lymph node involvement only in levels VIIa and Va in our study among the 1021 patients, and we didn’t observe a patient with isolated metastases in level V. Another study reported there was only 1 (0.1%, 1/924) NPC patient had nodal involvement in level V but without nodal spread in retropharyngeal region or level II17. Chone CT et al. had reported the histopathologic metastases in level II and III for all neck dissections are risk factors for metastases in the apex of the posterior triangle (the upper part of level V) in 51 patients with squamous cell carcinoma of head and neck tumors, and there was no case who only had lymph node metastasis in the upper part of level V18. Hamoir M et al. had reported the apex of level V (level Va) includes the drainage from occipital region and contains only superficial suprafascial occipital lymph nodes, the subfascial and submuscular lymph nodes located close to the occipital attachment of the sternocleidomastoid muscle19. From the anatomical structure in this region, the accessory nerve descends along the anterolateral side of the internal jugular vein after it exits the skull from the jugular foramen, and then passes through the anterior edge of the upper part of the sternocleidomastoid muscle to the deep surface of the trapezius muscle backward and downward. There are lymph nodes arranged along the accessory nerve, which means the lymph nodes can metastasize from level II to level V and PLV region along the accessory nerve, and this can explain why the nodal spread in level Va is mainly associated with level IIb and the lymph node metastasis in the PLV region is mainly associated with level Va. Therefore, the nodal spread in level Va is based on the lymph node involvement of level IIb in NPC.
Withers HR et al.had reported that the dose of 50 Gy can effectively control the potential lymph node involvement in the subclinical regions20, The rate of skip nodal involvement in NPC is quite low17,21,22,23, which means the lymph node metastasis of the uninvolved level is based on the involved levels and there are correlations between the NNL, so we just need to cover the NNL related to the involved levels rather than the whole neck as CTVn2, but the international guideline recommended covering the bilateral level Va as CTVn2 for all the NPC patients11. According to our analysis, there are about 15% of the NPC patients receive over prophylactic irradiation dose in the bilateral level Va because the rate of nodal spread in level IIb is about 85%, so it is inappropriate to perform high-dose prophylactic irradiation (about 60 Gy equivalent) on the bilateral level Va for all the NPC patients. Theoretically, the bilateral level Va can be considered as low-risk nodal regions (CTVn3, about 50 Gy equivalent) in patients with N0 stage or with isolated metastases in level VIIa (Fig. 4). We believe that it is beneficial for patients to reduce even 1 Gy of the prophylactic irradiation dose if the equivalent survival outcomes and regional control can be obtained, and high-dose prophylactic irradiation means the higher incidence of radioactive dermatitis and other dose-induced side effects. Furthermore, we consider the delineation of CTV based on the correlations of NNL rather than to cover the whole neck can reduce the prophylactic irradiation levels or dose of CTVn2.
The CTV delineation of NPC patient with nodal involvement in patients with N0 stage or with isolated metastases in level VIIa. (A, B) The CTV delineation recommended by the international guideline (the blue line represents CTVn2). (C, D) The CTV delineation recommended by this study (the red line represents CTVn2 and the green line represents CTVn3).
There are some limitations in this study. First, the lymph nodes in PLV region have no histopathology, performing histopathological examination and lymph node dissection in this deep region is difficult and not recommended for NPC patients. Second, lymph node metastasis in PLV region was mainly observed in NPC patients, and we don’t perform a further study to confirm whether the patients also present with lymph node involvement in the PLV region in other head and neck tumors. Third, there is no follow-up data to support the conclusion because this is a retrospective study, but it is a strong theoretical support for carrying out prospective research, and we are conducting a prospective study of the CTV delineation based on this conclusion, we will report the results in the future.
Conclusions
We report in detail the boundaries of PLV region and how to delineate it in NPC patients, which can provide a preliminary proposal for the further revision of NNL in head and neck tumors. We recommend using the PLV region as a new NNL. Theoretically, the bilateral level Va can be delineated as CTVn3 in patients with N0 stage or with isolated metastases in level VIIa.
Data availability
The datasets used during the current study available from the corresponding author on reasonable request.
Abbreviations
- PLV:
-
Posterior to level V region
- NPC:
-
Nasopharyngeal carcinoma
- NNL:
-
Neck node levels
- CTV:
-
Clinical target volumes
- CTVn2:
-
Intermediate-risk nodal regions
- CTVn3:
-
Low-risk nodal regions
References
Chen, Y. P. et al. Nasopharyngeal carcinoma. Lancet 394(10192), 64–80 (2019).
Guo, R. et al. The evolution of nasopharyngeal carcinoma staging. Br. J. Radiol. 92(1102), 20190244 (2019).
Guo, R. et al. Management of nasopharyngeal carcinoma: Current practice and future perspective. J. Clin. Oncol. 33(29), 3356–3364 (2015).
Grégoire, V., Coche, E., Cosnard, G., Hamoir, M. & Reychler, H. Selection and delineation of lymph node target volumes in head and neck conformal radiotherapy: Proposal for standardizing terminology and procedure based on the surgical experience. Radiother. Oncol. 56, 135–150 (2000).
Grégoire, V. et al. CT based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC, RTOG consensus guidelines. Radiother. Oncol. 69, 227–236 (2003).
Grégoire, V. et al. Delineation of the neck node levels for head and neck tumors: A 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother. Oncol. 110(1), 172–181 (2014).
Wang, X. et al. Patterns of lymph node metastasis from nasopharyngeal carcinoma based on the 2013 updated consensus guidelines for neck node levels. Radiother. Oncol. 115(1), 41–45 (2015).
Ding, Z. X. et al. Value of radiation therapy oncology group guidelines base on MR imaging in diagnosing lymph node metastasis of nasopharyngeal carcinoma. Chin. J. Cancer. 28(5), 533–537 (2009).
Jiang, C. et al. Distribution pattern and prognosis of metastatic lymph nodes in cervical posterior to level V in nasopharyngeal carcinoma patients. BMC Cancer. 20(1), 667 (2020).
Jiang, C. et al. Correlation analysis of neck node levels in 960 cases of Nasopharyngeal carcinoma (NPC). Radiother. Oncol. 161, 23–28 (2021).
Lee, A. W. et al. International guideline for the delineation of the clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiother. Oncol. 126, 25–36 (2018).
Pan, J. J. et al. Proposal for 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer. 122(4), 546–558 (2016).
Wijers, O. B. et al. A simplified CT-based definition of the lymph node levels in the node negative neck. Radiother. Oncol. 52, 35–42 (1999).
Ho, F. C., Tham, I. W., Earnest, A., Lee, K. M. & Lu, J. J. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: A meta-analysis of clinical evidence. BMC Cancer. 12, 98 (2012).
Ma, H. et al. Prognostic significance of quantitative metastatic lymph node burden on magnetic resonance imaging in nasopharyngeal carcinoma: A retrospective study of 1224 patients from two centers. Radiother. Oncol. 151, 40–46 (2020).
Wang, L., Huang, S., Zhang, L., He, X. & Liu, Y. Recommendation regarding the cranial upper border of level IIb in delineating clinical target volumes (CTV) for nasopharyngeal carcinoma. Radiat. Oncol. 15(1), 270 (2020).
Tang, L. et al. The volume to be irradiated during selective neck irradiation in nasopharyngeal carcinoma: Analysis of the spread patterns in lymph nodes by magnetic resonance imaging. Cancer. 115(3), 680–688 (2009).
Chone, C. T., Crespo, A. N., Rezende, A. S., Carvalho, D. S. & Altemani, A. Neck lymph node metastases to the posterior triangle apex: Evaluation of clinical and histopathological risk factors. Head Neck. 22(6), 564–571 (2000).
Hamoir, M. et al. Prevalence of lymph nodes in the apex of level V: A plea against the necessity to dissect the apex of level V in mucosal head and neck cancer. Head Neck. 27, 963–969 (2005).
Withers, H. R., Peters, L. J. & Taylor, J. M. Dose-response relationship for radiation therapy of subclinical disease. Int. J. Radiat. Oncol. Biol. Phys. 31(2), 353–359 (1995).
Kang, M. et al. A novel N staging system for NPC based on IMRT and RTOG guidelines for lymph node levels: Results of a prospective multicentric clinical study. Oncol. Lett. 308, 16 (2018).
Li, W. F. et al. Locoregional extension patterns of nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Chin. J. Cancer. 31, 579–587 (2012).
Cao, C. et al. Locoregional extension and patterns of failure for nasopharyngeal carcinoma with intracranial extension. Oral Oncol. 79, 27–32 (2018).
Funding
This work was supported by the medical science and technology project of the health planning committee of Sichuan in China (No. 21PJ068).
Author information
Authors and Affiliations
Contributions
The conception and design of the study: J.-C.Y., W.J. Drafting the article: J.-C.Y. Figures drawing: L.-Z.H., G.-B.L. The acquisition of data: W.J., G.-B.L., L.-X.K., L.-Z.H. The revision of manuscript: Z.L., Z.T. and G.H. Final approval of the version to be submitted: J.-C.Y. All authors contributed to the article and approved the submitted version. All authors have approved the manuscript and agree with submission to Scientific Reports.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, C., Li, X., Zhang, L. et al. The boundary of posterior to level V region and the theoretical feasibility of irradiation dose reduction of level Va in nasopharyngeal carcinoma. Sci Rep 14, 2308 (2024). https://doi.org/10.1038/s41598-024-52857-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52857-z
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.